Abstract
Study Objectives:
Obstructive sleep apnea (OSA) is prevalent among older adults. Although treatment with positive airway pressure (PAP) lowers subsequent morbidity, PAP adherence is inconsistent. Socioeconomic disparities have been observed in OSA treatment, but regional differences in OSA care are unknown. This study examined geographic variations in PAP treatment and adherence among older Americans.
Methods:
This study utilized a representative 5% sample of all Medicare fee-for-service beneficiaries aged 65+ years. An OSA diagnosis, treatment, and PAP adherence were confirmed with International Classification of Diseases, Ninth Revision, HCPCS (Health Care Common Procedure Coding System) codes, and ≥2 HCPCS claims for PAP supplies respectively. Descriptive statistics were used to examine proportions of Medicare beneficiaries who obtained and adhered to PAP. Maps described the proportion of treated and adherent beneficiaries by state and hospital referral region.
Results:
For state-level data, PAP treatment and adherence proportions among beneficiaries with an OSA diagnosis ranged between 54–87% and 59–81%, respectively. Proportions of treated patients were higher in Midwest states (>80%), in comparison to Northwest, Northeast, and Southern states (<73%). Southern states and California had lowest proportions of PAP adherence (<70%). Within-state variability in treatment patterns were apparent along the East and West coasts. Correlations of PAP treatment and adherence proportions were low in Washington, DC, New York, and New Jersey. Discordant treatment and adherence proportions were observed in Alabama and Mississippi.
Conclusions:
Significant state-level and regional disparities of PAP treatment and adherence among Medicare beneficiaries with OSA suggest gaps in delivery of OSA care for older Americans.
Citation:
Dunietz GL, Yu Y, Levine RS, et al. Obstructive sleep apnea in older adults: geographic disparities in PAP treatment and adherence. J Clin Sleep Med. 2021;17(3):421–427.
Keywords: obstructive sleep apnea, CPAP, geographical disparities, health care disparities, treatment, adherence, older adults, Medicare
BRIEF SUMMARY
Current Knowledge/Study Rationale: Treatment of obstructive sleep apnea and treatment adherence have been associated with socioeconomic position and demographic characteristics. Data on geographical differences in obstructive sleep apnea care are limited.
Study Impact: This study conducted spatial analyses to examine between- and within-state differences in proportions of positive airway pressure treatment and treatment adherence in a representative sample of US older adults diagnosed with obstructive sleep apnea. Our findings suggest significant geographic disparities in positive airway pressure treatment and treatment adherence and highlight regional gaps in delivery of obstructive sleep apnea care in older adults.
INTRODUCTION
Obstructive sleep apnea (OSA) affects at least one-quarter of older adults in the United States1 and negatively impacts health and quality of life.2,3 Although positive airway pressure (PAP) treatment has potential to reduce subsequent morbidity,4–6 adherence to PAP treatment is inconsistent.7,8 In older adults with OSA, the proportions of PAP treated and PAP adherent are estimated between 60% and 73%.9–11 Sociodemographic and health factors have been linked to OSA treatment gaps,10,12,13 but data on regional OSA disparities in the United States are scarce.14
Geographic differences have been reported in other chronic conditions such as metabolic syndrome and stroke recurrence and mortality, with the highest burden observed in central US states, the Southeast, and the Northeast, respectively.15–17 Treatment of cardiovascular disease and prostate cancer, as well as adherence to hypertension, diabetes, and hyperlipidemia therapies, provide just a few examples of apparent variations across US regions.18–21
Examination of regional patterns in OSA treatment and subsequent adherence could identify gaps and inform strategies to improve OSA care in the United States.
This study utilized the large and nationally representative Medicare Fee-for-Service database to examine patterns of OSA treatment, and adherence to treatment, among older adults by state and hospital referral region.
METHODS
Study participants
A 5% random sample of Medicare beneficiaries (n = 2,758,197) from the Medicare Beneficiary Summary File (2013) was used to identify US older adults, aged 65 years or older, who were enrolled in Medicare fee-for-service. This sample was further restricted to older adults who carried a diagnosis of OSA, defined by at least 1 ICD-9 (International Classification of Diseases, Ninth Revision) code in any position in the Medicare carrier file (n = 102,618).
