Abstract
Hemodynamic optimization remains the cornerstone of resuscitation in the treatment of sepsis and septic shock. Delay or inadequate management will inevitably lead to hypoperfusion, tissue hypoxia or edema, and fluid overload, leading eventually to multiple organ failure, seriously affecting outcomes. According to a large international survey (FENICE study), physicians frequently use inadequate indices to guide fluid management in intensive care units. Goal-directed and “restrictive” infusion strategies have been recommended by guidelines over “liberal” approaches for several years. Unfortunately, these “fixed regimen” treatment protocols neglect the patient’s individual needs, and what is shown to be beneficial for a given population may not be so for the individual patient. However, applying multimodal, contextualized, and personalized management could potentially overcome this problem. The aim of this review was to give an insight into the pathophysiological rationale and clinical application of this relatively new approach in the hemodynamic management of septic patients.
Keywords: septic shock, hemodynamic monitoring, early goal-directed therapy, lactate, fluid therapy
1. Introduction
Early, adequate hemodynamic stabilization remains the cornerstone of resuscitation of the critically ill. Fluid resuscitation and vasopressor support are the most frequent treatments used to avoid or treat hypoperfusion and maintain adequate oxygen delivery to the tissues. Theoretically, intravenous fluid administration can improve oxygen delivery (DO2) by increasing cardiac output (CO), and vasopressors can maintain adequate perfusion pressure. However, both treatments can have deleterious effects when used in an inappropriate manner: under-resuscitation may cause hypoperfusion and positive fluid balance could increase mortality, especially in acute respiratory distress syndrome (ARDS) or even in septic shock [1,2,3]. From a physiological standpoint, a coherence between macro- and microcirculation is necessary for adequate functioning [4]. Translating this into clinical practice means that whatever we do to correct systemic hemodynamics only makes sense if it is followed by improved microcirculatory perfusion and oxygen delivery. There have been several attempts to recommend the most feasible approach in hemodynamic management, but none of them has gained generalized acceptance as being superior to the others. One of the most investigated approaches is the so-called “goal-directed therapy” (GDT), which is a very broad term and by-and-large means that prespecified values of certain physiological indices are followed and compared to standard monitoring. Although goal-directed approaches have been tried and tested in several large trials, results are contradictory [5,6,7,8]. This could be due to the fact that these approaches mainly tried to optimize macrocirculatory indices according to fixed values and neglected the patients’ individual demand. To overcome this limitation, putting the available pieces of the “hemodynamic puzzle” (DO2, oxygen consumption (VO2), and tissue perfusion) together was proposed as an alternative approach [9]. Unfortunately, this concept is in contrast with the rather arbitrary and uncoordinated use of fluids by clinicians worldwide as demonstrated in the FENICE study [10]. However, the importance of individualizing resuscitation measures was also recommended by the recent European Society of Intensive Care Medicine task force [11].
The aim of this review was to give an insight into the pathophysiological rationale and clinical application of this relatively new approach in the hemodynamic management of the critically ill—including septic patients.
2. Paradigm Shift in Definitions
Although our title suggests sepsis-specific management, this may require some clarification. In 2016, sepsis was defined as “life threatening organ dysfunction caused by a dysregulated immune response to infection” [12]. The inclusion of the term “dysregulated immune response” was a fundamental and conceptual change compared to the long standing “systemic inflammatory response syndrome” [13]. Dysregulated host response means that the physiological balance between pro-, and anti-inflammation—which is fundamental for tackling and recovering from any type of injury (be it tissue trauma or infection)—is lost [14]. This imbalance is the result of an excessive release of pro-inflammatory mediators, causing a feature that is called a “cytokine storm”, “cytokine release syndrome”, or “hyperinflammation” [15]. The hemodynamic effects of a cytokine storm can lead to the loss of control of the vascular tone and may cause “vasoplegic shock”, which is identical to the condition that we see in septic shock. The only difference is that vasoplegic shock as a term can be applied in conditions when there is no infection, such as trauma, sterile inflammation, burns, etc., in which case the inflammation can be just as severe as—or even worse than—seen in sepsis. Discussing this in further detail is well beyond the scope of the current review, but it may become clear now that the message of the following paragraphs could be applied not only in sepsis, but in any critically ill conditions.
3. Hemodynamic Management Concepts
3.1. Goal-Directed Therapy
According to the recent recommendations of the Surviving Sepsis Campaign Guidelines [16], after the first 3 h of a fixed fluid regimen of 30 mL/kg crystalloids, a goal-directed approach should be followed with frequent re-assessment, preferring dynamic variables over static ones to ensure adequate perfusion and a balance between oxygen delivery and demand. These statements were supported by low and moderate quality evidence [16]. The guideline strongly recommends a target mean arterial pressure (MAP) of 65 mmHg and advises to refrain from the use of central venous pressure (CVP) and other static goals.
Rivers et al. performed a pivotal randomized controlled trial in 2001 with 263 patients to evaluate the efficacy of early goal-directed fluid therapy (EGDT) [5]. Patients with septic shock or severe sepsis were enrolled. Standard care was guided by CVP, MAP and urine output. In the intervention group, central venous oxygen saturation (ScvO2) was continuously monitored for 6 h alongside the parameters used in standard therapy, aiming to maintain ScvO2 equal to or above 70%. As per the protocol, 500 milliliters of crystalloids was given every 30 min to maintain a CVP between 8 and 12 mmHg. In the case of lower-than-target ScvO2, red blood cells were transfused until hematocrit values reached 30%.
