Abstract
Study Objectives:
Sleep disturbance is common in those who experience trauma. In a sample of nontreatment-seeking refugees, we examined the associations between trauma exposure, postmigration stress, sleep symptoms, and posttraumatic psychological symptoms.
Methods:
Syrian and Iraqi refugees (n = 86; 51% female; mean age = 45 years) residing in Australia were recruited from the local community. Cross-sectional descriptive design, multinominal regression analyses, and mediation analyses were used. Participants completed measures in Arabic assessing premigration trauma exposure, postmigration stress, sleep symptoms, and mental health. They also completed 7 days of sleep diaries and actigraphy.
Results:
We identified 34.9% of the participants as normal sleepers, 32.6% as probably having insomnia, and 32.6% as likely having insomnia. Variables associated with greater sleep disturbance (McFadden’s R2 = 0.57) included greater trauma exposure, increased time of resettlement, greater postmigration stress, and greater presleep arousal. The association of premigration trauma exposure to current posttraumatic symptoms was mediated sequentially by postmigration stress and sleep symptoms.
Conclusions:
Our findings highlight the extent of sleep disturbance in refugees. We found evidence for an indirect pathway between trauma exposure and posttraumatic symptoms through premigration stress and sleep (particularly presleep arousal). In the current global refugee crisis, improving the existing system of care in countries experiencing increased migration is critical. Because sleep disturbance is a modifiable condition associated with mental health, targeting sleep could be an important component of psychological interventions for refugees.
Citation:
Lies J, Jobson L, Mascaro L, Whyman T, Drummond SPA. Postmigration stress and sleep disturbances mediate the relationship between trauma exposure and posttraumatic stress symptoms among Syrian and Iraqi refugees. J Clin Sleep Med. 2021;17(3):479–489.
Keywords: insomnia, refugees, posttraumatic stress, presleep arousal
BRIEF SUMMARY
Current Knowledge/Study Rationale: An impressive body of research has shown the central role of sleep disturbance in the development, maintenance, and treatment of posttraumatic stress disorder symptoms, and refugee mental health research indicates a high prevalence of posttraumatic stress disorder in this population. Despite significant advances in these 2 research areas, these 2 bodies of literature have not been well integrated.
Study Impact: The current study is the first to present the prevalence of sleep disturbance and the association between sleep and trauma symptoms among nontreatment-seeking refugees. These cross-sectional findings shed light on the extent of sleep problems within refugees, identify sleep as a mediator between trauma exposure and trauma symptoms, and hold the potential to inform more effective evaluations and interventions for refugee populations.
INTRODUCTION
A major refugee crisis is occurring worldwide with record-high numbers of people being forcibly displaced. At the end of 2018, the United Nations High Commissioner for Refugees recorded that 70.8 million people were displaced from their homes; an estimated 16.2 million of these individuals were newly displaced during that single year, and one-quarter were from Syria alone.1 Refugee populations are often exposed to prolonged and repeated traumatic events in their countries of origin and during displacement. Consequently, refugees present with high prevalence rates of trauma-related mental health problems, particularly posttraumatic stress disorder (PTSD), depression, and anxiety.2
A dose-response relationship has been established between premigration trauma exposure (ie, war-related trauma) and psychological impairment.3 However, psychological impairment for a refugee does not simply resolve with relocation to a new country. During the postmigration (resettlement) phase, refugees may experience ongoing adversities that hamper recovery or worsen mental health, and this postmigration stress impacts mental health outcomes over and above the effects of direct trauma exposure.4 Indeed, both trauma exposure and postmigration stress influence PTSD prevalence rates.5 Notably, current theoretical frameworks posit that postmigration stress mediates the effects of trauma exposure on PTSD symptoms.6,7 In support of these theoretical frameworks, a recent meta-analysis found that the positive association between prior trauma and subsequent PTSD symptoms was fully mediated by self-reported daily stressors.8 This finding highlights the need to integrate multiple pathways (ie, beyond a dose-response relationship and adding different mediating factors) to more fully understand the relationship between trauma exposure and PTSD symptoms in refugee populations. The current study builds upon this literature by examining whether there is an indirect effect of trauma exposure on PTSD symptoms through both postmigration stress and sleep symptoms. In this study, the 2 sleep symptoms of interest are insomnia severity (measured by the Insomnia Severity Index [ISI]) and presleep arousal (measured by the Pre-Sleep Arousal Scale [PSAS]).
Sleep was chosen as a potential concomitant variable because of the clear relationship between sleep and PTSD. Sleep disturbance, either before9 or after trauma exposure,10 predicts the development of PTSD and exponentially exacerbates the distress and dysfunction of individuals with PTSD.11 Further, it has been argued that clinically addressing sleep disturbance can lead to improvements in PTSD symptoms.12 Based on these and similar findings, researchers have proposed that sleep disturbance may play a role in mediating the effect of trauma exposure on PTSD.13 However, only 2 studies have examined such mediation models, both of which focused on combat as the trauma exposure.14,15 In cross-sectional analyses, these studies found an indirect pathway between combat exposure and PTSD symptoms through sleep disturbance and/or nightmare symptoms among veterans14 and active-duty military personnel.15 However, it remains unknown whether trauma exposure is indirectly associated with PTSD symptoms through sleep disturbance in refugee groups. The current study is the first to examine that question in an adult refugee sample.
Of the sleep symptoms associated with PTSD symptoms, there are reasons to focus on presleep arousal because it is strongly related to both sleep disturbance and the hyperarousal component of PTSD. Presleep arousal is defined as the heightened arousal occurring during the sleep onset period; it comprises cognitive arousal (ie, excessive worry, problem-solving, rumination) and somatic arousal (ie, physiological responses).16 Relationships among stressful life events, presleep arousal, and sleep disturbance have been well-documented. For instance, presleep arousal mediates the relationship between perceived stress and self-reported sleep quality, with cognitive presleep arousal being particularly important as a mediator.17 Although presleep arousal plays a role between perceived life stress and sleep quality, no research to date has studied whether life stressors (eg, ongoing adversities experienced by refugees) are indirectly associated with posttraumatic symptoms through presleep arousal.
In summary, sleep disturbance is common in those who have been exposed to trauma, it is nearly ubiquitous in refugees, and it is associated with symptoms of PTSD.18 However, there are at least 2 key gaps in the literature limiting our understanding of the associations between sleep and mental health in refugees. First, no study to date has used both objective (eg, actigraphy) and self-reported (eg, sleep diaries) measures in an attempt to more fully characterize sleep in refugees. Second, although evidence suggests an indirect association between combat exposure and PTSD symptoms through sleep symptoms (eg, presleep arousal), these associations have not been examined in refugees, who have experienced a variety of trauma exposure types. The current study aimed to address both of those gaps in the literature using a sample of 86 refugees from Syria and Iraq resettled in Australia. Aim 1 used objective and self-reported measures to describe sleep in this group of refugees and examined measures of psychological distress associated with greater sleep disturbance. In Aim 2, we tested a serial mediation model for the relationships between trauma exposure and PTSD symptoms, including examining whether there was an indirect association between trauma exposure and PTSD symptoms through both postmigration stress and sleep symptoms.