PAP treatment and adherence
Medicare beneficiaries were classified as treated with PAP if an initial prescription for PAP equipment (at least 1 PAP HCPCS [Health Care Common Procedure Coding System] code for PAP machine or supplies) was present in the Medicare Durable Medical Equipment file. These HCPCS codes are unique for PAP equipment (Table S1 (285.5KB, pdf) in the supplemental material). Treatment adherence was defined by the presence of at least 2 HCPCS claims for PAP supplies (filters, cushions, masks, or tubing) separated by at least 1 month over the course of the claims study period. The definition of 2 or more equipment claims across 3 years as adherence proxy aligns with the validated threshold of 0.7 refills per year that discriminates between adherent and nonadherent adults with OSA, using the Medicare adherence definition of 4 or more hours per night, at least 70% of nights.22
Statistical analysis
Descriptive statistics were used to examine the demographic characteristics of Medicare beneficiaries with OSA. We estimated state-specific proportions of Medicare beneficiaries with OSA who obtained PAP treatment, and of those who adhered to their treatment. These proportions were described as quintile categories in 2 maps created using procedures in ArcGIS software (Esri, Redlands, California, USA). To examine more granular regional variations, we created 2 maps that represented Hospital Referral Region (HRR)–specific proportions of treated beneficiaries among those diagnosed and adherent beneficiaries among those treated. HRRs defined as regional health care markets, are widely used in studies of geographic variation.23,24 These regions cross borders of states, counties, and municipalities.25 Finally, we used scatterplots to identify the relationship between proportions of PAP treatment and adherence, by state. All study procedures were approved by the University of Michigan Institutional Review Board.
RESULTS
In this sample of 102,618 older adults with an OSA diagnosis, 57% were men and 43% were women. More than 60% were younger than 75 years. Whites represented nearly 90% of the sample (Table 1).
Table 1.
Demographic characteristics among 102,618 Medicare beneficiaries with obstructive sleep apnea, 2011–2013.
| Demographic and Health Characteristics | Total Sample (n = 102,618) | PAP Treated (n = 74,737) | PAP Adherent (n = 53,610) |
|---|---|---|---|
| Sex | |||
| Men | 58,293 (57) | 44,369 (59) | 32,341 (60) |
| Women | 44,325 (43) | 30,368 (41) | 21,269 (40) |
| Age | |||
| 65–69 years | 36,010 (35) | 26,336 (35) | 18,449 (34) |
| 70–74 years | 29,540 (29) | 21,977 (29) | 16,197 (30) |
| 75–79 years | 19,543 (19) | 14,347 (19) | 10,479 (20) |
| 80–84 years | 11,376 (11) | 8,097 (11) | 5,780 (11) |
| 85–89 years | 4,830 (5) | 3,225 (4) | 2,198 (4) |
| ≥90 years | 1,319 (1) | 755 (1) | 507 (1) |
| Race/ethnicity | |||
| Non-Hispanic White | 91,040 (89) | 67,031 (90) | 48,855 (91) |
| Non-Hispanic Black | 7,319 (7) | 5,019 (7) | 3,113 (6) |
| Hispanic | 1,267 (1) | 749 (1) | 375 (1) |
| Asian | 923 (1) | 514 (1) | 318 (1) |
| Other | 2,069 (2) | 1,424 (2) | 949 (2) |
Data are presented as n (%). Proportions are rounded to the nearest integer. “Other” race/ethnicity includes Pacific Islander and Native American. PAP = positive airway pressure.
