Abstract
Aims:
We evaluated survivorship, outcomes, and failures of an interlocking, reconstruction mode stem-sideplate implant used to preserve the native hip joint and achieve proximal fixation when there is little residual femur during large endoprosthetic reconstruction of the distal femur.
Patients and Methods:
Fourteen patients underwent primary or revision reconstruction of a large femoral defect with a short remaining proximal femur using an interlocking, reconstruction mode stem-sideplate for fixation after oncologic distal femoral and diaphyseal resections. None of these were amenable to standard cemented or uncemented stem fixation. Patient and disease characteristics, surgical history, final ambulatory status, and Musculoskeletal Tumor Society (MSTS) score were recorded. The percentage of proximal femur remaining was calculated from follow-up radiographs.
Results:
All 14 at-risk native hip joints were preserved at final follow-up of 4.7 years +/− 3.3 years, despite a short residual femur, often after proximal osteotomies through the lesser trochanter. Thirteen of 14 stems had long term successful fixation. Eight patients required no reoperation. Three patients required reoperation due to implant-related issues, and three patients required reoperation for wound healing problems or infection. There were no dislocations or fractures. Nine patients required no ambulation aids, and only one had a Trendelenburg gait.
Conclusion:
This interlocking, reconstruction mode stem-sideplate reliably preserves native hip joint anatomy and function after large femoral resection with a short remaining proximal femur, both in the primary and revision setting. This is particularly important for preventing or delaying total femoral replacement in young patients after oncologic reconstruction. Hip abductor strength and function could be maintained by this method, and the risk of dislocation eliminated. The success of the method in this modest series should be verified in a larger collaborative study and will be of interest to revision surgeons as well as oncologists.
Keywords: distal femoral replacement, total femoral replacement, custom implant, stem-sideplate, reconstruction screw fixation, megaprosthesis
INTRODUCTION
Large resections of the femur for skeletal tumours can leave short proximal segments adjacent to the hip, limiting proximal fixation of an implant, increasing the risk of dislocation and compromising abductor function if it cannot be preserved. This difficult situation can also be encountered in the setting of revision surgery, where bone loss from previous reconstructions leaves little proximal femur left for fixation. Several reconstructive options have been explored, each with their unique drawbacks. Short conventional stems leave relatively little fixation surface to counteract large lever-arm and rotational forces, likely leading to higher rates of aseptic loosening.1 Allograft-prosthetic composite (APC) reconstructions restore diaphyseal bone stock and facilitate the use of longer stems, but have a nonunion rate requiring further surgery that can approach 30%.2 When there is at least 5 cm of residual femur, the telescope method to intussuscept and overlap allografts can restore femoral diaphyseal bone stock and allow durable cemented fixation.3 Novel implants such as Compress ® (Biomet-Zimmer, Warsaw, IN, USA) can be used when there is 4–8 cm of residual subtrochanteric bone, but there are no reports documenting success rates when there is limited proximal fixation. Replacement of the entire femur is probably the most facile solution for the surgeon, but has a high infection rate and only fair functional restoration.4–6 Finally, custom implants have been used in this scenario, with varying degrees of success.7–9
Custom prostheses have been used in this clinical scenario for decades. Many of these designs evolved from the Stanmore bifid or “rhino” prostheses, which had a curved stem extending into the femoral neck, and was cemented.10 Kotz demonstrated the usefulness of a sideplate for rotational stability, as well as the ability of cementless stems to achieve durable fixation, predominantly in the tibia and distal femur.11 The helpful addition of cross-pin fixation to improve rotational stability was demonstrated by Cannon and again by Bernthal, but these stems were still cemented.9, 12 The stem used in the current study incorporates the best attributes of each of the previous designs, which include: an attached sideplate, screw fixation capturing the sideplate and stem in a “reconstruction” mode, a rectangular stem cross-section to resist rotational forces, a taper junction that attaches to a standard modular endoprosthetic system, and a porous ingrowth surface, which is probably the best long-term fixation strategy for young patients.13, 14 Here, we present the clinical indications, mid-term survivorship, clinical outcomes, and reasons for reoperations of this stem-sideplate implant designed for short proximal femoral segments.
PATIENTS, MATERIALS, AND METHODS
Implant Design and Technique
The interlocking reconstruction-mode, stem-sideplates were individually designed using CT data. They contained the common characteristics of an intramedullary stem, a collar, an extramedullary plate, slots or holes to accommodate interlocking screws, and a modular taper (Figure 1). The intramedullary stem is a titanium-6 aluminum-4 vanadium substrate with plasma-sprayed titanium porous coating for biologic fixation. A corresponding custom manufactured rasp measuring 0.75 mm less than the porous-coated stem (Figure 2) was used to prepare the medullary canal in the intertrochanteric space and base of the femoral neck.
