Abstract
In recent years, there has been a growing interest in identifying and applying new, naturally occurring molecules that promote health. Probiotics are defined as “live microorganisms which, when administered in adequate amounts, confer health benefits on the host”. Quite a few fermented products serve as the source of probiotic strains, with many factors influencing the effectiveness of probiotics, including interactions of probiotic bacteria with the host’s microbiome. Prebiotics contain no microorganisms, only substances which stimulate their growth. Prebiotics can be obtained from various sources, including breast milk, soybeans, and raw oats, however, the most popular prebiotics are the oligosaccharides contained in plants. Recent research increasingly claims that probiotics and prebiotics alleviate many disorders related to the immune system, cancer metastasis, type 2 diabetes, and obesity. However, little is known about the role of these supplements as important dietary components in preventing or treating cardiovascular disease. Still, some reports and clinical studies were conducted, offering new ways of treatment. Therefore, the aim of this review is to discuss the roles of gut microbiota, probiotics, and prebiotics interventions in the prevention and treatment of cardiovascular disease.
Keywords: cardiovascular disease, probiotic, prebiotic, gut microbiota, human health
1. Introduction
In recent decades, the incidence of cardiovascular disease (CVD) increased to such extant that they became the principal cause of death worldwide. This is especially noticeable in high- and intermediate-income countries. However, the complex etiologies of CVD and the incomplete understanding of the underlying mechanisms hampered the development of prevention strategies [1].
An unhealthy diet has long been recognized as a major factor for cardiovascular disease morbidity. A connection between diet and cardiovascular events was established through the determinants of metabolic stress and overweight, i.e., adiposity and the presence of visceral fat [2]. While genetic variation has an important influence on Body Mass Index and the distribution of body fat, environmental factors are believed to make a major but still-to-be elucidated contribution to the variation in obesity between different individuals [2,3]. It was not until recently that the complex interactions between dietary components and intestinal microbiota and their food-produced metabolites were acknowledged to play a role in cardiovascular health. Increasing awareness of the role of the gut microbiome in CVD attracted the attention of researchers interested regarding the potential role of probiotics as a study target, e.g., in the prevention of atherosclerosis and other forms of CVD [3,4]. Although knowledge of the changes in the composition of the microbiome associated with coronary heart disease or atherosclerosis is still limited, there is a growing body of evidence supporting this relationship [5].
Functional foods can have beneficial effects against various risk factors associated with cardiovascular disease. However, little is known about the roles of probiotic and prebiotic supplements as important dietary components in the prevention and treatment of CVD [6]. Therefore, the aim of this review is to discuss the roles of gut microbiota and probiotics supplementation in the development of cardiovascular disease based on available reports and clinical studies.
2. Cardiovascular Disease: Risk Factors and the Mechanism of Development
Cardiovascular diseases involve the heart or blood vessels, the most well-known being coronary artery disease, stroke, hypertensive heart disease, cardiomyopathy, venous thrombosis, arrhythmia, and thromboembolic disease. CVD is a growing global health problem [7,8,9]. In 2015, 18 million deaths were attributed to cardiovascular diseases, accounting for approximately one-third of all-cause deaths and representing an increase of 12.5% from 2005. The American Heart Association reports that 92.1 million adults in the US currently have CVD, and it is predicted that approximately 43.9% of the entire U.S. population will have CVD by 2030 [10].
Atherosclerosis is a lipid-driven, chronic, inflammatory disease that is characterized by the formation and progressive growth of atherosclerotic plaques in the walls of arteries. Atherosclerosis is a major predisposing factor for stroke and heart attack. Various immune-mediated mechanisms are implicated in the disease initiation and progression [11]. The initiating incidents of atherogenesis include the retention of lipoproteins in the subendothelial space of the arteries and the activation of endothelial cells. Monocytes enter the vascular wall and differentiate into tissue macrophages. The macrophages ingest lipoproteins and turn into foam cells. Synthetic vascular smooth muscle cells accumulate in atheromas and secrete extracellular matrix proteins. Smooth muscle cells and collagen are important components of the fibrous cap that covers the atherosclerotic plaque [12].
Factors that influence the risk of developing cardiovascular diseases include genetics and a poor lifestyle (lack of activity, unhealthy diet, smoking, alcohol). Hypertension is the most common modifiable risk factor in CVD [13,14]. High blood pressure is often associated with metabolic deregulation, which leads to high blood cholesterol levels that, such as glucose in type 2 diabetes, damage blood vessels and lead to atherosclerosis. The mutual interaction between hypertension and hypercholesterolemia and their influence on the development of atherosclerosis include the renin–angiotensin–aldosterone system and endothelial dysfunction [12,15].
3. Gut Microbiota and Its Effects on Human Health
Microbes colonize all surfaces of the human body, but the human gut is the site of a particularly rich microbiome. It is characterized by an ecological diversity of microorganisms, with more than 100 trillion microbial cells living symbiotically within it [16]. Microbial colonization in the gastrointestinal tract starts immediately after birth. In healthy people, the microbiota lives in a symbiotic relationship with the host, influencing host health by regulating the metabolism of nutrients, protecting against pathogens [17], and providing signals to immune cells to improve host physiology and immunity [18,19,20,21].
Research links the gut microbiota to the development of several cardio-metabolic diseases, including obesity, type 2 diabetes mellitus (T2DM), and cardiovascular disease [22,23,24,25]. The microbiome, particularly in the colon, forms a “bioreactor” that ferments food components that have escaped digestion in the upper parts of the intestine (proteins, carbohydrates, and dietary fibers), breaking these into metabolites or microbial products, e.g., short chain fatty acids and secondary bile acids. The gut microbiota can also transform other dietary components, e.g., polyphenols, into potentially metabolically more relevant forms [26]. Hence, it is not surprising that alternations in the gut microbiota composition might play a role in maintaining human metabolic balance and cardiovascular health.
4. Gut Microbiota, Its Diet-Derived Products, and Cardiovascular Diseases
Many factors are associated with the increase in risk of CVD [7,8,22], but growing evidence indicates that the intestinal microbiome and metabolites contribute importantly in the progression of such diseases. A study conducted by Cui et al. reported that significant differences in the bacterial composition were found between patients with chronic heart failure and control subjects. Of particular note, a decrease in the level of F. prausnitzii and an increase in the level of Ruminococcus gnavus were observed in patients with chronic heart failure [27]. Another study showed that patients with heart failure had higher levels of Prevotella, Hungatella, and Succinclasticum and lower levels of the Lachnospiraceae family (Faecalibacterium and Bifidobacterium) than did control subjects [28]. Moreover, juxtamucosal bacterial overgrowth and higher bacterial adhesion were observed in patients with heart failure [29]. In addition, pathogens such as Candida, Shigella, Yersinia, and Campylobacter were found to be increasingly present in the stools of patients with CVD [30]. Finally, Jie and coworkers [31] analyzed the gut bacterial composition in patients with atherosclerotic cardiovascular disease and observed significant differences with higher levels of Enterobacteriaceae and Streptococcus spp.
Gut bacteria are able to produce diet-derived metabolic products capable of influencing the host’s cardiovascular condition, for example, circulating levels of branched-chain amino acid metabolites, tryptophan, and histidine were associated with insulin resistance and vascular disease. An important example is imidazole propionate, which is formed after the metabolism of histidine. There was a clearly higher concentration of imidazole-propionate in the portal blood of obese diabetes patients compared to obese patients without diabetes [6].
The intestinal microbiome communicates with distant organs, including the heart, through a variety of ways. Among these are the production of trimethylamine (TMA)/trimethylamine N-oxide (TMAO), short-chain fatty acids, bile acids, lipopolysaccharides (LPS), and peptidoglycans [22]. TMAO is one of the more extensively studied metabolites formed by the gut microbiota and comes with a potential role in atherosclerosis. TMA is formed by gut microbiota after meals containing choline, phosphatidylcholine, or carnitine, which are present in foods with high levels of saturated or unsaturated fat. Humans do not possess TMA lyases, so all TMA is formed by the gut microbiota. After absorption, TMA is transported to the liver, where the hepatic enzyme flavin-monooxygenase-3 (FMO3) oxidizes TMA to TMAO [6].