Significantly lower in-hospital mortality was found in the intervention group (30.5% versus 46.5%, p = 0.009). Physiologic parameters and Acute Physiology and Chronic Health Evaluation (APACHE) II scores in the first 24 h indicated that the goal-directed approach resulted in less severe organ dysfunction.
Later, three workgroups attempted to repeat these results with slight alterations in the protocol. However, neither the PROMISE, ARISE, nor PROCESS trials could prove goal-directed to be superior to standard resuscitation strategies [6,7,8].
PROMISE was a multicenter pragmatic randomized trial from England with 1260 enrolled patients and 90-day follow-up [6]. The relative risk of 90–day mortality was 1.01 in the EGDT group, and there were no significant differences in secondary outcomes, including quality of life and adverse events. Moreover, EGDT increased the cost of treatment.
Similarly, the ARISE trial enrolled 1600 patients from 51 centers in Australia and New Zealand, with the same primary endpoint and non-significant results [7]. The PROCESS study was conducted at 31 centers in the United States, enrolling 1341 patients. Its primary endpoint was 60-day in-hospital mortality, which did not differ significantly in the two groups (21% for EGDT and 18.2% for standard therapy). Both 90-day and 1-year mortalities were similar [8].
The congruent conclusions of the three large multicenter studies highlighted that the results from the original study may have been biased. Furthermore, therapeutic advances from 2001 to 2014 could also have affected outcomes, as shown by the lower mortality rates of sepsis in general. The overall explanation at the time was that it could be due to the continuously updated Surviving Sepsis Guideline protocols [17]—including the new concept of a lower threshold of hemoglobin levels for transfusion, tighter blood glucose control, and the appearance of lung protective ventilation just to name a few; hence, the marginal advantage of early goal-directed therapy may have disappeared.
However, when we took a closer look at the mortality of septic shock reported in large observational studies, it has not really changed over the years and can be as high as 50% [18]; hence, there is still a lot of room for improvement. Therefore, one cannot exclude that the individualized approach of fluid management, which has strong pathophysiological rationale, could be more appropriate and may also improve outcomes in sepsis and septic shock.
3.2. Adding Measures of Oxygen Debt to the Picture
The ultimate aim of hemodynamic management is to restore the balance between oxygen demand and supply at the tissue level. Outside clinical trials, it is not yet feasible to directly measure tissue perfusion; therefore, we desperately need surrogate markers of global oxygen extraction and tissue hypoxia that are readily available at the bedside to guide therapeutic interventions. Central venous oxygen saturation, venous-to-arterial carbon dioxide gap (dCO2), lactate, and capillary refill time have all been proposed as potential resuscitation targets in hemodynamically unstable patients.
ScvO2 is a frequently used blood gas parameter—as a surrogate of mixed venous saturation taken from a catheter inserted in the superior vena cava—and is routinely used in patients with any shock. ScvO2 is generally influenced by the hemoglobin level, oxygen saturation, dissolved oxygen, CO (components of DO2), and oxygen consumption. Changes in ScvO2 can potentially indicate clinically significant anemia, hypovolemia, and impaired myocardial function and can be affected by medications, body temperature, or a combination of any other factors that are able to influence the VO2/DO2 relationship [19]. It is known that both low and high ScvO2 values are associated with higher mortality in patients with sepsis [20,21]. Furthermore, it was recently demonstrated that persistently low ScvO2 was associated with a higher 90-day mortality in septic shock, independent from other risk factors for death [22]. Low ScvO2 is likely secondary to inadequate oxygen delivery and resuscitation [20], whereas supranormal ScvO2 values should be interpreted as insufficient oxygen uptake due to microcirculatory shunting or sepsis-induced mitochondrial dysfunction [23,24]. It is important to note that this feature could make the interpretation of ScvO2 extremely difficult at the bedside. Although the three previously mentioned large, prospective, and multicenter randomized studies (PROCESS, ARISE, PROMISE) [6,7,8] failed to demonstrate any mortality benefits of an ScvO2-based approach, this may have been due in part to the protocols which applied fixed values of certain parameters as targets for the whole study population and neglected the patients’ individual needs.
Another important marker of tissue metabolism is lactate, which is known as an easily measurable parameter of tissue hypoperfusion/hypoxia, often reflecting anaerobic metabolism. Moreover, it is a recommended resuscitation target in septic shock [16], and its peak concentration and persistent hyperlactatemia after resuscitation is regarded as an important prognostic factor of unfavorable outcomes in shock [25,26]. It is essential to highlight that according to the latest evidence, sepsis-related lactate production is not solely due to tissue hypoxia or hypoperfusion; therefore, lactate “clearance” (a term often used, although not clearance per se, but rather the degree of change in lactate levels) or high lactate in sepsis are not always a true reflection of impaired oxygen delivery and tissue hypoperfusion [21,27].
One single-center retrospective cohort study examined the relationship between lactate and ScvO2 and found that lactate had very little predictive ability for ScvO2 in the vast majority of critically ill patients; therefore, lactate should not be used interchangeably with ScvO2 as a marker of tissue hypoxia [28]. This is not surprising if we take into account that lactate is only considered pathological when it is high, while ScvO2 reflects abnormality both when low and when elevated. It is also crucial to bear in mind that fluid resuscitation on its own can have a diluting effect on lactate levels; therefore, it may give a false positive signal of improvement in this scenario. Hence, putting it in context with other hemodynamic indices is important.