Figure 1:
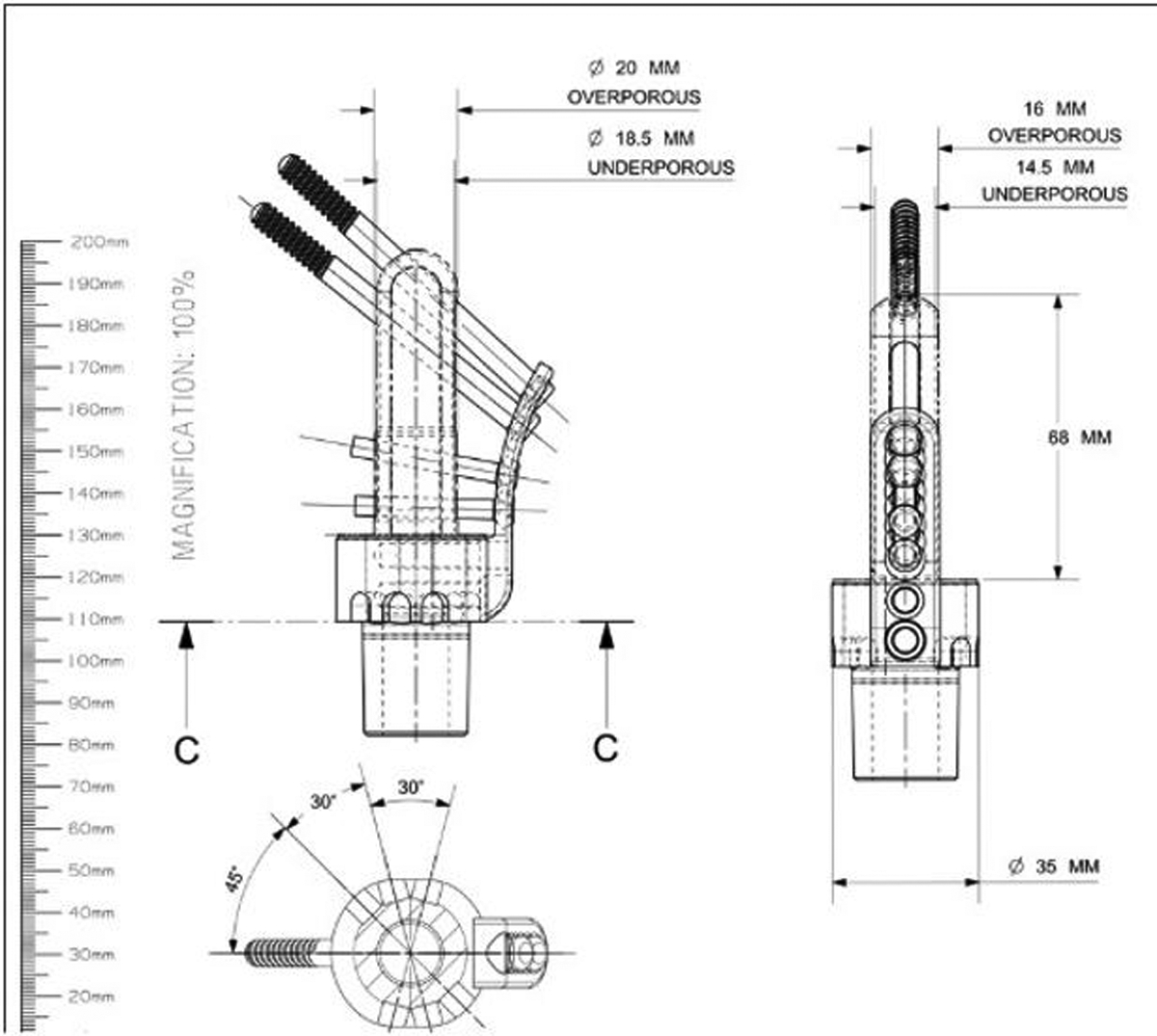
Diagram of custom stem-sideplate prosthesis including important features.
Figure 2:

Photograph of the custom stem-sideplate prosthesis with “reconstruction” screw aiming guide.
The collar is sized to be slightly larger than the extra-cortical diameter of the bone at the planned resection level. Stem collars are at least 2 cm thick to accommodate two transversely aligned threaded holes to which the extramedullary plate screws in. This modular extramedullary plate follows the contour of the bony anatomy of the proximal femur or greater trochanter. The adjustable attachment of the extramedullary plate facilitates insertion, avoids passively misdirecting the stem during insertion, and is secured by compression screws after final impaction of the implant. Porous coating is applied to the side of the plate facing bone. The plate is thick enough to provide adequate rigidity to the construct, yet thin enough that hand held plate benders can be used to make final geometric adjustments, and conform to the bone when compression screws are applied. Spacer shims, which can be placed between the stem and plate, are also provided so that the distance from stem centerline to plate may be adjusted intraoperatively.