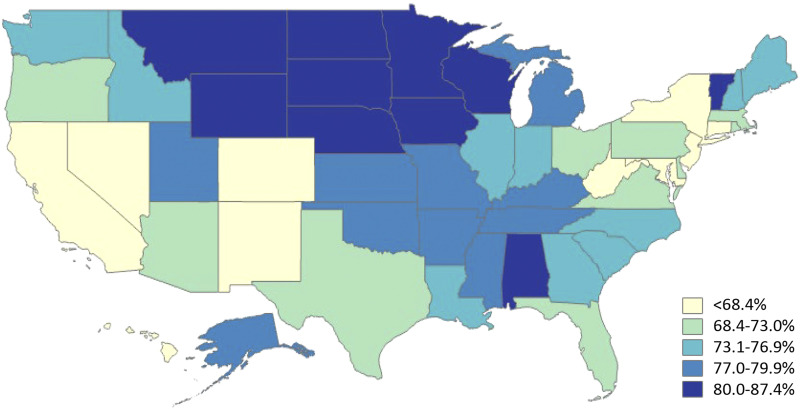
In state-level data, the proportion of PAP-treated and PAP-adherent beneficiaries with an OSA diagnosis ranged between 54–87% and 59–81%, respectively. Higher proportions of beneficiaries treated with PAP (>80%) were observed in the Midwest states of North and South Dakota, Minnesota, Nebraska, Iowa, as well as Wyoming and Hawaii. Of these states, North Dakota had the highest proportion treated with PAP (>87%). PAP treatment proportions were lower (<69%) in western states and the Northeast, including California, Nevada, Colorado, New Mexico, New York, and Alabama.
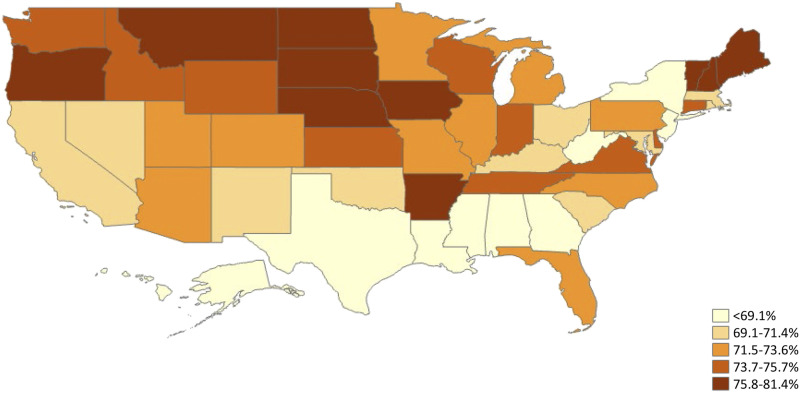
Adherence to PAP treatment showed somehow similar geographic patterns, as higher proportions were noted in New England and the Midwest and lower proportions in the mid-Atlantic and southern states (Figure 1 and Figure 2).
Figure 1. State-level proportions of PAP treatment among Medicare beneficiaries with obstructive sleep apnea.
PAP = positive airway pressure.
Figure 2. State-level proportions of adherence to PAP treatment among Medicare beneficiaries with obstructive sleep apnea.
PAP = positive airway pressure.