Another simply obtainable blood flow-related variable is central venous-to-arterial carbon dioxide partial pressure difference (pCO2 gap or dCO2), which requires the parallel analysis of arterial and central venous blood gas samples. From a physiological standpoint, adapting the Fick principle to carbon dioxide production and elimination, the following equation describes the pCO2 gap [29]:
| (1) |
where VCO2 is CO2 production, and CO is cardiac output. This clearly shows the indirect relationship between pCO2 gap and CO and explains why an increased pCO2 gap usually corresponds to low flow states. A very recent meta-analysis suggested that increased dCO2 (>6 mmHg) was associated with increased mortality, elevated lactate levels, and a lower cardiac index in critically ill patients [30].
In addition to laboratory parameters, clinical signs can also be extremely useful tools to assess hemodynamics. Therefore, assessing obvious vital signs, including changes in mental status, decreasing urine output, etc., are important signals to raise the alarm. Measurement of capillary refill time (CRT) is a widely used method to assess peripheral perfusion at the bedside and when it is prolonged (>3 sec), it usually indicates centralized circulation. Critically ill patients with abnormal CRT after fluid resuscitation were shown to have a significantly higher chance of worsening organ failure [31] and a persistently prolonged CRT after initial fluid resuscitation was associated with an adverse outcome in septic shock patients with elevated lactate levels [32]. The effect of CRT-guided resuscitation on 28-day mortality in septic shock compared to a lactate clearance targeted strategy was examined in the recent ANDROMEDA-SHOCK trial [33]. Unfortunately, this resuscitation strategy was not able to improve survival. Central venous oxygen saturation and dCO2 gradients were not significantly different between groups, but the CRT guided group showed improved sequential organ failure (SOFA) scores at 72 h and received significantly less resuscitation fluids within the first 8 h. However, the very same group compared CRT- to lactate-targeted resuscitation and found comparable effects on regional and microcirculatory flow parameters but a faster achievement of the predefined resuscitation target in the CRT group [34]. They also suggested that stopping fluids in patients with CRT ≤ 3 s is safe in terms of tissue perfusion.
Skin mottling also provides valuable information on skin perfusion, hence centralized circulation. A semi-quantitative evaluation of mottling on skin area extension on the legs can range from score 0 (no mottling) to score 5 (when it extends above the groin) and has been shown to be a good predictor of survival in septic shock [35,36].
In summary ScvO2, dCO2, lactate, and skin perfusion could be used as equally important surrogates and serve as helpful complimentary tools to guide our efforts in restoring normal tissue perfusion in the critically ill. It is also important to understand that no one parameter is appropriate as a single target to guide resuscitation. We need to put several pieces of the puzzle together in context to have a clearer picture in order to help us to individualize therapy.
3.3. The Individualized/Personalized Concept
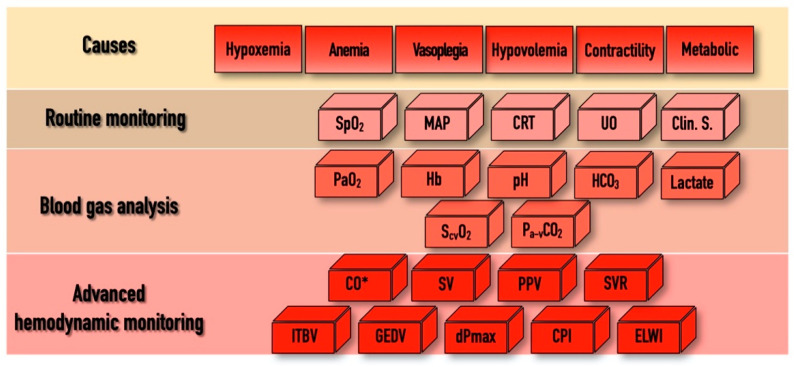
In addition to the above-mentioned physiological indices, there are several other hemodynamic parameters, both static and dynamic, which were tested as resuscitation targets over the last few decades within the domain of “functional hemodynamic monitoring” [37]. This often required “advanced hemodynamic monitoring”, including the measurement of CO and other derived variables, as depicted in Figure 1. Despite the pathophysiological rationale of this approach, according to a recent meta-analysis, results of clinical trials were not convincing enough to enable any of the proposed algorithms to become standard practice [38]. The main limitations of these studies, as depicted in an editorial by Saugel et al., were heterogeneity in timing, the applied technology, choosing the right endpoint, and indeed the lack of personalization [39]. Furthermore, there were no prospective randomized trials that showed an effect for GDTon patient outcome and mortality when using advanced hemodynamic monitoring, whatever the technique used—be it echography [40], a pulmonary artery catheter [41], or transpulmonary thermodilution [42].
Figure 1.
The “bricks” of individualized hemodynamic management. SpO2, pulse oximetry driven oxygen saturation; MAP, mean arterial pressure; CRT, capillary refill time; UO, urine output; Clin. S, clinical signs; PaO2, partial pressure of oxygen; Hb, hemoglobin; HCO3, bicarbonate; ScvO2, central venous oxygen saturation; Pa-vCO2, arterial-to-venous carbon dioxide gap; CO, cardiac output; SV, stroke volume; PPV, pulse pressure variability; SVR, systemic vascular resistance; ITBV, intrathoracic blood volume; GEDV, global end-diastolic volume; dPmax, left ventricle contractility index; CPI, cardiac power index; ELWI, extravascular lung water index; * indicates that CO can be determined by invasive hemodynamic measurements or by echo-cardiography. For explanation, please see text.