The intramedullary stem and extramedullary plate are manufactured to accommodate oblique interlocking screws oriented in “reconstruction” mode based on the femoral neck anteversion and varus-valgus alignment of the neck shaft angle based on preop CT measurements. The screws were leveraged from a commercially available trauma nail system (Figure 3). Hole diameters and slot widths were chosen in accordance with the quantity and quality of bone available for screw purchase and the availability of standard screws. Hole and slot dimensions were chosen in proportion to the stem diameter to avoid unacceptable weakening of the critical stem cross-sections.
Figure 3:
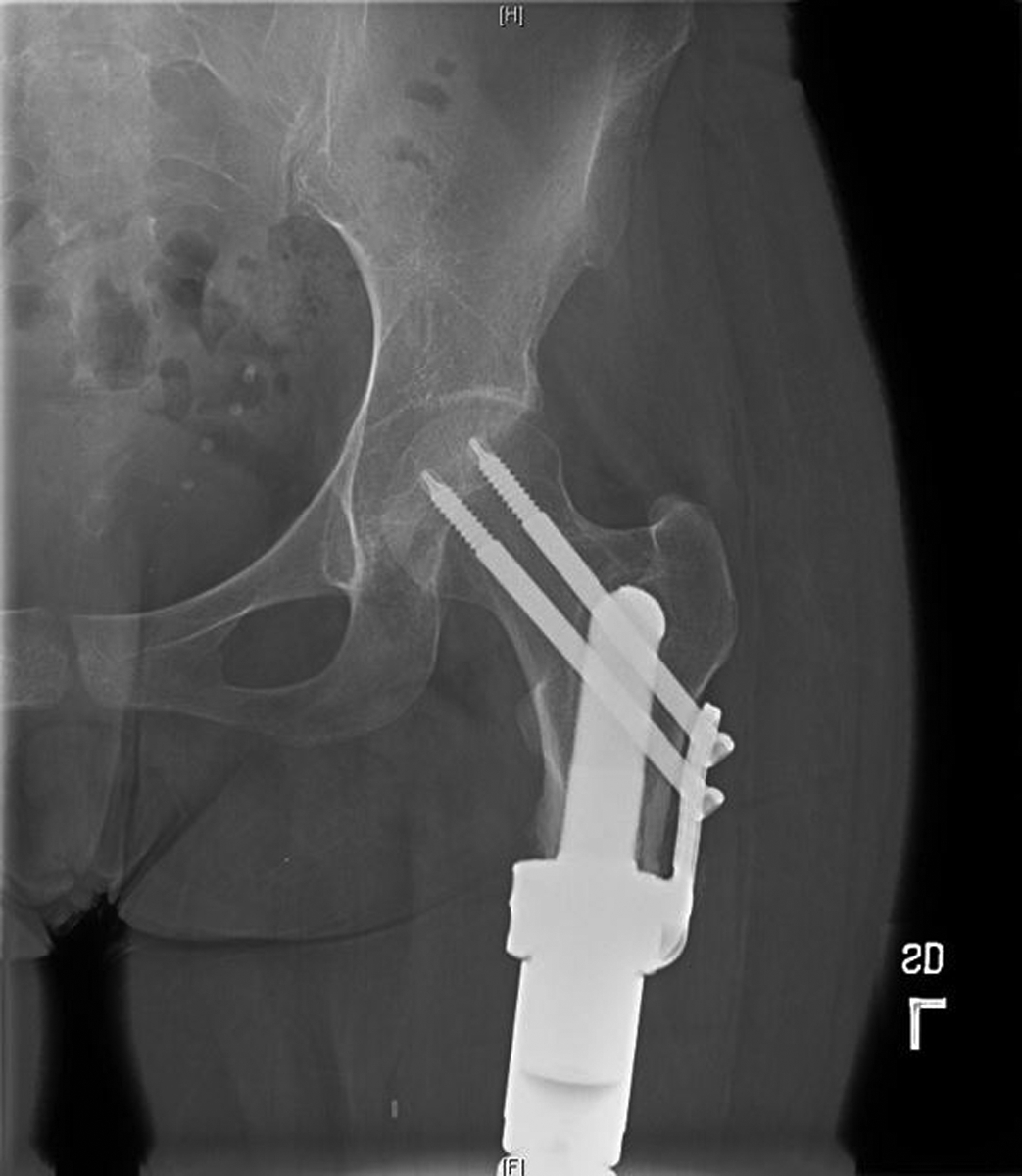
Post-operative anteroposterior radiograph of a primary implantation of a custom stem-sideplate prosthesis with interlocking “reconstruction” mode screws coupled to a modular distal femoral replacement.
The custom implants include a modular taper junction for connection to an appropriate commercially available modular segmental replacement system to recreate limb length. Most commonly, these custom stems are used with a segmental distal femoral rotating hinged knee, but can also be used with an intercalary device after diaphyseal tumour resection.
