Abstract
Point-of-care lung ultrasound (LUS) is an attractive alternative to chest X-ray (CXR), but its diagnostic accuracy compared to CXR has not been well studied in coronavirus disease 2019 (COVID-19) patients. We conducted a prospective observational study to assess the correlation between LUS and CXR findings in COVID-19 patients. Ninety-six patients with a clinical diagnosis of COVID-19 underwent an LUS exam and CXR upon presentation. Physicians blinded to the CXR findings performed all LUS exams. Detection of pulmonary infiltrates by CXR versus LUS was compared between patients categorized as suspected or confirmed COVID-19 based on reverse transcriptase-polymerase chain reaction. Sensitivities and correlation by Kappa statistic were calculated between LUS and CXR. LUS detected pulmonary infiltrates more often than CXR in both suspected and confirmed COVID-19 subjects. The most common LUS abnormalities were discrete B-lines, confluent B-lines, and small subpleural consolidations. Most important, LUS detected unilateral or bilateral pulmonary infiltrates in 55% of subjects with a normal CXR. Substantial agreement was demonstrated between LUS and CXR for normal, unilateral or bilateral findings (Κ = 0.48 (95% CI 0.34 to 0.63)). In patients with suspected or confirmed COVID-19, LUS detected pulmonary infiltrates more often than CXR, including more than half of the patients with a normal CXR.
Keywords: ultrasound, imaging, X-ray, chest, diagnosis, SARS
1. Introduction
Diagnosing coronavirus disease 2019 (COVID-19), the disease caused by the novel coronavirus SARS-CoV2, has been a major challenge as the pandemic has spread rapidly across the globe. Most patients present with nonspecific symptoms, including fever, cough, dyspnea, myalgias, and headache [1], that are indistinguishable from other respiratory infections. To confirm the disease in suspected patients, clinicians most often order reverse transcriptase-polymerase chain reaction (PCR) testing, but PCR testing has limited availability, relatively high false negative rates early in the course of the disease, and a delay of a few hours to days for results to be obtained [2,3].
Diagnostic imaging is being used to support a diagnosis of COVID-19 by detection of pulmonary infiltrates in suspected patients. Chest computed tomography (CT) scans have demonstrated superior diagnostic sensitivity for detecting pulmonary infiltrates in COVID-19 compared to chest X-ray (CXR) with reported sensitivity of 97–98% after 6 days of symptoms [2,3,4,5]. Though sensitive for pulmonary infiltrates, obtaining chest CT scans in all suspected COVID-19 patients is impracticable due to limited access to CT scanners worldwide and infection control requirements for disinfecting CT scanners. The American College of Radiology has recommended against routine use of CT scans for evaluating patients with suspected COVID-19 [6]. For these reasons, CXR and lung ultrasound (LUS) have been the primary imaging modalities used in the diagnosis of COVID-19 worldwide. CXRs can be obtained rapidly with minimal radiation exposure to patients, but have low sensitivity (46–69%) for detecting pulmonary infiltrates in COVID-19 patients [7,8].
Lung ultrasound (LUS) is an attractive alternative to CXRs and CT scans in COVID-19. Point-of-care or bedside LUS has several unique advantages in COVID-19, including immediate availability of findings to guide clinical decision-making, availability of portable ultrasound devices in austere settings such as field hospitals, repeatability to monitor patients serially, and ease of machine decontamination. Studies in non-COVID-19 patients have shown LUS has superior sensitivity (95% (95% CI 92–96%) vs. 49% (40–58%)) and similar specificity (94% (CI 90–97%) vs. 92% (CI 86–95%)) compared to CXRs when using chest CT scan as the gold standard [9]. Several recent studies have described lung ultrasound patterns in COVID-19 [10,11,12,13,14,15,16], but few studies have compared the diagnostic accuracy of LUS versus CXR for identifying lung abnormalities [17,18]. The objective of this study was to assess the correlation of LUS and CXR for detecting pulmonary infiltrates in COVID-19 patients.
2. Materials and Methods
2.1. The Study Design and Subjects
A prospective observational study of consecutive patients presenting with a clinical diagnosis of COVID-19 during the first COVID-19 surge in Spain was conducted from March 18, 2020 to April 5, 2020. The setting was an emergency department of a 247-bed university-affiliated teaching hospital in Madrid, Spain. Subjects were eligible for enrolment if they were an adult (age >18 years) and had a clinical diagnosis of COVID-19 based on classic symptoms of COVID-19 (fever, chills, cough, shortness of breath, sore throat, headache, myalgias, anosmia, ageusia, or diarrhea), close contact with an individual with active COVID-19, and abnormal laboratory findings (lymphopenia, elevated c-reactive protein, lactate dehydrogenase, D-dimer, and liver transaminases).
