Abstract
Timely postpartum care is associated with lower maternal morbidity and mortality, yet fewer than half of Medicaid beneficiaries attend a postpartum visit. Medicaid enrollees are at higher risk of postpartum disruptions in insurance because pregnancy-related Medicaid eligibility ends sixty days after delivery. We used Medicaid claims data for 2013–15 from Colorado, which expanded Medicaid under the Affordable Care Act, and Utah, which did not. We found that after expansion, new mothers in Utah experienced higher rates of Medicaid coverage loss and accessed fewer Medicaid-financed outpatient visits during the six months postpartum, relative to their counterparts in Colorado. The effects of Medicaid expansion on postpartum Medicaid enrollment and outpatient utilization were largest among women who experienced significant maternal morbidity at delivery. These findings provide evidence that expansion may promote the stability of postpartum coverage and increase the use of postpartum outpatient care in the Medicaid program.
The United States has the highest maternal mortality rate in the developed world.1 Maternal morbidity and mortality occur at higher rates among low-income women in minority racial/ethnic groups, who also disproportionately receive maternity care through the Medicaid program.2,3 Although one-third of pregnancy-related mortality in the US occurs after delivery,4 only 40 percent of women enrolled in Medicaid receive a postpartum follow-up visit.5 Women who do not receive postpartum care are at higher risk for undiagnosed complications of pregnancy, delayed initiation of contraception, and unaddressed infant care issues.6,7
Medicaid eligibility criteria create barriers to accessing postpartum care. Under current Medicaid policy, pregnant women are eligible for Medicaid coverage from conception through sixty days after delivery. After that time, women can remain enrolled in Medicaid only if they qualify for parental Medicaid coverage. Income thresholds for that coverage vary by state but are considerably lower than those for pregnancy coverage, particularly in states that did not expand eligibility for Medicaid coverage under the Affordable Care Act (ACA). As of June 2018, among the seventeen states that did not expand Medicaid, the median parental income cutoff was 43 percent of the federal poverty level, and the median pregnancy income cutoff was 200 percent of poverty.8 This eligibility cliff between pregnancy and parental coverage can lead to gaps in insurance coverage. Jamie Daw and co-authors found that before the ACA, 55 percent of women enrolled in Medicaid or the Children’s Health Insurance Program (CHIP) at the time of delivery experienced at least one month without insurance during the ensuing six months postpartum.9 The time-limited nature of pregnancy-related Medicaid coverage, combined with the risk of insurance loss after delivery, imposes barriers for new mothers and their care providers to achieve high-quality postpartum care.
The ACA gave states the option to expand eligibility for their Medicaid programs to all adults with incomes below 138 percent of poverty. In states where parental eligibility falls below pregnancy eligibility, Medicaid expansion narrows the eligibility gap between pregnancy coverage and parental coverage, which potentially improves the continuity of postpartum insurance coverage and access to care.
In this study we evaluated whether Medicaid expansion increased the duration of postpartum Medicaid enrollment and timely use of outpatient care. We compared Medicaid coverage and the use of outpatient care before and after Medicaid expansion, using rich Medicaid claims data from two states: Colorado, a state that expanded Medicaid, and Utah, a neighboring state that did not. Using a difference-in-differences framework, we assessed whether increasing Medicaid eligibility for low-income adults improves postpartum coverage and timely access to postpartum care among pregnant women.
Study Data And Methods
DATA AND SETTING
In Colorado in 2013, pregnant women with incomes below 185 percent of poverty and parents with incomes below 105 percent of poverty were eligible for Medicaid. In Utah in 2013, pregnant women with incomes below 133 percent of poverty and parents with incomes below 44 percent of poverty were eligible for Medicaid. On January 1, 2014, Colorado expanded its Medicaid program to cover all low-income adults with incomes up to 138 percent of poverty. In Utah, income eligibility for parents and pregnant women remained stable aside from the 2014 introduction of the modified adjusted gross income (MAGI) Medicaid eligibility requirements.10
Through data-use agreements with state agencies in Colorado and Utah, we acquired Medicaid claims that were part of all-payer claims databases. The Colorado database collects fee-for-service and managed care claims from the state Medicaid program, and the Utah database collects fee-for-service claims and 90 percent of managed care claims. These data sets are described in greater detail elsewhere.11 Our analyses used inpatient claims to identify dates of delivery and outpatient claims to identify outpatient visits during the postpartum period. We used enrollment files to determine whether beneficiaries were enrolled in Medicaid in a given month. Enrollment information was recorded regardless of whether health services were used.