Patients
Fourteen patients from 2002 to 2018 had interlocking reconstruction-mode stem-sideplates custom-manufactured. and 13 of 14 were implanted by the senior author (JHH. Approval for this study was granted by the Institutional Review Board (IRB 16–1123). Follow-up was performed at the same institution. Patient and surgical data was retrospectively reviewed from the medical record. The rationale to select this reconstruction could not be determined retrospectively for each patient. However, during this time frame, the alternative procedures were rarely done. Total femur replacement was only done if there was proximal tumour extension into the intertrochanteric area, (N = 2) radiotherapy was planned that could interfere with osteointegration into the porous prosthesis (N = 2), or there was significant pre-existing hip arthritis (N = 1). Primary rotationplasty was reserved for patients less than 12 years old with substantial remaining growth potential, and there were no salvage rotationplasties done in this epoch. All other patients received this implant when there was a 6 week interval available for the design and manufacture of the prosthesis. Demographics, date of surgery and final follow-up, oncologic indication, secondary indication for revision surgery, previous surgeries, subsequent surgeries, and radiographic outcomes were recorded. The primary outcome measures were of hip preservation and prosthetic retention. Failures were classified according to the Henderson Failure Mode Classification.15 Secondary outcome measures included function analyzed by clinical appearance of gait at final follow-up, the use of ambulatory assistive devices, and the Musculoskeletal Tumor Society (MSTS) system that also captured these critical features.16
Variables and Statistical Analysis
The primary outcome of this study was hip preservation and prosthesis survival. Patient age at the time of surgery and final follow-up, percentage of femur remaining, and reoperations were analyzed using descriptive statistics. Means, standard deviations (SD), and descriptive statistics were carried out using Microsoft Excel software (Microsoft, Redmond, Washington).
Individual patient characteristics are listed (Table 1). Mean age was 36 ± 14 years and mean follow up was 4.7 ± 3.3 years. There were 9 men and 5 women. Four patients had the custom implant placed during primary surgery for sarcoma resection (Figure 3). The custom implant was used during revision surgery in the other 10 patients (Figure 4). Patients who underwent revision with this implant had mean 3.6 (range 1–11) previous operations. Oncologic diagnoses included osteogenic sarcoma (10), Ewing sarcoma (2), pleomorphic sarcoma (1), and giant cell tumour of bone (1). Secondary diagnoses that necessitated revision reconstructive surgery included infection (3), aseptic loosening of a previous implant (7), and periprosthetic fracture (1). Ten custom implants were part of a distal femoral replacement; four were included as part of an intercalary prosthesis. The short proximal femur remaining was 24% (SD 1.5%) and 8 of 14 retained ≤ 20% of their femur.
Table 1:
Patient Demographics and Characteristics
| Age (years) | 36 ± 14 |
| Follow-up (years) | 4.7 ± 3.3 |
| Periprosthetic Fracture | 1* |
| Intercalary replacement | 4 |
| Previous surgeries (range) | 3.6 (0 – 11) |
| Chemotherapy | 12 |
| Radiotherapy | 1 |
= single patient who sustained both events
Figure 4.




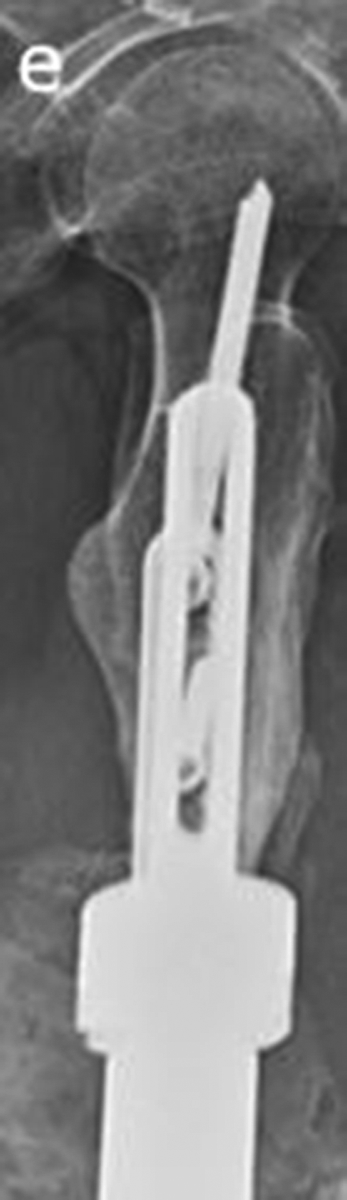
Secondary reconstruction of a failed, infected distal femoral replacement after osteosarcoma. a. Antero-posterior radiograph shows a pin-cement spacer and malalignment of the short proximal femoral segment. b. Lateral radiograph shows drastic malalignment of the short segment and the spacer. c. Oblique radiograph shows the distal femoral spacer. d. Antero-posterior radiograph shows stable fixation of the stem-side plate 10 years and 7 months after reconstruction. e. Lateral radiograph shows stable fixation 10 years and 7 months after reconstruction.