During the first surge of the COVID-19 pandemic in Spain in March of 2020, SARS-CoV-2 PCR testing had limited availability, and test results were delayed by 24–72 h. PCR test results of study subjects were not known at the time of study enrolment. During data analysis, subjects were categorized as having “confirmed” COVID-19 defined by a positive PCR test result or “suspected” COVID-19 defined by either a negative PCR test result or nonperformance of PCR testing.
After informing subjects about the study objectives and minimal risks, verbal consent was obtained and documented in the electronic medical record. Written consent using paper was not feasible due to the risk of fomite transmission of SARS-CoV-2 to study personnel. This study complied with the Declaration of Helsinki and was approved by the local ethics committee and hospital research committee (PI 64/20).
2.2. Lung Ultrasound Exam
A bedside LUS exam was performed on each subject by one of two physicians with expertise in point-of-care ultrasound (M.M.G., F.J.T.M.). Both physician sonographers performed an LUS exam on all subjects who were clinically diagnosed with COVID-19 by an attending physician in the emergency department. The LUS exam was performed independent of the evaluation by the attending physician in the emergency department. Both physician sonographers were blinded to each patient’s history, laboratory results, and radiographic images and were not directly involved in the patient’s care. PCR test results were not available until 24–72 h after presentation and were not known at the time of the LUS exam.
Two portable ultrasound machines with curvilinear transducers (Mindray M9 (Shenzhen, China) and Esaote MyLab Omega (Genoa, Italy)) were used. The ultrasound machine and transducer were covered with plastic cling film during each exam. The physician sonographers wore N-95/FFP2 masks, impermeable gowns, and two pairs of gloves. Despite the use of personal protective equipment, the physician sonographers were required to stand behind the subjects when performing the LUS exam to avoid face-to-face contact and minimize the risk of viral transmission. The chest wall skin was cleaned with an alcohol-based antiseptic solution before each LUS exam.
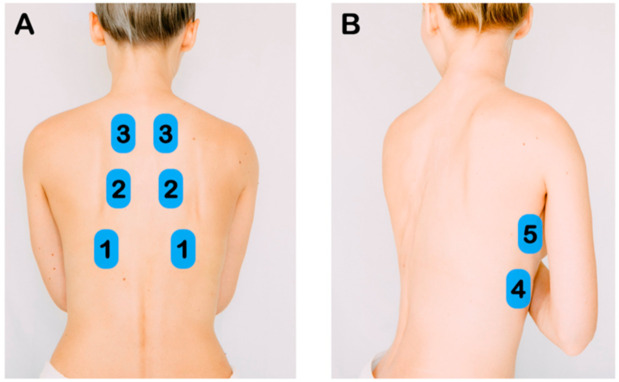
The LUS protocol included 5 zones per hemithorax—three posterior zones (superior, middle, and inferior) and two lateral zones along the mid-axillary line (superior and inferior) (Figure 1). A total of 10 zones were scanned per patient. Pathological LUS findings have been previously described [10,11,16]. LUS findings were categorized as normal, discrete B-lines (3 or more B-lines per rib interspace), confluent B-lines, small subpleural consolidations (<3 cm), and lobar consolidations (Figure 2). LUS findings were recorded as video clips and written descriptions were entered into a database.
Figure 1.
Lung Ultrasound Exam Points. (A) After identifying the diaphragm, the transducer was slide cephalad to image the inferior, middle, and superior zones of the posterior chest. (B) Along the mid-axillary line, the inferior and superior lung zones of the lateral chest were imaged.
Figure 2.
Characteristic Lung Lesions in coronavirus disease 2019 (COVID-19). (A) Normal lung ultrasound is defined by visualization of pleural sliding and A-lines. (B) Discrete B-lines are individual hyperechoic, laser-like artifacts the emanate from the pleural line and are due to increased interstitial fluid in the acute setting. Discrete B-lines are typically the first sign of COVID-19. (C) Fused or confluent B-lines are seen when individual B-lines coalesce as interstitial fluid increases. (D) Subpleural consolidations are typically small (<3 cm) areas of consolidation that are seen just below the pleural line.
2.3. Chest Radiographs
All CXRs were obtained by a radiology technician and interpreted by a board-certified radiologist. Two CXR views (posterior-anterior and lateral) were taken in the radiology department. The final CXR report was entered into a database for comparison with the LUS findings. A blinded third investigator with ultrasound expertise (G.G.C.) compared the LUS and CXR findings reported by the two physician sonographers and radiologists, respectively.