STUDY SAMPLE
The study sample consisted of live births paid for by Medicaid that occurred in the period January 2013-June 2015 among women ages nineteen and older in Colorado and Utah. Deliveries were identified using International Classification of Diseases, Ninth Revision (ICD-9), and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), codes (see online appendix A for a list of the codes used to identify deliveries).12 Our unit of analysis was the delivery. Medicaid coverage and outpatient use were assessed over the six months after delivery to capture enrollment as women transitioned out of the postpartum period. Because the six-month postpartum periods after deliveries occurring during July-December 2013 overlapped with the date of Colorado’s Medicaid expansion on January 1, 2014, we treated deliveries that occurred during this window as transitional. The study sample included 25,805 deliveries from 24,528 women in Utah and 44,647 deliveries from 42,144 women in Colorado.
VARIABLES
Our primary outcomes included Medicaid enrollment and outpatient visits over a six-month postpartum period. We measured postpartum Medicaid coverage by counting the number of months between the date of delivery and either the last day of Medicaid enrollment or the six-month mark, whichever occurred first. We selected a six-month follow-up period to capture the full postpartum period.13 This approach captures the critical transition points when pregnancy-related Medicaid coverage expires at sixty days and when care transitions from postpartum to well woman at six to twelve weeks after delivery. The approach was aligns with the American College of Obstetricians and Gynecologists’ 2018 updated recommendations that emphasize continuous care throughout the “fourth trimester.”5,14
We assessed the use of outpatient care by counting all unique Medicaid encounters, excluding emergency department, lab, and inpatient claims. We defined outpatient care broadly, to capture both postpartum care and visits that occurred after linkage to primary care.15
Given the importance of the timing of care during the postpartum period, we counted the number of outpatient visits occurring 0–30, 31–60,61–90, and 91–120 days after delivery. We also conducted stratified analyses by whether women experienced severe maternal morbidity, such as hemorrhage, acute myocardial infarction, or sepsis, defined using ICD-9 and ICD-10 codes present on the date of delivery.
We tested whether outcome trends in Colorado and Utah evolved similarly before the policy change. This test provided evidence that the difference-in-differences estimates captured the effect of Medicaid expansion and not that of differential trends before expansion. As shown in appendix exhibits C1–3, outcome trends did not differ significantly between the two states during the first six months of 2013, and a test simulating a placebo policy that took effect in July 2013 showed no significant differences between the states in our outcomes before 2014.12
We included a categorical age variable and an indicator variable for month of delivery in all adjusted difference-in-differences models. We also included area-level fixed effects to control for time-invariant differences between geographic regions. The unit of the area-level fixed effects was the ZIP code area in Colorado and the Small Health Statistical Area in Utah, a geographic measure computed by the Office of Health Care Statistics at the Utah Department of Health that aggregates neighboring sparsely populated ZIP codes into Statistical Areas to reduce the risk of identifying individuals living in rural areas.16 We assigned women to the category “missing” if their claims lacked area-level information. Geographic information was missing for less than 3 percent of women in both states.
ANALYSIS
We estimated multivariate linear regression models for the continuous outcomes of number of months of coverage and number of office visits in the six months after delivery. Each regression included an indicator variable for state, corresponding to whether enrollees lived in Colorado or Utah, and an indicator variable that identified prepolicy deliveries (January-June 2013), transitional deliveries (July-December 2013), and postpolicy deliveries (January 2014-June 2015). Models also included an interaction term between the state and postpolicy variables, which corresponded to the mean difference in the outcomes between Colorado and Utah before and after Medicaid expansion in Colorado. Models adjusted for age, month of delivery, and area-level fixed effects. We tested the significance of a triple interaction between state, Medicaid expansion period, and the presence of severe maternal morbidity using a fully interacted model (see appendix D for a list of conditions and appendix F for full regression equations).12
In our primary models we clustered Huber-White robust standard errors at the state level and obtained t-distributions with one degree of freedom, following the work of A. Colin Cameron and Douglas Miller17 and of John Pepper18 (see appendix G for an alternative approach to estimating the standard errors).12
As a sensitivity analysis we examined whether new mothers used commercial insurance-financed outpatient care during the six months postpartum and tested difference-in-differences estimates of the effect of expansion on commercially financed outpatient visits and a combined measure of both Medicaid-financed and commercially financed visits.
