Abstract
Background
Postpartum depression (PPD) has been identified as a recognized public health problem that may adversely affect mothers, infants, and family units. Recent studies have identified risk factors for PPD in Westerners; however, societal and cultural differences between China and the West could, potentially, lead to differences in risk factors for PPD. No comprehensive study has been conducted to collect all the evidence to provide estimates of psychological and social risk factors in China. Therefore, this study aimed to quantitatively assess all studies meeting the review’s eligibility criteria and identify the psychological and social risk factors for PPD in Chinese women.
Methods
The following databases were used in the literature search from their inception until December 2020: PubMed, Embase, Foreign Medical Literature Retrieval Service (FMRS), China Science and Technology Journal Database (VIP), China National Knowledge Infrastructure (CNKI), and China Biology Medicine disc (CBM). The quality was assessed through Newcastle-Ottawa quality assessment scale. The I2statistic was used to quantify heterogeneity. We extracted data for meta-analysis and generated pooled-effect estimates from a fixed-effects model. Pooled estimates from a random-effects model were also generated if significant heterogeneity was present. Funnel plot asymmetry tests were used to check for publication bias. Statistical analysis was conducted using Review Manager version 5.3 software.
Results
From a total of 1175 identified studies, 51 were included in the analysis. Prenatal depression (OR 7.70; 95% CI 6.02–9.83) and prenatal anxiety (OR 7.07; 95% CI 4.12–12.13) were major risk factors for PPD. A poor economic foundation (OR 3.67; 95% CI 3.07–4.37) and a poor relationship between husband and wife (OR 3.56; 95% CI 2.95–4.28) were moderate risk factors. Minor risk factors included a poor relationship between mother-in-law and daughter-in-law (OR 2.89; 95% CI 2.12–3.95), a lack of social support (OR 2.57; 95% CI 2.32–2.85), unplanned pregnancy (OR 2.55; 95% CI 2.08–3.14), and poor living conditions (OR 2.44; 95% CI 1.92–3.10), mother-in-law as the caregiver (1.95; 95% CI 1.54–2.48) .
Conclusions
This study demonstrated a number of psychological and social risk factors for PPD in Chinese women. The major and moderate risk factors are prenatal depression, prenatal anxiety, a poor economic foundation, and a poor relationship between husband and wife. These findings have potential implications for informing preventive efforts and modifying screening to target at-risk populations.
Keywords: Postpartum depression, Risk factors, Meta-analysis, Psychosocial
Background
Postpartum depression (PPD) is the most common type of nonpsychotic psychiatric syndrome during the perinatal period [1]. The Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) defines PPD as a depressive episode with moderate-to-severe symptoms that begins 4 weeks after delivery [2]. The prevalence of PPD varies from 0.5 to 60.8% around the world and from 3.5 to 63.3% in Asian countries, as measured using the Edinburgh Postpartum Depression scale (EPDS) [3]. The prevalence of PPD in China is 27.37% [4], and is increasing yearly [5]. PPD has been identified as a recognized public health problem that not only affects mothers’ health but also causes poor developmental outcomes in children and poor relationships in families [6].
Postpartum depressive symptoms include the inability to sleep, anxiety, sadness, extreme concern and worry about the baby, and even recurrent thoughts of death [7]. Because maternal emotion plays an important role in the development of children, the pathogenesis of PPD merits greater attention. At present, studies involving Chinese women have reported that poor relationships with husbands or mothers-in-law, introverted maternal personality, anxiety or depression during pregnancy, an unsmooth delivery process, poor postpartum sleep quality, dissatisfaction with neonatal sex, and poor health conditions of newborns were risk factors for PPD [8]. Although several risk factors have been identified, the results of some risk factors are still controversial. Of note, these reviews included some case-control studies and cross-sectional studies, which limited the strength and quality of such evidence.
In addition, review [9] on the risk factors for PPD have primarily included studies conducted in Western populations and have overlooked many studies undertaken in the Chinese cultural context. Western and Chinese women differ considerably in terms of genetics, philosophical traditions, cultural practices, ethnicity, religion, and attitudes toward psychological problems [10]. The two different cultural backgrounds lead to differences in the psychosocial risk factors for PPD [11]. Given the deeply rooted influence of the Chinese cultural traditions of Confucianism, Buddhism and Taoism, the thought processes of Chinese females have historically been more traditional and conservative in nature [12]. Some studies have shown that culturally and characteristically Westerners are more extroverted, while characteristically Chinese people are more introverted - introverted women with personality types that are dependent are more prone to experience PPD [13, 14].
In addition, although some Chinese individuals have emigrated to other countries, they have been influenced by traditional Chinese culture for a long time; thus their personality and their family structure are still similar to those of individuals in their motherland. In particular, many Chinese immigrant women continue to observe the Chinese traditional postpartum practices. Thus the aim of this review was to synthesis the evidence from eligible studies to identify the psychosocial risk factors for PPD in Chinese women, including those living in other countries.
Methods
Search strategy
A systematic search of the electronic databases PubMed, Embase, Foreign Medial Literature Retrieval Service (FMRS), the China Science and Technology Journal Database (VIP), China National Knowledge Infrastructure (CNKI), and China Biology Medicine disc (CBM) was performed for relevant studies published before June 2019. Chinese search terms included PPD, risk factors, influencing factors, social factors, and psychological factors. English search terms included the following: Postnatal Depression OR Depression, Postnatal OR Post-Partum Depression OR Depression, Post-Partum OR Post Partum Depression OR Postpartum Depression OR Post-Natal Depression OR Depression, Post-Natal OR Post Natal Depression AND Factor, Risk OR Factors, Risk OR Risk Factor OR Population at Risk OR Risk, Population at OR Populations at Risk OR Risk, Populations at AND Chinese OR in China. Additionally, we also performed a manual search of the reference lists of retrieved articles and recent reviews.
Population (P)
Chinese women who have given birth to at least one child, including those living in countries other than China.
Exposure (E)
A woman who has experienced childbirth and has been exposed to a risk factor for PPD.
Outcome (O)
PPD is the most common type of nonpsychotic psychiatric syndrome during the perinatal period, as a depressive episode with moderate-to-severe symptoms that begins 4 weeks after delivery.
Selection criteria
This systematic review and meta-analysis considered all studies on psychosocial risk factors for PPD in Chinese women, including Chinese women currently living in other countries.
Exclusion criteria
The title and abstracts of retrieved studies were assessed against the review’s inclusion criteria. Papers that were inaccessible, and those that did not report associated risk factors for PPD were excluded. Studies that were not a case-control study or a cohort study were also excluded. Once more, studies that did not report relative risks (RRs) or odds ratios (ORs) with corresponding 95% confidence intervals (CIs) or the numbers of women with PPD were also excluded from this review.
Data extraction and quality assessment
Data extraction and quality assessment was done by two reviewers independently. Disputes were discussed between the reviewers until consensus was reached. Data extracted from the studies included the first author, year, study sites, sample size, PPD Group, assessment method, quality score, investigation time, as well as risk factors associated with PPD. Articles that fulfilled the predefined criteria were used as a source of data for the final analysis.