2.4. Statistical Analysis
Subjects were categorized as having suspected or confirmed COVID-19 based on the PCR testing as stated above. CXR and LUS findings were classified into three ordinal categories for each diagnostic method—disease absent (normal lung), unilateral pulmonary infiltrates, and bilateral pulmonary infiltrates. Agreement between the two diagnostic methods was calculated using the weighted Kappa statistic using the ordinal classification system. The Kappa statistic was interpreted as follows—0.20 to 0.45 moderate agreement, 0.45 to 0.75 substantial agreement, and 0.75 to 1.0 perfect agreement [19]. Sensitivity of each method was calculated, and compared using the McNemar test. Statistical analyses were performed using the frequency (FREQ) procedure in SAS (v.9.4. Cary, NC, USA: SAS Institute Inc.; 2014).
3. Results
One hundred and one subjects were enrolled in the study. Five subjects were excluded (three were pregnant and could not receive a CXR; two had alternative diagnoses found). Data were analyzed from a total 96 subjects with a clinical diagnosis of COVID-19.
Characteristics of the subjects are presented in Table 1. The median age of all subjects was 48 years and half were women. The most common comorbidities were hypertension, obesity, asthma, and diabetes mellitus. A majority of subjects presented with fever, cough, and dyspnea. A greater proportion of suspected COVID-19 subjects presented <7 days whereas more confirmed COVID-19 subjects presented ≥7 days. Compared to suspected COVID-19 patients, the confirmed COVID-19 subjects had a significantly lower oxygen saturation, elevated C-reactive protein, elevated lactate dehydrogenase, and lower lymphocyte count. Most confirmed COVID-19 subjects (81%) were hospitalized while most suspected COVID-19 subjects (94%) were discharged home with close monitoring.
Table 1.
Characteristics of Subjects with Suspected and Confirmed COVID-19.
| Characteristic | Suspected n = 53 n (%) |
Confirmed n = 43 n (%) |
Total n = 96 n (%) |
p-Value |
|---|---|---|---|---|
| Gender | 0.105 | |||
| Male | 22 (41.5) | 25 (58.1) | 47 (49.0) | |
| Female | 31 (58.5) | 18 (41.9) | 49 (51.0) | |
| Age | 0.092 | |||
| Median years (IQR) | 47 (40.0–56.5) | 51 (41.0–64.0) | 48 (41.0–58.0) | |
| <30 | 5 (9.4) | 0 (0.0) | 5 (5.2) | |
| 30–39 | 8 (15.1) | 6 (14.0) | 14 (14.6) | |
| 40–49 | 18 (34.0) | 14 (32.5) | 32 (33.3) | |
| 50–59 | 13 (24.5) | 9 (20.9) | 22 (22.9) | |
| 60–69 | 7 (13.2) | 8 (18.6) | 15 (15.7) | |
| 70–79 | 2 (3.8) | 5 (11.7) | 7 (7.3) | |
| ≥80 | 0 (0.0) | 1 (2.3) | 1 (1.0) | |
| Ethnicity | 0.433 | |||
| Caucasian | 28 (52.8) | 29 (67.4) | 57 (59.4) | |
| Latin American | 17 (32.1) | 11 (25.6) | 28 (29.2) | |
| African | 5 (9.4) | 3 (7.0) | 8 (8.3) | |
| Asian | 2 (3.8) | 0 (0.0) | 2 (2.1) | |
| Other | 1 (1.9) | 0 (0.0) | 1 (1.0) | |
| Comorbidities | ||||