LIMITATIONS
Our study had several limitations. First, our analysis included only two states, which could limit the generalizability of our results. However, Colorado and Utah have similarities to several other states considering expansion, and Utah is in the process of implementing a Medicaid coverage expansion after the passage of a ballot initiative in November 2018.
Second, the all-payer claims databases lacked detailed information on race, ethnicity, and socioeconomic status. To account for geographic variation in these variables, we included area-level fixed effects in all adjusted models. Given the well-documented health disparities in maternal mortality, future work should examine the effects of expansion on different racial/ethnic groups. Furthermore, results should be considered in the context that on average, Medicaid populations in Utah and Colorado have lower proportions of black women and higher proportions of Hispanic women, compared to other states and the national average.3
Third, we could not rule out the possibility of differential prepolicy outcome trends, as we were limited to one year of prepolicy data.
Finally, our primary utilization outcome was outpatient visits financed by Medicaid. To assess whether women used postpartum care paid for by other types of insurance, we leveraged our multipayer state data to measure commercially financed postpartum visits. However, because the all-payer claims databases excluded approximately 30 percent of all commercial insurers, we could not rule out the possibility that rates of commercially financed postpartum care may be biased. For example, estimates may be biased downward if women enrolled in observable commercial plans have fewer postpartum health needs compared to women enrolled in unobservable self-funded commercial plans.
Study Results
POSTPARTUM MEDICAID COVERAGE
The age distribution of the women in our sample did not differ significantly between Colorado and Utah (p = 0.311) (exhibit 1). Although we found a small increase in Medicaid-financed deliveries in Colorado after expansion (appendix exhibit E1),12 the characteristics of women in the two states who delivered before and after Medicaid expansion in Colorado were similar (see appendix E for a comparison of the women who delivered before and after expansion).12
EXIBIT 1.
Descriptive statistics of women with Medicaid-financed deliveries in Colorado and Utah, January 2013-June 2015
| Colorado | Utah | |
|---|---|---|
| No. of women | 42,144 | 24,528 |
| No. of deliveries | 44,647 | 25,805 |
| Age (years) | ||
| 19–24 | 41.2% | 40.9% |
| 25–39 | 57.1 | 57.4 |
| 40–53 | 1.8 | 1.6 |
SOURCE Authors ‘analysis of data for 2013–15 from all-payer claims databases in Colorado and Utah.
Exhibit 2 presents adjusted difference-in-differences estimates of the effect of Medicaid expansion on postpartum Medicaid coverage, controlling for age, month of delivery, and area-level fixed effects. After expansion in Colorado, the difference in postpartum Medicaid coverage between the two states was 0.9 months of coverage over six months of follow-up. This difference is indicative of a preservation of coverage in Colorado compared to an erosion of postpartum Medicaid enrollment in Utah.
EXHIBIT 2.
Mean changes in Medicaid-financed postpartum coverage and utilization in Colorado and Utah before and after the expansion of eligibility for Medicaid in Colorado
| Colorado | Utah | Adjusted difference-in-differences | |||||
|---|---|---|---|---|---|---|---|
| January-June 2013 | After January 2014a | Change | January-June 2013 | After January 2014a | Change | ||
| NO. OF MONTHS OF COVERAGE IN 6 MONTHS AFTER DELIVERY | |||||||
| All women Women with severe | 5.3 | 5.4 | 0.1 | 4.6 | 3.6 | −1.0 | 0.90*** |
| maternal morbidity | 5.3 | 5.2 | −0.1 | 4.7 | 3.2 | −1.5 | 1.40** |
| NO. OF OUTPATIENT VISITS IN 6 MONTHS AFTER DELIVERY | |||||||
| All women Women with severe | 3.0 | 3.3 | 0.3 | 2.0 | 1.8 | −.0.2 | 0.52*** |
| maternal morbidity | 2.7 | 3.4 | 0.7 | 1.8 | 1.6 | −0.2 | 1.25*** |
| NO. OF OUTPATIENT VISITS (DAYS AFTER DELIVERY) | |||||||
| 0–30 days | 1.40 | 1.38 | 0.01 | 0.73 | 0.70 | −0.02 | 0.00 |
| 31–60 days | 0.77 | 0.73 | 0.04 | 0.88 | 0.67 | −0.21 | 0.19*** |
| 61–90 days | 0.44 | 0.49 | 0.05 | 0.32 | 0.27 | −0.05 | 0.10**** |
| 91–120 days | 0.34 | 0.42 | 0.08 | 0.13 | 0.13 | −0.00 | 0.08*** |
SOURCE Authors’ analysis of 2013–15 all-payer claims databases in Colorado and Utah. NOTES All models adjusted for age, month of delivery, and area-level fixed effects. Severe maternal morbidity is explained in the text.