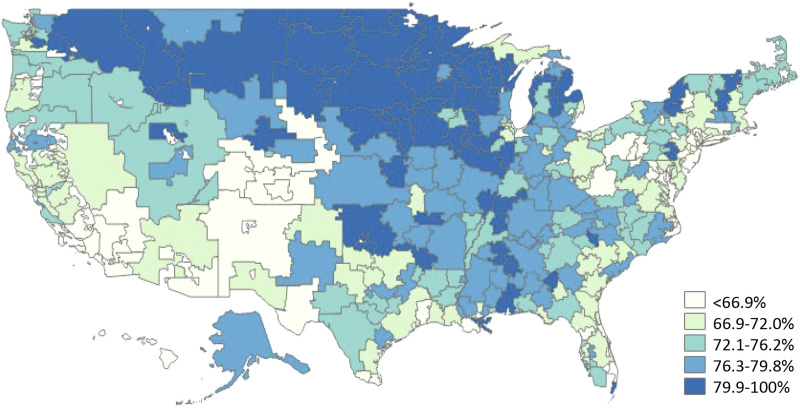
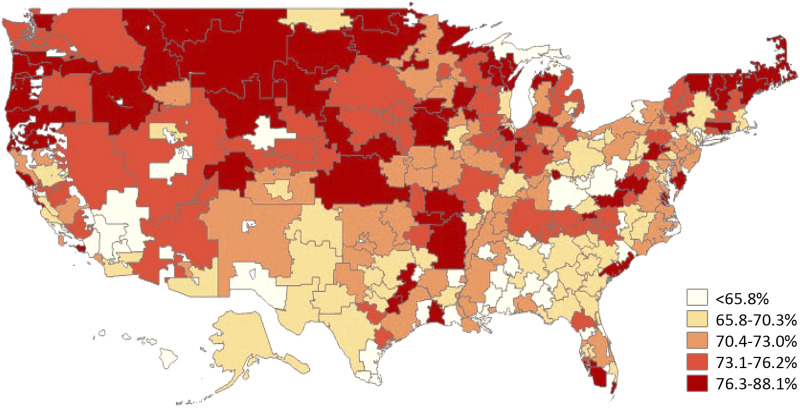
Analysis by HRR patterns of PAP treatment and treatment adherence showed minimal within-state variability in upper midwestern and mountain states, such as the Dakotas and Montana. However, higher variations in PAP treatment and treatment adherence were observed in eastern and southern states, as well as in California (Figure 3 and Figure 4).
Figure 3. HRR-level proportions of PAP treatment among Medicare beneficiaries with obstructive sleep apnea.
HRR = Hospital Referral Region; PAP = positive airway pressure.
Figure 4. HRR-level proportions of adherence to PAP treatment among Medicare beneficiaries with obstructive sleep apnea.
HRR = Hospital Referral Region; PAP = positive airway pressure.
State-level scatterplots showed that PAP treatment and adherence were linearly correlated. Montana and Vermont were among the states with the highest proportion of Medicare beneficiaries who were both treated for OSA and adhered to PAP. The southern states of Mississippi and Alabama had the highest discordance between proportions of treatment and treatment adherence with 80% of PAP treatment vs less than 70% adherence. Concordantly, low proportions of PAP treatment and adherence were apparent in Washington, DC (Figure 5).
Figure 5. Scatterplot of PAP treatment and adherence proportions by state among Medicare beneficiaries with obstructive sleep apnea.
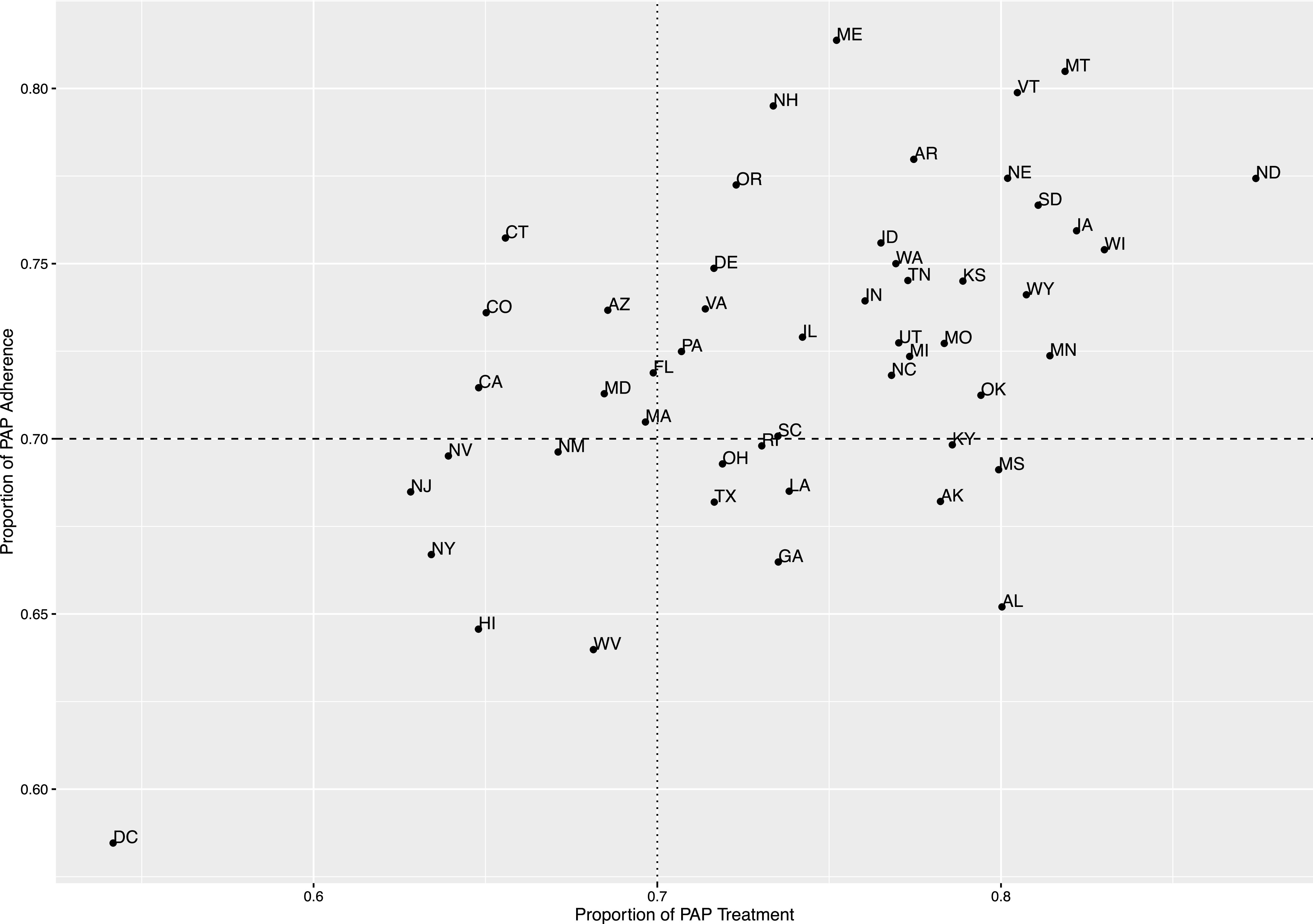
PAP = positive airway pressure.
DISCUSSION