| Hypertension | 14 (32.6) | 12 (22.6) | 26 (27.1) | 0.277 |
| Obesity | 11 (25.6) | 9 (17.0) | 20 (20.8) | 0.302 |
| Asthma | 7 (16.3) | 5 (9.4) | 12 (12.5) | 0.313 |
| Diabetes mellitus | 4 (9.3) | 4 (7.5) | 8 (8.3) | 0.757 |
| Coronary artery disease | 1 (2.3) | 2 (3.8) | 3 (3.1) | 0.685 |
| Chronic obstructive pulmonary disease | 1 (2.3) | 2 (3.8) | 3 (3.1) | 0.685 |
| Bronchitis | 1 (2.3) | 0 (0.0) | 1 (1.0) | 0.264 |
| Human immunodeficiency virus | 1 (2.3) | 0 (0.0) | 1 (1.0) | 0.264 |
| Other | 4 (9.3) | 1 (1.9) | 5 (5.2) | 0.104 |
| Symptoms | ||||
| Fever | 43 (81.1) | 38 (88.4) | 81 (84.4) | 0.331 |
| Cough | 42 (79.2) | 37 (86.0) | 79 (82.3) | 0.385 |
| Dyspnea | 28 (52.8) | 30 (69.8) | 58 (60.4) | 0.092 |
| Myalgia | 19 (35.8) | 11 (25.6) | 30 (31.3) | 0.280 |
| Diarrhea | 11 (20.8) | 9 (20.9) | 20 (20.8) | 0.983 |
| Headache | 10 (18.9) | 2 (16.7) | 12 (12.5) | 0.036 |
| Sore throat | 7 (13.2) | 3 (7.0) | 10 (10.4) | 0.320 |
| Other | 3 (5.7) | 1 (2.3) | 4 (4.2) | 0.416 |
| Days of Symptoms | ||||
| Median days (IQR) | 6.0 (3.0–9.5) | 7.0 (5.0–10.0) | 7.0 (4.0–10.0) | 0.080 |
| <7 days | 31 (58.5) | 13 (30.2) | 44 (45.8) | 0.006 |
| ≥7 days | 22 (41.5) | 30 (57.7) | 52 (54.2) | |
| Oxygen Saturation | ||||
| Median % (IQR) | 98.0 (96–99) | 95.0 (94–97) | 97.0 (95–98) | <0.001 |
| Lung Physical Examination | 0.285 | |||
| Normal | 25 (47.2) | 25 (58.1) | 50 (52.1) | |
| Abnormal | 28 (52.8) | 18 (41.9) | 46 (47.9) | |
| Laboratory Data, median (IQR) | ||||
| Leukocytes (n = 73) (×103 /µL) | 6.1 (5.4–8.2) | 6.8 (5.3–8.4) | 6.5 (5.4–8.2) | 0.696 |
| Lymphocytes (n = 73) (×103 /µL) | 1.6 (1.2–1.9) | 1.2 (0.8–1.4) | 1.4 (1.0–1.7) | <0.001 |
| LDH (n = 71) (Nl=120–240 U/L) | 208 (160–226) | 248 (208–310) | 220 (184–275) | 0.001 |
| CRP (n = 73) (Nl < 5 mg/L) | 26 (5.0–48.0) | 51 (28.7–113.2) | 41 (12.5–91.5) | 0.001 |
| D-dimer (n = 68) (Nl < 500 ng/mL) | 455 (350–700) | 535 (405–1052) | 500 (370–757.5) | 0.170 |
| Chest X-ray | ||||
| Normal | 32 (60.3) | 4 (9.3) | 36 (37.5) | <0.001 |
| Alveolar infiltrate | 15 (28.3) | 36 (83.7) | 51 (53.1) | <0.001 |
| Interstitial infiltrate | 9 (17.0) | 12 (27.9) | 21 (21.9) | 0.198 |
| Other | 1 (1.9) | 2 (4.7) | 3 (3.1) | 0.439 |
| Lung Ultrasound Findings | ||||
| Normal | 16 (30.2) | 2 (4.7) | 18 (18.8) | 0.001 |
| Discrete B-lines | 37 (69.8) | 41 (95.3) | 78 (81.3) | 0.001 |
| Confluent B-lines | 19 (35.8) | 29 (67.4) | 48 (50.0) | 0.002 |
| Small Subpleural Consolidations (<3 cm) | 18 (34.0) | 23 (53.5) | 41 (42.7) | 0.054 |
| Large Consolidations (>3 cm) | 2 (3.8) | 0 | 2 (2.1) | 0.198 |
| Pleural effusion | 1 (1.9) | 1 (2.3) | 2 (2.1) | 0.881 |
| Other | 1 (1.9) | 1 (2.3) | 2 (2.1) | 0.881 |
| Disposition | <0.001 | |||
| Hospitalized | 3 (5.7) | 35 (81.4) | 38 (39.6) | |
| Home with Close Follow-up | 50 (94.3) | 8 (18.6) | 58 (60.4) |
IQR, interquartile range; LDH, lactate dehydrogenase; CRP, C-reactive protein.