The only way to tailor hemodynamic support for the patients’ individual needs is to put the results of a detailed hemodynamic assessment, including components of macro-circulation, DO2 and VO2, into context. In a recent paper, this approach was named by Molnar et al. as a “multimodal, individualized, contextualized” concept [43]. The potential and most often used components of assessment, the “bricks” of this puzzle, are depicted in Figure 1. In practice, hemodynamic instability may occur for several reasons and in the combination of these, shown in the first row as “Causes”. As “Routine monitoring” records certain variables in a real-time fashion, it is highly likely that the first alarm signals will arrive from this domain. Blood gas analyses (both arterial and central venous) can help to confirm the severity of the alarm signal. In case of uncertainty, advanced monitoring can help to define the cause, severity, and the necessary interventions.
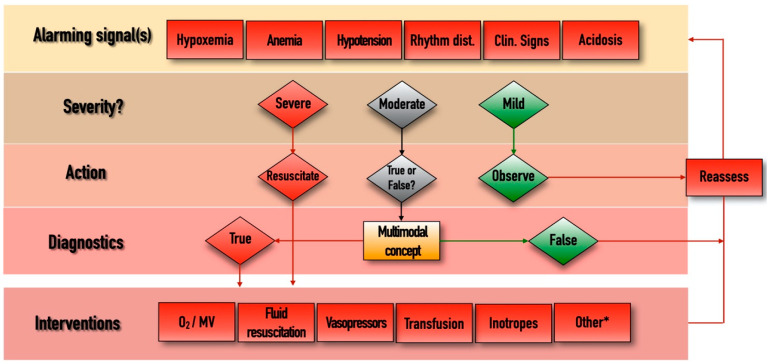
The management algorithm is summarized and explained in Figure 2. The most obvious interventions to stabilize patients include oxygen therapy/mechanical ventilation, fluid resuscitation, vasopressor and/or inotropic support, and blood transfusion. Sometimes other (*) measures may also be needed, such as fluid removal by hemofiltration, renal replacement therapy, or immunomodulation including pharmacological therapy or extracorporeal blood purification. Putting all pieces of this puzzle into context may help choose the best and most appropriate therapy for hemodynamically unstable critically ill patients.
Figure 2.
Management algorithm. Rhythm dist., cardiac rhythm disturbances; Clin, clinical; MV, mechanical ventilation. *, extracorporeal renal replacement therapies, immunomodulation, other adjuvant therapies. Whenever an “Alarming signal” is detected or suspected, the first step is to evaluate its “Severity”. If the signal is regarded as “Severe” (such as profound hypotension, extreme tachycardia, hypoxemia, etc.) then immediate resuscitation is needed in the form of the appropriate “Interventions”, after which the situation should be “Reassessed”, by checking the change in the alarming parameters and starting the loop again if necessary. If the alarm signal is regarded as “Mild”, then further observation and reassessment is enough. In cases of “Moderate” disturbances, when decisions cannot be made easily, the multimodal contextualized concept could become useful. This includes components listed in Figure 1, and putting these parameters in context can help us to determine whether the moderate alarm signal was indeed “True” or “False”. In cases of the presence of true pathology, the measures listed in the “Interventions” domain can be implemented, after which reassessment is again necessary.
Undoubtedly, this concept is certainly complicated, requires well-trained personnel, and the monitors and disposables can be invasive and costly. These circumstances, and the uncertainty reported in clinical trials, are the main reasons this approach has not gained worldwide popularity and has not become routine management. However, the spread of recently developed less invasive and especially the non-invasive technologies that enable real-time, continuous evaluation of cardiac dynamics may change the current situation.
4. Future Perspectives
With the recent shift from static (such as MAP, CO, CVP, global end-diastolic volume—GEDV, etc.) to dynamic measurements (especially pulse pressure or stroke volume variation) [44], there might be a bright future for non-invasive hemodynamic monitoring. With the improvement of sensors and the development of new methods (e.g., the pulse contour algorithms), completely non-invasive techniques have emerged, combining the advantages of non-invasiveness with the precision of new-generation devices [45]. However, results on the accuracy of these technologies are controversial [46].
With the help of pulse contour algorithms, stroke volume and cardiac output can be calculated from an arterial blood pressure curve [45]. Several methods are available for these measurements, such as finger cuffs using the volume clamp method [47], radial artery applanation tonometry [48], and noninvasive brachial pulse wave analysis by hydraulic coupling [49].
Bioimpedance and bioreactance use similar principles, based on the fact that the cardiac chambers are electrically isolated [50]. They have been known for a long time, but their use in hemodynamic monitoring still has some limitations. Nevertheless, several devices are available using these two methods [50].
With the partial CO2-rebreathing technique, one can estimate CO with an applied and modified Fick principle using expired CO2 as an indicator. The Fick principle assumes that the blood flow (i.e., CO) through the alveoli equals the elimination of CO2 (VCO2) divided by the difference in venous-to-arterial CO2 [51]. It was first applied only in sedated and ventilated patients and required invasive blood sampling. More recently, a non-invasive model was developed, but it resulted in several limitations, such as face mask leaks introducing measurement bias, dependency on a steady respiratory state, and the necessity of adjusting for atelectasis and shunts [50].
