We read with interest the study by Izquierdo et al. [1] that reported a lower proportion of patients with concurrent asthma and coronavirus disease 2019 (COVID-19), compared to other chronic diseases. During the ongoing pandemic, various studies have also observed a lower occurrence of persons with asthma amongst hospitalised COVID-19 cases [2, 3]. Several hypotheses have been postulated to account for these observations, including lower susceptibility to COVID-19 amongst patients with asthma [2, 3] and a remission in rates of common circulating respiratory viral infections (RVIs) [4]. RVIs are potential triggers of asthma exacerbations and may cause a loss of asthma control [5]. During the COVID-19 pandemic, community-wide public health measures introduced to reduce transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), such as universal masking and social distancing, may reduce community transmission of common RVIs [4], potentially decreasing the frequency and severity of asthma exacerbations and hence reducing hospitalisations. However, patients may demonstrate a higher threshold to seek care due to fear of nosocomial transmission during the pandemic. Significant community transmission of SARS-CoV-2 may thus confound causal interpretation of trends in asthma hospitalisations. While the ongoing pandemic provides a rare opportunity to ascertain the impact of public health measures on hospitalisations for asthma exacerbations, such observations are only possible in areas that have mitigated community transmission and maintained public health interventions over a sustained duration.
Short abstract
A sustained reduction in asthma admissions with PCR-proven respiratory viral infections coincided with the widespread adoption of public health measures, including social distancing and wearing of face coverings, during a pandemic https://bit.ly/2Kug9iw
To the Editor:
We read with interest the study by Izquierdo et al. [1] that reported a lower proportion of patients with concurrent asthma and coronavirus disease 2019 (COVID-19), compared to other chronic diseases. During the ongoing pandemic, various studies have also observed a lower occurrence of persons with asthma amongst hospitalised COVID-19 cases [2, 3]. Several hypotheses have been postulated to account for these observations, including lower susceptibility to COVID-19 amongst patients with asthma [2, 3] and a remission in rates of common circulating respiratory viral infections (RVIs) [4]. RVIs are potential triggers of asthma exacerbations and may cause a loss of asthma control [5]. During the COVID-19 pandemic, community-wide public health measures introduced to reduce transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), such as universal masking and social distancing, may reduce community transmission of common RVIs [4], potentially decreasing the frequency and severity of asthma exacerbations and hence reducing hospitalisations. However, patients may demonstrate a higher threshold to seek care due to fear of nosocomial transmission during the pandemic. Significant community transmission of SARS-CoV-2 may thus confound causal interpretation of trends in asthma hospitalisations. While the ongoing pandemic provides a rare opportunity to ascertain the impact of public health measures on hospitalisations for asthma exacerbations, such observations are only possible in areas that have mitigated community transmission and maintained public health interventions over a sustained duration.
In Singapore, a Southeast-Asian city state, various public health interventions were implemented community-wide from February 2020. A surge of COVID-19 cases amongst migrant workers in April 2020 triggered a 7-week public lockdown, with public mask-wearing being made mandatory [4]. However, the majority of COVID-19 cases remained confined to the migrant worker population staying in designated dormitories, with limited transmission in the wider community. Lockdown measures were lifted on 2 June 2020, with progressive relaxation of social distancing. However, compulsory mask-wearing in public places has been maintained [4]. At the largest tertiary hospital in Singapore, comprehensive infection prevention measures prevented patient–staff transmission of SARS-CoV-2 [6], allowing admissions to continue as usual. We evaluated trends in asthma admissions with concomitant RVIs over an unbroken 10-month period during the pandemic.
From January 2018 to November 2020, information on all admissions with a diagnosis of acute asthma exacerbation was extracted from our institution's electronic database. Inclusion criteria included a discharge diagnosis of acute asthma exacerbation according to appropriate ICD codes. Asthma admissions that had a PCR-proven RVI in the same admission were then identified. Pre-pandemic, patients with asthma and concurrent symptoms of upper respiratory tract infection (URTI) had samples tested for common RVIs via multiplex PCR, at the physician's discretion. During the pandemic, all inpatients with URTI symptoms were additionally tested for SARS-CoV-2 as well as common RVIs [6]. The rates of asthma admissions with PCR-proven RVI pre- and post-pandemic were compared using the incidence rate ratio method.