The instrument versions were Chinese. The risk factors were assessed by questionnaire and interview. We used the Newcastle-Ottawa Scale (NOS) to assess the quality of the selected cohort and case-control studies [15]. The NOS was used to score the studies on three criteria: the selection of the study groups; the comparability of the groups; and the ascertainment of outcome or exposure. The total score ranged from 0 to 9, with higher scores representing higher methodological quality and lower risk of bias.
Statistical analysis
The number of cases of PPD and the number of cases in the control group were converted into the form of odds ratios (ORs) with 95% confidence intervals (CIs), which were used to pool the outcome data. The Cochrane Q test was performed to assess statistical heterogeneity, and the Higgins I2 statistic was used to determine the extent of variation between effect estimates (0 to 100%). For outcomes with low heterogeneity, I2 < 50% and p > 0.1, the fixed-effects model (M-H method) was used for analysis. In addition to I2 ≥ 50% or p < 0.1, the random-effects model (D-l method) was used [16]. The sensitivity analysis was carried out by changing the model method. Publication bias was evaluated via the visual analysis of funnel plots. In the absence of bias, showing a symmetrical inverted funnel. When drawing a funnel chart, at least 10 studies are needed. The funnel plot may not detect publication bias when the number of studies is small [17]. Statistical analyses were performed using Review Manager 5.3 (Cochrane Collaboration, UK).
Results
Literature search
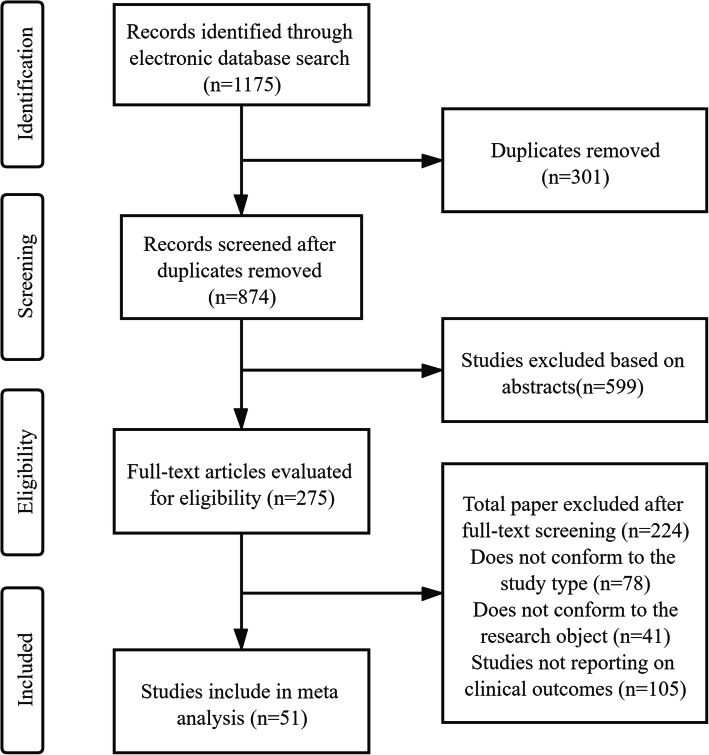
A total of 1175 studies were obtained through six database searches, of which 301 were excluded because of duplicates. Most articles (n = 599) were excluded after the title and abstract information were reviewed. Then, 224 articles that did not meet the inclusion criteria were excluded after the full text was reviewed. Finally, the meta-analysis included 51studies, and the study selection process is shown in Fig. 1.
Fig. 1.
Flowchart steps of the meta analysis
Study characteristics
A total of 36,705 perinatal women were included across the 12 cohort studies and 39 case-control studies, with 7008 women identified as having PPD. The studies investigated Chinese women in mainland China and Hong Kong, and Canadian immigrants. The EPDS and Self-Rating Depression Scale (SDS) were the most common instruments used to assess PPD. The quality score of the included studies ranged from 5 to 8, and 13 studies were scored 7 or more. The study characteristics and quality evaluation are summarized in Table 1.
Table 1.
Characteristics of included studies
| First author | Year | study sites | Sample size | PPD Group | Assessment method | Quality scores | Investigate time | Risk factors |
|---|---|---|---|---|---|---|---|---|
| Lee [18] | 2004 | Hong Kong | 781 | 122 | EPDS | 8 | first trimester/ 6 weeks postpartum | (1),(5) |
| Zhao [19] | 2018 | Shanghai | 215 | 67 | EPDS | 7 | late pregnancy/ week 3-days and 6-weeks after delivery | (1) |
| Pan [20] | 2004 | Sichuan | 427 | 33 | EPDS | 6 | third trimester/ 4 ~ 6 weeks postpartum | (1),(3) |
| Zhao [21] | 2018 | Sichuan | 1440 | 25 | EPDS | 6 | third trimester/ 8,18 weeks postpartum | (1) |
| Siu [18] | 2012 | Hong Kong | 805 | 126 | EPDS | 7 | third trimester/ around 2 months postnatally | (4),(5) |
| Li [22] | 2017 | Shanxi | 1759 | 593 | EPDS | 6 | third trimester/ 4 weeks postpartum | (4),(6) |
| Gu [23] | 2004 | Shanghai | 999 | 307 | HADS | 6 | Second trimester/ 4 weeks postpartum | (3),(4) |
| Sun [24] | 2015 | Yunnan | 528 | 96 | EPDS | 6 | third trimester/ 4 weeks postpartum | (6) |
| Kang [25] | 2015 | Jiangsu | 3972 | 468 | EPDS> 10 | 6 | first trimester/ 6 weeks postpartum | (6) |
| Dennis [26] | 2017 | Canadian immigrants | 549 | 120 | EPDS> 9 | 8 | third trimestery/ 4 weeks postpartum | (6) |
| Cai [27] | 2017 | Chongqing | 371 | 60 | EPDS≥13 | 7 | Second trimester/ 6 weeks postpartum | (6) |
| Hu [28] | 2010 | Sichuan | 264 | 146 | EPDS> 9 | 6 | Second trimester/ 4 weeks postpartum | (4) |
| Gu [29] | 2017 | Xinjiang | 824 | 286 | EPDS> 13 | 6 | 42 days postpartum | (1),(2) |
| Zhang [30] | 2017 | Guangdong | 538 | 49 | EPDS> 10 | 7 | 42 days postpartum | (1),(2) |
| Wu [31] | 2019 | Guangdong | 1437 | 100 | EPDS> 10 | 6 | 4 weeks postpartum | (1),(2) |
| Shen [32] | 2011 | Shanxi | 104 | 52 | EPDS> 13 | 6 | 4 weeks postpartum | (1) |
| Yang [33] | 2016 | Hubei | 400 | 37 | EPDS> 13 | 6 | 4 ~ 6 weeks postpartum | (1),(3),(8) |
| Zhang [34] | 2001 | Tianjin | 463 | 47 | EPDS≥13 | 7 | 4 weeks postpartum | (4) |