Date of Medicaid expansion in Colorado. Transition period of July-December 2013 is not shown; see the text for details.
p < 0.05
p< 0.0.01
p< 0.001
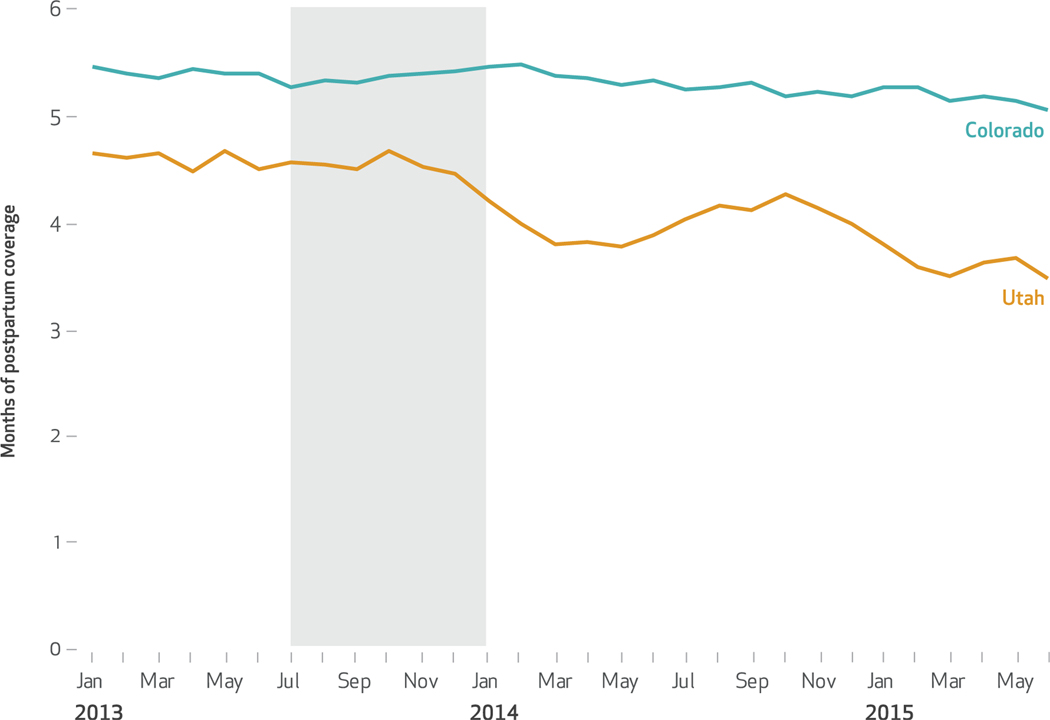
Exhibit 3 plots the mean number of months of postpartum Medicaid coverage in Colorado and Utah from January 2013 to June 2015. Trends in Medicaid enrollment were stable in both states during the first six months of 2013 (p = 0.637) but diverged after January 2014.Women in Utah experienced a decline in postpartum coverage in 2014 and 2015, while postpartum coverage durations remained relatively unchanged in Colorado. Coverage retention was significantly greater among women who experienced severe maternal morbidity at the time of their delivery. Relative to Utah, Colorado’s expansion was associated with 1.4 months of postpartum coverage among women with severe maternal morbidity and 0.9 months of postpartum coverage among women without severe maternal morbidity (triple-difference comparing women with severe maternal morbidity to women without in Colorado versus Utah, before and after expansion: 0.52; p = 0.030) (exhibit 2).
EXHIBIT 3.