METHODS
Participants and procedure
Participants (n = 86: 75 Syrian participants and 11 Iraqi participants) were refugees resettled in Australia under the Australian Government Humanitarian Program. Inclusion criteria were (1) being a Syrian or Iraqi refugee, (2) ability to speak and read Arabic, and (3) aged ≥18 years. Exclusion criteria included any self-reported pre-existing sleep disorder other than insomnia. The recruitment took place between February and November 2018. Participants were recruited from refugee social and community groups, such as sporting groups, faith groups, and educational/English classes. Based on a report presented at the Public Seminar on Responses to Syrian-Conflict Refugee Settlement in Australia, Canada, Finland, Germany, New Zealand, Sweden, and the UK,19 we were able to measure the representativeness of our sample of participants to the larger population of Syrian and Iraqi refugees resettling in Australia. The report was collected for Syrian and Iraqi refugees who arrived between mid-2015 and the end of 2017. The majority of our sample arrived in Melbourne (Australia) during this same time period. Using χ2 analyses, we found similar patterns of sex (P = .90), age (P = .27), marital status (P = .80), and education distribution (P = .16) in our sample to that described in Collins and colleagues.19
None of the participants in our study reported taking sleep medication, but some participants reported being on medications for anxiety (n = 1), pain (n = 2), and cholesterol/ hypertension/cardiovascular health concerns (n = 17). The sample included 15 sets of married couples (n = 30). To determine if inclusion of both members of the couples influenced our findings, we created a dummy variable (couple vs individual) and included this variable as a covariate when statistically testing our aims. In each instance, this variable was not significant and including it did not alter the outcome of any analyses reported herein.
Ethical approval was obtained from the Monash University Human Research Ethics Committee. Participants attended 2 appointments 1 week apart. Participants were provided with an explanatory statement and informed consent written in Arabic. In the first session, after informed consent, participants were instructed on the use of the actigraph (a wearable watch-like device) and completion of the sleep diary. Participants wore the actigraph for the following week and completed the sleep diary each night for 7 nights. In the second session, the actigraph and sleep diary were collected. Participants then completed a battery of questionnaires.
Measures
A standard double-blind translation and backtranslation procedure, in accordance with gold-standard translation practices, was used to develop Arabic versions of the questionnaires, unless adapted Arabic versions of questionnaires already existed. The data on the sleep diaries were translated and backtranslated by a professional translator service.
Sleep measures
Actigraphy
Participants wore an actigraph for the week to measure the sleep-wake schedule. Respironics Actiwatch Spectrum Pro (Philips, Murrysville, PA) and Actiware 6 software (Philips) algorithms generated values for objective time in bed, wake after sleep onset, total sleep time, and sleep efficiency (SE). Default sleep detection settings were used (ie, medium sensitivity). The window for analysis was manually set, corresponding to time in bed according to sleep diary entries and event markers indicated by the participants, although rest intervals could be extended < 60 minutes on either side to account for obvious errors in diary entries.12,20,21
Sleep diary
Based on the consensus sleep diary,22 our diary included self-reported measures of lights-out time, sleep latency, number and duration of awakenings, wake time, time in bed after final awakening, and daytime naps and calculated variables of total sleep time and SE. We calculated SE as the ratio of total time asleep to time in bed; ≥ 85% is generally considered normal SE.23 Participants also completed an open-ended question that qualitatively examined participants’ appraisal of sleep difficulty for the prior night: “What do you think is reason behind your sleep difficulty on the previous night?”
ISI
The ISI is a 7-item self-reported questionnaire assessing overall insomnia severity in the past week.24 The total possible score ranges from 0–28; a higher score indicates greater insomnia symptoms. A cutoff point of ISI ≥ 10 is commonly used to study community samples.25 The measure evidenced good internal consistency (α = .86) in the current study.
PSAS
The PSAS consists of 16 items and comprises 2 subscales assessing cognitive arousal and somatic arousal.26 Scores range from 16–80, with higher scores indicating greater arousal. Suggested cutoff scores for cognitive arousal are ≥ 20, and those for somatic arousal are ≥ 14.27 This scale showed good internal consistency for the cognitive arousal subscale (α = .92) and the somatic arousal subscale (α = .89).
Measures of trauma exposure and posttraumatic mental health
Harvard Trauma Questionnaire
The Harvard Trauma Questionnaire assesses trauma exposure and was developed specifically for trauma-affected refugees. It has been validated and widely used in refugee studies.28 This study used the trauma events section of the Iraqi version of the Harvard Trauma Questionnaire.29 Individuals responded “yes” or “no” to 40 items, indicating whether they had experienced the events directly. Total trauma exposure scores were calculated by a count of “yes” responses. The measure evidenced good internal consistency (α = .86) in the current study.
Short Posttraumatic Stress Disorder Inventory
The Posttraumatic Stress Disorder Inventory-8 is an 8-item screening questionnaire for PTSD.30 It was developed based on the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, and it covers 3 symptom clusters of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition PTSD diagnosis, including 4 intrusion items, 2 avoidance items, and 2 hypervigilance items, and excludes the diagnostically nonspecific items (eg, sleeping difficulty, difficulty concentrating). The Posttraumatic Stress Disorder Inventory-8 was chosen as the measure of PTSD symptoms because it has been used in several large-scale refugee studies.31,32 Items are scored on a 4-point Likert scale and are summed to provide a symptom severity score. A cutoff point of 18 has been found to be indicative of probable PTSD.30 In the current study, the scale showed sound internal consistency (α = .88).
Hopkins Symptoms Checklist
The Hopkins Symptoms Checklist has 25 items measuring the affective symptoms of anxiety and depression over the previous month.33 The checklist has been widely used in refugee populations to assess for affective symptoms. Items are scored on a 4-point Likert scale, and a cutoff of ≥ 1.75 for “clinically significant distress” is recommended.34 The scale showed strong internal consistency (α = .95).
Measure of postmigration stress
Post Migration Living Difficulties
Post Migration Living Difficulties is a 23-item checklist assessing the levels of stress resulting from postmigration stressors.35 It consists of 3 domains: protection concerns, access to health and welfare, and stress related to resettlement conditions. Participants rated the extent to which they considered each postmigration challenge to be a problem; only items rated “moderately serious problem” and “very serious problem” were considered positive. Overall Post Migration Living Difficulties scores were calculated by a count of living difficulties considered a problem. In the current study, the scale showed sound internal consistency (α = .89).
Data analysis plan
Data analyses were performed using the SPSS version 21 (IBM Corporation, Armonk, NY) statistical package. There were no missing data, but 1 participant was excluded because of current self-reported sleep apnea. To examine Aim 1, descriptive statistics of the study measures and the percentage of participants meeting clinical cutoffs were tabulated. We categorized each individual according to the level of sleep disturbance using ISI ≥ 1025 and/or SE ≤ 85.23 Individuals not exceeding the cutoffs on either measure were considered as normal sleepers; the “probable insomnia” category was defined as an ISI ≥ 10 or SE ≤ 85, and the “likely insomnia” category as ISI ≥ 10 and SE ≤ 85. We considered using only the ISI to categorize the severity of insomnia symptoms in our sample. However, given that this was a community sample not selected for any specific sleep features and because we did not conduct diagnostic interviews, we wanted to capture sleep quality more broadly. Diary-based sleep efficiency is one way to do that because sleep efficiency can be affected by a number of factors. In the end, we decided to take an arguably more conservative approach than using either measure alone, combining both measures to provide an overall assessment of sleep disturbance.
We used multinominal regression analysis to examine the extent to which demographics, migration-related stress, mental health, and presleep arousal were associated with levels of sleep disturbance.