Elevated serum levels of TMAO are positively correlated with early atherosclerosis in humans and monitoring helps to predict mortality risk in patients with stable coronary artery disease and acute coronary syndrome [32,33]. Studies showed that elevated plasma levels of TMAO were associated with the severity of peripheral artery disease and with high risk of cardiovascular mortality in patients with peripheral artery disease [34]. In meta and dose-response analysis studies, elevated plasma TMAO concentrations correlated with increased incidence of major adverse cardiovascular events in coronary heart disease patients [35]. Moreover, increased levels of TMAO were significantly correlated with proinflammatory monocytes in patients with stroke. Haghikia et al. [36] reported that the elevated plasma level of TMAO was also associated with increased cardiovascular events such as myocardial infarction, recurrent stroke, and cardiovascular death. Overall, the mechanisms underlying the effect of TMAO on CVD are not completely explored.
Many studies showed that short-chain fatty acids (SCFA) have a contributing role in CVD. High-fiber diet and acetate supplementation were shown to be able to alter the gut microbiota composition, resulting in the prevention of hypertension and heart failure in hypertensive mice [37]. Nondigestible fibers are fermented in the colon by gut microbiota, which leads to the production of SFCAs, mainly butyrate, propionate, and acetate. The concentrations of SFCAs are lower in patients with atherosclerotic vascular disease or hypertension [6]. SCFAs probably have a beneficial effect on atherosclerotic plaque formation by improving intestinal barrier function [38]. In mouse models of hypertensive cardiovascular disease, propionate attenuated hypertension and its cardiovascular sequelae and reduced the atherosclerotic plaque area and the frequencies of splenic effector memory T cells and splenic T helper 17 cells [6]. SCFAs modulate immune and inflammatory responses via many receptors, e.g., via activation of free fatty acid (FFA) receptors and G protein-coupled receptor 109A and inhibition of histone deacetylases (HDACs) [39]. Since FFA receptors are present in endothelial cells, binding of SFCAs to receptors may evoke not only the stimulation and dampening of the production of inflammatory cytokines, but also influence migration and recruitment of immune cells to the atherosclerotic plaque. SCFA metabolic effects are also mediated via FFA receptors and have direct effects on endothelial cells via HDACs.
It is also recognized that bile acids have a contributing role in CVD. These substances are primarily formed in the liver from cholesterol via two pathways, namely, the classical pathway and the alternative pathway. In the classical pathway, cholesterol is converted into the primary bile acids cholic acid and chenoxycholic acid by enzymes [6]. Bile acids are conjugated with glycine and taurine to form glycocholic acid, taurocholic acid, glycochenoxycholic acid, and taurochnoxycholic acid; these compounds lower pH and the solubility of many nutrients is improved. These bile acids are released into the duodenum, especially after the intake of food, to facilitate digestion and improve the uptake of lipids and lipophilic vitamins [40]. The majority of these substances are reabsorbed in the distal ileum via the sodium-dependent bile acid transporter and returned to the liver via the portal system [41]. The colonic microbiota can convert primary bile acids which are not reabsorbed to secondary bile acids, e.g., deoxycholic acid, lithocholic acid, and other secondary bile acids. The composition of the colonic microbiota has a strong influence on the amount of secondary bile acids formed [6]. In addition to their function in promoting the absorption of lipids and vitamins, bile acids are involved in metabolic processes, intestinal motility, inflammatory processes and liver regeneration. Bile acids exert these effects via bile acid receptors, of which farnesoid X receptor (FXR) and TGR5 receptor are most important and present in many cell types and tissues. Binding of bile acids to FXR reduces lipid levels, improves insulin sensitivity and suppresses hepatic gluconeogenesis, while stimulation of TGR5 reduces the production of cytokines.
In conclusion, the intestinal microbiome plays a vital role in CVD via several routes, and several studies were published relating these diseases to an altered intestinal microbiota structure and function (Table 1). Evidence exists that lifestyle and diet, physical activity, and smoking are modifiers of gut microbiota and, subsequently, are modifiers of cardiovascular health. Hence, therapeutics targeting the specific gut bacteria and probiotics supplementation have promising effects that could be used to treat CVD [22,42].
Table 1.
Studies concerning gut dysbiosis in CVD [6].
| Study Groups | Microbiota Results | References |
|---|---|---|
| Non ischemic heart failure with reduced ejection fraction; n = 28 (vs. 19 controls) | ↑ Streptococcus, Veillonella, Eggerthela ↓ Prevotella, SMB53 (Clostridiaceae) |
[42] |
| Patients with ischemic or dilated cardiomyopathy; n = 84 (vs. 266 controls) | ↑ Prevotella, Hungatella (Lacnospiraceae), Succiniclasticum ↓ Blautia, Anaerostipes, Faecalibacterium, Lachnospiraceae, Bifidobacterium, Eubacterium, Coprococcus |
[28] |
| Stable systolic heart failure; n = 20 (vs. 20 controls) | ↑ Escherichia-Shigella ↓ Blautia, Collinsella, Ruminococcaceae, Erysipelotrichaceaem Faecalibacterium |
[38] |
| Patients with ischemic or dilated cardiomyopathy; n = 53 (vs. 40 controls) | ↑ Ruminococcus, Acinetobacter, Veillonella ↓ Faecalibacterium, Alistipes, Oscilibacter |
[27] |
| Patients with hypertension (≥140/90 mmHg); n = 60 (vs. 60 controls) | ↑ Klebsiella, Salmonella, Streptococcus, Clostridium, Parabacteroides, Eggerthella ↓ Faecalibacterium, Roseburia, Synergistetes |
[43] |
| Patients with hypertension (≥140/90 mmHg) and pre-hypertensive patients (125/80–139/90 mmHg); n = 155 (vs. 41 controls) | ↑ Prevotella, Klebsiella, Porphyromonas ↓ Faecalibacterium, Roseburia, Bifidobacterium, Oscillibacter, Coprococcus, Butyrivibrio |
[44] |
| Patients with coronary artery disease; n = 70 (vs. 98 controls) | ↑ Escherichia-Shigella, Lactobacillus, Enterococcus, Streptococcus ↓ Faecalibacterium, Roseburia, Eubacterium, Subdoligranulum |
[45] |
| Patients with stable angina and old myocardial infarction who underwent percutaneous coronary intervention or bypass; n = 39 (vs. 30 controls) | ↑ Lactobacillales ↓ Bacteroides, Clostridium |
[46] |
| Patients with atherosclerotic plaques with clinical presentations of stable or unstable angina or acute myocardial infarction; n = 218 (vs. 187 controls) | ↑ Enterobacteriaceae, Streptococcus, Lactobacillus salivarius, Atopobium parvulum, Ruminococcus gnavus, Eggerthella lenta ↓ Roseburia, Faecalibacterium |
[31] |
5. Probiotics and Prebiotics: General Information
Probiotics (Greek; Pro: promotion, Biotic: life) are defined as “live microorganisms which, when administered in adequate amounts, confer health benefits on the host” [47]. A large range of fermented products, such as yogurt, kefir, sauerkraut, tempeh, and kimchi, which serve as sources of probiotic strains, are part of the human diet across diverse cultures. According to the current state of knowledge, probiotics encompass both bacteria (Lactobacillus, Lactococcus, Leuconostoc, Pediococcus, Propionibacterium, Bifidobacterium, Bacillus, some Streptococcus, Enterococcus, Escherichia coli) and yeast (Saccharomyces) genera [48].
Many factors influence the effectiveness of probiotics, including interactions of probiotic bacteria with the host and its microbiome. In order to make a positive impact, probiotics must chemically or physically inhibit the growth of pathogenic bacteria (e.g., Enterococcus faecalis, Salmonella enterica subsp. enterica serotype Enteritidis, Listeria monocytogenes, Staphylococcus aureus, and E. coli) by immune, hormonal, and neuronal manipulations. It is important that they also stimulate the growth of beneficial microorganisms [49].
More and more research increasingly claims that probiotics alleviate many disorders related to the immune system, cardiovascular health, cancer metastasis, depression, anxiety, type 2 diabetes, and obesity [48]. Recently, the safety profiles of different probiotics as a function of different genera, species, and strains, coupled with their relevance to diverse individuals or at-risk populations, attracted attention [48]. The FAO/WHO (Food and Agriculture Organization/ World Health Organization) [50] guidelines on probiotic evaluation from 2002 reported that probiotics may theoretically be linked to specific types of side effects in patients with underlying medical conditions. The at-risk population groups are broadly characterized by weakened immune systems, gut dysbiosis, and/or impaired intestinal barriers, therefore, it is important to carefully assess the safety associated with deliberate administration of probiotics.
According to the provisions of the WHO, the number of living cells in probiotic foods at the time of human consumption may not be lower than 106 cells per 1 mL or 1 g of product. Furthermore, the therapeutic dose is 108–109 cells in 1 mL or 1 g of product [51]. Of note, the contained microorganisms must be resistant to the action of gastric juice and bile salts. After passing through this chemical barrier, probiotics should then adhere to the surface of the intestine, where their health-promoting functions can be realized [51].