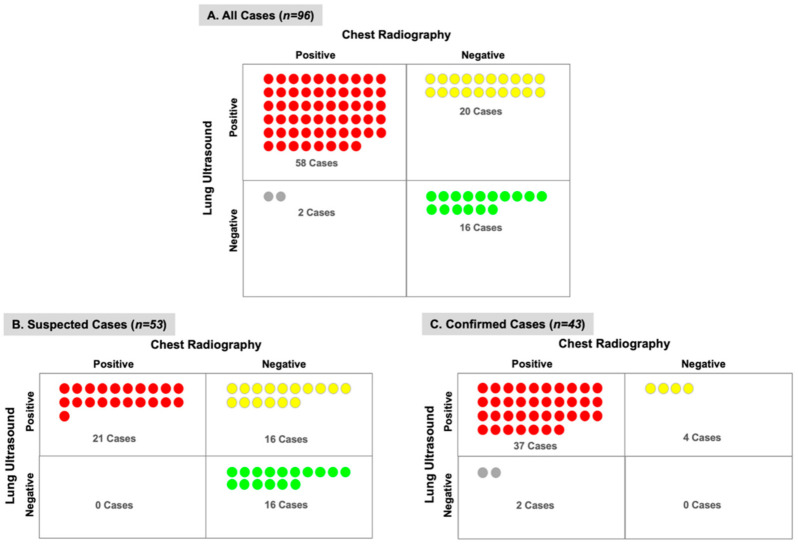
LUS detected pulmonary infiltrates in more subjects than CXR (81% vs. 63%) with a greater difference among subjects with suspected COVID-19 (70% vs. 40%) versus confirmed COVID-19 (95% vs. 91%) (Figure 3). Among the subjects with a normal CXR but abnormal LUS exam, 20 subjects (55%) had pulmonary infiltrates detectable by LUS (Figure 4). Furthermore, most of these subjects (n = 12) had bilateral infiltrates that were seen on LUS but not on CXR (Figure S1). On the contrary, among the subjects with a normal LUS exam but abnormal CXR, only two had pulmonary infiltrates detected on CXR which were described as “doubtful” or “minimal” infiltrates in the medial or left basilar lung fields per the radiologist’s official report (Figure 4).
Figure 3.
Chest X-ray and Lung Ultrasound for Detection of Pulmonary Infiltrates. The number of suspected or confirmed COVID-19 subjects (n) with or without pulmonary infiltrates detected by chest X-ray or lung ultrasound is demonstrated. In both suspected and confirmed COVID-19 subjects, lung ultrasound was able to detect pulmonary infiltrates more often than chest radiography.
Figure 4.
Correlation of Chest X-ray and Lung Ultrasound in Detection of Pulmonary Infiltrates. The number of subjects (n) and agreement between chest X-ray and lung ultrasound is shown for (A) all cases, (B) suspected COVID-19 cases, and (C) confirmed COVID-19 cases. Lung ultrasound detected pulmonary infiltrates in 20 subjects with a normal chest X-ray, whereas chest X-ray detected pulmonary infiltrates in 2 subjects with a normal LUS exam.
The types of LUS and CXR findings are shown in Table 1. More suspected COVID-19 subjects had a normal LUS and CXR compared to those with confirmed disease. Among all 78 subjects with LUS abnormalities, all subjects had discrete B-lines with pleural line irregularities. Half of all subjects had confluent B-lines and 43% had small subpleural consolidations (<3 cm). In confirmed COVID-19 subjects, alveolar infiltrates on CXR and discrete or confluent B-lines on LUS were more often seen compared to those with suspected COVID-19.
The distribution of pulmonary infiltrates detected by LUS versus CXR in suspected and confirmed COVID-19 subjects is shown in Figure 5 (Tables S1 and S2). LUS detected pulmonary infiltrates compared to CXR in a greater proportion of subjects in both the right (77% vs. 57%) and left lungs (67% vs. 58%). Regarding specific lung lobes, LUS detected pulmonary infiltrates more often than CXR in all lung lobes with the greatest differences in the right middle lobe (62% vs. 32%), right lower lobe (65% vs. 46%), and left upper lobe (52% vs. 35%). In all lung lobes, pulmonary infiltrates were detected more frequently in confirmed versus suspected COVID-19 subjects by either LUS or CXR.
Figure 5.
Distribution of Pulmonary Infiltrates Detected by Chest X-ray vs. Lung Ultrasound. The number of subjects (n) with confirmed or suspected COVID-19 who had pulmonary infiltrates detected in the upper, middle, or lower lobes of the right and left lung is demonstrated.
The correlation between LUS and CXR was assessed by weighted Kappa statistic (Figure S2). A substantial level of agreement was demonstrated between LUS and CXR for normal, unilateral or bilateral pulmonary infiltrates (Κ = 0.48 (95% CI 0.34 to 0.63)), as defined by Munoz et al. [19]. Comparing normal versus abnormal LUS and CXR, the Kappa statistic similarly showed substantial agreement (Κ = 0.46 (95% CI 0.28 to 0.63)). LUS was more sensitive than CXR for detecting pulmonary infiltrates (81% vs. 63%; p = 0.002) using the McNemar test.
4. Discussion
We reported the findings of a large prospective study assessing the correlation of LUS and CXR for detection of pulmonary infiltrates in noncritically ill COVID-19 patients. A substantial level of agreement was demonstrated between LUS and CXR, and LUS detected pulmonary infiltrates more frequently compared to CXR in all subjects. Most importantly, among the subjects with a negative CXR, abnormalities were detected by LUS in more than half of these subjects.