Mean number of months of postpartum Medicaid coverage in the six months after delivery in Colorado and Utah, January 2013-June 2015
SOURCE Authors’ analysis of data for 2013–15 from all-payer claims databases in Colorado and Utah. NOTES The shaded area highlights deliveries occurring during July-December 2013. These deliveries were treated as transitional in our models because the six-month postpartum periods for deliveries occurring during July-December 2013 extended beyond the date of Colorado’s Medicaid expansion on January 1, 2014. In a test for difference of January-June 2013 trends across states, β = −0.00 and p = 0.637.
USE OF OUTPATIENT POSTPARTUM CARE IN MEDICAID
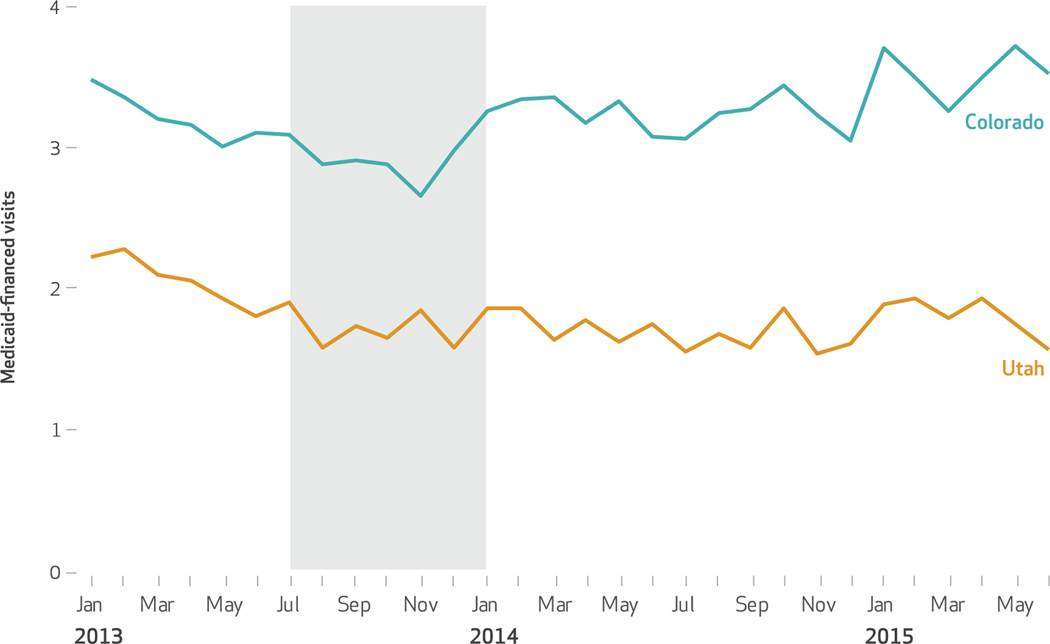
Exhibit 4 plots the mean number of postpartum outpatient visits from January 2013 to June 2015. Before expansion, the mean number of such visits in Medicaid was higher in Colorado than in Utah. Trends from January to June did not differ significantly between the two states (p = 0.243). After expansion, the number of visits increased in Colorado and decreased in Utah, resulting in a 17.3 percent increase in outpatient utilization relative to the baseline rate in Colorado, or 0.52 additional Medicaid-financed visits in the six months after delivery, compared to women in Utah (exhibit 2). Utilization increases were significantly greater among women who experienced severe maternal morbidity at the time of their deliveries. Among these women, Colorado’s expansion was associated with 1.3 Medicaid-financed postpartum outpatient visits compared to 0.5 visits among women without severe maternal morbidity, a relative increase of 46.3 percent from Colorado’s baseline mean (triple-difference: 0.76; p = 0.024).
Exhibit 4.
Mean number of Medicaid-financed outpatient visits in the six months after delivery in Colorado and Utah, January 2013-June 2015
SOURCE Authors’ analysis of data for 2013–15 from all-payer claims databases in Colorado and Utah. NOTES The shaded area highlights deliveries occurring during July–December 2013. These deliveries were treated as transitional in our models because the six-month postpartum periods for deliveries occurring during July–December 2013 extended beyond the date of Colorado’s Medicaid expansion on January 1, 2014. In a test for difference of January–June 2013 trends across states, β = −0.00 and p = 0.243.
We also examined the number of visits that occurred 0–120 days after delivery. The largest gains in Colorado compared to Utah were concentrated among visits that occurred 31–60 or 61–90 days after delivery (difference-in-differences estimates: 0.19 and 0.10, respectively), the period that coincides with the transition from Medicaid pregnancy eligibility to parental eligibility (exhibit 2).