Serial multiple mediation analysis was used for Aim 2. We examined whether the relationship between premigration trauma exposure (independent variable) and PTSD symptoms (dependent variable) was mediated through postmigration stress (first mediator) and sleep symptoms (second mediator). This model was tested separately for 2 sleep measures: overall insomnia severity (ISI) and presleep arousal (PSAS). Because we conducted separate models with 2 different sleep measures, we applied a threshold of P < .025 for the significance of each full model. If PSAS was a significant mediator, then we planned to analyze additional models to assess each subscale of PSAS (ie, cognitive arousal and somatic arousal) independently as the sleep mediator. Serial multiple mediation analysis allowed for 2 subsequent mediators to be examined simultaneously and provided an estimate of the specific indirect effect for each mediator and the total indirect effect. We chose to place postmigration stress as the first mediator and sleep symptoms as the second mediator given findings that trauma exposure affects postmigration living difficulties,36,37 daily stress influences presleep arousal and sleep quality,17,26 and sleep disturbance and nightmares seem to play a role in mediating the effect of trauma exposure on PTSD symptoms.14,15,38 To test these mediation analyses we used the PROCESS macro in SPSS; 5,000 bootstrapped resamples and a 95% confidence interval were applied to construct the indirect path. Bias-corrected confidence intervals that did not contain zero were considered significant. Effect sizes were reported using standardized indirect effect size and interpreted as small (0.01), medium (0.09), and large (0.25).39
We also conducted the analyses controlling for demographic variables that were significantly correlated with our main study variables (ie, those included in the mediation models; Table S1 (30.4KB, pdf) in the supplemental material). These demographic variables included age, sex, marital status, employment, and length of resettlement, and we also evaluated the number of people in the household and the number of people sleeping in the bedroom. In each instance, a similar pattern of results emerged to that reported below (see Results section for Aim 2), for both the full models and the individual pathways. Because researchers must be careful when making inferences from cross-sectional data and because alternative models should be considered,40 we also conducted the mediation analyses by reversing the 2 mediators and using PTSD symptoms as a mediator with sleep symptoms (ISI and PSAS, individually) as the outcome measure. Finally, as an exploratory analysis, we coded qualitative data from the sleep diary on the perceived causes of sleep disturbance using thematic analysis41 (for details, see the supplemental material).
To determine the sample size needed for the study, we examined the separate literature related to mediators of the relationship between trauma exposure and PTSD symptoms. In the refugee literature, postmigration living difficulties mediated the relationship between premigration trauma exposure and PTSD symptoms in Tamil asylum-seekers residing in Australia, with a medium effect observed (β = .11).42 In the sleep literature, sleep disturbance mediated the relationship between combat trauma and PTSD symptoms, with a large effect observed (β = .22).15 Based on these findings, the current study adopted a conservative medium effect size. An a priori power analysis was conducted using G*Power 3 (Franz Faul, Universität Kiel, Kiel, Germany) and showed that assuming a medium effect size (f2 = .15)43 with sufficient power (β = .80) at α = .05 and 3 predictors, a total sample size of 77 participants would be needed to conduct a serial mediation analysis.
RESULTS
Table 1 summarizes the social and demographic characteristics of the participants. More than half of the sample scored above the clinical cutoff range for PTSD (59%) and affective symptoms (57%). Our sample reported having been exposed to 17 different trauma types listed in the Harvard Trauma Questionnaire, with > 90% of participants reporting having experienced home confinement because of outside chaos and violence, forced displacement to a different part of the country with minimal services, and involuntary flight from country of origin (Table S2 (30.4KB, pdf) ). Regarding postmigration stress, > 50% of our sample reported stress related to unemployment, financial strain, and an inability to return home during an emergency (Table S3 (30.4KB, pdf) ).
Table 1.
Participant characteristics and study variables.
| Characteristic (n = 86) | Value | Range | Above Clinical Cutoff, n (%) |
|---|---|---|---|
| Age, mean (SD), y | 45.41 (16.39) | 18–80 | |
| Duration of displacement, mean (SD), mo | 18.91 (12.86) | 1–24 | |
| Duration of resettlement, mean (SD), mo | 20.09 (10.58) | 2–57 | |
| Sex, n (%) | |||
| Female | 44 (51.2) | ||
| Male | 42 (48.8) | ||
| Marital status, n (%) | |||
| Single | 20 (23.26) | ||
| Married | 55 (63.95) | ||
| Widowed | 11 (12.79) | ||
| Employment, n (%) | |||
| Unemployed | 69 (80.2) | ||
| Student | 12 (14.0) | ||
| Employed | 5 (5.8) | ||
| Education, n (%) | |||
| No formal education | 7 (8.1) | ||
| Primary education | 14 (16.3) | ||
| Secondary education | 44 (51.2) | ||
| Tertiary education | 21 (24.4) | ||
| Number of people sharing a room | 1.67 (0.58) | 1–3 | |
| Number of people in the house | 4.77 (1.70) | 2–8 | |
| Sleep diary SE, mean (SD), min | 85.90 (7.78) | 49.1–97.3 | 25 (39.5) |
| Sleep diary TST, mean, min | 450.83 | 232.9–628.6 | 29 (33.7) |
| ISI, mean (SD) | 11.48 (6.01) | 1–26 | 50 (58) |
| PSAS, mean (SD) | 30.79 (12.08) | 16–68 | |
| Cognitive | 17.63 (7.84) | 8–38 | 31 (36) |
| Somatic | 13.16 (5.27) | 8–30 | 34 (39.5) |
| HTQ, mean (SD) | 16.85 (5.59) | 5–29 | |
| PMLD, mean (SD) | 8.91 (2.27) | 5–18 | |
| PTSD-8 total, mean (SD) | 21.65 (9.00) | 8–48 | 51 (59) |
| HSCL-25, mean (SD) | 1.92 (0.66) | 1.0–3.8 | 49 (57) |
HSCL-25 = Hopkins Symptoms Checklist, HTQ = Harvard Trauma Questionnaire, ISI = Insomnia Severity Index, PMLD = Post Migration Living Difficulties, PSAS = Pre-Sleep Arousal Scale, PTSD-8 = Short Posttraumatic Stress Disorder Inventory, SD = standard deviation, SE = sleep efficiency, TST = total sleep time.
Characterizing sleep and insomnia symptoms (Aim 1)
The mean ISI score (M = 11.50; standard deviation = 6.00) was above the ISI clinical cutoff point (≥ 10 in community samples),25 with more than half of the sample (n = 50; 58%) scoring above this cutoff point. From the sleep diary (Table 2), the mean self-reported SE was 85.90 (standard deviation = 7.80), with 24 (39.5%) individuals reporting an SE < 85%. The mean self-reported total sleep time was 7.5 (standard deviation = 1.2) hours, with 29 (33.7%) participants reporting sleep less than the recommended 7 hours/night.44 When classifying participants in terms of level of sleep disturbance, we found that 30 (34.9%) participants were normal sleepers, 28 (32.6%) participants were in the probable insomnia category, and 28 (32.6%) participants were in the likely insomnia category. As is common in samples not selected for specific clinical disorders, the average sleep diary data slightly overestimated sleep quality and quantity compared to objective sleep data from actigraphy for the normal and probable insomnia groups. The likely insomnia group showed a pattern more consistent with chronic insomnia, whereas the sleep diaries underestimated sleep quality and quantity, relative to actigraphy.