Products deemed probiotics enhance the nonspecific cellular immune response through the activation of natural killer cells and macrophages and the release of various cytokines. They can also improve the gut mucosal immune system by increasing the number of IgA(+) cells [52]. Moreover, probiotics can aid the process of digestion and the breakdown of lactose, improve the absorption of minerals, and enhance the synthesis of many vitamins (thiamin, riboflavin, niacin, pantothenic acid, vitamin K). They play an important role in the treatment of various diseases, such as hepatic disease, diarrhea, and gastroenteritis. In addition, they were also shown to have antiproliferative, proapoptotic, and antioxidative properties [52].
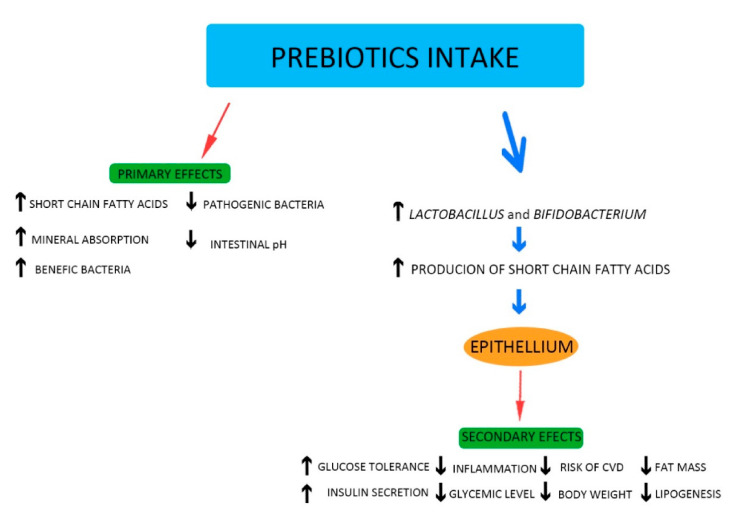
Prebiotics represent substances most used to maintain a normal gut microbiota and restore its equilibrium when homeostasis is affected [53,54,55]. Prebiotics contain only substances which stimulate microorganism growth; there are no bacteria in their composition [9]. These substances can be obtained from various sources, including soybeans, raw oats. and honey [9,56]. However, the most popular prebiotics are plant oligosaccharides [51]. Nondigestible carbohydrates, including polysaccharides (resistant starch, pectin, and dextrin) and oligosaccharides, such as fructooligosaccharides, galactooligosaccharide, xylooligosacharides, isomaltooligosaccharides, mannanooligosaccharides, raffinose oligosaccharides, arabinoxylanoligosaccharides, lactulose, and inulin, possess prebiotic properties [53,54,57]. Prebiotics have the potential to improve human health by controlling the balance of the intestinal microbiome. They are fermented by the gut bacteria and produce short-chain fatty acids, e.g., propionate, butyrate, and acetate. The production of short-chain fatty acids has positive effects, including improvement of intestinal membrane integrity and absorption of minerals, lowering both glycemic levels and body weight, improved immunity, and modulation of metabolic, cardiovascular, and inflammatory biomarkers [53]. Also, the intake of prebiotics favors the growth of beneficial bacteria, such as Lactobacillus and Bifidobacterium, which are responsible for inhibition of the proliferation of harmful bacteria (Figure 1) [53,54].
Figure 1.
Positive effects of prebiotics.
Due to the benefits to human health, prebiotics are increasingly used by the food industry as functional ingredients. These compounds can be employed in the production of whole-wheat bread, cereal bars, chocolate, dairy products, infant formulas, and meat products, among others. In addition to natural sources, microorganisms and enzymes can be used for the synthesis of prebiotic compounds [58]. Combinations of prebiotics and probiotics are called synbiotics [53].
6. The Influence of Probiotics and Prebiotics on the Mechanisms and Factors Causing CVD
6.1. Oxidative Stress
Oxidative stress is known to play a role in the course of CVD [59,60]. This phenomenon refers to elevated intracellular levels of oxygen radicals that cause damage to lipids, proteins, and DNA [61]. Reactive oxygen species (ROS), including superoxide anion radicals, hydroxyl radicals, and hydrogen peroxide, are one of the highly active free radicals. Most living organisms possess enzymatic defenses (superoxide dismutase (SOD), glutathione peroxidase (GPx), glutathione reductase (GR), catalase (CAT), nonenzymatic antioxidant defenses (glutathione (GSH), thioredoxin, vitamin C, vitamin E), and repair systems to protect them against oxidative stress [61]. However, these native antioxidant systems are generally not enough to prevent living organisms from oxidative damage. Many researches showed that probiotic bacteria present significant antioxidant abilities both in vivo and in vitro [62]. ROS can be both endogenously and exogenously generated. Due to their highly reactive nature, ROS can modify other oxygen species, DNA, proteins, or lipids. It is believed that excessive amounts of ROS can cause genomic instability, leading to a variety of chronic diseases, including atherosclerosis and cardiovascular disease [63]. ROS are generated by several enzymatic reactions and chemical processes. NADPH oxidase (NOX) complex is considered to be a major source of ROS generation [64]. There are seven human NOX homologues that function to purposely produce ROS for a range of host defense and signaling functions. Recently, Gómez-Guzmán and colleagues suggested that the probiotics Lactobacillus fermentum CECT5716, Lactobacillus coryniformis CECT5711 (K8), and Lactobacillus gasseri CECT5714 (LC9) (1:1) are able to decrease NOX activity and mRNA expression of NOX-1 and NOX-4 in spontaneously hypertensive rats [65].
Cyclo-oxygenase (COX) is a rate-limiting enzyme in prostaglandin biosynthesis and a two-step enzymatic process in which ROS are generated. COX-2 is upregulated in atherosclerotic lesions and catalyzes the production of the majority of vascular prostanoids in human atherosclerotic areas. Downregulated COX-2 was found in Helicobacter pylori-infected mongolian gerbils with a commercial probiotic Lacidofil treatment [66]. Patel and colleagues demonstrated that Lactobacillus acidophilus pretreatment decreased COX-2 expression in catla thymus macrophages compared to Aeromonas hydrophila and co-stimulated macrophages [67].
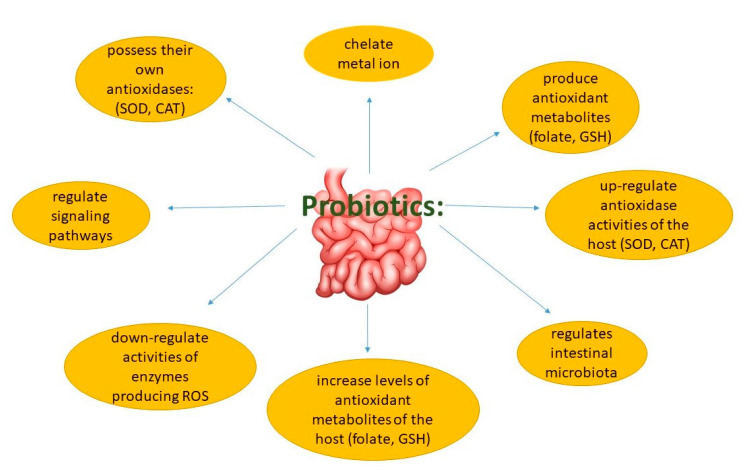
In recent years, many studies focused on antioxidant properties of probiotics. The culture supernatant, intact cells, and intracellular cell-free extracts of Bifidobacterium animalis 01 were found to scavenge hydroxyl radicals and superoxide anions in vitro [61]. Further, oxidative stress in patients with type 2 diabetes was found to be ameliorated by multispecies probiotics [68]. Lactic acid bacteria stains (LAB) were studied widely both in animals and the human body, revealing that LAB can resist ROS, including peroxide radicals, superoxide anions, and hydroxyl radicals [61]. Rats fed high-fat diets supplemented with Lactobacillus plantarum P-8 presented an elevated antioxidant ability, as reflected by curtailing the accumulation of liver lipids and protecting healthy liver function [69]. In humans, Lactobacillus rhamnosus exerted strong antioxidant activity in situations of elevated physical stress [61]. During the past decades, studies demonstrated that probiotic bacteria strains could exert antioxidant capacity in different ways (Figure 2).
Figure 2.
Modulation of antioxidation by probiotics.