| Yin [35] | 2011 | Guangdong | 202 | 37 | SDS > 40 | 5 | 4 weeks postpartum | (3),(4) |
| Huang [36] | 2012 | Hunan | 302 | 56 | EPDS | 6 | 6 ~ 7 weeks postpartum | (4) |
| Song [37] | 2012 | Hunan | 285 | 69 | SDS | 5 | 4 weeks postpartum | (3),(4),(5) |
| Wang [38] | 2013 | Beijing | 435 | 27 | SCL-90 > 2 | 6 | 42 days postpartum | (4) |
| Lin [39] | 2014 | Zhejiang | 2023 | 204 | EPDS | 5 | 42 days postpartum | (4) |
| Zhou [40] | 2014 | Hubei | 378 | 294 | EPDS/SDS | 5 | 4 ~ 6 weeks postpartum | (4) |
| Wang [41] | 2014 | Guizhou | 875 | 112 | EPDS | 7 | 42 days postpartum | (3),(4),(8) |
| Chen [42] | 2017 | Zhejiang | 380 | 260 | EPDS> 13 | 7 | 42 days postpartum | (4),(8) |
| Jiang [43] | 2018 | Shandong | 185 | 25 | EPDS | 5 | 6 weeks postpartum | (4) |
| Han [44] | 2018 | Henan | 248 | 124 | EPDS> 10 | 5 | 4 weeks postpartum | (4) |
| He [45] | 2019 | Zhejiang | 398 | 217 | SDS EPDS | 5 | 4 weeks postpartum | (4) |
| Yu [46] | 2010 | Shanghai | 673 | 73 | EPDS | 7 | 6 weeks postpartum | (3),(7) |
| Zhang [47] | 2012 | Hunan | 215 | 67 | EPDS> 13 | 6 | 30 ~ 42 days postpartum | (7) |
| Zhang [48] | 2014 | Guangdong | 586 | 87 | EPDS> 13 | 6 | 6 weeks postpartum | (7) |
| Li [49] | 2014 | Anhui | 687 | 103 | EPDS | 7 | 6 weeks postpartum | (3),(7) |
| Liu [50] | 2015 | Hunan | 232 | 43 | EPDS/HAD | 5 | 42 days postpartum | (7) |
| Liu [51] | 2015 | Heilongjiang | 576 | 162 | EPDS | 6 | 42 days postpartum | (6),(7) |
| Chen [52] | 2018 | Northwest China | 640 | 84 | EPDS> 13 | 6 | 6 weeks postpartum | (7),(9) |
| Wang [53] | 2013 | Shandong | 917 | 168 | EPDS/SDS | 5 | 6 weeks postpartum | (3) |
| Li [54] | 2019 | Shanxi | 170 | 85 | SDS | 5 | 6 weeks postpartum | (3),(6) |
| Guan [55] | 2012 | Inner Mongolia | 246 | 92 | EPDS> 9 | 6 | 30 ~ 42 days postpartum | (9) |
| Zhang [56] | 2011 | Hubei | 479 | 167 | BDI > =5 | 6 | 7 ~ 30 days postpartum | (9) |
| Deng [57] | 2014 | Guangdong | 2021 | 158 | CES-D > 20 | 6 | 42 days postpartum | (5) |
| Deng [4] | 2014 | Guangdong | 1823 | 499 | EPDS> 13 | 7 | 4 weeks postpartum | (5) |
| Han [58] | 2015 | Beijing | 203 | 189 |
EPDS> 13 HAD> 9 |
6 | 42 days postpartum | (5),(8) |
| Liu [59] | 2017 | Guangdong | 418 | 93 | EPDS> 9.5 | 5 | 4 ~ 6 weeks postpartum | (5) |
| Zhou [60] | 2019 | Jiangsu | 849 | 142 | EPDS> 10 | 6 | 2 ~ 6 weeks postpartum | (5) |
| Liu [61] | 2015 | Hubei | 1427 | 198 | EPDS≥9 | 5 | 42 days postpartum | (6),(8) |
| Xie [62] | 2018 | Hubei | 534 | 103 | EPDS | 6 | 6 weeks postpartum | (6) |
| Pan [63] | 2015 | Zhejiang | 745 | 93 | EPDS | 5 | 42 days postpartum | (2) |
| Yang [64] | 2020 | Jiangxi | 371 | 94 | EPDS | 6 | 42 days postpartum, third trimester, | (3),(4),(9) |
| Huang [65] | 2020 | Jiangsu | 784 | 59 | EPDS | 6 | 42 days postpartum | (3) |
| Qing [66] | 2020 | Guangdong | 522 | 90 | EPDS | 7 | 2nd to 4th postnatal months | (9) |
Risk factors: (1) Prenatal depression, (2) prenatal anxiety, (3) poor economic foundation, (4) poor relationship between husband and wife, (5) poor relationship between mother-in-law and daughter-in-law, (6) lack of social support, (7) unplanned pregnancy and (8) poor living conditions, (9) mother-in-law as the caregiver
PPD postpartum depression, EPDS Edinburgh postnatal depression scale, HADS Hospital Anxiety and Depression Scale, SDS self-rating depression scale, SCL-90 symptom checklist 90, BDI beck depression inventory, CES-D Center for Epidemiological Studies Depression Scale
Quantitative synthesis
Case-control studies and cohort studies
Seventeen studies (13 case-control studies and 4 retrospective cohort studies) reported that a poor relationship between husband and wife was associated with an increased risk of PPD (OR = 3.56; 95% CI 2.95–4.28; I2 = 30%; p < 0.00001) (Fig. 2).
Fig. 2.
Poor relationship between husband and wife
Eleven studies (10 case-control studies, 2 retrospective cohort studies) investigated the association between poor economic foundation and the risk of PPD (OR = 3.67; 95% CI 3.07–4.37; I2 = 22%; p < 0.00001) (Fig. 3).
Fig. 3.
Poor economic foundation
Nine studies (5 case-control studies, 4 retrospective cohort studies) investigated the association between prenatal depression and the risk of PPD (OR = 7.70; 95% CI 6.02–9.83; I2 = 69%; p < 0.00001) (Fig. 4). Thus, poor economic foundation and prenatal depression were significantly related to PPD.
Fig. 4.
Prenatal depression
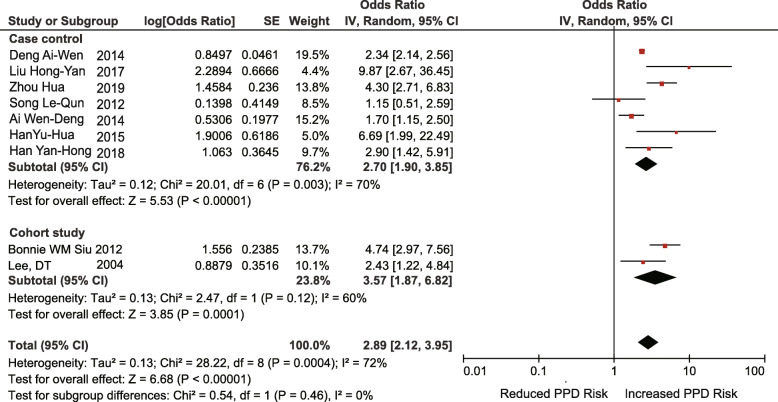
Nine studies (7 case-control studies, 2 retrospective cohort studies) reported that a poor relationship between mother-in-law and daughter-in-law was associated with an increased risk of PPD (OR = 2.89; 95% CI 2.12–3.95; I2 = 72%; p < 0.00001) (Fig. 5).