This analysis of a nationally representative sample of Medicare beneficiaries aged 65 and older with OSA suggests substantial variation in both treatment and adherence, at the state and HRR levels. A positive, linear correlation between state-level proportions of OSA treatment and treatment adherence was apparent. These data provide new insight into US regions that may be vulnerable to gaps in OSA care for older Americans. For example, in general, northern Midwest and central mountain states had relatively high rates of treatment and adherence, whereas southwestern states and some mid-Atlantic states had relatively low rates.
To date, national-level patterns of PAP therapy and treatment adherence among OSA-diagnosed patients have been largely unexplored. The observed variations in PAP treatment patterns in this study are a first step in understanding the greatest areas of need to improve sleep health care delivery for older patients with OSA.
Gaps in OSA care could be attributed to state-level demographic variations. While age distributions were similar in states with high and low treatment and PAP-adherence proportions, racial differences were apparent. States with higher vs lower proportions of PAP treatment patterns are predominantly White, with lower racial and ethnic diversity. For example, Medicare beneficiaries who reside in North Dakota, Wisconsin, Maine, Montana, and Vermont—overwhelmingly White states (95%)—had higher proportions of treatment and treatment adherence in comparison to more racially and ethnically diverse areas such as Washington, DC, and Hawaii. Although socioeconomic position, urbanicity, and access to accredited sleep centers could also explain variation in OSA care, these data were not available for our analyses. Detailed nationwide study with individual-level information is needed to examine the potential influence of geographic variations in sociodemographic factors and sleep care access on OSA treatment in older adults.
