The cluster of viral pneumonia cases that first began in Wuhan, Hubei province, China, in December 2019 has rapidly spread within China and globally. The virus responsible was subsequently identified on 7 January 2020 and the infection was given the official name of coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) on 11 February 2020. The first imported case of COVID-19 infection in Singapore was reported on 23 January 2020, the day on which all forms of travel into and out of Wuhan city were prohibited. As of 21 February 2020, 77,691 COVID-19 cases and 2,362 deaths had been reported worldwide. This skyrocketed to 617,548 cases as of 28 February 2020, with 732 cases in Singapore.
Coronaviruses are enveloped, non-segmented, single-stranded, positive-sense RNA (ribonucleic acid) viruses that have a characteristic appearance on electron microscopy negative staining.(1) They are zoonotic pathogens that cause respiratory illnesses of varying severity.(1) The closely related severe acute respiratory syndrome-related coronavirus (SARS-CoV), which caused the outbreak of severe acute respiratory syndrome (SARS) in 2003, infected over 8,000 persons and caused 774 deaths with a case fatality rate of 9.5%.(2) Comparing SARS and COVID-19, COVID-19 has affected significantly more countries than SARS-CoV by the 77 days since disease detection, with this number projected to increase further (Fig. 1).
Fig. 1.
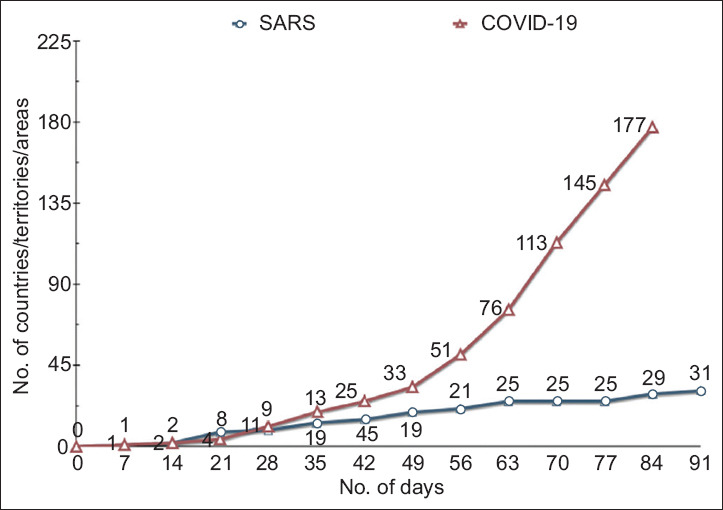
Chart shows comparison between SARS in 2003 and COVID-19 by the number of countries/territories/areas affected and days from start of outbreak (data last updated on 28 March 2020). COVID-19: coronavirus disease 2019; SARS: severe acute respiratory syndrome
In January 2020, a study by Wu et al estimated the outbreak size of COVID-19 in Wuhan at that time and the probable extent of disease spread to other cities domestically. The findings suggested that independent, self-sustaining human-to-human spread was already present in multiple major Chinese cities, many of which were global transport hubs with massive numbers of both inbound and outbound passengers (e.g. Beijing, Shanghai, Guangzhou and Shenzhen).(3) On 14 February 2020, Lipsitch et al predicted a global pandemic given that the R0 estimates were in the 2–3 range, with infection rates ranging from 40% to 90% (depending on the model adopted).(4) Until this number falls below 1.0 with containment and countermeasures implemented globally, the pandemic will continue.(4)
The past two decades have seen three major outbreaks of zoonotic coronaviruses with vastly different disease trajectories – SARS, MERS (Middle East respiratory syndrome) and COVID-19. SARS (SARS-CoV) exploded on the scene in 2002 and the outbreak was declared contained in July 2003 by the WHO. Predicted to return the following fall or winter, it never did. Its R0 was estimated to be 3. SARS-CoV, like SARS-CoV-2, is believed to have arisen from bats and transmitted to wild game markets (mammals), which led to the outbreak. Unlike SARS-CoV-2, its symptomatology was more pronounced, and the fever that was present in most cases of transmission was believed to occur predominantly after the onset of symptoms. The outbreak ceased after stringent control measures were adopted by affected countries. MERS, first recognised in June 2012 in Saudi Arabia, has led to 2,494 infections and 858 deaths in 27 countries, although cases have largely been in the Middle East. It disproportionately affects elderly men with comorbidities (e.g. diabetes mellitus) and has remained endemic because of its reservoir, the dromedary camel population. COVID-19 seemed to have started as an outbreak of pneumonia, but has now vastly outstripped SARS and MERS in terms of case counts and has exhausted multiple healthcare systems around the world.
Virus characteristics, eventual herd immunity, whether a vaccine become available, and human behaviour in this era of connectivity and globalisation will play a role in shaping the future direction of this pandemic. COVID-19 appears to be quite different from SARS and MERS, given its broader range of clinical presentation (ranging from asymptomatic and mildly symptomatic cases to severe disease, especially in older persons) and more dramatic spread.
Given what we have seen so far, the pandemic will likely continue to affect multiple countries for many months more, and more countries will be affected. If countries act fast and decisively, the curve might be ‘flattened’ – which must be done to preserve healthcare capacity and the most vulnerable among us. The experience in China has shown that it is indeed possible to contain and stop this outbreak, even if draconian measures need to be adopted and enforced, such as social distancing, widespread mask wearing (including reusable cloth masks for general use), postponement or cancellation of mass gatherings, and telework and remote-meeting options in workplaces. The public must understand that this battle cannot take place primarily on the healthcare front; if that occurs, it may perhaps be too late. The fight must also take place at the broader societal level, where strong messages for social distancing and hygiene must be sent and heeded.
Even after control is achieved, given our global connectivity, countries must be prepared for second and subsequent waves of disease brought on by relaxation of travel advisories and exacerbated by seasonal climatic factors. Chronic, endemic surges in SARS-CoV-2 transmission may continue to occur, considering that it is already present globally in human populations, indicating the need for fundamental changes in the way healthcare is delivered around the world.
SARS-CoV-2 is not another ‘common cold coronavirus’ or ‘influenza’. It is clearly able to devastate health systems and economies, in addition to the severe clinical disease it may cause in the medically vulnerable. Decisive public health measures and social responsibility are paramount even as we await scientific advancements such as effective vaccines and antivirals for COVID-19.
REFERENCES
- 1.Guarner J. Three emerging coronaviruses in two decades:the story of SARS, MERS, and now COVID-19. Am J Clin Pathol. 2020;153:420–1. doi: 10.1093/ajcp/aqaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vasoo S, Ang B, Leo YS. Chapter 11:Respiratory diseases potentially warranting care in a high-level containment unit. In: Cieslak TJ, Kortepeter MG, Kratochvil CJ, Lawler JV, editors. Nebraska Isolation and Quarantine Manual. Vol. 2019. Nebraska Medicine: University of Nebraska Medical Center; pp. 113–26. [Google Scholar]
- 3.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China:a modelling study. Lancet. 2020;395:689–97. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 - studies needed. N Engl J Med. 2020;382:1194–6. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]