Fig. 5.
Poor relationship between mother-in-law and daughter-in-law
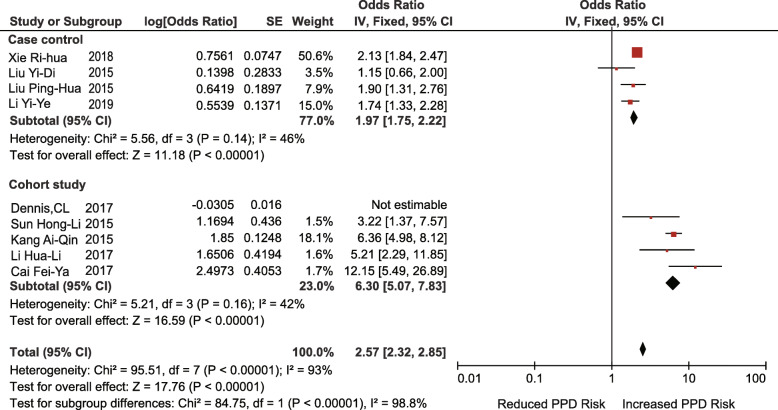
Nine studies (4 case-control studies, 5 retrospective cohort studies) investigated the association between a lack of social support and the risk of PPD (OR = 2.66; 95% CI 1.57–4.53; I2 = 98%; p = 0.0003). After subgroup analysis according to the type of study design, the heterogeneity of the case-control group decreased (I2 = 46%, p = 0.14), but the heterogeneity of the cohort group was still very high (I2 = 99%, p < 0.00001). The heterogeneity of the cohort group decreased significantly when one study was excluded [67]. (I2 = 42%, p = 0.16) (Fig. 6, 7). This may be due to major differences in social support between Chinese-Canadian women and Chinese women [26].
Fig. 6.
Lack of social support (before adjustment)
Fig. 7.
Lack of social support (after adjustment)
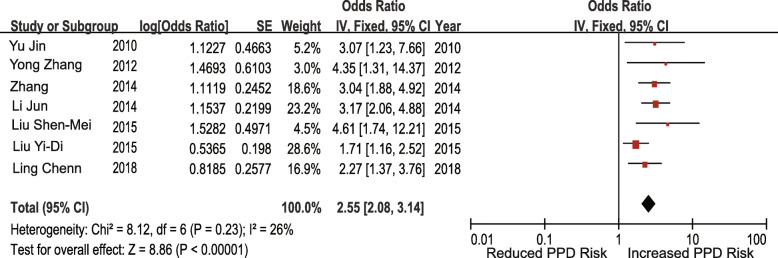
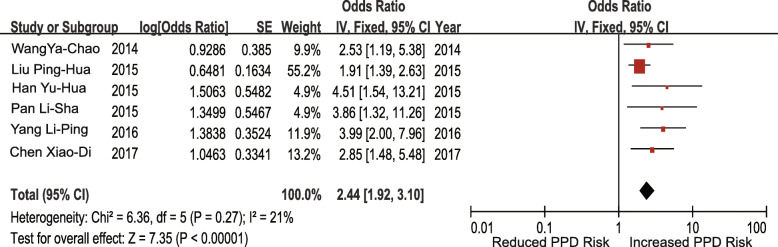
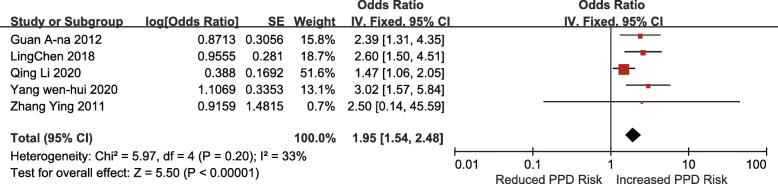
Case-control studies
Seven studies investigated the association between unplanned pregnancy and the risk of PPD. The pooled OR for unplanned pregnancy was 2.55 (95% CI 2.08–3.14; I2 = 26%; p < 0.00001) (Fig. 8). Six studies investigated the association between poor living conditions and the risk of PPD. The pooled OR for poor living conditions was 2.44 (95% CI 1.92–3.10; I2 = 21%; p < 0.00001) (Fig. 9). Four studies investigated the association between prenatal anxiety and the risk of PPD. The pooled OR for prenatal anxiety was 7.07 (95% CI 4.12–12.13; I2 = 59%; p < 0.00001), and a random-effects model was adopted (Fig. 10). Five studies investigated the association between mothers-in-law as caregivers and the risk of PPD. The pooled OR for mothers-in-law as caregivers was 1.95 (95% CI 1.54–2.48; I2 = 33%; p < 0.00001) (Fig. 11).
Fig. 8.
Unplanned pregnancy
Fig. 9.
Poor living conditions
Fig. 10.
Prenatal anxiety
Fig. 11.
Mother-in-law as the caregiver
Therefore, unplanned pregnancy, poor living conditions, prenatal anxiety, and mothers-in-law as caregivers were found to be significantly associated with PPD.
Heterogeneity test and sensitivity analysis
The results of 51 studies were tested by the Cochrane Q test. The heterogeneity test results of the seven risk factors were low or medium (prenatal depression, poor economic foundation, poor relationship with partner, lack of social support, unplanned pregnancy, mothers-in-law as caregivers, and poor living conditions). However, for the poor mother-in-law relationship and prenatal anxiety, the random-effects model was used because of the high heterogeneity. Among them, the high heterogeneity of the poor relationship between mother-in-law and daughter-in-law may be due to the lack of targeted questionnaire surveys, the setting of the questionnaires being more subjective, and the measurement standard more difficult to unify. The high heterogeneity of prenatal anxiety may be due to the different times of prenatal measurement [17]. In sensitivity analyses, the change model method was used to estimate the point and interval of the OR values of all risk factors to judge the stability of the meta-analysis (Table 2). The point estimates of the combined OR values of the fixed-effects model and the random-effects model were similar, and the interval estimation range of the random-effects model was slightly wider than that of the fixed-effects model. This result indicated that the comprehensive analysis results of the influencing factors in this study were reliable overall.
Table 2.