Pulse wave transit time measurements only require an electrocadiogram and a plethysmograph to detect the time delay between the R wave and the peripheral pulse wave. Although these devices have several advantages, they must be calibrated frequently, and the algorithms are not yet capable of accounting for individual differences [52]. Pulse wave velocity is known for measuring arterial stiffness but is also being tested for continuous blood pressure measurements as well. One must take into account that this measure is age-dependent due to the general increase of arterial stiffness over time [53].
The above-mentioned technologies are certainly promising, but it is important to emphasize that the data we have at present are not robust enough to come to firm conclusions on the efficacy and patient benefit. However, new technologies are on the horizon, including regional perfusion and metabolic monitoring. Apart from potential new sensors and devices, visualization and handling of data are also rapidly developing fields. The availability of cross-checking measurements through device connectivity and more informed decision making by better visualization of data may transform hemodynamic monitoring in the near future [45].
The predictive capabilities of machine learning and artificial intelligence have also been tested in the field of hemodynamic monitoring with promising results. Hatib et al. reported that their algorithm was able to predict hypotension from arterial waveforms 15 min earlier with 88% specificity and 87% sensitivity. Five minutes before the onset of hypotension, these values were 92% and 92% with a 0.97 area under the curve [54]. The algorithm proved to be superior to other hemodynamic measurements in patients undergoing major surgery [55]. Artificial intelligence has performed remarkably in decision making when tested on patients with sepsis. Those patients who received the amount of intravenous fluids and dose of vasopressors calculated with the artificial intelligence tool had the lowest mortality in the tested septic cohort [56]. However, there is a long road ahead until big data and artificial intelligence become a bedside tool to help decision making, but it is certainly something with great potential to improve care in the future.
5. Conclusions
Hemodynamic support remains the cornerstone in the management of the critically ill regardless of its cause. However, all resuscitation measures (fluids, catecholamines, blood, etc.) can have harmful effects if they are under- or over-used. Therefore, being the most effective and causing the least harm concurrently should be of utmost importance. Personalizing therapy is a very intriguing and promising approach and can help us to deliver “as much treatment as needed”. At the moment, it seems complicated, sometimes invasive and costly, but hopefully in the long run, new technologies will help us to make it our usual routine. Until then, this multimodal, contextualized approach provides an excellent training tool for junior doctors by helping them to unveil pathophysiology at the bedside and also to understand the rationale of their actions. By doing so, they will hopefully understand the utmost importance of personalized medicine while treating the critically ill.
Acknowledgments
The authors would like to thank Harriet Adamson for language editing the manuscript.
Author Contributions
The concept was developed by Z.M.; Section 3.1 was written by M.V.; Section 3.2 was written by T.L.; Section 4 was written by K.O.; figures were developed by M.R.; the rest of the text was written by Z.M. All authors have read and agreed to the published version of the manuscript.
Funding
Open access funding was provided by the University of Pécs. The research of the group has been funded in part by “GINOP-2.3.2-15-2016-00048—STAY ALIVE” co-financed by the European Union (European Regional Development Fund) within the framework of Program Széchenyi 2020 and by the Human Resources Development Operational Program Grant, Grant Number: EFOP 3.6.2-16-2017-00006—LIVE LONGER, which is co-financed by the European Union (European Regional Development Fund) within the framework of Program Széchenyi 2020.
Conflicts of Interest
Z.M. receives regular honoraria for being in the medical advisory board of Pulsion Medical Systems SE (Feldkirchen, Germany), and for lectures from Biotest AG (Dreieich, Germany) and Thermo Fisher Scientific (Berlin, Germany). He also acts as a Medical Director for CytoSorbents Europe GmbH (Berlin, Germany). The other authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jozwiak M., Silva S., Persichini R., Anguel N., Osman D., Richard C., Teboul J.L., Monnet X. Extra-Vascular Lung Water Is An Independent Prognostic Factor In Patients With Acute Respiratory Distress Syndrome. Crit. Care Med. 2012;41:472–480. doi: 10.1097/CCM.0b013e31826ab377. [DOI] [PubMed] [Google Scholar]
- 2.Vincent J.-L., Sakr Y., Sprung C.L., Ranieri V.M., Reinhart K., Gerlach H., Moreno R., Carlet J., Le Gall J.-R., Payen D. Sepsis in European intensive care units: Results of the SOAP study*. Crit. Care Med. 2006;34:344–353. doi: 10.1097/01.CCM.0000194725.48928.3A. [DOI] [PubMed] [Google Scholar]