In sensitivity analyses we found higher numbers of postpartum outpatient visits financed by commercial insurers among new mothers in Utah compared to those in Colorado over all three follow-up years (see appendix exhibit H1).12 We also found a small increase in commercially financed outpatient postpartum utilization in Utah relative to Colorado after expansion (difference-in-differences estimate: −0.03; p = 0.012), which represented approximately 5 percent of the effect of expansion on Medicaid-financed postpartum visits. Including the commercially financed postpartum outpatient visits (from the plans available in the all-payer claims databases) in the utilization outcome resulted in a slight attenuation of the effect of expansion. The point estimate decreased from 0.52 for Medicaid-financed visits only to 0.49 for all visits combined (p value for Medicaid and commercial utilization combined: 0.001). See appendix exhibit H for full results.12
Discussion
In this two-state claims-based analysis of the effect of Medicaid expansion on postpartum Medicaid coverage and use of postpartum outpatient care, women who lived in the expansion state of Colorado experienced improved coverage stability relative to women who lived in Utah, a neighboring state that did not expand Medicaid during the study period. We also found greater use of Medicaid-financed outpatient care in Colorado during the postpartum period. Outpatient utilization increased significantly in Colorado compared to Utah across all four postpartum months we examined, with the largest increases 31–90 days after delivery—the period when new mothers transition from pregnancy to parental Medicaid coverage and are at the highest risk of losing coverage. While Medicaid expansion under the ACA was originally intended to close a coverage gap by extending coverage to low-income childless adults regardless of categorical eligibility, our findings demonstrate that expansion has important benefits for pregnant women, a vulnerable group that has been categorically eligible for Medicaid coverage since the program’s inception.
Our study found larger effects of Medicaid expansion among women who experienced severe maternal morbidity. After expansion, Colorado women who experienced severe morbidity during their deliveries had nearly 50 percent more postpartum Medicaid-financed outpatient visits compared to women with similarly complicated deliveries in Utah. Postpartum visits offer critical opportunities to assess the well-being of mothers and monitor adverse pregnancy-related conditions, particularly among those at greater risk of postpartum morbidity. These findings suggest that utilization gains are concentrated among a high-risk population.19
To our knowledge, this is the first study to examine the impact of the ACA’s Medicaid expansion on postpartum coverage and outpatient utilization among pregnant women. Laura Wherry found that pre-ACA parental coverage expansions improved insurance coverage during the prenatal period among women who were already mothers.20 Our study builds on this prior work by using longitudinal administrative claims data from after the implementation of the ACA, employing a two-state quasi-experimental study design, and assessing both coverage measures and corresponding use of outpatient care during the postpartum period.21
Differences in postpartum Medicaid enrollment appear to be driven by declines in coverage after 2014 in Utah (a nonexpansion state) rather than by increases in coverage in Colorado (an expansion state). One reason why we observed declining Medicaid coverage rates in Utah after 2013 maybe because new mothers with incomes of 100–138 percent of poverty transitioned to Marketplace coverage earlier in the postpartum period, and the expansion in Colorado protected new mothers from having to do so. This interpretation raises the question of whether new mothers in Utah who lost their Medicaid coverage after delivery were able to access similar levels of outpatient care financed by other insurance, such as a plan obtained through the Marketplace. We found suggestive evidence that this was not the case. After expansion, women in Utah did not use commercially financed outpatient postpartum care at the same rates as women in Colorado used Medicaid-financed outpatient care.
One possible reason we did not observe sub-stitution in postpartum outpatient care via Utah’s private market is that mothers with incomes below 100 percent of poverty are ineligible for subsidized Marketplace coverage. Even if women are eligible for an alternative source of postpartum health insurance, transitions from Medicaid to other commercial coverage may still disrupt continuity of care. Prior work has demonstrated that even seamless transitions between health insurers can have negative effects on health.22 Work by Daw and co-authors indicated that over half of Medicaid-enrolled women experience coverage lapses during postpartum coverage transitions, and even without a gap in insurance, the process of accessing care in a new plan may impose barriers that deter utilization.9
There are also several potential reasons why coverage and utilization changes might have been attenuated in this two-state comparison. First, we could not identify women who qualified for pre-ACA coverage via disability or parental eligibility. The inclusion of these women may have offset coverage gains in Colorado, since they were likely to retain their coverage regardless of expansion. Second, new mothers in Colorado experienced only a modest increase in income eligibility (from 105 percent to 138 percent of poverty), which suggests that postpartum coverage retention and use of outpatient care could be greater in Utah as well as other nonexpansion states if they expanded Medicaid.