Sensitivity analysis of risk factors of PPD
| Fixed effect model | Random effect model | ||||
|---|---|---|---|---|---|
| Risk factors | Type of research | OR | 95%CI | OR | 95%CI |
| Prenatal depression | Cohort study | 4.21 | [2.82, 6.27] | 4.40 | [2.64, 7.34] |
| Case control study | 11.09 | [8.13, 15.12] | 12.72 | [7.85, 20.62] | |
| marriage relationship | Cohort study | 5.76 | [3.86, 8.59] | 5.76 | [3.27, 10.13] |
| Case control study | 3.12 | [2.53, 3.84] | 3.12 | [2.53, 3.84] | |
| Mother-in-law relationship | Cohort study | 3.84 | [2.61, 5.65] | 3.57 | [1.87, 6.82] |
| Case control study | 2.37 | [2.17, 2.58] | 2.70 | [1.90, 3.85] | |
| Social support | Cohort study | 6.30 | [5.07, 7.83] | 6.18 | [4.10, 9.31] |
| Case control study | 1.97 | [1.75, 2.22] | 1.85 | [1.52, 2.25] | |
| Economic foundation | Cohort study | 3.50 | [1.65, 7.43] | 3.67 | [2.97, 4.55] |
| Case control study | 3.68 | [3.07, 4.40] | 4.46 | [1.09, 8.20] | |
| Unplanned pregnancy | Case control study | 2.55 | [2.08, 3.14] | 2.64 | [2.04, 3.40] |
| Prenatal anxiety | Case control study | 7.93 | [5.76, 10.90] | 7.07 | [4.12, 12.13] |
| Mother-in-law as the caregiver | Case control study | 1.95 | [1.54, 2.48] | 2.11 | [1.52, 2.93] |
| Living conditions | Case control study | 2.44 | [1.92, 3.10] | 2.65 | [1.96, 3.57] |
ORs odds ratios, CIs corresponding 95% confidence intervals
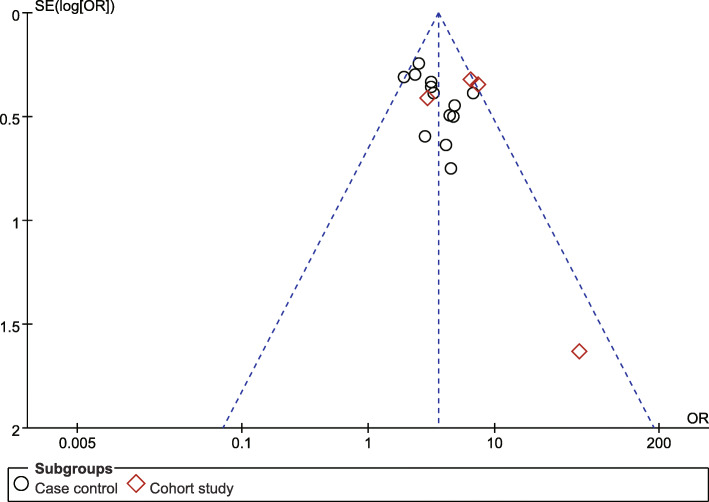
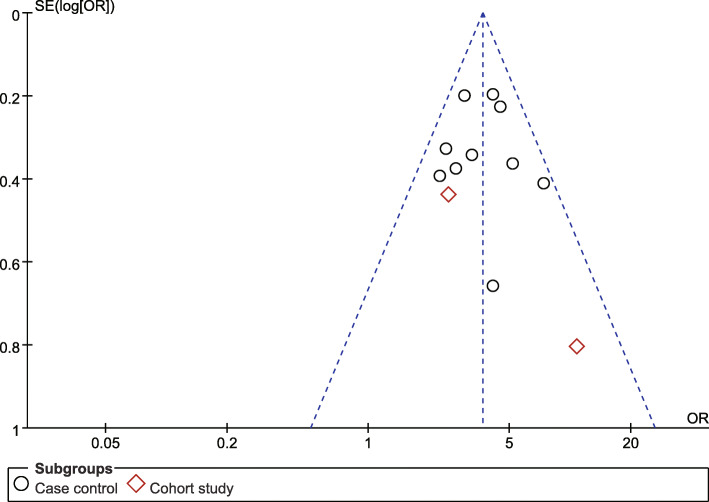
Publication bias
Publication bias was evaluated via the visual analysis of funnel plots. The funnel plot generally appeared to be symmetrical, indicating no publication bias (Fig. 12, 13).
Fig. 12.
Poor relationship between husband and wife funnel plot
Fig. 13.
Poor economic foundation funnel plot
Discussion
PPD is a crucial part of the spectrum of mood disturbances affecting postpartum women. A variety of factors affect the physical and mental health of pregnant women. Thus, identifying alterable risk factors for PPD and controlling them at an early stage are essential for the treatment and prevention of this condition.
The psychosocial risk factors for PPD in Chinese women identified in this meta-analysis mainly included three kinds: prenatal emotional factors (prenatal anxiety and prenatal depression), social demographic factors (poor marital relationship, poor living conditions, lack of social support, and unplanned pregnancy) and social and interpersonal factors (poor relationship between husband and wife, poor relationship between mother-in-law and daughter-in-law,and mother-in-law as the caregiver). First, prenatal anxiety and depression were significantly associated with an increased risk of PPD, as confirmed by some Western studies. An Italian study [68] showed that women with depression or anxiety during pregnancy and a lack of support from family and friends were at a higher risk of PPD. This result has also been confirmed in China. According to the report of Lee [69], most PPD was the continuation of prenatal psychological problems and emotional disorders, indicating a significant correlation between prenatal psychological status and the occurrence of PPD.
Another explanation for the effect of prenatal emotional distress is physiological changes. For example, excessive anxiety and depression in pregnant women may lead to a series of physiological and pathological reactions, such as a decrease in norepinephrine secretion and changes in other endocrine hormones, which may lead to the weakening of uterine contractions, a prolonged stage of labor, and increased bleeding. These challenges further aggravate the anxiety of pregnant women and lead to an increased risk of developing PPD [70].
Second, this study found that social demographic factors were also risk factors for PPD, such as a poor economic foundation, poor living conditions, a lack of social support, and unplanned pregnancy. Among them, the economic foundation of the family had an important effect on the psychological status of the mother. Previous reviews suggested that the status of the family’s economic income was positively related to the level of stress in pregnant women. Yu [46] suggested that after adjustments were made for other related factors, the incidence of PPD among women who were worried about family economic status was 3.162 times higher than among those who did not worry about it. The probable explanation may be that after childbirth, the cost of raising the baby and the basic cost of living for the family significantly increases. If the family income is insufficient, it will lead to high levels of pressure for pregnant women and can easily cause negative emotions. In recent years, with China’s two-child policy, raising multiple children in a family increases the family’s financial burden, which may be a factor of PPD. A study in Turkey shows that there was a significant relationship between monthly income and depression, which was similar to the results of the present study [71].
In addition, previous studies have shown that social support was a protective factor against PPD, and as far as mothers were concerned, the greatest social support comes from their husbands. Xiong et al. [72] suggested that puerperae with spousal support were much less likely to develop PPD. A Chinese study also confirmed that high levels of social support can reduce the risk of PPD, with other factors were fixed [27]. Our findings are generally consistent with those of previous reviews. Therefore, giving adequate social support to parturients during the puerperal period can help them get through this critical period smoothly.