- 3.Acheampong A.A., Vincent J.-L. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit. Care. 2015;19:1–7. doi: 10.1186/s13054-015-0970-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit. Care. 2015;19:S8. doi: 10.1186/cc14726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rivers E., Nguyen B., Havstad S., Ressler J., Muzzin A., Knoblich B., Peterson E., Tomlanovich M. Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock. N. Engl. J. Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 6.Mouncey P.R., Osborn T.M., Power G.S., Harrison D.A., Sadique M.Z., Grieve R.D., Jahan R., Harvey S.E., Bell D., Bion J.F., et al. Trial of Early, Goal-Directed Resuscitation for Septic Shock. N. Engl. J. Med. 2015;372:1301–1311. doi: 10.1056/NEJMoa1500896. [DOI] [PubMed] [Google Scholar]
- 7.Peake S.L., Delaney A., Bailey M., Bellomo R., Cameron P.A., Cooper D.J., Higgins A.M., Holdgate A., Howe B.D., Webb S.A.R., et al. Goal-directed resuscitation for patients with early septic shock. N. Engl. J. Med. 2014;371:1496–1506. doi: 10.1056/NEJMoa1404380. [DOI] [PubMed] [Google Scholar]
- 8.Yealy D.M., Kellum J.A., Huang D.T., Barnato A.E., Weissfeld L.A., Pike F., Terndrup T., Wang H.E., Hou P.C., LoVecchio F., et al. A randomized trial of protocol-based care for early septic shock. N. Engl. J. Med. 2014;370:1683–1693. doi: 10.1056/NEJMoa1401602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tánczos K.N.M., Molnár Z. Annual Update in Intensive Care and Emergency Medicine 2014. Springer; Berlin/Heidelberg, Germany: 2014. The Hemodynamic Puzzle: Solving the Impossible? [Google Scholar]
- 10.Cecconi M., Hofer C., Teboul J.L., Pettila V., Wilkman E., Molnar Z., del la Rocca G., Aldecoa C., Artigas A., Jog S., et al. Fluid challenges in intensive care: The FENICE study: A global inception cohort study. Intensive Care Med. 2015;41:1529–1537. doi: 10.1007/s00134-015-3850-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cecconi M., Hernandez G., Dunser M., Antonelli M., Baker T., Bakker J., Duranteau J., Einav S., Groeneveld A.B.J., Harris T., et al. Fluid administration for acute circulatory dys-function using basic monitoring: Narrative review and expert panel recommendations from an ESICM task force. Intensive Care Med. 2019;45:21–32. doi: 10.1007/s00134-018-5415-2. [DOI] [PubMed] [Google Scholar]
- 12.Singer M., Deutschman C.S., Seymour C.W., Shankar-Hari M., Annane D., Bauer M., Bellomo R., Bernard G.R., Chiche J.-D., Coopersmith C.M., et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bone R.C., Fisher C.J., Jr., Clemmer T.P., Slotman G.J., Metz C.A., Balk R.A. Sepsis syndrome: A valid clinical entity. Methylpred-nisolone Severe Sepsis Study Group. Crit. Care Med. 1989;17:389–393. doi: 10.1097/00003246-198905000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Hotchkiss R.S., Monneret G., Payen D. Sepsis-induced immunosuppression: From cellular dysfunctions to immunotherapy. Nat. Rev. Immunol. 2013;13:862–874. doi: 10.1038/nri3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molnar Z., Bakker J. Attenuating hyperinflammation in COVID-19: A change in paradigm? J. Crit. Care. 2020;60:334–336. doi: 10.1016/j.jcrc.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhodes A.A., Evans L.E., Alhazzani W., Levy M.M., Antonelli M., Ferrer R., Kumar A., Sevransky J.E., Sprung C.L., Nunnally M.E., et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 17.Dellinger R.P., Levy M.M., Rhodes A., Annane D., Gerlach H., Opal S.M., Sevransky J.E., Sprung C.L., Douglas I.S., Jaeschke R., et al. Surviving Sepsis Campaign: International Guide-lines for Management of Severe Sepsis and Septic Shock, 2012. Intensive Care Med. 2013;39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shankar-Hari M., Phillips G.S., Levy M.L., Seymour C.W., Liu V.X., Deutschman C.S., Angus D.C., Rubenfeld G.D., Singer M., Force S.D.T. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:775–787. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Beest P., Wietasch G., Scheeren T., Spronk P., Kuiper M. Clinical review: Use of venous oxygen saturations as a goal—A yet unfinished puzzle. Crit. Care. 2011;15:232. doi: 10.1186/cc10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pope J.V., Jones A.E., Gaieski D.F., Arnold R.C., Trzeciak S., Shapiro N.I. Multicenter Study of Central Venous Oxygen Saturation (ScvO2) as a Predictor of Mortality in Patients With Sepsis. Ann. Emerg. Med. 2010;55:40–46.e1. doi: 10.1016/j.annemergmed.2009.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gattinoni L., Vasques F., Camporota L., Meessen J., Romitti F., Pasticci I., Duscio E., Vassalli F., Forni L.G., Payen D., et al. Understanding Lactatemia in Human Sepsis. Potential Impact for Early Management. Am. J. Respir. Crit. Care Med. 2019;200:582–589. doi: 10.1164/rccm.201812-2342OC. [DOI] [PubMed] [Google Scholar]