Table 2.
Descriptive statistics for objective and self-reported sleep data.
| All Participants (n = 86) | Subgroups | Posthoc t tests for Comparison Between Sleep Categoriesc,d | |||||
|---|---|---|---|---|---|---|---|
| Normal Sleepers (n = 30) | Probable Insomnia (n = 28) | Likely Insomnia (n = 28) | 0 vs 1 | 0 vs 2 | 1 vs 2 | ||
| Sleep diary statisticsa,b | |||||||
| SE | 85.90 (7.78) | 91.19 (2.92) | 88.26 (3.75) | 77.87 (7.97) | .015** | <.001** | <.001** |
| TST | 450.83 (72.90) | 475.60 (67.76) | 468.39 (62.13) | 406.72 (70.15) | NS | <.001** | <.001** |
| SOL | 26.94 (14.84) | 20.73 (10.35) | 24.48 (9.25) | 36.06 (18.90) | NS | <.001** | .005** |
| WASO | 22.34 (23.91) | 9.42 (10.37) | 16.85 (13.76) | 41.68 (29.84) | .023* | <.001** | <.001** |
| EMWT | 23.53 (17.82) | 15.66 (8.85) | 21.65 (16.60) | 33.84 (21.39) | NS | <.001** | .021* |
| Actigraphy statistics | |||||||
| SE | 81.88 (6.44) | 82.25 (4.75) | 82.88 (5.77) | 80.46 (8.47) | NS | NS | NS |
| TST | 433.96 (57.83) | 431.39 (53.79) | 444.99 (60.61) | 425.90 (60.04) | NS | NS | NS |
| SOL | 20.84 (16.19) | 24.61 (19.01) | 20.86 (16.74) | 16.49 (10.62) | NS | NS | NS |
| WASO | 54.08 (23.01) | 51.53 (17.23) | 53.54 (25.24) | 57.57 (26.70) | NS | NS | NS |
| EMWT | 22.17 (16.71) | 18.82 (9.22) | 18.51 (9.83) | 29.69 (24.96) | NS | .031* | .039* |
Values are presented as mean (standard deviation). aSE calculated as a percentage; time asleep divided by time in bed. TST, SOL, WASO, and EMWT represented in minutes. bEMWT defined as time in bed since last awakening. cAn ANOVA was run to first determine which sleep variables had a significant difference between any groups. Independent t tests were then used posthoc to determine which groups significantly differed from each other. d0 = normal sleepers, 1 = probable insomnia, 2 = likely insomnia. *P < .05; **Bonferroni correction, *P < .017. ANOVA = analysis of variance, EMWT = early morning wake time, SE = sleep efficiency, SOL = sleep onset latency, TST = total sleep time, WASO = wake after sleep onset.
When all variables were considered in a multinomial regression, a longer period of resettlement, greater premigration trauma exposure, greater postmigration stress, and higher presleep arousal were all associated with greater levels of insomnia symptoms (P < .001; omnibus model McFadden’s R2 = 0.57; Table 3). Follow-up analyses showed, relative to the normal sleep group, that greater postmigration stress and presleep arousal were significantly associated with probable insomnia symptoms. Longer periods of resettlement, greater trauma exposure, and higher presleep arousal were associated with likely insomnia symptoms.
Table 3.
Multinomial logistic regression analysis for levels of insomnia symptoms.
| Variable | LRT | Probable Insomnia vs Normal Sleepers | Likely Insomnia vs Normal Sleepers | |||
|---|---|---|---|---|---|---|
| P | OR (95% CI) | P | OR (95% CI) | P | ||
| Age | .06 | 1.04 (0.99–1.09) | .16 | 0.96 (0.87–1.05) | .33 | |
| Sex: female | .10 | 1.37 (0.22–8.62) | .73 | 37.89 (0.76–1877) | .07 | |
| Duration of displacement | .15 | 1.05 (0.98–1.13) | .17 | 1.09 (0.98–1.21) | .11 | |
| Duration of resettlement | <.001** | 0.94 (0.83–1.06) | .29 | 1.28 (1.01–1.61) | .04* | |
| PSAS total | <.001** | 1.17 (1.00–1.37) | .046* | 1.59 (1.18–2.15) | .002** | |
| HTQ | .002* | 0.94 (0.74–1.19) | .59 | 1.70 (1.06–2.73) | .03* | |
| PMLD | <.001** | 3.33 (1.14–9.66) | .03* | 0.15 (0.02–1.07) | .06 | |
| PTSD-8 | .14 | 1.00 (0.85–1.18) | .97 | 1.24 (0.95–1.62) | .11 | |
| HSCL-25 | .15 | 0.90 (0.80–1.02) | .09 | 0.99 (0.85–1.15) | .89 | |
*P < .05, two-tailed; **P < .001, two-tailed. CI = confidence interval, HSCL-25 = Hopkins Symptoms Checklist, HTQ = Harvard Trauma Questionnaire, LRT = likelihood ratio tests, OR = odds ratio, PMLD = Post Migration Living Difficulties, PSAS = Pre-Sleep Arousal Scale, PTSD-8 = Short Posttraumatic Stress Disorder Inventory.
Serial mediation analyses (Aim 2)
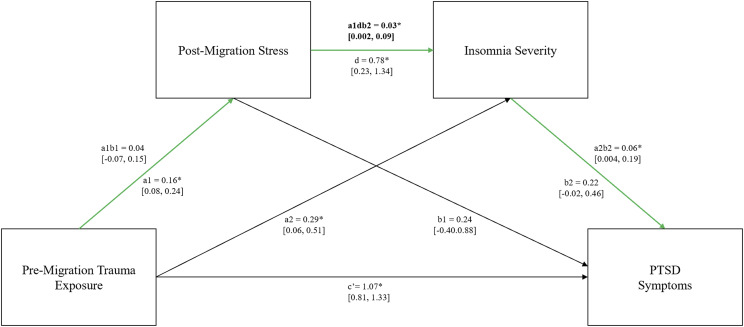
ISI
As expected, trauma exposure had a significant direct effect on PTSD symptoms (path c’: B = 1.07; 95% confidence interval [CI], 0.81–1.33; P < .001; see Figure 1). The indirect effect through just postmigration stress was nonsignificant (path a1b1: B = 0.04; 95% CI, –0.07 to 0.15). The indirect effect through just insomnia severity was significant (path a2b2: B = 0.06; 95% CI, 0.004–0.19), with 22.3% of the effect coming indirectly from insomnia severity. When both postmigration stress and insomnia severity were included in serial, the model showed a significant indirect relationship between trauma exposure and PTSD symptoms (path a1db2: B = 0.03; 95% CI, 0.002–0.09; P < .001), with 59% of the effect coming indirectly through the 2 serial mediators. When the alternative model was tested by reversing the 2 mediators, the indirect relationship between trauma exposure and PTSD symptoms was nonsignificant (path a1db2: B = 0.01; 95% CI, –0.01 to 0.06). When an alternative model placing PTSD symptoms as a mediator and ISI as the outcome measure was run, the indirect relationship between trauma exposure and ISI was not significant.
Figure 1. PMLD and ISI mediators in serial mediation analysis.