It should be noted that, while this sample is representative of OSA-diagnosed Medicare beneficiaries, its racial/ethnic distribution differs in comparison to the general Medicare population. For example, White Medicare beneficiaries with an OSA diagnosis accounted for 89% of the sample; yet, the fraction of Whites more generally in the Medicare population is 75%. Similarly, Hispanics with OSA represented 1% of this sample vs 10% in the Medicare population. Prior reports have identified rates of OSA among Hispanics in the United States exceeding those of non-Hispanic Whites.26 Therefore, the racial/ethnic differences between our sample and the general Medicare population may well highlight racial/ethnic disparities in recognition of OSA among older adults as well.
The reported treatment proportions could be influenced by underlying, state-specific OSA prevalence, and therefore may not entirely reflect success in identification and treatment of Medicare beneficiaries with OSA. In post hoc analyses, we found state-specific prevalence of OSA to be extremely low, less than 1% across the board, in comparison to estimated prevalence of approximately 7% among older populations.27 This suggests that widespread underrecognition of OSA in Medicare beneficiaries, a finding that we also observed in a prior study,28 is likely a larger issue than is regional variation in recognition of OSA.
This descriptive study has several limitations. First, the use of 2 or more Medicare claims for PAP equipment, as a surrogate measure for treatment adherence, may not be sufficiently specific. This could result in some overestimation of participants as adherent. Nonetheless, a study composed of 220 patients with OSA found a PAP equipment claim rate of at least 0.7 claims per year to be a good predictor for long-term PAP adherence.22 Conversely, beneficiaries who decided to seek alternative treatments for OSA (such as a dental appliance or surgery) or those who purchased PAP equipment out-of-pocket could have been misclassified in our analyses as nonadherent. It is also possible that some beneficiaries remained adherent but did not refill their PAP supplies on a regular basis. A known limitation of Medicare data is the lack of measurable socioeconomic indicators, cohabitation, or neighborhood characteristics, linked to PAP treatment.29–32 Finally, this sample of older adults was predominantly White (89%) and adjustment for race/ethnicity would have minimal impact on the reported findings.
This study has several strengths. Utilization of nationally representative data of Medicare beneficiaries allows description of both state and HRR-level disparities in patterns of OSA treatment among older adults with OSA. The high sensitivity of ICD-9 codes for OSA diagnosis is another strength.33 Although informative for national decision making, examinations of state-level data create crude geographic aggregates that average regions within a state with optimal and poor access to OSA care. The present analysis of HRR-level PAP treatment and adherence patterns provided more precise geographic information and highlighted within-state variations in OSA care.
In short, significant state- and HRR-level geographic variations in PAP treatment and treatment adherence appear to exist, at least among older Medicare beneficiaries with OSA. These geographic disparities could inform future efforts to enhance regional health care delivery for older adults in the United States. Recent technological advances allow robust asynchronous telemedicine monitoring for continuous positive airway pressure adherence. These and other technological innovations may offer opportunities to ameliorate regional disparities in OSA treatment.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Work for this study was performed at the University of Michigan. This study was funded by the American Sleep Medicine Foundation Strategic Research Award 115-SR-15 (principal investigator: Dr. Braley). Dr. Braley is the principal investigator for studies funded by the National Multiple Sclerosis Society (RG5280-A-2) and the Patient-Centered Outcomes Research Institute (MS-1610-36980). She is named in a patent, held by the University of Michigan, concerning treatment for sleep apnea. She is site principal investigator for several industry-funded studies of MS immunotherapeutics at the University of Michigan (sponsors include Genzyme-Sanofi and Genentech-Roche). Dr. Chervin has received research support from the National Institutes of Health R01 HL105999 and U01 NS099043. He is named in or has developed patented and copyrighted materials owned by the University of Michigan and designed to assist with assessment or treatment of sleep disorders. He served on the boards of the American Academy of Sleep Medicine; Associated Professional Sleep Societies; American Board of Sleep Medicine; American Academy of Sleep Medicine Foundation (which funded the current research); International Pediatric Sleep Society; and the nonprofit Sweet Dreamzzz. He is an editor for UpToDate, has edited a book for Cambridge University Press, and has consulted for Zansors; Dr. Burke is funded by National Institutes of Health R01s AG059733 and MD008879. Mr. Conceicao is the Deputy Director of Science Debate, Inc, a 501(c)3 nonprofit. The authors report no conflicts of interest.