Dietary supplementation of prebiotics, e.g., inulin or oligofructose, contributes to protection from oxidative stress. Inulin, through short-chain fatty acids, can act as a scavenger of reactive oxygen species (ROS). It is also able to modulate responses to pathogenic bacterial insults (LPS) and protect gut from inflammatory processes, probably stimulating defenses against ROS by upregulating colonic mucosal detoxification enzymes (GSTs); in this way, inulin restores the level of some important proteins involved in intestinal smooth muscle contraction [70].
6.2. Inflammation
Low-grade inflammation is the cornerstone of many chronic diseases. This type of inflammation increases with age, being common in people of advanced age, and is known to be a risk factor for CVD [6]. In these cardiovascular conditions, higher plasma levels of proinflammatory mediators, such as TNFα, IL1, and IL6, are frequently found. Often, inflammation is linked to an increased intestinal permeability, with elevated intestinal translocation of proinflammatory mediators of bacterial origin, such as LPS. Increased cumulative incidence of CVD with increased serum levels of LPS-binding protein was previously noted. LPS and other bacterial cell membrane constituents are recognized by several receptors on endothelial cells. Binding of LPS directly induces adhesion molecules, such as ICAM-1 and P-selectin on endothelial cells, which are important for interactions with leukocytes [71].
The abovementioned data highlight the potential role of the gut microbiota in controlling intestinal permeability and endotoxemia and, therefore, the development of chronic, low-grade inflammation and the risk for CVD. These findings explain why there is increasing interest in developing intervention strategies targeting the microbiota to achieve downregulation of low-grade inflammation as a way of preventing CVD. Therefore, foods and ingredients, such as probiotics and prebiotics, represent promising tools for the dietary management of CVD risk [6].
Tenorio-Jimenez et al. [72] reported that a 12-week administration of L. reuteri V3401 was associated, beyond a reduced risk of CVD, with lower levels of inflammation biomarkers, such as TNF-α, IL-6, IL-8, and soluble intercellular adhesion molecule-1, in obese adults aged 18 to 65 years with metabolic syndrome. However, although some studies demonstrated that probiotics can decrease the production of proinflammatory cytokines, their underlying mechanism remains unclear [9].
In recent years, many research focused on the use of dietary fibers and prebiotics, since many of these polysaccharides can be metabolized by intestinal microbiota, leading to the production of short-chain fatty acids. These metabolites of prebiotic fermentation show anti-inflammatory and immunomodulatory capabilities [53,54]. Kanner et al. [73] showed that inulins, as dietary antioxidants, may play a role in preventing lipid peroxidation in the stomach. In general, dietary supplementation of inulin or oligofructose contributes to protection from oxidative stress, consequently preventing inflammatory reactions associated with oxidative stress [70]. Goderska valuated the prebiotic and anti-inflammatory properties of lactobionic acid (LBA), observing bacterial growth proportional to its concentration, especially for Lactobacilli and Bifidobacterium [74]. LBA is probably resistant to digestive enzymes, so it reaches the colon intact where it is fermented by microbiota. On the other hand, LBA also has anti-inflammatory properties, and it was demonstrated that its administration was associated with a decrease in obesity and better control of metabolic parameters [75].
Isomaltooligosaccarides (IMOs) also promote Lactobacilli and Bifidobacterium growth both in vitro and in vivo [76]. An in vivo study showed the positive effects of isomaltooligosaccarides, green tea extract (GTE), and a combination of IMO and GTE on visceral adipose tissue on the production of proinflammatory cytokines and on lipid and glycemic control. It was also shown to improve insulin, glucagon, and leptin levels in mice [77]. It was investigated that galactooligosaccharides (GOS) can modulate inflammatory process and immune function. GOS increases the levels of cytokine IL-10, interleukin 8 (IL-8), and C-reactive protein and improves natural killer (NK) cell activity [78].
6.3. Hypercholesterolemia and High Blood Pressure
Probiotics may reduce cholesterol levels by means of several mechanisms [9]. Most Bifidobacteria bacteria demonstrate higher choliloglicin hydrolase activity than do other microorganisms. This enzyme hydrolyzes the amide bonds conjugated with taurine or glycine in bile acids, resulting in the release of primary bile acids; these are easily precipitated at low pH, resulting in their expulsion from the gastrointestinal tract. As these are not reabsorbed from the intestine, they must be replaced by bile produced in the liver from blood cholesterol [51]. Probiotics may exert cholesterol-lowering effects through bile salt hydrolase (an enzyme of probiotics which hydrolyzes bile salts into amino acid residues and free bile salts) [79]. These beneficial effects were demonstrated in both animal models and clinical trials [80,81]. Furthermore, the relationship between gut microbiota, probiotics, and disturbances in lipid metabolism are well explained.
In a randomized, single-blinded, controlled clinical trial, the supplementation with 200 g/day of a probiotic yogurt containing Streptococcus thermophiles, L. bulgaricus, L. acidophilus LA-5, and B. animalis BB12 for nine weeks among 70 pregnant women in the third trimester of gestation resulted in a significant reduction in total cholesterol, low-density lipoprotein (LDL) cholesterol, and high-density lipoprotein (HDL) levels, as well as serum triglyceride concentrations [82]. In another study conducted by Hoppu et al. [83], 256 pregnant women allocated into three groups, including dietary counseling with probiotics (L. rhamnosus GG and B. lactis), placebo dietary counseling, and without counseling (control group) from the first trimester of pregnancy to 12 months postpartum, exhibited similar lipid serum levels during pregnancy. In other research, small-scale, double-blind, placebo-controlled studies observed the beneficial effects of probiotic supplementation in dyslipidemia [84].
It was indicated that probiotic supplementation reduces blood lipid concentrations [85]. Lew et al. [86] found that L. plantarum DR7 exerts cholesterol-lowering properties via AMPK phosphorylation. Another group of researchers [87] suggested that the probiotic L. plantarum PH40 may also possess cholesterol-lowering properties.
Many clinical trials found probiotic use to be associated with a moderate or significant reduction in blood pressure [9,88,89]. The antihypertensive action of probiotics is believed to act via several mechanisms, including regulating the renin–angiotensin system [89]. Probiotics also play a role in thrombotic disorders. Although the precise roles played by probiotics in the modulation of hemostasis and its various elements, such as blood platelet function, are generally not well documented, several reports were produced on this subject. For example, Schreiber et al. indicated that L. reuteri reduces P-selectin expression on the platelet surface and decreases blood platelet–endothelial cell interactions in rats treated with dextran sodium sulfate [90]. Moreover, Haro and Medina [91] reported that the oral administration of L. casei CRL431 may be a promising candidate for the prevention of thrombotic complications associated with pneumococcal pneumonia.
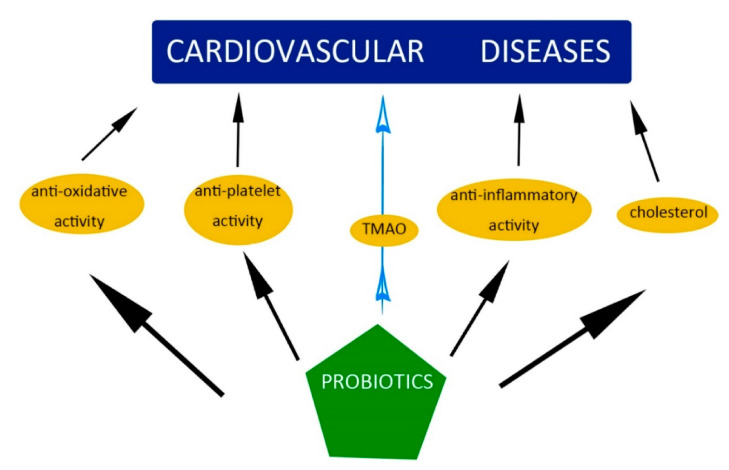
In summary, probiotics play an important role in the treatment of various diseases, such as hepatic disease, diarrhea, and gastroenteritis. Probiotics were also shown to have antioxidative, antiplatelet, and anti-inflammatory properties and to lower the level of cholesterol (Figure 3).
Figure 3.
The impact of probiotics on cardiovascular disease (CVD).
Prebiotics also reduce levels of cholesterol. Parnell and Reiner [92] reported that prebiotic intake lowered total serum cholesterol in a hypercholesterolemic rat model. During this research, rats were administered one of three diets with 0, 10, or 20% prebiotic fiber for 10 weeks. Both doses of prebiotic fiber reduced serum cholesterol concentrations about 25%. Moreover, this change was correlated with an increase in caeca digesta, as well as the upregulation of genes involved in cholesterol biosynthesis and bile production. In addition, the obese rats with 10% prebiotic supplementation demonstrated an approximately 40% reduction in triacylglycerol accumulation in the liver. Obesity is often associated with the progression of cardiovascular disease and both probiotic and prebiotic intake were reported to have antiobesogenic effects in various clinical trials [93,94,95].