Path a1b1 represents the effect of premigration trauma exposure on PTSD symptoms mediated via postmigration stress; path a2b2 represents the effect of premigration trauma exposure on PTSD symptoms mediated via insomnia severity; path a1db2 represents the effect of premigration trauma exposure on PTSD symptoms mediated via postmigration stress and insomnia severity; c’ represents the direct effect of trauma exposure on PTSD symptoms. ISI = Insomnia Severity Index, PMLD = Post Migration Living Difficulties, PTSD = posttraumatic stress disorder. *P value <.05, two-tailed.
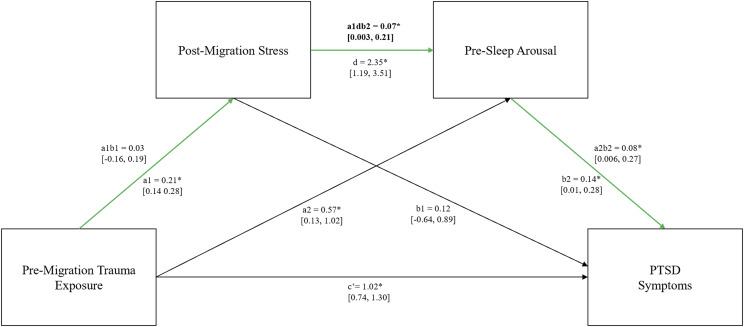
Presleep arousal (PSAS)
As depicted in Figure 2, trauma exposure had a significant direct effect on PTSD (path c’: B = 1.02; 95% CI, 0.74–1.30; P < .001). Similar to the previous model, the indirect effect through postmigration stress was nonsignificant (path a1b1: B = 0.03; 95% CI, –0.16 to 0.19), whereas the indirect effect through presleep arousal was significant (path a2b2: B = 0.08; 95% CI, 0.006–0.27), with 36.9% of the effect indirectly coming from presleep arousal. When both postmigration stress and presleep arousal were included as serial mediators, there was a significant indirect effect of trauma exposure on PTSD symptoms (path a1db2: B = 0.07; 95% CI, 0.003–0.21; P < .001), again with 59% of the effect coming indirectly through the 2 serial mediators. The alternative model, ie, reversing the order of the mediators (path a1db2: B = 0.01; 95% CI, –0.02 to 0.08) was not significant. As with the ISI, when an alternative model placing PTSD symptoms as a mediator and PSAS as the outcome measure was run, the indirect relationship between trauma and PSAS was not significant.
Figure 2. PMLD and PSAS mediators in serial mediation analysis.
Path a1b1 represents the effect of premigration trauma exposure on PTSD symptoms mediated via postmigration stress; path a2b2 represents the effect of premigration trauma exposure on PTSD symptoms mediated via presleep arousal; path a1db2 represents the effect of premigration trauma exposure on PTSD symptoms mediated via postmigration stress and presleep arousal; and c’ represents the direct effect of trauma exposure on PTSD symptoms. PMLD = Post Migration Living Difficulties, PSAS = Pre-Sleep Arousal Scale, PTSD = posttraumatic stress disorder. *P value <.05, two-tailed.
Posthoc analyses examining the role of cognitive and somatic presleep arousal separately showed that the model remained significant when cognitive presleep arousal was the second mediator. The indirect pathway between trauma exposure and PTSD symptoms through postmigration stress and cognitive presleep arousal was significant (path a1db2: B = 0.05; 95% CI, 0.007–0.14; R2 = 0.62; P < .001). This particular model accounted for the highest total variance in PTSD symptoms tested in this study (62%). Using somatic presleep arousal as the second mediator resulted in a nonsignificant indirect relationship between trauma exposure and PTSD symptoms via the serial mediators (path a1db2: B = 0.004; 95% CI, –0.01 to 0.06).
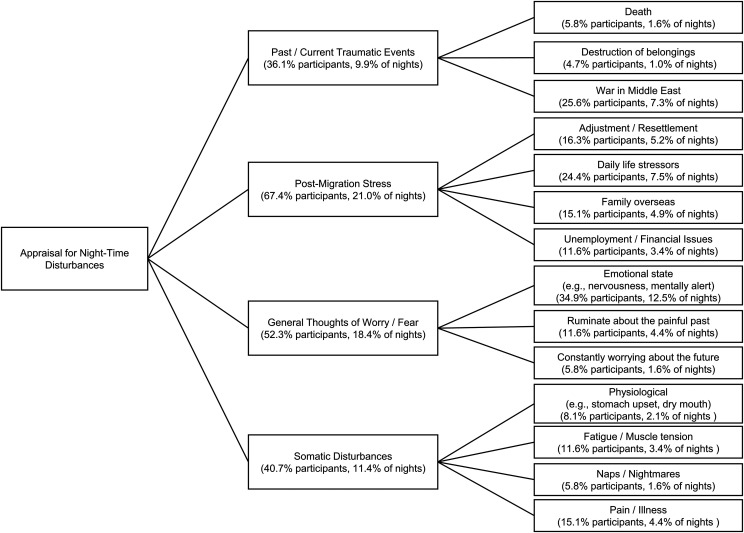
Thematic analysis of the qualitative data
On 385 out of 602 (64%) nights in the sleep diary, participants listed factor(s) contributing to their disturbed sleep. Thematic analysis of this qualitative data resulted in 4 key themes: past/current traumatic events, postmigration stress, general thoughts of worry or fear, and somatic disturbances (Figure 3). The qualitative data suggested that the majority of the appraisals were associated with cognitive arousal rather than somatic arousal. The cognitive arousal themes related to (1) current/past traumatic events, ie, the death of family members, destruction of property, and thinking/ruminating/worrying about the war and their home villages; (2) postmigration stress—specifically, adapting to new roles and responsibility, general life stressors living in Australia, missing/worrying about family overseas, and financial issues; and (3) general thoughts of worry or fear, ie, feeling worried and apprehensive without a specific context, being reminded of the painful past, and worrying and fearful about the future. The somatic disturbances were mainly physiological discomfort, fatigue and tiredness, pain in the body, and feeling awake because of naps, nightmares, and dreams.
Figure 3. Qualitative themes.
Themes and subthemes of commonly reported appraisal for nighttime disturbances. Number of participants who mentioned the theme/subtheme: at least once out of n = 86, and number of nights: out of 385 entries.
DISCUSSION
This study is the first to use a combination of actigraphy, sleep diary, and sleep questionnaires in examining sleep among nontreatment-seeking refugees. We combined empirical models from 2 separate literatures to propose and test whether trauma exposure was indirectly associated with PTSD symptoms through postmigration stress and sleep symptoms. We found that 65% of the community sample of refugees had probable or likely insomnia, with symptoms typically deemed sufficient for a clinical referral. This result is slightly higher than that reported by Al-Smadi and colleagues45 in a similar population. Using the ISI, they found that 52% of Syrian and Iraqi refugees residing in Jordan had moderate to severe insomnia symptoms. However, if we were to use the ISI alone, 58% of our participants would be in the same range.
We also found that higher presleep arousal was the only factor associated with both probable and likely insomnia in our sample. Interestingly, mental health variables were not associated with levels of sleep disturbance. Exploratory posthoc analyses examined why, especially because past research documented the close relationship between mental health and sleep.46 Because both PTSD symptoms and trauma exposure, and affective symptoms and presleep arousal, were correlated, it is possible that collinearity between these sets of variables impacted the regression models. In support of this hypothesis, when trauma exposure and presleep arousal were removed from the regression model, duration of displacement and postmigration stress remained significant correlates and PTSD and affective symptoms were now also significantly associated with levels of insomnia symptoms (Table S4 (30.4KB, pdf) ).