Confirming a diagnosis of COVID-19 by laboratory testing or diagnostic imaging is challenging, especially early in the course of the disease. PCR testing is limited by availability, high false negative rate (sensitivity 65–83%), and delays in test positivity (mean 5.1 days) [2,3,4,5]. In one study, PCR test results turned positive in 21% of patients after two consecutive negative results [20]. In our study, PCR test results were not available until 24–72 h after presentation and were unknown when the LUS exam and CXR were performed. Among the diagnostic imaging modalities, chest CT scan has been reported to have the highest sensitivity (97–98%) [2,3,4,5]. However, obtaining chest CT scans on all patients with suspected COVID-19 is impracticable during a pandemic when resources are limited, and most of the world’s population lacks access to CT imaging [21]. Thus, clinicians have had to rely primarily on CXRs and LUS to detect pulmonary infiltrates to support a clinical diagnosis of COVID-19.
The LUS findings in COVID-19 have been well described in several reports [10,11,12,13,14,15,16]. However, only two small case series have reported both CXR and LUS findings in COVID-19 patients, but neither study directly compared CXR and LUS findings nor assessed the correlation of the two imaging tests [17,18]. In our study, all patients underwent both LUS and CXR upon presentation that were interpreted by blinded experts. We demonstrated a substantial level of agreement between LUS and CXR, but LUS had a higher sensitivity for detecting pulmonary infiltrates compared to CXR (81% vs. 63%). Our findings are consistent with another study reporting the sensitivity of CXR (69%) in COVID-19 patients [8]. Similar sensitivity of LUS (85%) was reported in a meta-analysis of non-COVID pneumonia studies comparing LUS to CXR or chest CT scans [22].
A key finding of our study was the ability of LUS to detect pulmonary infiltrates in more than half of the subjects with a normal CXR. Furthermore, one-third of these subjects had bilateral findings on LUS that were not seen on CXR (Figure S1). On the contrary, only two subjects had lung infiltrates reported on CXR that were not seen on LUS; however, the radiologist’s official report commented that these were “doubtful” or “minimal” infiltrates. Based on our findings, institutions with trained clinicians can develop protocols that include LUS as part of the initial bedside evaluation of suspected COVID-19 patients. Though not assessed in our study, bedside detection of pulmonary infiltrates by LUS has the potential to guide triage and treatment decisions as new therapies emerge.
In our study, disposition decisions about hospital admission versus close monitoring at home were determined using a hospital protocol independent of the LUS findings. However, a few points deserve mention from our post-hoc analysis of disposition (Tables S3 and S4). First, subjects with a normal CXR or LUS were more often discharged home. Second, though COVID-19 PCR test results were not known at the time of presentation, more confirmed versus suspected COVID-19 subjects were admitted to the hospital versus discharged home (81% vs. 15%). Most importantly, LUS detected more unilateral (25% vs. 17%) or bilateral pulmonary infiltrates (42% vs. 19%) compared to CXR in suspected COVID-19 subjects that were safely discharged home. Whether LUS is overly sensitive for detecting pulmonary infiltrates that could lead to unnecessary admission of individuals that could be safely monitored at home is an important question to address in future studies.
We recognize that our study has limitations. First, PCR testing could only be performed on approximately half of subjects in our study because laboratory testing supplies were extremely limited during the initial surge of the COVID-19 pandemic in Madrid. However, given the high false negative rates of early PCR test kits and the 24–72 h delay in obtaining PCR test results, a clinical diagnosis of COVID-19 was typically made based on close contact and supportive laboratory findings. Second, due to concerns of healthcare workers contracting COVID-19, a rapid and focused LUS exam was performed with the physician sonographer standing behind the patient and interrogating the posterior and lateral chest walls. Recent publications have recommended standardization of LUS protocols in COVID-19 to foster pooling of data from multiple institutions in future studies [14,23]. Third, chest CT scans could not be obtained in all patients with suspected COVID-19 due to limited hospital resources, and only three subjects underwent a chest CT scan.
5. Conclusions
In summary, LUS findings correlated well with those of CXR in patients with suspected or confirmed COVID-19. Lung ultrasound was able to detect pulmonary infiltrates in more than half of patients with a normal CXR. Thus, a LUS exam may be performed at the bedside as the initial diagnostic imaging test in patients with COVID-19. Future studies are needed to evaluate the use of a standardized LUS protocol on triage decisions and health services of patients with suspected COVID-19.