Third, when Colorado expanded Medicaid, the state invested in Medicaid infrastructure and outreach that may have assisted new mothers in understanding and retaining their coverage. A lack of awareness of coverage in Utah could have resulted in lower postpartum outpatient utilization. Finally, the magnitude of the results may have been limited by high postpartum coverage rates in Colorado before expansion and by provider supply limitations in rural areas of both states.
Our study suggests that narrowing the gap between pregnancy and parental Medicaid eligibility requirements could improve stability of coverage and use of postpartum care. However, more than 400,000 new mothers remained un-insured in 2016, two years after the ACA’s coverage expansions.21 This is in part because in all states an income gap remains between the state’s pregnancy eligibility cutoff and either the parental coverage threshold in nonexpansion states or the 138 percent of poverty income limit in expansion states.
While Medicaid expansion is an important policy option to mitigate coverage loss after delivery, many women will still experience insurance disruptions during the postpartum period. American College of Obstetricians and Gynecologists guidelines for postpartum care explicitly state that insurance coverage policies should be aligned with ongoing and sustained postpartum care.5 Expanding the postpartum Medicaid coverage window beyond sixty days reduces pressure on providers to tailor their care to insurance policies rather than patients’ needs. Prior research suggests that Medicaid eligibility policies impede providers’ ability to deliver adequate postpartum care.23 Other policy options to address postpartum coverage disruptions include extending Medicaid pregnancy eligibility to twelve months after delivery, increasing parental income eligibility limits to match pregnancy income eligibility limits, and providing care co-ordination services to facilitate new mothers’ insurance transitions. The Mothers and Off-spring Mortality and Morbidity Awareness Act (MOMMA’s Act), a bill to extend national postpartum coverage policy to twelve months, was introduced in the House of Representatives in June 2018, but the measure has not progressed. State-level twelve-month continuous eligibility policies for Medicaid-eligible adults would also assist pregnant women in maintaining insurance after delivery.
Conclusion
We found that Medicaid expansion in Colorado was associated with improved postpartum Medicaid coverage and increased use of Medicaid-financed postpartum outpatient care. These findings have implications for other states considering expansion and also represent an important step toward reducing rates of maternal morbidity and mortality in the United States.
Supplementary Material
Our study found larger effects of Medicaid expansion among women who experienced severe maternal morbidity.
Acknowledgments
This project was funded under Grant No. R36 HS025560–01 to Sarah Gordon from the Agency for Healthcare Research and Quality (AHRQ), Department of Health and Human Services. The opinions expressed in this document are those of the authors and do not reflect the official position of AHRQ, the Department of Health and Human Services, the Department of Veterans Affairs, or the US government. The authors thank the Colorado Center for Improving Value in Health Care and the Utah Department of Health for their valuable data assistance and Omar Galarraga for his feedback on this study.
Contributor Information
Sarah H. Gordon, Department of Health Law, Policy, and Management, Boston University School of Public Health, in Massachusetts..
Benjamin D. Sommers, Department of Health Policy and Management, Harvard T. H. Chan School of Public Health, and a professor of medicine at Brigham and Women’s Hospital, both in Boston..
Ira B. Wilson, Department of Health Services, Policy, and Practice, Brown University School of Public Health, in Providence, Rhode Island..
Amal N. Trivedi, Department of Health Services, Policy, and Practice, Brown University School of Public Health, and a research investigator at the Providence Veterans Affairs Medical Center..