Prior studies have shown an indirect effect of trauma on posttraumatic symptoms through both postmigration living difficulties and sleep disturbance separately, but to date no study has examined these variables simultaneously. We believe it is important to do so in refugees because refugees experience both postmigration living difficulties and sleep disturbance at high levels, which is somewhat unique for trauma-exposed populations. However, this model may be relevant in recently discharged veterans as well. Veterans, especially combat veterans, can experience stressors reintegrating into civilian life similar to the postmigration stressors assessed here, and veterans also experience a high rate of sleep disturbance.47 Thus, one might expect a similar indirect pathway between trauma exposure and mental health symptoms as found in this study.
As hypothesized, our findings showed an indirect association between trauma exposure and PTSD symptoms through postmigration stress and sleep symptoms, in that sequential order. When these 2 variables were reversed, the indirect pathways were no longer significant. Similarly, when sleep symptoms and PTSD symptoms were flipped (ie, sleep symptoms as the outcome measure), a nonsignificant indirect relationship was observed. Interestingly, when we tested the sequential mediation models using the presleep arousal subscales, the mediation model including cognitive presleep arousal accounted for the greatest amount of variance in PTSD symptoms of any model tested in our analyses. Combined with presleep arousal being the only variable associated with both probable and likely insomnia symptoms, our data suggest that (cognitive) presleep arousal is a noteworthy construct requiring further research and clinical attention in this population.
Finally, we performed a thematic analysis from daily reports about factors disturbing each individual’s sleep. Four themes emerged, 3 of which are arguably related to cognitive presleep arousal. These themes are consistent with findings from other research indicating that after resettling into a new country, refugees often report concerns pertaining to the adversities to which they were exposed, ongoing conflict in their country, and/or stressors related to their postmigration situation.4,5 These self-reports of factors contributing to disturbed sleep seem to support modeling data suggesting that presleep arousal is an important correlate of PTSD symptoms. Indeed, some of the subthemes in the past/current traumatic events, postmigration stress, and general thoughts of worry or fear themes (Figure 3) mirrored specific questions on the cognitive PSAS subscale (having depressing or anxious thoughts, worry about problems other than sleep, being mentally alert, and inability to shut the mind off). Similarly, participants’ descriptions in the somatic disturbances theme were analogous to questions on the somatic PSAS subscale (nervous feeling in the body, tenseness in the muscles, stomach upset, and dry feeling in the mouth/throat). It is worth highlighting that the individuals conducting the thematic analysis had not seen the PSAS items, and thus it is not the case that they intentionally or unintentionally created themes to mirror those PSAS items. As with the quantitative findings, these qualitative data suggest that presleep arousal is a specific type of sleep disturbance impacting this population’s sleep and, potentially, posttraumatic symptoms. The present findings also support the use of the PSAS in refugees when assessing their mental health.
Although our study provides evidence for both postmigration stress and sleep being associated with PTSD symptoms in nontreatment-seeking refugees, the cross-sectional nature of the study prevents us from determining the extent to which these variables serve as variable markers or risk factors for PTSD in this population.48 Nonetheless, it is worth considering the potential clinical implications of these findings for addressing trauma symptoms in community-dwelling refugees, perhaps particularly in those not currently seeking treatment for mental health concerns. Literature examining the perceptions of mental health and barriers to accessing services among Syrian and Iraqi refugees has highlighted that mental health stigma is a key barrier to seeking mental health services.49,50 Work with U.S. veterans has shown that individuals with either PTSD or depression prefer to receive treatment for sleep problems rather than for the psychiatric condition.51 It is possible that the stigma associated with mental health concerns in Syrian and Iraqi refugees would result in a similar preference, although this hypothesis needs to be examined directly. If it is true, then sleep may serve as a more acceptable target for assessment and, if appropriate, intervention in this population. There are evidence-based psychological treatments for improving sleep disturbance in individuals with PTSD, including cognitive-behavioral therapy for insomnia12 and nightmare interventions.52 Both cognitive-behavioral therapy for insomnia and nightmare interventions typically have a strong behavioral focus. However, given that both the statistical models and the qualitative data showed that presleep arousal, especially cognitive presleep arousal, was associated with PTSD symptoms in these refugees, employing interventions with a strong cognitive focus could be particularly helpful in this population. It would also be beneficial for studies to explicitly examine cultural contexts and perspectives on sleep and sleep disturbance to inform whether sleep assessments and/or interventions for sleep should be culturally adapted.
In evaluating our findings, it is important to consider the strengths and limitations of our study. Recruiting a representative sample of refugees living in the community to participate in health and mental health survey research is known to be a challenging task because they are considered a “hard-to-reach” or “hidden” group, because of issues around trust and safety.53 This challenge precluded the possibility of implementing a fully representative sampling strategy, requiring us to recruit a sample of individuals attending social, sport, and religious activities. It is difficult to ascertain whether these participants exhibited more or less severe mental health difficulties than those Syrian and Iraqi refugees who were not attending those activities. However, in comparing our participants’ demographic to the larger population of Syrian and Iraqi refugees who arrived in Australia at approximately the same period,19 our sample seems to be representative of the overall Syrian and Iraqi refugee population resettling in Australia.
The main limitation of this study is the cross-sectional nature of data collection. By definition, cross-sectional research cannot address causality and cannot truly identify the risk factors of the outcome variable (in this case, PTSD symptoms).48 Indeed, although we included PTSD symptoms as the outcome variable and sleep as a mediator, PTSD symptoms and sleep are known to have a bidirectional relationship. The direction of association in our models was chosen based on theoretical considerations and prior research, as briefly outlined in the Introduction. Nonetheless, we also examined models reversing the positions of PTSD symptoms and sleep, and in these models, the indirect pathway was no longer significant. Although considerable research has examined the association between sleep disturbance and PTSD,9–15 surprisingly few studies have specifically evaluated both directions of the bidirectional link between sleep disturbance and PTSD symptoms. A longitudinal study examined a large sample of earthquake survivors in China and found that sleep disturbance (measured by the Pittsburgh Sleep Quality Index) could predict and was predicted by PTSD plus depression symptoms at 12 months, 18 months, and 24 months, suggesting a bidirectional relationship between sleep disturbance and PTSD and depression.54 However, Wright and colleagues55 found that among combat veterans, sleep disturbance (measured by the ISI) at 4 months posttrauma was a significant predictor of change in PTSD symptoms at 12 months posttrauma but PTSD symptoms 4 months posttrauma did not predict sleep disturbance at 12 months. Similarly, Acheson and colleagues9 reported that whereas sleep disturbance in active-duty soldiers before deployment predicted subsequent re-experiencing symptoms, predeployment re-experiencing symptoms did not predict subsequent sleep disturbance. Together, these findings indicate that the stronger direction of the bidirectional relationship between sleep and PTSD symptoms, if either, remains unclear and suggest that the answer may depend on the type of trauma(s) experienced. Future longitudinal research in samples of refugee populations should directly compare mediation models testing the influence that sleep and mental health symptoms have on one another to better assess the strength of each direction of the relationship in this specific population.
