A 16-year-old girl with a history of contact with another person with coronavirus disease-2019 (COVID-19) presented with cough, dyspnea, and anosmia. The severe acute respiratory syndrome coronavirus-2 real-time polymerase chain reaction test was positive. Upon physical examination, bilateral medium coarse rales were noticed. The laboratory workup revealed hemoglobin of 16 g/dL, white blood cell count of 5.1x109/L, platelet count of 158x109/L, and serum C-reactive protein level of 1.2 mg/L. B12 and folic acid tests were not performed because she was evaluated in the emergency department. Peripheral smear showed many giant platelets, vacuolated monocytes, and dysplastic neutrophils. We also observed similar dysplastic changes in other children with COVID-19 (Figure 1; May-Grunewald-Giemsa stain; 100x).
Figure 1.
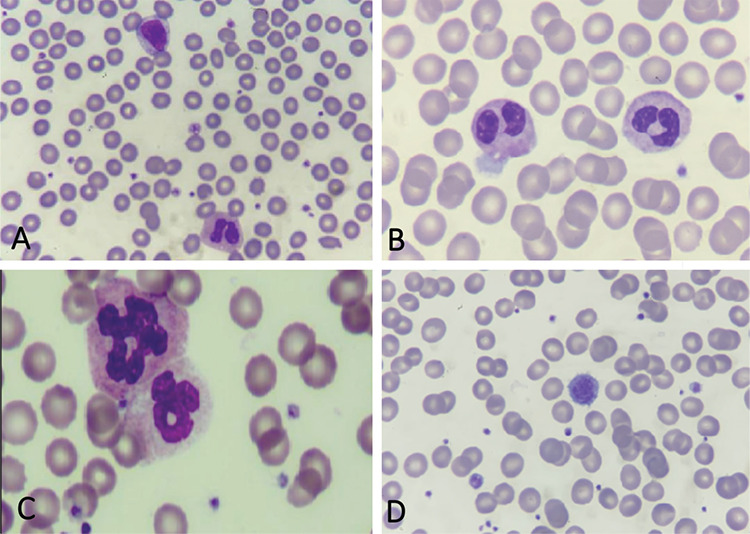
Dysplastic changes in peripheral blood (May-Grunewald-Giemsa stain; 100x). A) A reactive lymphocyte and pseudo-Pelger-Huet anomaly of the neutrophil. B) Pseudo-Pelger-Huet anomaly of neutrophils. C) Lobulation anomaly of the neutrophils. D) A giant platelet.
Dysplastic morphology of blood cells can be noted in both myelodysplastic syndrome and in many nonclonal diseases such as infections, autoimmune disorders, nutritional deficiencies, drugs, or cases of toxins [1]. Prominent morphological abnormalities of the neutrophils and platelets are reported in adult patients with COVID-19 [2,3]. In patients with COVID-19 infection, the upregulation of proinflammatory cytokines was reported [4]. Inhibitory effects of cytokines from virus-infected cells on hematopoiesis may also be responsible for myelodysplastic changes [1].
Footnotes
Ethics
Informed Consent: Obtained.
Authorship Contributions
Analysis or Interpretation: Y.M.A., D.G.G., N.Y.; Literature Search: Y.M.A., D.G.G., N.Y.; Writing: Y.M.A., D.G.G., N.Y.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Olcay L, Yetgin S. Disorders mimicking myelodysplastic syndrome and difficulties in its diagnosis. In: Fuchs O (ed) Myelodysplastic Syndromes. Rijeka, InTech. 2016. [Google Scholar]
- 2.Salib C, Teruya-Feldstein J. Hypersegmented granulocytes and COVID-19 infection. Blood. 2020;135:2196. doi: 10.1182/blood.2020006483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zini G, Bellesi S, Ramundo F, d’Onofrio G. Morphological anomalies of circulating blood cells in COVID‐19. Am J Hematol. 2020;95:870–872. doi: 10.1002/ajh.25824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Molloy EJ, Bearer CF. COVID-19 in children and altered inflammatory responses. Pediatr Res. 2020;88:340–341. doi: 10.1038/s41390-020-0881-y. [DOI] [PubMed] [Google Scholar]