A number of researches reported synbiotics to possess promising hypercholesterolemic properties [96,97,98]. Mofid et al. [96] noted that the regular intake of synbiotic yogurts reduces the risk of cardiovascular diseases among hypercholesterolemic patients. Liong et al. [97] reported that a synbiotic containing L. acidophilus ATCC 4962 reduced total cholesterol, triacylglycerol, and LDL-cholesterol in hypercholesterolemic pigs via the interrelated ways of lipid transporters, including high-density lipoprotein, low-density lipoprotein, and very low-density lipoprotein (VLDL). The animals on the synbiotic diet were fed with L. acidophilus ATCC 4962 (1 g/pig per day), mannitol (1.56 g/pig per day), fructo-oligosacharides (1.25 g/pig per day), and inulin (2.2 g/pig per day).
7. Conclusions
The intake of probiotics and prebiotics plays an important role in the restoring the normal intestinal flora favoring the growth of beneficial bacteria and reducing the risk of development of chronic ailments, such as cardiovascular disease. Therefore, the interest of these compounds as ingredients for the elaboration of novel foods with functional characteristics is well accepted. Addressing these problems is at the early stages of research. The scientific community must fully clarify how native microbiota affects human health and wellbeing while reliably modeling predictions of interactions of probiotic strains and native gut microbiota, which would allow successful personalization of prebiotic and probiotic therapy, determination of the length of supplementations, and definition of the optimal dosages for individuals to maintain cardiovascular health or to ameliorate some cardiovascular disease.
The field of gut microbiome research is relatively new and complex, and the methods used are far from standardized and harmonized. In many clinical studies, sample sizes were relatively small, with control groups often lacking. A disturbing issue is that different methods were applied for samples for collecting, processing, and storing. It was shown that these methodological differences pose a risk for introducing artefacts. The enormous datasets generated when microbiota, metabolomes, genomes, and transcriptomes are evaluated in cohorts or in intervention studies are challenging, and different complex bioinformatics methods have been applied. There is clearly a need to develop this area of research both in observational and randomized intervention trials. Thus, to enhance the current level of understanding, well-designed clinical trials involving all the aspects of lifestyle, gut microbiota, metabolites, and genetic background should be developed.
Author Contributions
Conceptualization, A.O. and T.O.; methodology, A.O.; writing—original draft preparation, A.O., T.O., and M.G.; writing—review and editing, A.O., M.G., and J.S.; supervision, A.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Katsimichas T., Antonopoulos A.S., Katsimichas A., Ohtani T., Sakata Y., Tousoulis D. The intestinal microbiota and cardiovascular disease. Cardiovasc. Res. 2019;115:1471–1486. doi: 10.1093/cvr/cvz135. [DOI] [PubMed] [Google Scholar]
- 2.Attaye I., Pinto-Sietsma S., Herrema H., Nieuwdorp M. A crucial role for diet in the relationship between gut microbiota and cardiometabolic disease. Annu. Rev. Med. 2020;71:149–161. doi: 10.1146/annurev-med-062218-023720. [DOI] [PubMed] [Google Scholar]
- 3.Jonsson A.L., Bäckhed F. Role of gut microbiota in atherosclerosis. Nat. Rev. Cardiol. 2017;14:79–87. doi: 10.1038/nrcardio.2016.183. [DOI] [PubMed] [Google Scholar]
- 4.Tang W.H.W., Kitai T., Hazen S.L. Gut microbiota in cardiovascular health and disease. Circ. Res. 2017;120:1183–1196. doi: 10.1161/CIRCRESAHA.117.309715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang W.H.W., Bäckhed F., Landmesser U., Hazen S.L. Intestinal microbiota in cardiovascular health and disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2019;73:2089–2105. doi: 10.1016/j.jacc.2019.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerdes V., Gueimonde M., Pajunen L., Nieuwdorp M., Laitinen K. How strong is the evidence that gut microbiota composition can be influenced by lifestyle interventions in a cardio-protective way? Atherosclerosis. 2020;311:124–142. doi: 10.1016/j.atherosclerosis.2020.08.028. [DOI] [PubMed] [Google Scholar]
- 7.Shanthi M., Pekka P., Bo N. Global Atlas on Cardiovascular Diseases Prevention and Control. World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization; Geneva, Switzerland: 2011. pp. 3–18. [Google Scholar]
- 8.Guarner F., Malagelada J.R. Gut flora in health and disease. Lancet. 2003;361:512–519. doi: 10.1016/S0140-6736(03)12489-0. [DOI] [PubMed] [Google Scholar]
- 9.Olas B. Probiotics, prebiotics and synbiotics—A promising strategy in prevention and treatment of cardiovascular diseases? Int. J. Mol. Sci. 2020;21:9737. doi: 10.3390/ijms21249737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu C., Weng Z., Zhang L., Xu J., Dahal M., Basnet T., Gu A. HDL cholesterol: A potential mediator of the association between urinary cadmium concentration and cardiovascular disease risk. Ecotoxicol. Environ. Saf. 2021;208:111433. doi: 10.1016/j.ecoenv.2020.111433. [DOI] [PubMed] [Google Scholar]
- 11.Kurilenko N., Fatkhullina A.R., Mazitova A., Koltsova E.K. Act Locally, Act Globally-Microbiota, Barriers, and Cytokines in Atherosclerosis. Cells. 2021;10:348. doi: 10.3390/cells10020348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paganelli F., Mottola G., Fromonot J., Marlinge M., Deharo P., Guieu R., Ruf J. Hyperhomocysteinemia and cardiovascular disease: Is the adenosinergic system the missing link? Int. J. Mol. Sci. 2021;22:1690. doi: 10.3390/ijms22041690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krasi G., Precone V., Paolacci S., Stuppia L., Nodari S., Romeo F., Perrone M., Bushati V., Dautaj A., Bertelli M. Genetics and pharmacogenetics in the diagnosis and therapy of cardiovascular diseases. Acta Biomed. 2019;90:7–19. doi: 10.23750/abm.v90i10-S.8748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doughty K.N., Del Pilar N.X., Audette A., Katz D.L. Lifestyle medicine and the management of cardiovascular disease. Curr. Cardiol. Rep. 2017;19:116. doi: 10.1007/s11886-017-0925-z. [DOI] [PubMed] [Google Scholar]
- 15.Ma W., Zhang B., Yang Y., Qi L., Meng L., Zhang Y., Huo Y. Correlating the relationship between interarm systolic bloodpressure and cardiovascular disease risk factors. J. Clin. Hypertens. 2017;19:466–471. doi: 10.1111/jch.12987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eckburg P.B., Bik E.M., Bernstein C.N., Purdom E., Dethlefsen L., Sargent M., Gill S.R., Nelson K.E., Relman D.A. Diversity of the human intestinal microbial flora. Science. 2005;308:1635–1638. doi: 10.1126/science.1110591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bäumler A.J., Sperandio V. Interactions between the microbiota and pathogenic bacteria in the gut. Nature. 2016;535:85–93. doi: 10.1038/nature18849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Filippo C., Cavalieri D., Di Paola M., Ramazzotti M., Poullet J.B., Massart S., Collini S., Pieraccini G., Lionetti P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA. 2010;107:14691–14696. doi: 10.1073/pnas.1005963107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gensollen T., Iyer S.S., Kasper D.L., Blumberg R.S. How colonization by microbiota in early life shapes the immune system. Science. 2016;352:539–544. doi: 10.1126/science.aad9378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katsi V., Didagelos M., Skevofilax S., Armenis I., Kartalis A., Vlachopoulos C., Karvounis H., Tousoulis D. Gut microbiota—Gut dysbiosis—Arterial hypertension: New horizons. Curr. Hyperten. Rev. 2019;15:40–46. doi: 10.2174/1573402114666180613080439. [DOI] [PubMed] [Google Scholar]