Third, in this study, the interpersonal risk factors for PPD were a poor relationship between husband and wife, a poor relationship between mother-in-law and daughter-in-law, and mother-in-law as the caregiver. The poor relationship between husbands and wives, as an important factor affecting human physical and mental health, has attracted the close attention of researchers worldwide. Zhang [73] suggested that the quality of the husband-wife relationship was mainly reflected in the quality of the husband’s care for his wife, and women who were less satisfied with their husband’s care were more likely to have depression. Poor marriage and family relationships will not only reduce maternal social support but also become a maternal stressful life event, which brings about an increased risk of developing PPD. This study was confirmed in a Polish study. Malus et al. [74] confirmed the significance of the marital relationship in the development of PPD. A sense of closeness and intimacy in the relationship were associated with better mood and a greater ability to cope with the difficulties of labor, puerperium, and caring for a newborn baby.
In addition, the results of this study found that the risk factors for PPD related to Chinese cultural characteristics included the mother-in-law as the caregiver and a poor relationship between mother-in-law and daughter-in-law.
From the perspective of family structure, Chinese families have a close relationship, intergenerational support shows a circular mode, and it is very common to expand families, especially families with three generations living together. Even if the whole family emigrates to other countries, it is still common for parents to live together with their children’s families. The kinship network linked by blood relationship is complicated, and the conflict increases accordingly [75].
In Western countries, nuclear families are the main organizational form; they attach importance to the development of personality, pay attention to independence and privacy, and think that the lifestyle of several generations living together seriously infringes upon the privacy of individuals, which is unbearable. Therefore, adult children live independently of their parents. Kinship is more distant than that of China, and contradictions and intergenerational conflicts are correspondingly less [76].
Traditionally, mothers-in-law exercise significant power in the family and are a major influence on the postpartum care of new mothers. In China, due to the influence of doing-the-month culture, mothers and newborns are mostly cared for by their mothers-in-law. The strain between mothers-in-law and daughters-in-law is a sensitive problem and may be a cause of PPD in China. Steinberg [77] indicated that the strain between mothers-in-law and daughters-in-law often offset the benefits of assistance and may even contribute to negative mood during the postpartum period. In traditional Confucian philosophy, the new mother should be considered a good daughter-in-law if she behaves in a way that is respectful at home and is obedient to her in-laws and husband [78]. The relationship between women and their parents-in-law is based on the environment rather than consanguinity. Sometimes they are reluctant to express their own feelings and opinions to their in-laws. New mothers feel very stressed when they have opinions different from their care providers. The situation may become even worse when conflicts occur with mothers-in-law. Because of the differences in backgrounds, values, identity, and logic of ideas, conflicts with respect to childcare between women and their mothers-in-law become prominent [18].
Limitations
This study had several inevitable limitations. First, some risk factors have received less attention; for example, non-uniform measurement standards and statistical difficulties have not been combined, such as the type of residence, postpartum wound recovery, postpartum work stress, and maternal occupation. Second, PPD is the result of the interaction of multiple factors, but due to methodological limitations, it is difficult to investigate the interaction among risk factors. Third, in terms of language selection, this study only includes literature in Chinese and English, which may lead to bias in the comprehensiveness of the literature search, thus affecting the research results and the intensity of the argument.
In addition, this study covers a wide range of research sites, including pregnant Chinese women in mainland China and Hong Kong, and Canadian immigrants. Although some Chinese individuals have emigrated to other countries, they have been influenced by traditional Chinese culture for a long time; thus their personality and their family structure are still similar to those of individuals in their motherland. In particular, many Chinese immigrant women continue to observe the Chinese traditional postpartum practices.
Conclusion
In conclusion, psychosocial risk factors for PPD mainly include prenatal depression, prenatal anxiety, a poor economic foundation, a poor relationship between husband and wife, a poor relationship between mother-in-law and daughter-in-law, a lack of social support, unplanned pregnancy, the mother-in-law as the caregiver, and poor living conditions. These psychosocial risk factors are meaningful for identifying mothers “at-risk” during pregnancy even earlier. Meanwhile, some psychosocial interventions targeting these risk factors may be conducted during the pregnancy period to prevent PPD, such as interpersonal psychotherapy, mindfulness therapy, and psychoeducational programs.
Acknowledgements
We appreciate the contribution of all people who participated in this study. We are also grateful for the valuable insight and feedback from the reviewers and the editorial team.
Abbreviations
- PPD
Postpartum depression
- EPDS
Edinburgh Postnatal Depression Scale
- HADS
Hospital Anxiety and Depression Scale
- SDS
Self-rating depression scale
- SCL-90
Symptom checklist 90
- BDI
Beck depression inventory
- CES-D
Center for Epidemiological Studies Depression Scale
- VIP
the China Science and Technology Journal Database
- CNKI
China National Knowledge Infrastructure
- CBM
China Biology Medicine Disc
- RRs
Relative risks
- ORs
Odds ratios
- CIs
Corresponding 95% confidence intervals
- NOS
Newcastle-Ottawa Scale
Authors’ contributions
WQ, FZ, JH, YL, and QL were all involved in the processes of study design, data extraction, and statistical analysis. WQ wrote the manuscript. JH and FZ were responsible for the selection of articles. All authors read and approved the final version of the manuscript.
Funding
This work was supported by Hebei Education Department Humanities and Social Sciences Young Talent Project (Grant numbers: BJ2016082) and National Natural Science Foundation of China (Grants 72074067).
The funding organization was not involved in the design of the study or collection, analysis, and interpretation of data, or in writing the manuscript.
Availability of data and materials
Data will be available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Weijing Qi and Fuqing Zhao contributed equally to this work.
References
- 1.O'Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- 2.Diagnostic and Statistical Manual of Mental Disorders DSM-V. American Psychiatric Association. Washington, DC 2013;
- 3.Norhayati MN, Hazlina NH, Asrenee AR, Emilin WM. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. 2015;175:34–52. doi: 10.1016/j.jad.2014.12.041. [DOI] [PubMed] [Google Scholar]
- 4.Deng A, Xiong R, Jiang T, Luo Y, Chen W. Prevalence and risk factors of postpartum depression in a population-based sample of women in Tangxia community, Guangzhou. Asian Pac J Trop Med. 2014;7:244–249. doi: 10.1016/S1995-7645(14)60030-4. [DOI] [PubMed] [Google Scholar]
- 5.Mu T, Li Y, Pan H, Zhang L, Zha D, Zhang C, Xu R. Postpartum depressive mood (PDM) among Chinese women: a meta-analysis. Arch Women’s Ment Health. 2019;22:279–287. doi: 10.1007/s00737-018-0885-3. [DOI] [PubMed] [Google Scholar]
- 6.Johannsen BM, Larsen JT, Laursen TM, Ayre K, Howard LM, Meltzer-Brody S, Bech BH, Munk-Olsen T. Self-harm in women with postpartum mental disorders. Psychol Med. 2019;50:1–7. [DOI] [PubMed]
- 7.Chang H, Chen J, Huang Y, Chin-Hung CV. Prevalence and factors associated with depressive symptoms in mothers with infants or toddlers. Pediatr Neonatol. 2014;6:470–479. doi: 10.1016/j.pedneo.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Liu SX, Xia W. A Meta-analysis of risk factors of postpartum depression. Shanxi Med J. 2014;24:2847–2849. [Google Scholar]
- 9.Beck CT. A Meta-analysis of predictors of postpartum depression. Nurs Res. 1996;45:297–303. doi: 10.1097/00006199-199609000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Klainin P, Arthur DG. Postpartum depression in Asian cultures: a literature review. Int J Nurs Stud. 2009;46:1355–1373. doi: 10.1016/j.ijnurstu.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Guitian Z. A comparison of cultural characters between China and the west on “emotion and reason”. Yin du Acad J. 1993;04:63–66. [Google Scholar]
- 12.Zhao SQ. Analysis of the Causes of the Transformation of Female Concepts in Modern China. J Shandong Normal Univ (Humanities and Social Sciences) 2015;04:34–43. [Google Scholar]
- 13.Wang D, Hong C. Chinese “openness” Western “Open” Personality Dimension and Chinese Personality. J Southwest University (Humanities and Social Sciences Edition). 2006;06:1–10.