RESULTS
The interlocking reconstruction mode, stem-sideplate design was clinically and radiographically successful. At final follow-up, all patients maintained their native hip joint. 13 of 14 stems were retained with durable fixation. One patient had early aseptic loosening and was revised with an analogous uncemented implant. One construct required revision of a broken screw and achieved long term stable fixation of the original stem. Nine patients required no ambulation aid, 3 required a cane, and 2 required one crutch. Only one patient had a noticeable Trendelenburg gait. The mean MSTS score was 24 (range 16–30). The patient with an MSTS score of 16 had the custom implant placed after treatment for chronic periprosthetic infection and an absent quadriceps. This individual experienced reinfection and underwent 11 subsequent operations with retention of their implant and suppressive therapy for their infection. All other patients had an MSTS score >20 with a mean of 24.6.
Eight patients required no reoperation. The 6 patients who required further surgery averaged 1.4 ± 2.8 additional procedures. Failures are categorized according to Henderson et al. (Table 2).15 The patient with infection and 11 subsequent operations experienced a dislocation of the non-articulated rotating hinge knee replacement, requiring knee, but not hip revision surgery. This was the only Type 1 (soft tissue) failure. There were two Type 2 (aseptic loosening) events described above. One was rapid after implantation by a surgeon inexperienced with the implant, and was salvaged with revision using an analogous implant. The second patient had the implant salvaged by revision of the interlocking screw fixation and retention of the stem. Two patients experienced Type 3 (structural) failures of their implant – consisting of fractures of the taper at the modular junction between the custom stem and the rest of the modular prosthesis. Both were successfully revised with retention of the custom stem-sideplate. No patient required revision of his or her custom prosthesis for Type IV (infection) or Type IV (tumour progression) failure.
Table 2:
Reoperation and Revision Classified According to Henderson el al.15
| Reoperations | Patients | Stem Revisions | |
|---|---|---|---|
| Type 3 (structural failure) | 2 | 2 | 0 |
| Type 4 (infection) | 6 | 1 | 0 |
| Type 5 (tumour progression) | 0 | 0 | 0 |
There were additional surgical complications not related to the interlocking reconstruction-mode stem-sideplates. One patient had an unplanned leg-length discrepancies of 2-cm Another had a planned discrepancy and lengthening procedure. One patient required revision surgery for aseptic loosening of their tibial component. Finally, one patient require reoperation to drain a hematoma.
DISCUSSION
The problem of fixation of a megaprosthesis in a short proximal femoral segment in musculoskeletal tumour surgery is not new, and the techniques and prostheses used to address this problem have evolved over time. Our cohort demonstrated that this interlocking reconstruction-mode, stem-side plate was feasible and very effective in achieving fixation in short residual proximal femoral segments despite demonstrating common complications associated with all megaprosthetic surgery. All hips at risk were retained, avoiding total femur replacement and its corresponding functional consequences of weakness, limp, and instability. There were two cases of fracture at the modular taper junction, which implies that fixation at the stem-bone interface was so secure that forces were then transferred to the taper junction. There were no periprosthetic fractures. This is the result of strong initial fixation, optimization of the stem position, and stabilization of the entire remaining short femoral segment.17 The only case requiring revision for early loss of fixation reasons was performed by a surgeon inexperienced with the implant and was successfully revised using the same implant. Plain radiographs showed persistence of the bone stock and no stress bypass effect during this early to mid follow-up time frame, concerning consequences that developed in interlocking screw and side plate constructs of the distal femur and proximal tibia.18 The interlocking reconstruction-mode stem-sideplates preserved at-risk hips with short residual proximal femoral segments.
Historically several surgeons used the rhino prosthesis, which was a cemented horn-shaped proximal femur stem that curved into the femoral neck. These initially performed well, but eventually loosened or fractured the neck of the femur).10 In general, custom cemented distal femur replacements experienced a high rate of aseptic loosening, and different strategies were explored to mitigate this mode of failure.19 Kotz first implanted custom cementless stems with sideplates and interlocking or non-interlocking screw fixation in 1975.18 This concept was then developed into a comprehensive 26-piece system in 1982, and outcomes on 52 patients were published in 1986.7, 11 Subsequent reports demonstrated improved aseptic loosening rates compared to cemented implants.20–22 However, these implants had profound stress bypass effects and mechanical complication rates of 5%–12%, and have been replaced by more modern segmental systems.20, 21, 23 However, extra-cortical plate attachment has been relegated to use in individualized implant designs.24
Custom cross-pin fixation with cemented prosthesis, but without the use of a side plate is effective in preventing aseptic loosening at mid-term follow-up, and remains durable in the long term.9, 12 However, mechanical failure and aseptic loosening still occur with those designs, as cement does not gain biologic fixation and requires smaller stems to make room for a cement mantle. Our cohort, while demonstrating common complications associated with all megaprosthetic surgery, avoids aseptic loosening if initial stability is achieved. The only case requiring revision for fixation reasons was performed by a surgeon inexperienced with the implant and was successfully revised using the same implant. There were two cases of fracture at the modular junction, which implies that fixation at the stem-bone interface was so secure that forces were then transferred to the taper junction. Finally, there were no periprosthetic fractures, which is the result of strong initial fixation and the ability to plan for ideal stem position.17
The goal of this custom implant is to preserve the at-risk hip joint and prevent loss of the abductor mechanism. Loss of abductor strength increases the energy expenditure of walking to 141% of normal.6 As a result, patients with proximal femoral replacement experience significantly lower functional outcomes.25–30 Younger patients fare worse, experiencing higher rates of aseptic loosening and instability.31 Studies have shown that sacrifice of two joints during endoprosthetic reconstruction is associated with significantly worse function than one joint. As expected, total femur replacements have even lower functional scores than distal femoral replacements.32 In primary reconstructions patients achieve reasonable functional results, but still suffer from instability, especially when the abductors cannot be effectively tied secured to the prosthesis.33–35 However, in the revision setting, complication rates are high and restoration of abductor function is poor, so the majority of patients require ambulatory aids.36–39 Therefore, especially in young oncology patients with long life expectancies, it is imperative to preserve the hip joint and abductor attachments, both for function and to decrease the number of future complications and operations.