- 22.Protti A., Masson S., Latini R., Fumagalli R., Romero M., Pessina C., Pasetti G., Tognoni G., Pesenti A., Gattinoni L., et al. Persistence of Central Venous Oxygen Desaturation during Early Sepsis Is Associated With Higher Mortality: A Retrospective Analysis of the ALBIOS Trial. Chest. 2018;154:1291–1300. doi: 10.1016/j.chest.2018.04.043. [DOI] [PubMed] [Google Scholar]
- 23.Ince C., Sinaasappel M. Microcirculatory oxygenation and shunting in sepsis and shock. Crit. Care Med. 1999;27:1369–1377. doi: 10.1097/00003246-199907000-00031. [DOI] [PubMed] [Google Scholar]
- 24.Wittayachamnankul B., Apaijai N., Sutham K., Chenthanakij B., Liwsrisakun C., Jaiwongkam T., Chattipakorn S.C., Chattipakorn N. High central venous oxygen saturation is associated with mitochondrial dysfunction in septic shock: A prospective observational study. J. Cell. Mol. Med. 2020;24:6485–6494. doi: 10.1111/jcmm.15299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferreruela M., Raurich J.M., Ayestarán I., Llompart-Pou J.A. Hyperlactatemia in ICU patients: Incidence, causes and associated mortality. J. Crit. Care. 2017;42:200–205. doi: 10.1016/j.jcrc.2017.07.039. [DOI] [PubMed] [Google Scholar]
- 26.Casserly B., Phillips G.S., Schorr C., Dellinger R.P., Townsend S.R., Osborn T.M., Reinhart K., Selvakumar N., Levy M.M. Lactate measurements in sepsis-induced tissue hypoperfusion: Results from the Surviving Sepsis Campaign database. Crit. Care Med. 2015;43:567–573. doi: 10.1097/CCM.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 27.Garcia-Alvarez M., Marik P., Bellomo R. Sepsis-associated hyperlactatemia. Crit. Care. 2014;18:1–11. doi: 10.1186/s13054-014-0503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bisarya R., Shaath D., Pirzad A., Satterwhite L., He J., Simpson S.Q. Serum lactate poorly predicts central venous oxygen satu-ration in critically ill patients: A retrospective cohort study. J. Intensive Care. 2019;7:47. doi: 10.1186/s40560-019-0401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lamia B., Monnet X., Teboul J.L. Meaning of arterio-venous PCO2 difference in circulatory shock. Minerva Anestesiol. 2006;72:597–604. [PubMed] [Google Scholar]
- 30.Al Duhailib Z., Hegazy A.F., Lalli R., Fiorini K., Priestap F., Iansavichene A., Slessarev M. The Use of Central Venous to Arterial Carbon Dioxide Tension Gap for Outcome Prediction in Critically Ill Patients: A Systematic Review and Meta-Analysis. Crit. Care Med. 2020;48:1855–1861. doi: 10.1097/CCM.0000000000004578. [DOI] [PubMed] [Google Scholar]
- 31.Lima A., Jansen T.C., Van Bommel J., Ince C., Bakker J. The prognostic value of the subjective assessment of peripheral perfusion in critically ill patients. Crit. Care Med. 2009;37:934–938. doi: 10.1097/CCM.0b013e31819869db. [DOI] [PubMed] [Google Scholar]
- 32.Lara B., Enberg L., Ortega M., Leon P., Kripper C., Aguilera P., Kattan E., Castro R., Bakker J., Hernandez G. Capillary refill time during fluid resuscitation in patients with sepsis-related hyperlactatemia at the emergency department is related to mortality. PLoS ONE. 2017;12:e0188548. doi: 10.1371/journal.pone.0188548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hernández G., Ospina-Tascón G.A., Damiani L.P., Estenssoro E., Dubin A., Hurtado J., Friedman G., Castro R., Alegría L., Teboul J., et al. Effect of a Resuscitation Strategy Targeting Peripheral Perfusion Status vs Serum Lactate Levels on 28-Day Mortality among Patients with Septic Shock: The ANDROMEDA-SHOCK Randomized Clinical Trial. JAMA. 2019;321:654–664. doi: 10.1001/jama.2019.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Castro R., Kattan E., Ferri G., Pairumani R., Valenzuela E.D., Alegría L., Oviedo V., Pavez N., Soto D., Vera M., et al. Effects of capillary refill time-vs. lactate-targeted fluid resuscitation on regional, microcirculatory and hypoxia-related perfusion parameters in septic shock: A randomized controlled trial. Ann. Intensive Care. 2020;10:150. doi: 10.1186/s13613-020-00767-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ait-Oufella H., Lemoinne S., Boelle P.Y., Galbois A., Baudel J.L., Lemant J., Joffre J., Margetis D., Guidet B., Maury E., et al. Mottling score predicts survival in septic shock. Intensive Care Med. 2011;37:801–807. doi: 10.1007/s00134-011-2163-y. [DOI] [PubMed] [Google Scholar]
- 36.Dumas G., Lavillegrand J.-R., Joffre J., Bigé N., De-Moura E.B., Baudel J.-L., Chevret S., Guidet B., Maury E., Amorim F., et al. Mottling score is a strong predictor of 14-day mortality in septic patients whatever vasopressor doses and other tissue perfusion parameters. Crit. Care. 2019;23:1–9. doi: 10.1186/s13054-019-2496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pinsky M.R. Functional Hemodynamic Monitoring. Crit. Care Clin. 2015;31:89–111. doi: 10.1016/j.ccc.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cronhjort M., Wall O., Nyberg E., Zeng R., Svensen C., Mårtensson J., Joelsson-Alm E. Impact of hemodynamic goal-directed resuscitation on mortality in adult critically ill patients: A systematic review and meta-analysis. J. Clin. Monit. 2017;32:403–414. doi: 10.1007/s10877-017-0032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saugel B., Michard F., Scheeren T.W.L. Goal-directed therapy: Hit early and personalize! J. Clin. Monit. 2017;32:375–377. doi: 10.1007/s10877-017-0043-x. [DOI] [PubMed] [Google Scholar]