- 14.Li M, Deng H. Study on correlation between personality characteristics and postpartum depression in primiparous women in Beijing city. Matern Child Health Care China. 2013;28:760–763. [Google Scholar]
- 15.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 16.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 17.Joseph Lau JPAI. The case of the misleading funnel plot. BMJ. 2006;333:597–600. doi: 10.1136/bmj.333.7568.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siu BW, Leung SS, Ip P, Hung SF, O'Hara MW. Antenatal risk factors for postnatal depression: a prospective study of Chinese women at maternal and child health centres. BMC Psychiatry. 2012;12:22. doi: 10.1186/1471-244X-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao Y, Munro-Kramer ML, Shi S, Wang J, Zhu X. A longitudinal study of perinatal depression among Chinese high-risk pregnant women. Women Birth. 2018;31:395–402. doi: 10.1016/j.wombi.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Pan XF, Lu ZM, Xiao J. Prospective study on occurrence of postnatal depression and its psychosocial risk factors. Matern Child Health Care China. 2004;11:28–30. [Google Scholar]
- 21.Zhao ZM, Zhao F, Yang X, Wen Y, Xu MY, Qi XR, Yang CX, Pan XF. Antenatal and postnatal depression in Chengdu, China: a longitudinal study. Chin J Dis Control Prev. 2018;22:1051–1054. [Google Scholar]
- 22.Li HL, Li WL, Liu DH. Related facter of postpartum depressionin1994 cases in a hospital in Xi’an. Chin J Woman Child Health Res. 2017;10:1374–1376. [Google Scholar]
- 23.Gu W, Tang YF, Huang YM, Shi SS. Study on incidence and risk factors associated with postpartum depression. Shanghai Med J. 2004;10:756–758. [Google Scholar]
- 24.Sun HL, Su H, Zhang J, Fan W. Analysis of Correlat ion factors of postpartum depression. J Kunming Med Univ. 2015;12:60–64. [Google Scholar]
- 25.Kang AQ, Wu CM, Yang L. The incidence status and effect factors of postpartum depression in Rudong county. Chin J Fam Plan. 2015;10:652–655. [Google Scholar]
- 26.Dennis CL, Brown HK, Wanigaratne S, Vigod SN, Grigoriadis S, Fung K, Marini F, Brennenstuhl S. Determinants of comorbid depression and anxiety postnatally: a longitudinal cohort study of Chinese-Canadian women. J Affect Disord. 2018;227:24–30. doi: 10.1016/j.jad.2017.09.033. [DOI] [PubMed] [Google Scholar]
- 27.Cai FY, Kuang L, Wang W, Li DQ, Cao J, Hui X. Prediction model for postpartum depression base on social psychological factors establishment and evaluation. Acad J Second Mil Univ. 2017;04:476–481. [Google Scholar]
- 28.Hu J, Wang YQ. Study on related risk factors of patients with pre -and postnatal depression. Nurs Res China. 2010;09:765–767. [Google Scholar]
- 29.Gu SS, Qian Y, Chen H, Fu R, Wang FQ, Cheng JY. Status and related factors of postpartum depression in patients with second child. Chin J Woman Child Health Res. 2017;10:1177–1180. [Google Scholar]
- 30.Zhang X, Li SF. Risk factors of postpartum depression of the parturients in Meilin and corresponding health care guidance. J Guangdong Med Univ. 2017;03:303–306. [Google Scholar]
- 31.Wu XQ, Ma J, Zhang Y, Zhu DL. Analysis of postpartum depression and its influencing factors in Futian District. Appl Prev Med. 2019;02:95–98. [Google Scholar]
- 32.Shen R. Investigation and analysis of postpartum depression status and its influence factors and psychological intervention research. Master Thesis, Shanxi Medical University; 2011.
- 33.Yang LP, Xu Q, Qi L. Risk factors and preventive measures of postpartum depression. Chin Clin Nurs. 2016;06:501–504. [Google Scholar]
- 34.Zhang X, Tu Q, Xi W, Jiang YL, Gao Y. A study of incidence and the related factors of postpartum depression. Chin J Psychiatry. 2001;04:47–49. [Google Scholar]
- 35.Yin J. The risk factors of postpartum depression and nursing strategy. Hebei Med. 2011;12:1673–1676. [Google Scholar]
- 36.Huang GH. Analysis of pathogenic factors of postpartum depression. Today Nurse. 2012;06:29–30. [Google Scholar]
- 37.Song LQ. Discussion on related factors and nursing countermeasures of postpartum depression. Today Nurse. 2012;01:77–79. [Google Scholar]
- 38.Wang XL, Dong Y, Zhou XM, Hou GZ, Qi JL, Guo L, Wang J. Risk factors of postnatal depression among women in urban nuclear family. China J Health Psychol. 2013;04:513–515. [Google Scholar]
- 39.Lin YP, Gu SQ, Shen HL. Analysis of the incidence and influencing factors of postpartum depression in 2023 parturients. Chin Rural Health Serv Adm. 2014;08:979–980. [Google Scholar]
- 40.Zhou Q, Zhang FZ. Analysis on related factors of postpartum depression and its preventive measures. Med Recapitulate. 2014;18:3417–3418. [Google Scholar]
- 41.Wang YC, Zou T, Deng B. Cross-sectional survey of postpartum depression in the old town of Guiyang City and analysis of its influencing factors. Pract Prev Med. 2014;10:1257–1260. [Google Scholar]
- 42.Chen XD, Jiang WW. Influencing factors and intervention measures of postpartum depression in rural pregnant women. Chin J Public Health Manage. 2017;06:877–879. [Google Scholar]
- 43.Yan J, Qin SH, Zhao YM, Li XY, Kun ML. Analysis of the incidence and influencing factors of postpartum depression in a grass-roots hospital. Guide China Med. 2018;10:135–136. [Google Scholar]
- 44.Han YH. Analysis of influencing factors of postpartum depression of pregnant women and related nursing countermeasures. J Shanxi Med Coll Contin Educ. 2018;01:111–113. [Google Scholar]
- 45.He KL, Tao M, Zhu XZ. Analysis of related factors of postpartum depression and preventive measure. Chin J Woman Child Health Res. 2019;06:705–707. [Google Scholar]
- 46.Yu J. The study of postpartum depression in Shanghai. Master Thesis, Fudan University; 2010.