SUPPLEMENTARY MATERIAL
ACKNOWLEDGMENTS
The authors thank Chun Chieh Lin for her contribution to spatial analyses.
ABBREVIATIONS
- HRR
Hospital Referral Region
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
REFERENCES
- 1.Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O. Sleep-disordered breathing in community-dwelling elderly. Sleep. 1991;14(6):486–495. 10.1093/sleep/14.6.486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silva GE, Goodwin JL, Vana KD, Quan SF. Obstructive sleep apnea and quality of life: comparison of the SAQLI, FOSQ, and SF-36 questionnaires. Southwest J Pulm Crit Care. 2016;13(3):137–149. 10.13175/swjpcc082-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gozal D, Kheirandish-Gozal L. Cardiovascular morbidity in obstructive sleep apnea: oxidative stress, inflammation, and much more. Am J Respir Crit Care Med. 2008;177(4):369–375. 10.1164/rccm.200608-1190PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Avlonitou E, Kapsimalis F, Varouchakis G, Vardavas CI, Behrakis P. Adherence to CPAP therapy improves quality of life and reduces symptoms among obstructive sleep apnea syndrome patients. Sleep Breath. 2012;16(2):563–569. 10.1007/s11325-011-0543-8 [DOI] [PubMed] [Google Scholar]
- 5.Kakkar RK, Berry RB. Positive airway pressure treatment for obstructive sleep apnea. Chest. 2007;132(3):1057–1072. 10.1378/chest.06-2432 [DOI] [PubMed] [Google Scholar]
- 6.Chotinaiwattarakul W, O’Brien LM, Fan L, Chervin RD. Fatigue, tiredness, and lack of energy improve with treatment for OSA. J Clin Sleep Med. 2009;5(3):222–227. 10.5664/jcsm.27490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–356. 10.1016/j.smrv.2011.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collard P, Pieters T, Aubert G, Delguste P, Rodenstein DO. Compliance with nasal CPAP in obstructive sleep apnea patients. Sleep Med Rev. 1997;1(1):33–44. 10.1016/S1087-0792(97)90004-6 [DOI] [PubMed] [Google Scholar]
- 9.Russo-Magno P, O’Brien A, Panciera T, Rounds S. Compliance with CPAP therapy in older men with obstructive sleep apnea. J Am Geriatr Soc. 2001;49(9):1205–1211. 10.1046/j.1532-5415.2001.49238.x [DOI] [PubMed] [Google Scholar]
- 10.Dunietz GL, Chervin RD, Burke JF, Braley TJ. Obstructive sleep apnea treatment disparities among older adults with neurological disorders. Sleep Health. 2020;6(4):534–540. 10.1016/j.sleh.2020.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Posadas T, Oscullo G, Zaldívar E, et al. Treatment with CPAP in elderly patients with obstructive sleep apnoea. J Clin Med. 2020;9(2):E546. 10.3390/jcm9020546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandey A, Mereddy S, Combs D, et al. Socioeconomic inequities in adherence to positive airway pressure therapy in population-level analysis. J Clin Med. 2020;9(2):442. 10.3390/jcm9020442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsu N, Zeidler MR, Ryden AM, Fung CH. Racial disparities in positive airway pressure therapy adherence among veterans with obstructive sleep apnea. J Clin Sleep Med. 2020;16(8):1249–1254. 10.5664/jcsm.8476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee W, Nagubadi S, Kryger MH, Mokhlesi B. Epidemiology of obstructive sleep apnea: a population-based perspective. Expert Rev Respir Med. 2008;2(3):349–364. 10.1586/17476348.2.3.349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gurka MJ, Filipp SL, DeBoer MD. Geographical variation in the prevalence of obesity, metabolic syndrome, and diabetes among US adults. Nutr Diabetes. 2018;8(1):14. 10.1038/s41387-018-0024-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lanska DJ, Kuller LHJS. The geography of stroke mortality in the United States and the concept of a stroke belt. Stroke. 1995;26(7):1145–1149. 10.1161/01.STR.26.7.1145 [DOI] [PubMed] [Google Scholar]