Supplementary Materials
The following are available online at https://www.mdpi.com/2075-4418/11/2/373/s1, Figure S1: Comparison of Normal, Unilateral and Bilateral Infiltrates on Chest X-ray and Lung Ultrasound. The agreement be-tween chest X-ray and lung ultrasound is shown for (A) all cases, (B) suspected COVID-19 cases, and (C) confirmed COVID-19 cases. Lung ultrasound detected bilateral pulmonary infiltrates in a substantial proportion of subjects with either a normal or unilateral infiltrates on chest X-ray, Figure S2: Correlation of Lung Ultrasound and Chest X-ray in COVID-19. (A) This plot shows the correlation of findings for normal, unilateral, or bilateral disease. (B) This plot shows the correlations between normal and any disease. The darkest areas indicate exact agreement between LUS and CXR, lightest areas indicate partial or no agreement between LUS and CXR. The 45-degree line above the intersection of the middle rectangles indicates that LUS (plotted vertically) detects more disease than does CXR (plotted horizontally), Table S1: Number of lobes with pulmonary infiltrates detected by chest radiograph stratified by the suspected and confirmed groups of patients with COVID-19, Table S2: Number of lobes with pulmonary infiltrates detected by lung ultrasound stratified by the suspected and confirmed groups of patients with COVID-19, Table S3: Detection of pulmonary infiltrates (none, unilateral, or bilateral) by lung ultrasound versus disposition to discharge home in all, suspected, and confirmed patients with COVID-19, Table S4: Detection of pulmonary infiltrates (none, unilateral, or bilateral) by chest X-ray versus disposition to discharge home in all, suspected, and confirmed patients with COVID-19.
Author Contributions
Conceptualization, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., M.M., J.C.L., M.I.R., and N.J.S.; methodology, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., M.M., J.C.L., M.I.R., and N.J.S.; software, X.X.; validation, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., M.M., J.C.L., M.I.R., and N.J.S.; formal analysis, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., G.E.O.J., M.M., J.C.L., M.I.R., and N.J.S.; investigation, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., G.E.O.J., M.M., J.C.L., M.I.R., and N.J.S.; resources, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., M.M., J.C.L., M.I.R., and N.J.S.; data curation, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., G.E.O.J., M.M., J.C.L., M.I.R., and N.J.S.; writing—original draft preparation, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., G.E.O.J., M.M., J.C.L., M.I.R., and N.J.S.; writing—M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., G.E.O.J., M.M., J.C.L., M.I.R., and N.J.S.; visualization, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., G.E.O.J., M.M., J.C.L., M.I.R., and N.J.S.; supervision, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., M.M., J.C.L., M.I.R., and N.J.S.; project administration, M.M.G., G.G.d.C.S., K.P., F.J.T.M., D.L., J.-V.S., M.M., J.C.L., M.I.R., and N.J.S.; funding acquisition, none. G.G.d.C.S. has full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors have read and agreed to the published version of the manuscript.
Funding
Nilam J. Soni receives funding from the U.S. Department of Veterans Affairs, Quality Enhancement Research Initiative (QUERI) Partnered Evaluation Initiative Grant, I50 HX002263-01A1. This material is the result of work supported with resources and the use of facilities at the South Texas Veterans Health Care System in San Antonio, Texas. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and was approved by the ethics and research committee of Hospital Universitario Puerta de Hierro-Majadahonda in March 2020 (PI 64/20).
Informed Consent Statement
Verbal consent was obtained and documented in the electronic medical record. Written consent using paper was not feasible due to the risk of fomite transmission of SARS-CoV-2 to study personnel.
Data Availability Statement
All the data used in this study will be made publicly upon publication of the study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., et al. Clinical features of patients infected with 2019 novel coronavirus in wuhan, china. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P., Ji W. Sensitivity of chest ct for covid-19: Comparison to rt-pcr. Radiology. 2020:200432. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., Tao Q., Sun Z., Xia L. Correlation of chest ct and rt-pcr testing in coronavirus disease 2019 (covid-19) in china: A report of 1014 cases. Radiology. 2020:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Long C., Xu H., Shen Q., Zhang X., Fan B., Wang C., Zeng B., Li Z., Li X., Li H. Diagnosis of the coronavirus disease (covid-19): Rrt-pcr or ct? Eur. J. Radiol. 2020;126:108961. doi: 10.1016/j.ejrad.2020.108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Y., Dong C., Hu Y., Li C., Ren Q., Zhang X., Shi H., Zhou M. Temporal changes of ct findings in 90 patients with covid-19 pneumonia: A longitudinal study. Radiology. 2020:200843. doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American College or Radiology ACR Recommendations for the Use of Chest Radiography and Computed Tomography (ct) for Suspected Covid-19 Infection. [(accessed on 10 April 2020)]; Available online: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection.