This study has several limitations inherent to the population being studied. It is a small case series, there was no control group, and it could not be determined retrospectively it could not be determined retrospectively why this approach was selected. However, during this time frame, alternative procedures were rarely done and this procedure progressively replaced the previously popular alternatives at our institution, the telescoped alloprosthetic replacement and the short fixation Compress® replacement due to the senior author’s subjective sense that it was more effective and dependable. Total femur replacement was only done if there was proximal extension into the intertrochanteric area, radiotherapy was planned that could interfere with osteointegration into the porous prosthesis, or there was significant pre-existing hip arthritis. Rotationplasty was reserved for patients less than 12 years old with substantial remaining growth potential. All other patients received this implant when there was a 6-week interval available for the design and manufacture of the prosthesis. These limitations are common in orthopaedic oncology due to the rarity of the diseases treated and cannot be overcome by a single center. It is not clear how easily this concept and design can be generalized to other manufacturers, institutions, or surgeons.
This custom interlocking reconstruction-mode stem-sideplate implant preserved all adjacent hip joints and abductors, and stems survived at mid-term follow-up, despite complications associated with megaprosthesis surgery that were design-independent. Although direct comparison to alternative reconstructions is impossible, the authors are not aware of published series of bone, prosthetic, or hybrid reconstructions with better results under these challenging conditions.2, 3, 12, 24, 40–42 Most importantly, functional outcomes are at least as good as those published to those offered by primary and revision total femur replacement.5, 34, 36–39, 43 This study demonstrates the mid-term success of this cementless custom interlocking reconstruction-mode stem-sideplate implant for fixation in a short proximal femur segment, with two patients’ implants having greater than 10 year survivorship. Only one patient had a noticeable limp at final follow-up, and 9/14 required no ambulatory aid. This option is compelling if the goal is to save a short residual proximal femur for fixation of a distal femoral reconstruction. The success of the method in this modest series should be verified in a larger collaborative study, and the relative merits of this implant can only be proven by direct comparison with alternative strategies. The results will be of interest to revision surgeons as well as oncologists.
TAKE HOME MESSAGE.
The interlocking stem-sideplate construct successfully preserves hip anatomy and function the limitations of short residual proximal femoral segments in primary or revision reconstructions.
Funding:
This research was funded in part through the NIH/NCI Cancer Center Support Grant, P30 CA008748, The OMeGA Medical Grants Association, and The Perlman Research Fund.
Ethical Review Committee Statement: Approval for this study was granted by the Institutional Review Board (IRB# 16-1123).
Footnotes
Conflict of Interest: None declared.