- 47.Zhang Y, Zou S, Cao Y, Zhang Y. Relationship between domestic violence and postnatal depression among pregnant Chinese women. Int J Gynecol Obstet. 2012;116:26–30. doi: 10.1016/j.ijgo.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 48.Zhang H, Zhou P, Liu L. Analysis of relevant factors of postpartum depression in rural primiparas. Med J Chin People’s Health. 2014;4:1–5. [Google Scholar]
- 49.Li J, Wang X. Analysis of influencing factors of postpartum depression in parturients in northern Anhui. J Fuyang Inst Technol. 2104;02:51-53.
- 50.Liu S, Hu Y. Postpartum depression status and the influencing factors analysis. Chin Clin Nurs. 2015;04:281–283. [Google Scholar]
- 51.Liu Y, Li X, Zhang H, Liu Y. Current situation of postpartum depression and analysis of related social and psychological factors. Matern Child Health Care China. 2015;22:3794–3796. [Google Scholar]
- 52.Chen L, Ding L, Qi M, Jiang C, Mao X, Cai W. Incidence of and social-demographic and obstetric factors associated with postpartum depression: differences among ethnic Han and Kazak women of northwestern China. Peerj. 2018;6:e4335. doi: 10.7717/peerj.4335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang P. Analysis of related factors in 168 patients with postpartum depression. J Shandong Med Coll. 2013;04:278–280. [Google Scholar]
- 54.Li Y. Related risk factors for postpartum depression and its nursing intervention. J Clin Med Pract. 2019;6:126–128. [Google Scholar]
- 55.Guan A. Postpartum Depression Status and Influencing Factors of Hospitalized Parturients in Three General Hospitals of Baotou. Master Thesis: Shandong University; 2012. [Google Scholar]
- 56.Zhang Y. Study of psychosocial factors for postpartum depression among 479 Wome. Doctor Thesis, Huazhong University of Science and Technology; 2011.
- 57.Aiwen D, Ribo X, Jiang T, Luo Y, Wei D. Epidemiological study of postpartum depression among migrant women at Tianhe District of Guangzhou. J Pract Med. 2014;10:1648–1651. [Google Scholar]
- 58.Han YH. Investigation on the incidence and influencing factors of postpartum depression in a certain area. Guide China Med. 2015;12:107–108. [Google Scholar]
- 59.Liu H. Analysis on the influencing factors of postpartum depression in rural women in Doumen District of Zhuhai city and the prevention countermeasures. Matern Child Health Care China. 2017;14:3100–3102. [Google Scholar]
- 60.Zhou H, Qin Z, Yang X, Tang J, Mo J, Qian Q. Investigation and analysis of related factors of postpartum depression among women in Changzhou. Matern Child Health Care China. 2019;6:1347–1351. [Google Scholar]
- 61.Liu P, Ya X. Analysis of influencing factors and nursing strategies of postpartum depression. Matern Child Health Care China. 2014;33:5402–5403. [Google Scholar]
- 62.Xie R, He G, Koszycki D, Walker M, Wen SW. Fetal sex, social support, and postpartum depression. Can J Psychiatry. 2009;54:750–756. doi: 10.1177/070674370905401105. [DOI] [PubMed] [Google Scholar]
- 63.Pan L. An analysis of the higher risk factors engendering postpartum depression. Health Res. 2015;05:544–545. [Google Scholar]
- 64.Yang W. Discussion on risk factors of postpartum depression in rural women and nursing intervention. Med Forum. 2020;32:4718–4720. [Google Scholar]
- 65.Yun-xia H, Jiang-ye K. Investigation on the occurrence of depression in 784 postpartum women. China Foreign Med Treat. 2020;39:82–84. [Google Scholar]
- 66.Li Q, Yang S, Xie M, Wu X, Huang L, Ruan W, Liu Y. Impact of some social and clinical factors on the development of postpartum depression in Chinese women. BMC Pregnancy Childb. 2020;20:226. [DOI] [PMC free article] [PubMed]
- 67.Dan W, Jun-xia Z, Zhen-yun M, Hong-xia Z, Xiao-dong Z, Xue-yi W, Ping G. Discussing on the research of heterogeneity in Meta-analysis. Chin J Evid Based Med. 2009;9:1115–1118. [Google Scholar]
- 68.Palumbo G, Mirabella F, Gigantesco A. Positive screening and risk factors for postpartum depression. Eur Psychiat. 2017;42:77–85. doi: 10.1016/j.eurpsy.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 69.Lee DT, Yip AS, Leung TY, Chung TK. Ethnoepidemiology of postnatal depression. Prospective multivariate study of sociocultural risk factors in a Chinese population in Hong Kong. Br J Psychiatry. 2004;184:34–40. doi: 10.1192/bjp.184.1.34. [DOI] [PubMed] [Google Scholar]
- 70.Chen W, Li Y. Analysis of the effect of prenatal anxiety and depression on obstetric complications and pregnancy outcomes. Modern Medical Imageology. 2018;08:2886–2887. [Google Scholar]
- 71.Oztora S, Arslan A, Caylan A, Dagdeviren HN. Postpartum depression and affecting factors in primary care. Niger J Clin Pract. 2019;22:85–91. doi: 10.4103/njcp.njcp_193_17. [DOI] [PubMed] [Google Scholar]
- 72.Xiong R, Deng A, Wan B, Liu Y. Prevalence and factors associated with postpartum depression in women from single-child families. Int J Gynecol Obstet. 2018;141:194–199. doi: 10.1002/ijgo.12461. [DOI] [PubMed] [Google Scholar]
- 73.Zhang YL, Zhang QG, Han JL, et al. Med Philos (Clinical Decision Making Forum Edition) 2008;02:57–58. [Google Scholar]
- 74.Malus A, Szyluk J, Galinska-Skok B, Konarzewska B. Incidence of postpartum depression and couple relationship quality. Psychiatr Pol. 2016;50:1135–1146. doi: 10.12740/PP/61569. [DOI] [PubMed] [Google Scholar]
- 75.Fu D, Qin Y. An analysis of Chinese and Western family culture from the perspective of comparative culture. J Taiyuan Normal Univ (Social Science Edition). 2017;2:29–31.
- 76.Deng W. On the cultural differences between China and the west from the comparison of family education between China and the United States. J Ansh Un Univers Ity. 2009;11:23–25. [Google Scholar]
- 77.Steinberg S. Childbearing research: a transcultural review. Soc Sci Med. 1996;43:1765–1784. doi: 10.1016/S0277-9536(96)00071-8. [DOI] [PubMed] [Google Scholar]
- 78.Leung SK, Arthur D, Martinson IM. Perceived stress and support of the Chinese postpartum ritual “doing the month”. Health Care Women Int. 2005;26:212–224. doi: 10.1080/07399330590917771. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be available from the corresponding author upon reasonable request.