- 21.Suárez-Zamorano N., Fabbiano S., Chevalier C., Stojanović O., Colin D.J., Stevanović A., Veyrat-Durebex C., Tarallo V., Rigo D., Germain S., et al. Microbiota depletion promotes browning of white adipose tissue and reduces obesity. Nat. Med. 2015;21:1497–1501. doi: 10.1038/nm.3994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suganya K., Son T., Kim K.W., Koo B.S. Impact of gut microbiota: How it could play roles beyond the digestive system on development of cardiovascular and renal diseases. Microb. Pathog. 2020:104583. doi: 10.1016/j.micpath.2020.104583. in press. [DOI] [PubMed] [Google Scholar]
- 23.Arora T., Bäckhed F. The gut microbiota and metabolic disease: Current understanding and future perspectives. J. Intern. Med. 2016;280:339–349. doi: 10.1111/joim.12508. [DOI] [PubMed] [Google Scholar]
- 24.Wang Z., Koonen D., Hofker M., Fu J. Gut microbiome and lipid metabolism: From associations to mechanisms. Curr. Opin. Lipidol. 2016;27:216–224. doi: 10.1097/MOL.0000000000000308. [DOI] [PubMed] [Google Scholar]
- 25.Trautwein E.K., Peters H.P.F., Mela D.J., Edwards C., Herrema H., Fud J., Geldof M., Albers R. Is gut microbiota a relevant and competitive dietary target for cardiometabolic health? Proceedings of an expert workshop. Trends Food Sci. Technol. 2018;81:146–154. doi: 10.1016/j.tifs.2018.09.005. [DOI] [Google Scholar]
- 26.Levy M., Kolodziejczyk A.A., Thaiss C.A., Elinav E. Dysbiosis and the immune system. Nat. Rev. Immunol. 2017;17:219–232. doi: 10.1038/nri.2017.7. [DOI] [PubMed] [Google Scholar]
- 27.Cui X., Ye L., Li J., Jin L., Wang W., Li S., Bao M., Wu S., Li L., Geng B., et al. Metagenomic and metabolomic analyses unveil dysbiosis of gut microbiota in chronic heart failure patients. Sci. Rep. 2018;8:635. doi: 10.1038/s41598-017-18756-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kummen M., Mayerhofer C.C.K., Vestad B., Broch K., Awoyemi A., StormLarsen C., Ueland T., Yndestad A., Hov J.R., Trøseid M. Gut microbiota signature in heart failure defined from profiling of 2 independent cohorts. J. Am. Coll. Cardiol. 2018;71:1184–1186. doi: 10.1016/j.jacc.2017.12.057. [DOI] [PubMed] [Google Scholar]
- 29.Sandek A., Swidsinski A., Schroedl W., Watson A., Valentova M., Herrmann R., Scherbakov N., Cramer L., Rauchhaus M., Grosse-Herrenthey A., et al. Intestinal blood flow in patients with chronic heart failure: A link with bacterial growth, gastrointestinal symptoms, and cachexia. J. Am. Coll. Cardiol. 2014;64:1092–1102. doi: 10.1016/j.jacc.2014.06.1179. [DOI] [PubMed] [Google Scholar]
- 30.Pasini E., Aquilani R., Testa C., Baiardi P., Angioletti S., Boschi F., Verri M., Dioguardi F. Pathogenic gut flora in patients with chronic heart failure. JACC Heart Fail. 2016;4:220–227. doi: 10.1016/j.jchf.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 31.Jie Z., Xia H., Zhong S.L., Feng Q., Li S., Liang S., Zhong H., Liu Z., Gao Y., Zhao H., et al. The gut microbiome in atherosclerotic cardiovascular disease. Nat. Commun. 2017;8:845. doi: 10.1038/s41467-017-00900-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Randrianarisoa E., Lehn-Stefan A., Wang X., Hoene M., Peter A., Heinzmann S.S., Zhao X., Konigsrainer V., Konigsrainer A., Balletshofer B., et al. Relationship of serum trimethylamine N-oxide (TMAO) levels with early atherosclerosis in humans. Sci. Rep. 2016;6:26745. doi: 10.1038/srep26745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Senthong V., Wang Z., Li X.S., Fan Y., Wu Y., Tang W.H.W., Hazen S.L. Intestinal microbiota-generated metabolite trimethylamine-N-oxide and 5-year mortality risk in stable coronary artery disease: The contributory role of intestinal microbiota in a COURAGE-like patient cohort. J Am. Heart. Assoc. 2016;5:e002816. doi: 10.1161/JAHA.115.002816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roncal C., Martínez-Aguilar E., Orbe J., Ravassa S., Fernandez-Montero A., Saenz-Pipaon G., Ugarte A., Estella-Hermoso de Mendoza A., Rodriguez J.A., Fernandez-Alonso S., et al. Trimethylamine-N oxide (TMAO) predicts cardiovascular mortality in peripheral artery disease. Sci. Rep. 2019;9:15580. doi: 10.1038/s41598-019-52082-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miao-En Y., Peng-Da L., Xu-Jie Z., Lei W. Trimethylamine-N-oxide has prognostic value in coronary heart disease: A meta-analysis and dose-response analysis. BMC Cardiovasc. Disord. 2020;20:6953212. doi: 10.1186/s12872-019-01310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haghikia A., Li X.S., Liman T.G., Bledau N., Schmidt D., Zimmermann F., Kränkel N., Widera C., Sonnenschein K., Haghikia A., et al. Gut microbiota-dependent trimethylamine N-oxide predicts risk of cardiovascular events in patients with stroke and is related to proinflammatory monocytes. Arterioscler. Thromb. Vasc. Biol. 2018;38:2225–2235. doi: 10.1161/ATVBAHA.118.311023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marques F.Z., Nelson E., Chu P.Y., Horlock D., Fiedler D., Ziemann M., Tan J.K., Kuruppu S., Rajapakse N.W., El-Osta A., et al. High-Fiber diet and acetate supplementation change the gutmicrobiota and prevent the development of hypertension and heart failure in hypertensive mice. Circulation. 2017;135:964–977. doi: 10.1161/CIRCULATIONAHA.116.024545. [DOI] [PubMed] [Google Scholar]
- 38.Luedde M., Winkler T., Heinsen F.A., Rühlemann M.C., Spehlmann M.E., Bajrovic A., Lieb W., Franke A., Ott S.J., Frey N. Heart failure is associated with depletion of core intestinal microbiota. ESC Heart Fail. 2017;4:282–290. doi: 10.1002/ehf2.12155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li M., van Esch B.C.A.M., Wagenaar G.T.M., Garssen J., Folkerts G., Henricks P.A.J. Pro- and anti-inflammatory effects of short chain fatty acids on immune and endothelial cells. Eur. J. Pharmacol. 2018;831:52–59. doi: 10.1016/j.ejphar.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Kuipers F., Bloks V.W., Groen A.K. Beyond intestinal soap–bile acids in metabolic control. Nat. Rev. Endocrinol. 2014;10:488–498. doi: 10.1038/nrendo.2014.60. [DOI] [PubMed] [Google Scholar]
- 41.Döring B., Lütteke T., Geyer J., Petzinger E. The SLC10 carrier family: Transport functions and molecular structure. Curr. Top. Membr. 2012;70:105–168. doi: 10.1016/B978-0-12-394316-3.00004-1. [DOI] [PubMed] [Google Scholar]
- 42.Katsimichas T., Ohtani T., Motooka D., Tsukamoto Y., Kioka H., Nakamoto K., Konishi S., Chimura M., Sengoku K., Miyawaki H., et al. Non-Ischemic Heart Failure with Reduced Ejection Fraction Is Associated with Altered Intestinal Microbiota. Circ. J. 2018;82:1640–1650. doi: 10.1253/circj.CJ-17-1285. [DOI] [PubMed] [Google Scholar]
- 43.Yan Q., Gu Y., Li X., Yang W., Jia L., Chen C., Han X., Huang Y., Zhao L., Li P., et al. Alterations of the gut microbiome in hypertension. Front. Cell. Infect. Microbiol. 2017;7:381. doi: 10.3389/fcimb.2017.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li J., Zhao F., Wang Y., Chen J., Tao J., Tian G., Wu S., Liu W., Cui Q., Geng B., et al. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome. 2017;5:14. doi: 10.1186/s40168-016-0222-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhu Q., Gao R., Zhang Y., Pan D., Zhu Y., Zhang X., Yang R., Jiang R., Xu Y., Qin H. Dysbiosis signatures of gut microbiota in coronary artery disease. Physiol. Genom. 2018;50:893–903. doi: 10.1152/physiolgenomics.00070.2018. [DOI] [PubMed] [Google Scholar]