REFERENCES
- 1.Jeon DG, Kawai A, Boland P, Healey JH. Algorithm for the surgical treatment of malignant lesions of the proximal tibia. Clin Orthop Relat Res 1999(358):15–26. [PubMed] [Google Scholar]
- 2.Moon BS, Gilbert NF, Cannon CP, Lin PP, Lewis VO. Distal Femur Allograft Prosthetic Composite Reconstruction for Short Proximal Femur Segments following Tumor Resection. Adv Orthop 2013;2013:397456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Healey JH, Abdeen A, Morris CD, Athanasian EA, Boland PJ. Telescope allograft method to reconstitute the diaphysis in limb salvage surgery. Clin Orthop Relat Res 2009;467(7):1813–1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramanathan D, Siqueira MB, Klika AK, Higuera CA, Barsoum WK, Joyce MJ. Current concepts in total femoral replacement. World J Orthop 2015;6(11):919–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medellin MR, Fujiwara T, Clark R, Stevenson JD, Parry M, Jeys L. Mechanisms of failure and survival of total femoral endoprosthetic replacements. Bone Joint J 2019;101-b(5):522–528. [DOI] [PubMed] [Google Scholar]
- 6.Kawai A, Backus SI, Otis JC, Inoue H, Healey JH. Gait characteristics of patients after proximal femoral replacement for malignant bone tumour. J Bone Joint Surg Br 2000;82(5):666–669. [DOI] [PubMed] [Google Scholar]
- 7.Kotz RI. Progress in musculoskeletal oncology from 1922 – 2012. Int Orthop 2014;38(5):1113–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal M, Puri A, Gulia A, Reddy K. Joint-sparing or physeal-sparing diaphyseal resections: the challenge of holding small fragments. Clin Orthop Relat Res 2010;468(11):2924–2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cannon CP, Eckardt JJ, Kabo JM, Ward WG Sr., Kelly CM, Wirganowicz PZ, et al. Custom cross-pin fixation of 32 tumor endoprostheses stems. Clin Orthop Relat Res 2003(417):285–292. [DOI] [PubMed] [Google Scholar]
- 10.Grimer RJ, Carter SR, Sneath RS, Unwin P, Walker PS, editor Fixation of Implants in Short Segments of Femur. Limb Salvage: Current Trends. International Society of Limb Salvage; 1993; Singapore. [Google Scholar]
- 11.Kotz R, Ritschl P, Trachtenbrodt J. A modular femur-tibia reconstruction system. Orthopedics 1986;9(12):1639–1652. [DOI] [PubMed] [Google Scholar]
- 12.Bernthal NM, Upfill-Brown A, Burke ZDC, Ishmael CR, Hsiue P, Hori K, et al. Long-term follow-up of custom cross-pin fixation of 56 tumour endoprosthesis stems: a single-institution experience. Bone Joint J 2019;101-b(6):724–731. [DOI] [PubMed] [Google Scholar]
- 13.Bruns J, Delling G, Gruber H, Lohmann CH, Habermann CR. Cementless fixation of megaprostheses using a conical fluted stem in the treatment of bone tumours. J Bone Joint Surg Br 2007;89(8):1084–1087. [DOI] [PubMed] [Google Scholar]
- 14.Hu CC, Chen SY, Chen CC, Chang YH, Ueng SW, Shih HN. Superior Survivorship of Cementless vs Cemented Diaphyseal Fixed Modular Rotating-Hinged Knee Megaprosthesis at 7 Years’ Follow-Up. J Arthroplasty 2017;32(6):1940–1945. [DOI] [PubMed] [Google Scholar]
- 15.Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am 2011;93(5):418–429. [DOI] [PubMed] [Google Scholar]
- 16.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993(286):241–246. [PubMed] [Google Scholar]
- 17.Orlic D, Smerdelj M, Kolundzic R, Bergovec M. Lower limb salvage surgery: modular endoprosthesis in bone tumour treatment. Int Orthop 2006;30(6):458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kotz R The History of Bone Tumour Treatment and the State of the Art in Vienna. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2017;38(3):31–38. [DOI] [PubMed] [Google Scholar]
- 19.Unwin PS, Cannon SR, Grimer RJ, Kemp HB, Sneath RS, Walker PS. Aseptic loosening in cemented custom-made prosthetic replacements for bone tumours of the lower limb. J Bone Joint Surg Br 1996;78(1):5–13. [PubMed] [Google Scholar]
- 20.Griffin AM, Parsons JA, Davis AM, Bell RS, Wunder JS. Uncemented tumor endoprostheses at the knee: root causes of failure. Clin Orthop Relat Res 2005;438:71–79. [DOI] [PubMed] [Google Scholar]
- 21.Ritschl P, Capanna R, Helwig U, Campanacci M, Kotz R. [KMFTR (Kotz Modular Femur Tibia Reconstruction System) modular tumor endoprosthesis system for the lower extremity]. Z Orthop Ihre Grenzgeb 1992;130(4):290–293. [DOI] [PubMed] [Google Scholar]
- 22.Mittermayer F, Windhager R, Dominkus M, Krepler P, Schwameis E, Sluga M, et al. Revision of the Kotz type of tumour endoprosthesis for the lower limb. J Bone Joint Surg Br 2002;84(3):401–406. [DOI] [PubMed] [Google Scholar]
- 23.Hauer TM, Houdek MT, Bhumbra R, Griffin AM, Wunder JS, Ferguson PC. Component Fracture in the Kotz Modular Femoral Tibial Reconstruction System: An Under-Reported Complication. J Arthroplasty 2018;33(2):544–547. [DOI] [PubMed] [Google Scholar]