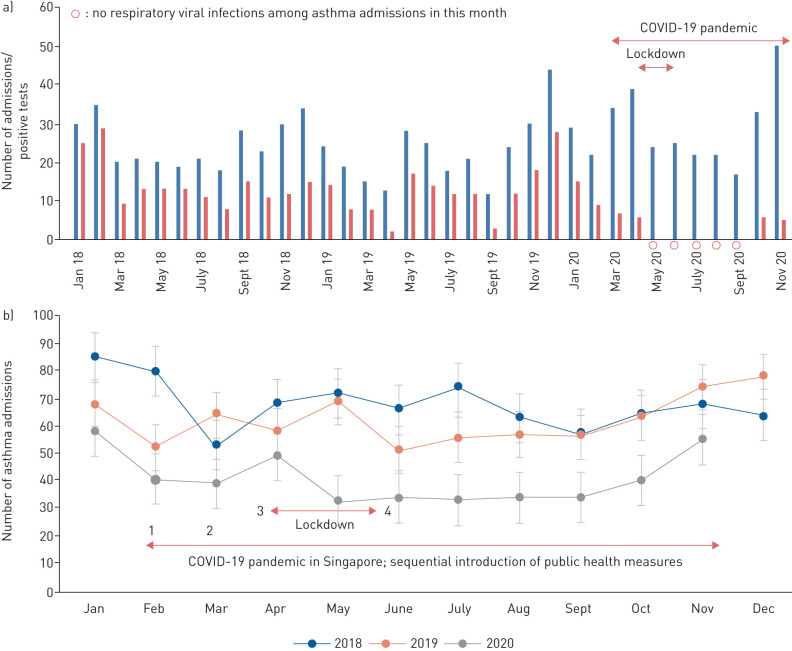
Our results showed a significant and sustained reduction in asthma admissions with concomitant reduction in RVIs during the pandemic (figure 1a). The incidence rate of PCR-proven RVI was 84.2 cases per 1000 asthma admissions during the pandemic, compared with 212.6 cases per 1000 asthma admissions pre-pandemic; the decline was statistically significant (incidence rate ratio 0.39, 95% CI 0.27–0.57; p<0.001). The total number of asthma admissions per month dropped from a mean±sd of 64.7±9.1 pre-pandemic to 39.2±7.5 admissions per month during the pandemic (p<0.001) (figure 1b). During the pandemic, only 11.5% (33/288) of asthma admissions had a concurrent PCR-proven RVI, while one-half (53.5%, 348/651) of asthma admissions had a positive result pre-pandemic (OR 0.11, 95% CI 0.08–0.17; p<0.001). This decline was noted despite increased sampling, likely due to heightened vigilance for respiratory symptoms during the pandemic. During the pandemic, close to three-quarters (73.5%, 288/392) of asthma admissions were tested for RVIs, while pre-pandemic, around two-fifths (39.7%, 651/1637) of asthma admissions were tested for RVIs (OR 4.19, 95% CI 3.28–5.35; p<0.001). Notably, over a 5-month period from May to September 2020 onwards, zero asthma admissions had concomitant RVIs. This observation was unprecedented in the preceding 2 years.
FIGURE 1.
Admissions for asthma with concurrent respiratory viral infections at a tertiary hospital in Singapore (January 2018 to November 2020). a) Number of asthma admissions tested for respiratory viruses, and number that tested positive, at the Singapore General Hospital (January 2018 to November 2020). The routine panel for respiratory virus testing included testing for influenza A, influenza B, respiratory syncytial virus, rhinoviruses, parainfluenza virus types 1–4, human metapneumovirus, coronaviruses and adenoviruses. b) All asthma admissions at the Singapore General Hospital (January 2018 to November 2020). 1) First reported case of coronavirus disease 2019 (COVID-19) in Singapore on 23 January 2020. Nationwide emphasis on hand and respiratory hygiene. 2) 24 March 2020: social distancing measures limiting gatherings outside of work and school to a maximum of 10 people; closure of large public venues (e.g. religious places and entertainment venues). 3) 7 April 2020 to 2 June 2020: nationwide lockdown. All non-essential workplaces and schools closed. Wearing of face coverings in public made compulsory from 14 April 2020 onwards. 4) 2 June 2020 onwards: lockdown lifted; continued emphasis on hand hygiene; compulsory wearing of face coverings in public; gatherings of up to five people allowed outside of work and school.