Although measures employed in this study have been validated with refugee groups from multiple cultures,31 they were not specifically adapted for the Syrian and Iraqi community, increasing the risk of transcultural error. On a related note, our models mainly focused on variables at the individual level rather than on broader factors of family, community, and environmental factors important within our sample’s cultures. Future studies should assess the potential moderating roles that such cultural factors may play in the relationships among trauma exposure, postmigration stress, sleep, and PTSD symptoms (eg, appraisals, emotion regulation).56,57 Another potential limitation is that the mental health outcome measures used were based upon symptom scales alone and were not diagnostic assessments. We chose to do this because we recruited a community sample as opposed to a treatment-seeking sample. Nonetheless, the results could be different if outcomes represented formal diagnoses rather than symptom severity. In addition, we did not have a control group (eg, native-born Australians of similar socioeconomic status or refugees who had lived in Australia longer).
Thus, it is unclear to what extent these findings are unique to refugees resettled within the last few years. Future research should consider longitudinal analyses to examine changes in these relationships over time, especially as refugees become more settled in their new country.
DISCLOSURE STATEMENT
All authors have seen and accepted the manuscript in its current form. Sean P.A. Drummond serves on a Data Safety Monitoring Board for Zelda Pharmaceuticals, unrelated to the submitted work. The remaining authors report no conflicts of interest.
SUPPLEMENTARY MATERIAL
ACKNOWLEDGMENTS
The authors acknowledge many community leaders, organizations, and programs who provided their support to this research study. Special thanks to Hani Pito from the Upfield Football Club for organizing and allowing us to use the space for data recruitment. We also thank Abdel Ahad Youkanna from the Syrian Social Club and Dr. Salam Danhka from the Assyrian Chaldean Women’s Group for introducing our study to the communities.
ABBREVIATIONS
- CI
confidence interval
- ISI
Insomnia Severity Index
- PTSD
posttraumatic stress disorder
- PSAS
Pre-Sleep Arousal Scale
- SE
sleep efficiency
REFERENCES
- 1.United Nations High Commissioner for Refugees (UNHCR) . Figures at a Glance. https://www.unhcr.org/ph/figures-at-a-glance. Accessed July 9, 2019.
- 2.Turrini G, Purgato M, Ballette F, Nosè M, Ostuzzi G, Barbui C. Common mental disorders in asylum seekers and refugees: umbrella review of prevalence and intervention studies. Int J Ment Health Syst. 2017;11:51. 10.1186/s13033-017-0156-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson H, Thompson A. The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: a review. Clin Psychol Rev. 2008;28(1):36–47. 10.1016/j.cpr.2007.01.017 [DOI] [PubMed] [Google Scholar]
- 4.Li SSY, Liddell BJ, Nickerson A. The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Curr Psychiatry Rep. 2016;18(9):82. 10.1007/s11920-016-0723-0 [DOI] [PubMed] [Google Scholar]
- 5.Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA. 2005;294(5):602–612. 10.1001/jama.294.5.602 [DOI] [PubMed] [Google Scholar]
- 6.Miller KE, Rasmussen A. The mental health of civilians displaced by armed conflict: an ecological model of refugee distress. Epidemiol Psychiatr Sci. 2017;26(2):129–138. 10.1017/S2045796016000172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller KE, Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. Soc Sci Med. 2010;70(1):7–16. 10.1016/j.socscimed.2009.09.029 [DOI] [PubMed] [Google Scholar]
- 8.Hou WK, Liu H, Liang L, et al. Everyday life experiences and mental health among conflict-affected forced migrants: a meta-analysis. J Affect Disord. 2020;264:50–68. 10.1016/j.jad.2019.11.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acheson DT, Kwan B, Maihofer AX, et al. Sleep disturbance at pre-deployment is a significant predictor of post-deployment re-experiencing symptoms. Eur J Psychotraumatol. 2019;10(1):1679964. 10.1080/20008198.2019.1679964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33(1):69–74. 10.1093/sleep/33.1.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giosan C, Malta LS, Wyka K, et al. Sleep disturbance, disability, and posttraumatic stress disorder in utility workers. J Clin Psychol. 2015;71(1):72–84. 10.1002/jclp.22116 [DOI] [PubMed] [Google Scholar]
- 12.Walters EM, Jenkins MM, Nappi CM, et al. The impact of prolonged exposure on sleep and enhancing treatment outcomes with evidence-based sleep interventions: a pilot study. Psychol Trauma. 2020;12(2):175–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pace-Schott EF, Germain A, Milad MR. Sleep and REM sleep disturbance in the pathophysiology of PTSD: the role of extinction memory. Biol Mood Anxiety Disord. 2015;5(1):3. 10.1186/s13587-015-0018-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Picchioni D, Cabrera OA, McGurk D, et al. Sleep symptoms as a partial mediator between combat stressors and other mental health symptoms in Iraq War veterans. Mil Psychol. 2010;22(3):340–355. 10.1080/08995605.2010.491844 [DOI] [Google Scholar]
- 15.Steele M, Germain A, Campbell JS. Mediation and moderation of the relationship between combat experiences and post-traumatic stress symptoms in active duty military personnel. Mil Med. 2017;182(5):e1632–e1639. 10.7205/MILMED-D-16-00169 [DOI] [PubMed] [Google Scholar]
- 16.Riemann D, Spiegelhalder K, Feige B, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14(1):19–31. 10.1016/j.smrv.2009.04.002 [DOI] [PubMed] [Google Scholar]
- 17.Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. 2003;65(2):259–267. 10.1097/01.PSY.0000030391.09558.A3 [DOI] [PubMed] [Google Scholar]
- 18.Lies J, Mellor A, Jobson L, Drummond SPA. Prevalence of sleep disturbance and its relationships with mental health and psychosocial issues in refugees and asylum seekers attending psychological services in Australia. Sleep Health. 2019;5(4):335–343. 10.1016/j.sleh.2019.06.002 [DOI] [PubMed] [Google Scholar]
- 19.Collins J, Reid C, Groutsis D, Watson K, Ozkul D. Syrian and Iraqi refugee settlement in Australia. University of Technology Sydney working paper 1. 2018. https://www.uts.edu.au/sites/default/files/article/downloads/Collins.Reid_.Groutsis.Australia.Syrian-Conflict%20Refugee%20Settlement%20in%20Australia.pdf. Accessed November 10, 2020.