- 24.Stevenson JD, Wigley C, Burton H, Ghezelayagh S, Morris G, Evans S, et al. Minimising aseptic loosening in extreme bone resections: custom-made tumour endoprostheses with short medullary stems and extra-cortical plates. Bone Joint J 2017;99-b(12):1689–1695. [DOI] [PubMed] [Google Scholar]
- 25.De Martino I, D’Apolito R, Nocon AA, Sculco TP, Sculco PK, Bostrom MP. Proximal femoral replacement in non-oncologic patients undergoing revision total hip arthroplasty. Int Orthop 2019;43(10):2227–2233. [DOI] [PubMed] [Google Scholar]
- 26.Sewell MD, Hanna SA, Carrington RW, Pollock RC, Skinner JA, Cannon SR, et al. Modular proximal femoral replacement in salvage hip surgery for non-neoplastic conditions. Acta Orthop Belg 2010;76(4):493–502. [PubMed] [Google Scholar]
- 27.Viste A, Perry KI, Taunton MJ, Hanssen AD, Abdel MP. Proximal femoral replacement in contemporary revision total hip arthroplasty for severe femoral bone loss: a review of outcomes. Bone Joint J 2017;99-b(3):325–329. [DOI] [PubMed] [Google Scholar]
- 28.Parvizi J, Tarity TD, Slenker N, Wade F, Trappler R, Hozack WJ, et al. Proximal femoral replacement in patients with non-neoplastic conditions. J Bone Joint Surg Am 2007;89(5):1036–1043. [DOI] [PubMed] [Google Scholar]
- 29.Houdek MT, Watts CD, Wyles CC, Rose PS, Taunton MJ, Sim FH. Functional and oncologic outcome of cemented endoprosthesis for malignant proximal femoral tumors. J Surg Oncol 2016;114(4):501–506. [DOI] [PubMed] [Google Scholar]
- 30.Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu AT. Modular endoprosthetic replacement for metastatic tumours of the proximal femur. J Orthop Surg Res 2008;3:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Savvidou OD, Mavrogenis AF, Sakellariou V, Christogiannis I, Vottis C, Christodoulou M, et al. Salvage of failed total hip arthroplasty with proximal femoral replacement. Orthopedics 2014;37(10):691–698. [DOI] [PubMed] [Google Scholar]
- 32.Qu H, Guo W, Yang R, Tang X, Yan T, Li D, et al. Cortical strut bone grafting and long-stem endoprosthetic reconstruction following massive bone tumour resection in the lower limb. Bone Joint J 2015;97-b(4):544–549. [DOI] [PubMed] [Google Scholar]
- 33.Jones KB, Griffin AM, Chandrasekar CR, Biau D, Babinet A, Deheshi B, et al. Patient-oriented functional results of total femoral endoprosthetic reconstruction following oncologic resection. J Surg Oncol 2011;104(6):561–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sewell MD, Spiegelberg BG, Hanna SA, Aston WJ, Bartlett W, Blunn GW, et al. Total femoral endoprosthetic replacement following excision of bone tumours. J Bone Joint Surg Br 2009;91(11):1513–1520. [DOI] [PubMed] [Google Scholar]
- 35.Mankin HJ, Hornicek FJ, Harris M. Total femur replacement procedures in tumor treatment. Clin Orthop Relat Res 2005;438:60–64. [DOI] [PubMed] [Google Scholar]
- 36.Christ AB, Mendez L, Gausden EB, Blevins JL, Bostrom MP, Sculco PK. Outcomes and complications following non-oncologic total femoral replacement. Hip Int 2019:1120700019864867. [DOI] [PubMed] [Google Scholar]
- 37.Amanatullah DF, Trousdale RT, Hanssen AD, Lewallen DG, Taunton MJ. Non-oncologic total femoral arthroplasty: retrospective review. J Arthroplasty 2014;29(10):2013–2015. [DOI] [PubMed] [Google Scholar]
- 38.Friesecke C, Plutat J, Block A. Revision arthroplasty with use of a total femur prosthesis. J Bone Joint Surg Am 2005;87(12):2693–2701. [DOI] [PubMed] [Google Scholar]
- 39.Berend KR, Lombardi AV Jr., Mallory TH, Adams JB, Dodds KL. Total femoral arthroplasty for salvage of end-stage prosthetic disease. Clin Orthop Relat Res 2004(427):162–170. [DOI] [PubMed] [Google Scholar]
- 40.Calvert GT, Cummings JE, Bowles AJ, Jones KB, Wurtz LD, Randall RL. A dual-center review of compressive osseointegration for fixation of massive endoprosthetics: 2- to 9-year followup. Clin Orthop Relat Res 2014;472(3):822–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dieckmann R, Henrichs MP, Gosheger G, Holl S, Hardes J, Streitburger A. Short-stem reconstruction for megaendoprostheses in case of an ultrashort proximal femur. BMC Musculoskelet Disord 2014;15:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Safir O, Kellett CF, Flint M, Backstein D, Gross AE. Revision of the deficient proximal femur with a proximal femoral allograft. Clin Orthop Relat Res 2009;467(1):206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fountain JR, Dalby-Ball J, Carroll FA, Stockley I. The use of total femoral arthroplasty as a limb salvage procedure: the Sheffield experience. J Arthroplasty 2007;22(5):663–669. [DOI] [PubMed] [Google Scholar]