- 7.Kim E.S., Chin B.S., Kang C.K., Kim N.J., Kang Y.M., Choi J.P., Oh D.H., Kim J.H., Koh B., Kim S.E., et al. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: A preliminary report of the first 28 patients from the korean cohort study on covid-19. J. Korean Med. Sci. 2020;35:e142. doi: 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong H.Y.F., Lam H.Y.S., Fong A.H., Leung S.T., Chin T.W., Lo C.S.Y., Lui M.M., Lee J.C.Y., Chiu K.W., Chung T., et al. Frequency and distribution of chest radiographic findings in covid-19 positive patients. Radiology. 2019:201160. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winkler M.H., Touw H.R., van de Ven P.M., Twisk J., Tuinman P.R. Diagnostic accuracy of chest radiograph, and when concomitantly studied lung ultrasound, in critically ill patients with respiratory symptoms: A systematic review and meta-analysis. Crit. Care Med. 2018;46:e707–e714. doi: 10.1097/CCM.0000000000003129. [DOI] [PubMed] [Google Scholar]
- 10.Huang Y., Wang S., Liu Y., Zhang Y., Zheng C., Zheng Y., Zhang C., Min W., Zhou H., Yu M. A Preliminary Study on the Ultrasonic Manifestations of Peripulmonary Lesions of Non-Critical Novel Coronavirus Pneumonia (Covid-19) [(accessed on 15 May 2020)];2020 Available online: https://ssrn.com/abstract=3544750.
- 11.Peng Q.Y., Wang X.T., Zhang L.N. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020;46:849–850. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xing C., Li Q., Du H., Kang W., Lian J., Yuan L. Lung ultrasound findings in patients with covid-19 pneumonia. Crit. Care (Lond. Engl.) 2020;24:174. doi: 10.1186/s13054-020-02876-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poggiali E., Dacrema A., Bastoni D., Tinelli V., Demichele E., Ramos P.M., Marcianò T., Silva M., Vercelli A., Magnacavallo A. Can lung us help critical care clinicians in the early diagnosis of novel coronavirus (covid-19) pneumonia? Radiology. 2020:200847. doi: 10.1148/radiol.2020200847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soldati G., Smargiassi A., Inchingolo R., Buonsenso D., Perrone T., Briganti D.F., Perlini S., Torri E., Mariani A., Mossolani E.E., et al. Proposal for international standardization of the use of lung ultrasound for covid-19 patients; a simple, quantitative, reproducible method. J. Ultrasound Med. 2020;39:1413–1419. doi: 10.1002/jum.15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soldati G., Smargiassi A., Inchingolo R., Buonsenso D., Perrone T., Briganti D.F., Perlini S., Torri E., Mariani A., Mossolani E.E., et al. Is there a role for lung ultrasound during the covid-19 pandemic? J. Ultrasound Med. 2020;39:1459–1462. doi: 10.1002/jum.15284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Volpicelli G., Gargani L. Sonographic signs and patterns of covid-19 pneumonia. Ultrasound J. 2020;12:22. doi: 10.1186/s13089-020-00171-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yasukawa K., Minami T. Point-of-care lung ultrasound findings in patients with novel coronavirus disease (covid-19) pneumonia. Am. J. Trop. Med. Hyg. 2020 doi: 10.4269/ajtmh.20-0280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lomoro P., Verde F., Zerboni F., Simonetti I., Borghi C., Fachinetti C., Natalizi A., Martegani A. Covid-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and ct: Single-center study and comprehensive radiologic literature review. Eur. J. Radiol. Open. 2020;7:100231. doi: 10.1016/j.ejro.2020.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munoz S.R., Bangdiwala S.I. Interpretation of kappa and b statistics measures of agreement. J. Appl. Stat. 1997;24:105–112. doi: 10.1080/02664769723918. [DOI] [Google Scholar]
- 20.Xiao A.T., Tong Y.X., Zhang S. False-negative of rt-pcr and prolonged nucleic acid conversion in covid-19: Rather than recurrence. J. Med. Virol. 2020;92:1755–1756. doi: 10.1002/jmv.25855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mollura D., Lungren M. Radiology in Global Health: Strategies, Implementation, and Applications. Springer; New York, NY, USA: 2013. [Google Scholar]
- 22.Alzahrani S.A., Al-Salamah M.A., Al-Madani W.H., Elbarbary M.A. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit. Ultrasound J. 2017;9:6. doi: 10.1186/s13089-017-0059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Volpicelli G., Lamorte A., Villén T. What’s new in lung ultrasound during the covid-19 pandemic. Intensive Care Med. 2020:1–4. doi: 10.1007/s00134-020-06048-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data used in this study will be made publicly upon publication of the study.