- 20.Straus LD, Anderson D, Salamat J, Nappi CM, Drummond SP. A comparison of three analytic scoring methods of actigraphically recorded sleep in PSTD. Paper presented at: SLEEP 2012; June 9–13, 2012; Boston, MA. [Google Scholar]
- 21.Walters EM, Phillips AJK, Mellor A, et al. Sleep and wake are shared and transmitted between individuals with insomnia and their bed-sharing partners. Sleep. 2020;43(1):zsz206. 10.1093/sleep/zsz206 [DOI] [PubMed] [Google Scholar]
- 22.Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302. 10.5665/sleep.1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reed DL, Sacco WP. Measuring sleep efficiency: what should the denominator be? J Clin Sleep Med. 2016;12(2):263–266. 10.5664/jcsm.5498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morin CM. Insomnia: Psychological Assessment and Management. New York: Guilford Press; 1993. [Google Scholar]
- 25.Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nicassio PM, Mendlowitz DR, Fussell JJ, Petras L. The phenomenology of the pre-sleep state: the development of the pre-sleep arousal scale. Behav Res Ther. 1985;23(3):263–271. 10.1016/0005-7967(85)90004-X [DOI] [PubMed] [Google Scholar]
- 27.Puzino K, Amatrudo G, Sullivan A, Vgontzas A, Fernandez-Mendoza J. Clinical significance and cut-off scores for the Pre-Sleep Arousal Scale in chronic insomnia disorder: a replication in a clinical sample. Behav Sleep Med. 2020;18(6):705–718. [DOI] [PubMed] [Google Scholar]
- 28.Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. 1992;180(2):111–116. 10.1097/00005053-199202000-00008 [DOI] [PubMed] [Google Scholar]
- 29.Shoeb M, Weinstein H, Mollica R. The Harvard Trauma Questionnaire: adapting a cross-cultural instrument for measuring torture, trauma and posttraumatic stress disorder in Iraqi refugees. Int J Soc Psychiatry. 2007;53(5):447–463. 10.1177/0020764007078362 [DOI] [PubMed] [Google Scholar]
- 30.Hansen M, Andersen TE, Armour C, Elklit A, Palic S, Mackrill T. PTSD-8: a short PTSD inventory. Clin Pract Epidemiol Ment Health. 2010;6(1):101–108. 10.2174/1745017901006010101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bryant RA, Edwards B, Creamer M, et al. The effect of post-traumatic stress disorder on refugees’ parenting and their children’s mental health: a cohort study. Lancet Public Health. 2018;3(5):e249–e258. 10.1016/S2468-2667(18)30051-3 [DOI] [PubMed] [Google Scholar]
- 32.Nickerson A, Hadzi-Pavlovic D, Edwards B, et al. Identifying distinctive psychological symptom profiles among a nationally representative sample of refugees resettled in Australia. Aust N Z J Psychiatry. 2019;53(9):908–919. 10.1177/0004867419846403 [DOI] [PubMed] [Google Scholar]
- 33.Mollica RF, Wyshak G, de Marneffe D, Khuon F, Lavelle J. Indochinese versions of the Hopkins Symptom Checklist-25: a screening instrument for the psychiatric care of refugees. Am J Psychiatry. 1987;144(4):497–500. 10.1176/ajp.144.4.497 [DOI] [PubMed] [Google Scholar]
- 34.Nettelbladt P, Hansson L, Stefansson CG, Borgquist L, Nordström G. Test characteristics of the Hopkins Symptom Check List-25 (HSCL-25) in Sweden, using the Present State Examination (PSE-9) as a caseness criterion. Soc Psychiatry Psychiatr Epidemiol. 1993;28(3):130–133. 10.1007/BF00801743 [DOI] [PubMed] [Google Scholar]
- 35.Silove D, Sinnerbrink I, Field A, Manicavasagar V, Steel Z. Anxiety, depression and PTSD in asylum-seekers: associations with pre-migration trauma and post-migration stressors. Br J Psychiatry. 1997;170(4):351–357. 10.1192/bjp.170.4.351 [DOI] [PubMed] [Google Scholar]
- 36.Nickerson A, Steel Z, Bryant R, Brooks R, Silove D. Change in visa status amongst Mandaean refugees: relationship to psychological symptoms and living difficulties. Psychiatry Res. 2011;187(1–2):267–274. 10.1016/j.psychres.2010.12.015 [DOI] [PubMed] [Google Scholar]
- 37.Porter M, Haslam N. Forced displacement in Yugoslavia: a meta-analysis of psychological consequences and their moderators. J Trauma Stress. 2001;14(4):817–834. 10.1023/A:1013054524810 [DOI] [PubMed] [Google Scholar]
- 38.Straus LD, Drummond SPA, Risbrough VB, Norman SB. Sleep Disruption, Safety Learning, and Fear Extinction in Humans: Implications for Posttraumatic Stress Disorder. In: Vermetten E, Baker DG, Risbrough VB, eds. Behavioral Neurobiology of PTSD. Cham, Switzerland: Springer International Publishing; 2018: 193–205. [DOI] [PubMed] [Google Scholar]
- 39.Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16(2):93–115. 10.1037/a0022658 [DOI] [PubMed] [Google Scholar]
- 40.MacCallum RC, Austin JT. Applications of structural equation modeling in psychological research. Annu Rev Psychol. 2000;51(1):201–226. 10.1146/annurev.psych.51.1.201 [DOI] [PubMed] [Google Scholar]
- 41.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 42.Steel Z, Silove D, Bird K, McGorry P, Mohan P. Pathways from war trauma to posttraumatic stress symptoms among Tamil asylum seekers, refugees, and immigrants. J Trauma Stress. 1999;12(3):421–435. 10.1023/A:1024710902534 [DOI] [PubMed] [Google Scholar]
- 43.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 44.Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Al-Smadi AM, Tawalbeh LI, Gammoh OS, Ashour A, Tayfur M, Attarian H. The prevalence and the predictors of insomnia among refugees. J Health Psychol. 2019;24(8):1125–1133. [DOI] [PubMed] [Google Scholar]
- 46.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. 10.5665/sleep.2810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jenkins MM, Colvonen PJ, Norman SB, Afari N, Allard CB, Drummond SPA. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep. 2015;38(10):1547–1554. 10.5665/sleep.5044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Arch Gen Psychiatry. 1997;54(4):337–343. 10.1001/archpsyc.1997.01830160065009 [DOI] [PubMed] [Google Scholar]
- 49.Al Laham D, Ali E, Mousally K, Nahas N, Alameddine A, Venables E. Perceptions and health-seeking behaviour for mental illness among Syrian refugees and Lebanese community members in Wadi Khaled, North Lebanon: a qualitative study. Community Ment Health J. 2020;56(5):875–884. 10.1007/s10597-020-00551-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schlaudt VA, Bosson R, Williams MT, et al. Traumatic experiences and mental health risk for refugees. Int J Environ Res Public Health. 2020;17(6):1943. 10.3390/ijerph17061943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gutner CA, Pedersen ER, Drummond SPA. Going direct to the consumer: examining treatment preferences for veterans with insomnia, PTSD, and depression. Psychiatry Res. 2018;263:108–114. 10.1016/j.psychres.2018.02.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nappi CM, Drummond SPA, Hall JMH. Treating nightmares and insomnia in posttraumatic stress disorder: a review of current evidence. Neuropharmacology. 2012;62(2):576–585. 10.1016/j.neuropharm.2011.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Enticott JC, Shawyer F, Vasi S, et al. A systematic review of studies with a representative sample of refugees and asylum seekers living in the community for participation in mental health research. BMC Med Res Methodol. 2017;17(1):37. 10.1186/s12874-017-0312-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Geng F, Liang Y, Li Y, et al. Bidirectional associations between insomnia, posttraumatic stress disorder, and depressive symptoms among adolescent earthquake survivors: a longitudinal multiwave cohort study. Sleep. 2019;42(11):zsz162. 10.1093/sleep/zsz162 [DOI] [PubMed] [Google Scholar]
- 55.Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. 2011;67(12):1240–1258. 10.1002/jclp.20845 [DOI] [PubMed] [Google Scholar]
- 56.Bernardi J, Jobson L. Investigating the moderating role of culture on the relationship between appraisals and symptoms of posttraumatic stress disorder. Clin Psychol Sci. 2019;7(5):1000–1013. 10.1177/2167702619841886 [DOI] [Google Scholar]
- 57.Nagulendran A, Jobson L. Exploring cultural differences in the use of emotion regulation strategies in posttraumatic stress disorder. Eur J Psychotraumatol. 2020;11(1):1729033. 10.1080/20008198.2020.1729033 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.