- 46.Emoto T., Yamashita T., Kobayashi T., Sasaki N., Hirota Y., Hayashi T., So A., Kasahara K., Yodoi K., Matsumoto T., et al. Characterization of gut microbiota profiles in coronary artery disease patients using data mining analysis of terminal restriction fragment length polymorphism: Gut microbiota could be a diagnostic marker of coronary artery disease. Heart Ves. 2017;32:39–46. doi: 10.1007/s00380-016-0841-y. [DOI] [PubMed] [Google Scholar]
- 47.Gerritsen J., Smidt H., Rijkers G.T., de Vos W.M. Intestinal microbiota in human health and disease: The impact of probiotics. Genes Nutr. 2011;6:209–240. doi: 10.1007/s12263-011-0229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kothari D., Patel P., Kim S.K. Probiotic supplements might not be universally-effective and safe: A review. Biomed. Pharmacoth. 2019;11:537–547. doi: 10.1016/j.biopha.2018.12.104. [DOI] [PubMed] [Google Scholar]
- 49.Zucko J., Starcevic A., Diminic J., Oros D., Mortazavian A.M., Putnik P. Probiotic-friend or foe? Curr. Opin. Food Sci. 2020;32:45–49. doi: 10.1016/j.cofs.2020.01.007. [DOI] [Google Scholar]
- 50.Guildelines for the Evaluation of Probiotics in Food. Joint FAO/WHO Working Group on Drafting Guidelines for the Evaluation of Probiotics in Food; London, ON, Canada: 2002. [Google Scholar]
- 51.Pandey K.R., Naik S.R., Vakil B.V. Probiotics, prebiotics and synbiotics-A review. J. Food Sci. Technol. 2010;52:7577–7587. doi: 10.1007/s13197-015-1921-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nowak A., Paliwoda A., Blasiak J. Anti-proliferative, pro-apoptotic and anti-oxidative activity of Lactobacillus and Bifidobacterium strains: A review of mechanism and therapeutic perspectives. Crit. Rev. Food. Sci. Nutr. 2018;1:1–12. doi: 10.1080/10408398.2018.1494539. [DOI] [PubMed] [Google Scholar]
- 53.Farias D.P., Araújo F.F., Neri-Numa I.A., Pastore G.M. Prebiotics: Trends in food, health and technological applications. Trends Food Sci. Technol. 2019;93:23–35. doi: 10.1016/j.tifs.2019.09.004. [DOI] [Google Scholar]
- 54.Mohanty D., Misra S., Mohapatra S., Sahu P.S. Prebiotics and synbiotics: Recent concepts in nutrition. Food Biosci. 2018;26:152–160. doi: 10.1016/j.fbio.2018.10.008. [DOI] [Google Scholar]
- 55.Quigley E.M.M. Prebiotics and probiotics in digestive health. Clin. Gastroenterol. Hepatol. 2019;17:333–344. doi: 10.1016/j.cgh.2018.09.028. [DOI] [PubMed] [Google Scholar]
- 56.Pokusaeva K., Fitzgerald G.F., van Sinderen D. Carbohydrate metabolism in Bifidobacteria. Genes Nutr. 2011;6:285–306. doi: 10.1007/s12263-010-0206-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Colantonio A.G., Werner S.L., Brown M. The effects of prebiotics and substances with prebiotic properties on metabolic and inflammatory biomarkers in individuals with type 2 diabetes mellitus: A systematic review. J. Acad. Nutr. Diet. 2020;120:587–607. doi: 10.1016/j.jand.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 58.Khangwal I., Shukla P. Potential prebiotics and their transmission mechanisms: Recent approaches. J. Food Drug Anal. 2019;27:649–656. doi: 10.1016/j.jfda.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang L., Zhou B., Zhou X., Wang Y., Wang H., Jia S., Zhang Z., Chu C., Mu J. Combined lowering effects of rosuvastatin and L. acidophilus on cholesterol levels in rat. J. Microbiol. Biotechnol. 2019;29:473–481. doi: 10.4014/jmb.1806.06004. [DOI] [PubMed] [Google Scholar]
- 60.Lin M.Y., Chang F.J. Antioxidative effect of intestinal bacteria Bifidobacterium longum ATCC 15708 and Lactobacillus acidophilus ATCC 4356. Dig. Dis. Sci. 2000;45:1617–1622. doi: 10.1023/A:1005577330695. [DOI] [PubMed] [Google Scholar]
- 61.Wang Y., Wu Y., Wang Y., Xu H., Mei X., Yu D., Wang Y., Li W. Antioxidant properties of probiotic bacteria. Nutrients. 2017;9:521. doi: 10.3390/nu9050521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang Y., Wu Y., Wang Y., Fu A., Gong L., Li W., Li Y. Bacillus amyloliquefaciens SC06 alleviates the oxidative stress of IPEC-1 via modulating Nrf2/Keap1 signaling pathway and decreasing ROS production. Appl. Microbiol. Biotechnol. 2016;101:1–12. doi: 10.1007/s00253-016-8032-4. [DOI] [PubMed] [Google Scholar]
- 63.Harrison D., Griendling K.K., Landmesser U., Hornig B., Drexler H. Role of oxidative stress in atherosclerosis. Am. J. Cardiol. 2003;91:7–11. doi: 10.1016/S0002-9149(02)03144-2. [DOI] [PubMed] [Google Scholar]
- 64.Lee I.T., Yang C.M. Inflammatory signalings involved in airway and pulmonary diseases. Mediat. Inflamm. 2013;2013:791231. doi: 10.1155/2013/791231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gómez-Guzmán M., Toral M., Romero M., Jimenez R., Galindo P., Sanchez M., Zarzuelo M.J., Olivares M., Galvez J., Duarte J. Antihypertensive effects of probiotics Lactobacillus strains in spontaneously hypertensive rats. Mol. Nutr. Food Res. 2015;59:2326–2336. doi: 10.1002/mnfr.201500290. [DOI] [PubMed] [Google Scholar]
- 66.Belton O., Byrne D., Kearney D., Leahy A., Fitzgerald D.J. Cyclooxygenase-1 and -2-dependent prostacyclin formation in patients with atherosclerosis. Circulation. 2000;102:840–845. doi: 10.1161/01.CIR.102.8.840. [DOI] [PubMed] [Google Scholar]
- 67.Patel B., Kumar P., Banerjee R., Basu M., Pal A., Samanta M., Das S. Lactobacillus acidophilus attenuates Aeromonas hydrophila induced cytotoxicity in catla thymus macrophages by modulating oxidative stress and inflammation. Mol. Immunol. 2016;75:69–83. doi: 10.1016/j.molimm.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 68.Asemi Z., Zare Z., Shakeri H., Sabihi S.S., Esmaillzadeh A. Effect of multispecies probiotic supplements on metabolic profiles, hs-CRP, and oxidative stress in patients with type 2 diabetes. Ann. Nutr. Metab. 2013;63:1–9. doi: 10.1159/000349922. [DOI] [PubMed] [Google Scholar]
- 69.Bao Y., Wang Z., Zhang Y., Zhang J., Wang L., Dong X., Su F., Yao G., Wang S., Zhang H. Effect of Lactobacillus plantarum P-8 on lipid metabolism in hyperlipidemic rat model. Eur. J. Lipid Sci. Technol. 2012;114:1230–1236. doi: 10.1002/ejlt.201100393. [DOI] [Google Scholar]
- 70.Guarino M.P.C., Altomare A., Emerenziani S., Di Rosa C., Ribolsi M., Balestrieri P., Iovino P., Rocchi G., Cicala M. Mechanisms of Action of Prebiotics and Their Efects on Gastro-Intestinal Disorders in Adults. Nutrients. 2020;12:1037. doi: 10.3390/nu12041037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Formes H., Reinhardt C. The gut microbiota-a modulator of endothelial cell function and a contributing environmental factor to arterial thrombosis. Expert Rev. Hematol. 2019;12:541–549. doi: 10.1080/17474086.2019.1627191. [DOI] [PubMed] [Google Scholar]
- 72.Tenorio-Jimenez C., Martinez-Rmirez M.J., Tercero-Lozano M., Arraiza-Irigoyen C., Del Castillo-Codes I., Olza J., Plaza-Diaz J., Fontana L., Migueles J.H., Olivares M., et al. Evaluation of the effect of Lactobacillus reuteri V3401 on biomarkers of inflammation, cardiovascular risk and liver steatosis in obese adults with metabolic syndrome: A randomized clinical trial (PROSIR) BMC Compl. Alter. Med. 2018;18:1–8. doi: 10.1186/s12906-018-2371-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kanner J., Lapidot T. The stomach as a bioreactor: Dietary lipid peroxidation in the gastric fluid and the efects of plant-derived antioxidants. Free Radic. Biol. Med. 2001;31:1388–1395. doi: 10.1016/S0891-5849(01)00718-3. [DOI] [PubMed] [Google Scholar]