NOTES
- 1.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, Shackelford KA, Steiner C, Heuton KR, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9947): 980–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howell EM. The impact of the Medicaid expansions for pregnant women: a synthesis of the evidence. Med Care Res Rev. 2001;58(1):3–30. [DOI] [PubMed] [Google Scholar]
- 3.Henry J Kaiser Family Foundation. Distribution of the nonelderly with Medicaid by race/ethnicity [Internet]. San Francisco (CA): KFF; 2017. [cited 2019 Nov 22]. Available from: https://www.kff.org/medicaid/state-indicator/distribution-by-raceethnicity-4/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D [Google Scholar]
- 4.Centers for Disease Control and Prevention. Pregnancy-related deaths [Internet]. Atlanta (GA): CDC; 2019. [cited 2019 Dec 5]. Available from: https://www.cdc.gov/vitalsigns/maternal-deaths/ [Google Scholar]
- 5.American College of Obstetricians and Gynecologists. Optimizing postpartum care [Internet]. Washington (DC): ACOG; 2018. May [cited 2019 Nov 22]. (ACOG Committee Opinion No. 736). Available from: http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Optimizing-Postpartum-Care [Google Scholar]
- 6.Banti S, Mauri M, Oppo A, Borri C, Rambelli C, Ramacciotti D, et al. From the third month of pregnancy to 1 year postpartum. Prevalence, incidence, recurrence, and new onset of depression. Results from the Perinatal Depression—Research & Screening Unit study. Compr Psychiatry. 2011;52(4):343–51. [DOI] [PubMed] [Google Scholar]
- 7.Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295(15):1809–23. [DOI] [PubMed] [Google Scholar]
- 8.Henry J Kaiser Family Foundation. Medicaid and CHIP income eligibility limits for pregnant women, 2003–2019 [Internet]. San Francisco (CA): KFF; 2019. [cited 2019 Nov 6]. Available from: https://www.kfforg/medicaid/state-indicator/medicaid-and-chip-income-eligibility-limits-for-pregnant-women/ [Google Scholar]
- 9.Daw JR, Hatfield LA, Swartz K, Sommers BD. Women in the United States experience high rates of coverage “churn” in months before and after childbirth. Health Aff (Millwood). 2017;36(4):598–606. [DOI] [PubMed] [Google Scholar]
- 10.Utah Department of Health. Medicaid: annual reports 2013–2015 [Internet]. Salt Lake City (UT): The Department; [cited 2019 Nov 6]. Available from: https://medicaid.utah.gov/annual-reports [Google Scholar]
- 11.Gordon SH, Sommers BD, Wilson I, Galarraga O, Trivedi AN. The impact of Medicaid expansion on continuous enrollment: a two-state analysis. J Gen Intern Med. 2019;34(9): 1919–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.To access the appendix, click on the Details tab of the article online.
- 13.Tulman L, Fawcett J. Recovery from childbirth: looking back 6 months after delivery. Health Care Women Int. 1991;12(3):341–50. [DOI] [PubMed] [Google Scholar]
- 14.Tully KP, Stuebe AM, Verbiest SB. The fourth trimester: a critical transition period with unmet maternal health needs. Am J Obstet Gynecol. 2017;217(1):37–41. [DOI] [PubMed] [Google Scholar]
- 15.National Committee for Quality Assurance. Prenatal and postpartum care (PPC) [Internet]. Washington (DC): NCQA; c 2019. [cited 2019 Nov 6]. Available from: https://www.ncqa.org/hedis/measures/prenatal-and-postpartum-care-ppc/ [Google Scholar]
- 16.Utah Department of Health. Small Health Area ZIP Code Crosswalk. Salt Lake City (UT): The Department; updated 2014 Jun. [Google Scholar]
- 17.Cameron AC, Miller DL. A practitioner’s guide to cluster-robust inference. J Hum Resour. 2015;50(2): 317–72. [Google Scholar]
- 18.Pepper JV. Robust inferences from random clustered samples: an application using data from the Panel Study of Income Dynamics. Econ Lett. 2002;75(3):341–5. [Google Scholar]
- 19.Blenning CE, Paladine H. An approach to the postpartum office visit. Am Fam Physician. 2005;72(12): 2491–6. [PubMed] [Google Scholar]
- 20.Wherry LR. State Medicaid expansions for parents led to increased coverage and prenatal care utilization among pregnant mothers. Health Serv Res. 2018;53(5): 3569–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McMorrow S, Kenney G. Despite progress under the ACA, many new mothers lack insurance coverage. Health Affairs Blog [blog on the Internet]. 2018. September 19 [cited 2019 Nov 7]. Available from: http://www.healthaffairs.org/do/10.1377/hblog20180917.317923/full/ [Google Scholar]
- 22.Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. 2018;8(6): e021161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gordon SH, Gadbois EA, Shield RR, Vivier PM, Ndumele CD, Trivedi AN. Qualitative perspectives of primary care providers who treat Medicaid managed care patients. BMC Health Serv Res. 2018;18(1):728. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.