- 40.Vignon P., Begot E., Mari A., Silva S., Chimot L., Delour P., Vargas F., Filloux B., Vandroux D., Jabot J., et al. Hemodynamic Assessment of Patients With Septic Shock Using Transpulmonary Thermodilution and Critical Care Echocardiography: A Comparative Study. Chest. 2018;153:55–64. doi: 10.1016/j.chest.2017.08.022. [DOI] [PubMed] [Google Scholar]
- 41.Rajaram S.S., Desai N.K., Kalra A., Gajera M., Cavanaugh S.K., Brampton W., Young D., Harvey S., Rowan K. Pulmonary artery catheters for adult patients in intensive care. Cochrane Database Syst. Rev. 2013;2013:CD003408. doi: 10.1002/14651858.CD003408.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Trof R.J., Beishuizen A., Cornet A.D., de Wit R.J., Girbes A.R., Groeneveld A.B. Volume-limited versus pressure-limited hemo-dynamic management in septic and nonseptic shock. Crit. Care Med. 2012;40:1177–1185. doi: 10.1097/CCM.0b013e31823bc5f9. [DOI] [PubMed] [Google Scholar]
- 43.Molnar Z., Benes J., Saugel B. Intraoperative hypotension is just the tip of the iceberg: A call for multimodal, individualised, contextualised management of intraoperative cardiovascular dynamics. Br. J. Anaesth. 2020;125:419–423. doi: 10.1016/j.bja.2020.05.048. [DOI] [PubMed] [Google Scholar]
- 44.Scheeren T.W., Ramsay M.A. New Developments in Hemodynamic Monitoring. J. Cardiothorac. Vasc. Anesth. 2019;33:S67–S72. doi: 10.1053/j.jvca.2019.03.043. [DOI] [PubMed] [Google Scholar]
- 45.Michard F. Hemodynamic monitoring in the era of digital health. Ann. Intensive Care. 2016;6:15. doi: 10.1186/s13613-016-0119-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Joosten A., Desebbe O., Suehiro K., Murphy L.-L., Essiet M., Alexander B., Fischer M.-O., Barvais L., Van Obbergh L., Maucort-Boulch D., et al. Accuracy and precision of non-invasive cardiac output monitoring devices in perioperative medicine: A systematic review and meta-analysis † †This Article is accompanied by Editorial Aew442. Br. J. Anaesth. 2017;118:298–310. doi: 10.1093/bja/aew461. [DOI] [PubMed] [Google Scholar]
- 47.Wagner J.Y., Negulescu I., Schöfthaler M., Hapfelmeier A., Meidert A.S., Huber W., Schmid R.M., Saugel B. Continuous noninvasive arterial pressure measurement using the volume clamp method: An evaluation of the CNAP device in intensive care unit patients. J. Clin. Monit. 2015;29:807–813. doi: 10.1007/s10877-015-9670-2. [DOI] [PubMed] [Google Scholar]
- 48.Wagner J.Y., Sarwari H., Schön G., Kubik M., Kluge S., Reichenspurner H., Reuter D.A., Saugel B. Radial Artery Applanation Tonometry for Continuous Noninvasive Cardiac Output Measurement: A Comparison with Intermittent Pulmonary Artery Thermodilution in Patients After Cardiothoracic Surgery. Crit. Care Med. 2015;43:1423–1428. doi: 10.1097/CCM.0000000000000979. [DOI] [PubMed] [Google Scholar]
- 49.Saugel B., Kouz K., Sessler D.I. Hydraulic Coupling: A New Method for Noninvasive Intermittent Blood Pressure Monitoring. Anesthesiology. 2020;133:964–966. doi: 10.1097/ALN.0000000000003530. [DOI] [PubMed] [Google Scholar]
- 50.Nguyen L.S., Squara P. Non-Invasive Monitoring of Cardiac Output in Critical Care Medicine. Front. Med. 2017;4:200. doi: 10.3389/fmed.2017.00200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jaffe M.B. Partial CO2 rebreathing cardiac output–operating principles of the NICO system. J. Clin. Monit. Comput. 1999;15:387–401. doi: 10.1023/A:1009981313076. [DOI] [PubMed] [Google Scholar]
- 52.Sinha A., Singh P.M., Grewal N., Aman M., Dubowitz G. Comparison between continuous non-invasive estimated cardiac output by pulse wave transit time and thermodilution method. Ann. Card. Anaesth. 2014;17:273. doi: 10.4103/0971-9784.142059. [DOI] [PubMed] [Google Scholar]
- 53.Peter L., Noury N., Černý M. A review of methods for non-invasive and continuous blood pressure monitoring: Pulse transit time method is promising? IRBM. 2014;35:271–282. doi: 10.1016/j.irbm.2014.07.002. [DOI] [Google Scholar]
- 54.Hatib F., Jian Z., Buddi S., Lee C., Settels J., Sibert K., Rinehart J., Cannesson M. Machine-learning Algorithm to Predict Hypotension Based on High-fidelity Arterial Pressure Waveform Analysis. Anesthesiology. 2018;129:663–674. doi: 10.1097/ALN.0000000000002300. [DOI] [PubMed] [Google Scholar]
- 55.Davies S.J., Vistisen S.T., Jian Z., Hatib F., Scheeren T.W.L. Ability of an Arterial Waveform Analysis–Derived Hypotension Prediction Index to Predict Future Hypotensive Events in Surgical Patients. Anesth. Analg. 2020;130:352–359. doi: 10.1213/ANE.0000000000004121. [DOI] [PubMed] [Google Scholar]
- 56.Komorowski M., Celi L.A., Badawi O., Gordon A.C., Faisal A.A. The Artificial Intelligence Clinician learns optimal treatment strategies for sepsis in intensive care. Nat. Med. 2018;24:1716–1720. doi: 10.1038/s41591-018-0213-5. [DOI] [PubMed] [Google Scholar]