A sustained reduction in asthma admissions with PCR-proven RVIs coincided with the widespread adoption of public health measures during a pandemic. While a reduction in admissions could also be driven by diversion of patients away from hospitals designated for COVID-19 care, our institution was not designated as the national centre for handling COVID-19 cases and services continued as usual. Additionally, there was no significant increase in the number of admissions with concomitant RVIs at our institution requiring intensive care [7], suggesting no corresponding rise in case severity associated with delayed presentation. While outdoor air pollution in Singapore also significantly decreased during the lockdown period due to movement restrictions [8], the reduction in asthma admissions was sustained for more than 6 months after the lifting of lockdown. The trends seen for asthma admissions mirrored observations for other chronic diseases, including COPD and heart failure [9, 10]. While the single-centre nature of our study potentially restricts the generalisability of our observations, the complementary role of simple preventive measures such as wearing of face coverings, hand hygiene and social distancing in mitigating asthma exacerbations deserves further evaluation and investigation.
Shareable PDF
Footnotes
Author contributions: Concept and design: Liang En Wee, Indumathi Venkatachalam. Analysis of data: Liang En Wee, Edwin Philip Conceicao, Indumathi Venkatachalam. Drafting of manuscript: Liang En Wee, Edwin Philip Conceicao, Jing Yuan Tan, Jean Xiang Ying Sim, Indumathi Venkatachalam. Supervision: Indumathi Venkatachalam.
Conflict of interest: L.E. Wee has nothing to disclose.
Conflict of interest: E.P. Conceicao has nothing to disclose.
Conflict of interest: J.Y. Tan has nothing to disclose.
Conflict of interest: J.X.Y. Sim has nothing to disclose.
Conflict of interest: I. Venkatachalam has nothing to disclose.
References
- 1.Izquierdo JL, Almonacid C, González Y, et al. . The impact of COVID-19 on patients with asthma. Eur Respir J 2021; 57: 2003142. doi: 10.1183/13993003.03142-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carli G, Cecchi L, Stebbing J, et al. . Is asthma protective against COVID-19? Allergy 2021; 76: 866–868. doi: 10.1111/all.14426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Assaf SM, Tarasevych SP, Diamant Z, et al. . Asthma and severe acute respiratory syndrome coronavirus 2019: current evidence and knowledge gaps. Curr Opin Pulm Med 2021; 27: 45–53. doi: 10.1097/MCP.0000000000000744 [DOI] [PubMed] [Google Scholar]
- 4.Tan JY, Conceicao EP, Sim XYJ, et al. . Public health measures during COVID-19 pandemic reduced hospital admissions for community respiratory viral infections. J Hosp Infect 2020; 106: 387–389. doi: 10.1016/j.jhin.2020.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Britto CJ, Brady V, Lee S, et al. . Respiratory viral infections in chronic lung diseases. Clin Chest Med 2017; 38: 87–96. doi: 10.1016/j.ccm.2016.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wee LE, Venkatachalam I, Sim XY, et al. . Containment of COVID-19 and reduction in healthcare-associated respiratory viral infections through a multi-tiered infection control strategy. Infect Dis Health 2020; in press [ 10.1016/j.idh.2020.11.004]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wee LE, Ko KKK, Ho WQ, et al. . Community-acquired viral respiratory infections amongst hospitalized inpatients during a COVID-19 outbreak in Singapore: co-infection and clinical outcomes. J Clin Virol 2020; 128: 104436. doi: 10.1016/j.jcv.2020.104436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li JY, Tartarini F. Changes in air quality during the COVID-19 lockdown in Singapore and associations with human mobility trends. Aerosol Air Qual Res 2020; 20: 1748–1758. doi: 10.4209/aaqr.2020.06.0303 [DOI] [Google Scholar]
- 9.Tan JY, Conceicao EP, Wee LE, et al. . COVID-19 public health measures: a reduction in hospital admissions for COPD exacerbations. Thorax 2020; in press [ 10.1136/thoraxjnl-2020-216083]. doi: 10.1136/thoraxjnl-2020-216083 [DOI] [PubMed] [Google Scholar]
- 10.Wee LE, Conceicao EP, Tan JY, et al. . Reduction in heart failure admissions with concomitant respiratory viral infections during the novel coronavirus disease-2019 pandemic: unintended consequence of public health measures in Singapore. J Card Fail 2021; 27: 117–119. doi: 10.1016/j.cardfail.2020.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This one-page PDF can be shared freely online.
Shareable PDF ERJ-04493-2020.Shareable (322.1KB, pdf)