- 17.Allen NB, Holford TR, Bracken MB, et al. Geographic variation in one-year recurrent ischemic stroke rates for elderly Medicare beneficiaries in the USA. Neuroepidemiology. 2010;34(2):123–129. 10.1159/000274804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Couto JE, Panchal JM, Lal LS, et al. Geographic variation in medication adherence in commercial and Medicare part D populations. J Manag Care Spec Pharm. 2014;20(8):834–842. 10.18553/jmcp.2014.20.8.834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Connor GT, Quinton HB, Traven ND, et al. Geographic variation in the treatment of acute myocardial infarction: the Cooperative Cardiovascular Project. JAMA. 1999;281(7):627–633. 10.1001/jama.281.7.627 [DOI] [PubMed] [Google Scholar]
- 20.Sporer SM, Weinstein JN, Koval KJJ. The geographic incidence and treatment variation of common fractures of elderly patients. J Am Acad Orthop Surg. 2006;14(4):246–255. 10.5435/00124635-200604000-00006 [DOI] [PubMed] [Google Scholar]
- 21.Cary KC, Punnen S, Odisho AY, Litwin MS, Saigal CS, Cooperberg MR; NIDDK Urologic Diseases in America Project . Nationally representative trends and geographic variation in treatment of localized prostate cancer: the Urologic Diseases in America Project. Prostate Cancer Prostatic Dis. 2015;18(2):149–154. 10.1038/pcan.2015.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel N, Sam A, Valentin A, Quan SF, Parthasarathy S. Refill rates of accessories for positive airway pressure therapy as a surrogate measure of long-term adherence. J Clin Sleep Med. 2012;8(2):169–175. 10.5664/jcsm.1772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodney PP, Travis LL, Malenka D, et al. Regional variation in carotid artery stenting and endarterectomy in the Medicare population. Circ Cardiovasc Qual Outcomes. 2010;3(1):15–24. 10.1161/CIRCOUTCOMES.109.864736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turner A, Ricketts T, Leslie LK. Comparison of number and geographic distribution of pediatric subspecialists and patient proximity to specialized care in the US between 2003 and 2019. JAMA Pediatr. 2020;174(9):852-860. 10.1001/jamapediatrics.2020.1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368(16):1465–1468. 10.1056/NEJMp1302981 [DOI] [PubMed] [Google Scholar]
- 26.Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep. 2015;38(6):877–888. 10.5665/sleep.4732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–143. 10.1513/pats.200709-155MG [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Braley TJ, Dunietz GL, Chervin RD, Lisabeth LD, Skolarus LE, Burke JF. Recognition and diagnosis of obstructive sleep apnea in older Americans. J Am Geriatr Soc. 2018;66(7):1296–1302. 10.1111/jgs.15372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32(4):545–552. 10.1093/sleep/32.4.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653–1658. 10.5665/sleep.1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gagnadoux F, Le Vaillant M, Goupil F, et al. ; IRSR Sleep Cohort Group . Influence of marital status and employment status on long-term adherence with continuous positive airway pressure in sleep apnea patients. PLoS One. 2011;6(8):e22503. 10.1371/journal.pone.0022503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greenberg H, Fleischman J, Gouda HE, et al. Disparities in obstructive sleep apnea and its management between a minority-serving institution and a voluntary hospital. Sleep Breath. 2004;8(4):185–192. 10.1055/s-2004-860895 [DOI] [PubMed] [Google Scholar]
- 33.Jolley RJ, Liang Z, Peng M, et al. Identifying cases of sleep disorders through International Classification of Diseases (ICD) codes in administrative data. Int J Popul Data Sci. 2018;3(1):448. 10.23889/ijpds.v3i1.448 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.