- 74.Goderska K. The antioxidant and prebiotic properties of lactobionic acid. Appl. Microbiol. Biotechnol. 2019;103:3737–3751. doi: 10.1007/s00253-019-09754-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mukherjee R., Yun J.W. Lactobionic acid reduces body weight gain in diet induced obese rats by targeted inhibition of galectin-1. Biochem. Biophys. Res. Commun. 2015;463:1311–1316. doi: 10.1016/j.bbrc.2015.06.114. [DOI] [PubMed] [Google Scholar]
- 76.Kaulpiboon J., Rudeekulthamrong P., Watanasatitarpa S., Ito K., Pongsawasdi P. Synthesis of long-chain isomaltooligosaccharides from tapioca starch and an in vitro investigation of their prebiotic properties. J. Mol. Catal. B. 2015;120:127–135. doi: 10.1016/j.molcatb.2015.07.004. [DOI] [Google Scholar]
- 77.Singh D.P., Singh J., Boparai R.K., Zhu J.H., Mantri S., Khare P., Khardori R., Kondepudi K.K., Chopra K., Bishnoi M. Isomalto-oligosaccharides, a prebiotic, functionally augment green tea e_ects against high fat diet-induced metabolic alterations via preventing gut dysbacteriosis in mice. Pharmacol. Res. 2017;123:103–113. doi: 10.1016/j.phrs.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 78.Vulevic J., Juric A., Walton G.E., Claus S.P., Tzortzis G., Toward R.E., Gibson G.R. Influence of galactooligosaccharide mixture (B-GOS) on gut microbiota, immune parameters and metabolomics in elderly persons. Br. J. Nutr. 2015;114:586–595. doi: 10.1017/S0007114515001889. [DOI] [PubMed] [Google Scholar]
- 79.Jiang J., Feng N., Zhang C., Liu F., Zhao J., Zhang H., Chen W. Lactobacillus reuteri A9 and Lactobacillus mucosae A13 isolated from Chinese superlongevity people modulate lipid metabolism in a hypercholesterolemia rat model. FEMS Microbiol. Lett. 2019;366 doi: 10.1093/femsle/fnz254. [DOI] [PubMed] [Google Scholar]
- 80.Jones M.L., Martoni C.J., Prakash S. Oral supplementation with probiotic L. reuteri NCIMB 30242 increases mean circulating 25-hydroxyvitamin D: A post hoc analysis of a randomized controlled trial. J. Clin. Endocrinol. Metab. 2013;98:2944–2951. doi: 10.1210/jc.2012-4262. [DOI] [PubMed] [Google Scholar]
- 81.Jung S., Lee Y.J., Kim M., Kim M., Kwak J.H., Lee J.W., Lee J.H. Supplementation with two probiotic strains, Lactobacillus curvatus HY7601 and Lactobacillus plantarum KY1032, reduced body adiposity and Lp-PLA 2 activity in overweight subjects. J. Func. Foods. 2015;19:744–752. doi: 10.1016/j.jff.2015.10.006. [DOI] [Google Scholar]
- 82.Asemi Z., Samimi M., Tabasi Z., Talebian P., Azarbad Z., Hydarzadeh Z., Esmaillzadeh A. Effect of daily consumption of probiotic yoghurt on lipid profiles in pregnant women: A randomized controlled clinical trial. J. Matern. Fetal. Neonatal. Med. 2012;25:1552–1556. doi: 10.3109/14767058.2011.640372. [DOI] [PubMed] [Google Scholar]
- 83.Hoppu U., Isolauri E., Koskinen P., Laitinen K. Maternal dietary counseling reduces total and LDL cholesterol postpartum. Nutrition. 2014;30:159–164. doi: 10.1016/j.nut.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 84.de Brito Alves J.L., de Oliveira Y., Carvalho N.N.C., Cavalcante R.G.S., Lira M.M.P., do Nascimento L.C.P., Magnani M., Vidal H., de Andrade Bragad V., de Souza E.L. Gut microbiota and probiotic intervention as a promising therapeutic for pregnant women with cardiometabolic disorders: Present and future directions. Pharmacol. Res. 2019;145:1–11. doi: 10.1016/j.phrs.2019.104252. [DOI] [PubMed] [Google Scholar]
- 85.Jiang J., Wu C., Zhang C., Zhao J., Yu L., Zhang H., Narbad A., Chen W., Zhai Q. Effects of probiotic supplementation on cardiovascular risk factors in hypercholesterolemia: A systematic review and meta-analysis of randomized clinical trial. J. Funct. Foods. 2020;74:104–177. doi: 10.1016/j.jff.2020.104177. [DOI] [Google Scholar]
- 86.Lew L.C., Choi S.B., Khoo B.Y., Sreenivasan S., Ong K.L., Liong M.T. Lactobacillus plantarum DR7 reduces cholesterol via phosphorylation of AMPK that down-regulated the mRNA expression of HMG-CoA reductase. Kor. J. Food Sci. Animal Res. 2018;38:350–361. doi: 10.5851/kosfa.2018.38.2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lew Nguyen T.D.T., Kang J.H., Lee M.S. Characterization of Lactobacillus plantarum PH04, a potential probiotic bacterium with cholesterol-lowering effects. Inter. J. Food Microbiol. 2007;113:358–361. doi: 10.1016/j.ijfoodmicro.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 88.Mizushima S., Ohshige K., Watanabe J., Kimura M., Kodowski T., Nakamurs Y., Tochikubo O., Ueshima H. Randomized controlled trial of sour milk on blood pressure in bordeline hypertensive men. Am. J. Hypertens. 2004;17:701–706. doi: 10.1016/j.amjhyper.2004.03.674. [DOI] [PubMed] [Google Scholar]
- 89.Matsumoto T. Potential benefits of garlic and other dietary supplements for the management of hypertension. Rev. Exp. Ther. Med. 2020;19:1479–1484. doi: 10.3892/etm.2019.8375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schreiber O., Petersson J., Phillipson M., Perry M., Ross S., Holm L. Lactobacillus reuteri prevents colitis by reducing P-selectin-associated leukocyte- and platelet-endothelial cell interactions. Am. J. Physiol. Gastrointest. Liver Physiol. 2009;296:534–542. doi: 10.1152/ajpgi.90470.2008. [DOI] [PubMed] [Google Scholar]
- 91.Haro C., Medina M. Lactobacillus casei CRL 431 improves endothelial and platelet functionality in a pneumococcal infection model. Benef. Microbes. 2019;10:533–541. doi: 10.3920/BM2018.0099. [DOI] [PubMed] [Google Scholar]
- 92.Parnell J.A., Reimer R.A. Effect of prebiotic fibre supplementation on hepatic gene expression and serum lipids: A dose-response study in JCR:LA-cp rats. Br. J. Nutr. 2010;103:1177–1184. doi: 10.1017/S0007114509993539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hume M.P., Nicolucci A.C., Reimer R.A. Prebiotic supplementation improves appetite control in children with overweight and obesity: A randomized controlled trial. Am. J. Clin. Nutr. 2017;105:790–799. doi: 10.3945/ajcn.116.140947. [DOI] [PubMed] [Google Scholar]
- 94.Nicolucci A.C., Hume M.P., Martinez I., Mayengbam S., Walter J., Reimer R.A. Prebiotics reduce body fat and alter intestinal microbiota in children who are overweight or with obesity. Gastroenterology. 2017;153:711–722. doi: 10.1053/j.gastro.2017.05.055. [DOI] [PubMed] [Google Scholar]
- 95.Kim B., Choi H.N., Yim J.E. Effect of diet on the gut microbiota associated with obesity. J. Obesity Metab. Synd. 2019;28:216–224. doi: 10.7570/jomes.2019.28.4.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mofid V., Izadi A., Majtehedi S.Y., Khemoat L. Therapeutic and nutritional effects of synbiotic yogurts in children and adults: A clinical review. Probiotics Antimicrob. Proteins. 2019;10:1–17. doi: 10.1007/s12602-019-09594-x. [DOI] [PubMed] [Google Scholar]
- 97.Liong M.T., Dunshea F.R., Shah N.P. Effects of a symbiotic containing Lactobacillus acidophilus ATCC 4962 on plasma lipid profiles and morphology of erythrocytes in hypercholesterolemic pigs on high- and low-fat diets. Br. J. Nutr. 2007;98:736–744. doi: 10.1017/S0007114507747803. [DOI] [PubMed] [Google Scholar]
- 98.Haghighat N., Mohammadshahi M., Shayanpour S., Haghighizadeh M.H. Effect of symbiotic and probiotic supplementation on serum levels of endothelial cell adhesion molecules in hemodialysis patients: A randomized control study. Probiotics Antimicro. Proteins. 2018;1:1–9. doi: 10.1007/s12602-018-9477-9. [DOI] [PubMed] [Google Scholar]