Abstract
Background:
Plain chest radiograph (CXR), although less sensitive than chest CT, is usually the first-line imaging modality used for patients with symptomatic SARS-CoV-2 infection. The relation between radiological changes in CXR and clinical severity of the disease in symptomatic patients with COVID 19 has not been fully studied and there is no scoring system for the severity of the lung involvement, using the plain CXR.
Aim of the study:
Current COVID-19 radiological literature is dominated by CT and a detailed description CXR appearances in relation to the disease time course is lacking. We propose an easy scoring system (CO X-RADS) to describe the severity of chest involvement in symptomatic COVID 19 patients using CXR and to correlate the radiological changes with the clinical severity of the disease.
Patients and methods:
The clinical manifestations and CXR findings were recorded in 500 symptomatic COVID-19 positive patients who were admitted to Hamad Medical Corporation (HMC) COVID-19 designated facility Center from January to June 2020. The severity and outcome of the disease included: intensive care unit admission, need for oxygen therapy, mechanical ventilation. and mortality rate.
Results:
Most of our symptomatic patients (86.8%) had mild and moderate clinical manifestations. The remaining 13.2% had severe manifestations, including: fever, persistent dry cough, shortness of breath, dyspnea, abdominal and generalized body pains. Based on our radiological scoring system (0 to 10) patients were distributed according to their CXR findings into different categories and according to our suggested (CO X-RADS) severity system into five categories (0 to IV). Patients with mild clinical manifestations showed low scoring in CXR (score 0 up to 4) and they represented 72% of our patients. Patients with moderately severe clinical manifestations showed mainly GGO (scoring 5 and 6) and represented about 14.8% of patients. Patients presented with severe clinical manifestations had obvious lung consolidations at the time of presentation with CXR scoring system ≥ 7 and represented about 13.2% of patients.
Conclusion:
We proposed a simple CXR reporting scoring system (CO X-RADS) to categorize COVID19 patients according to their radiological severity. This radiological score was correlated well with the clinical severity score of patients. We encourage other centers to test this scoring system in correlation with the clinical status of patients. (www.actabiomedica.it)
Keywords: COVID-19, SARS-CoV-2, chest radiograph, CT CO-RADS, CO X-RADS severity system
Introduction
COVID-19 (coronavirus disease 2019) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a strain of coronavirus. The first cases were seen in Wuhan, China, in December 2019 before spreading globally, with more than 12 million cases now confirmed. The current outbreak was officially recognized as a pandemic by the World Health Organization (WHO) on 11 March 2020. Definitive diagnosis of COVID-19 requires a positive reverse transcription– polymerase chain reaction (RT-PCR test). Many questions were raised on the potential relationship between various clinical and radiological parameters and the development and progression of COVID-19 (https://www.who.int/data/gho/whs-2020-visual-summary).
According to the Fleischner Society consensus statement, published on 7 April 2020: “ imaging is not indicated in patients with suspected COVID-19 and mild clinical features unless they are at risk for disease progression” (1). Imaging is indicated in a patient with COVID-19 and worsening respiratory status and for medical triage of patients with suspected COVID-19 who present with moderate to severe clinical features and a high pretest probability of disease (2).
Chest radiography, although less sensitive than chest CT, is usually the first-line imaging modality used for patients with suspected COVID-19 (3). The American College of Radiology notes that CT decontamination required after scanning COVID-19 patients may disrupt radiological service availability, and suggests that portable chest x-ray (CXR) may be considered to minimize the risk of cross-infection (4). Chest radiographs may be normal in asymptomatic patients and those with early/mild disease. It has been reported that in COVID-19 cases requiring hospitalization, 69% had an abnormal chest radiograph at the initial time of admission, and 80% had radiographic abnormalities during hospitalization (3). Radiological findings appear to be most extensive about 10-12 days after symptom onset (3).
Although most of the radiological findings presented in these patients are generic and can be seen in many systemic infectious processes such as pneumonia (viral or bacterial), inflammatory conditions (inflammatory lung diseases, vasculitis) and cardiac etiologies affecting lung parenchyma such as decompensated congestive heart failure, early recognition and high index of suspicion is of paramount importance (5).
The use of CT as a primary screening tool is discouraged because these studies tended to suffer from selection bias, with a pooled sensitivity of 94% and specificity 37% (6,7). Multiple radiological organizations and learned societies have stated that CT should not be relied upon as a diagnostic/screening tool for COVID-19 patients (8). Furthermore, performing CT routinely for large cohorts of patients carries additional risks. These include depletion of finite resources, increased risk of viral transmission (to staff, patients and carriers), and additional ionizing radiation exposures (6-8).
In March 2020, the “COVID-19 standardized reporting working group” of the Dutch Association for Radiology (NVvR) proposed a CT scoring system for COVID-19. They called it CO-RADS (COVID-19 Reporting and Data System) to ensure an uniform and replicable CT reporting This designates a score of CO-RADS from 1 to 5, based on the CT findings. In some cases, a score of 0 or 6 may need to be assigned as an alternative. If the CT is uninterpretable then it is CO-RADS 0, and if there is a confirmed positive RT-PCR test then it is CO-RADS 6 (6,9,10). In April 2020, American radiologists based at the University of Southern California proposed the COVID-19 imaging reporting and data system (COVID-RADS), which has a confusingly similar name to CO-RADS (11).
So far there is no scoring system using CXR that describes the severity of the lung involvement and its relation to the clinical severity in patients with SARS-CoV-2 infection.
Therefore, we proposed an easy scoring system (COX-RADS) to describe the severity of chest involvement in symptomatic COVID 19 patients using plain chest radiographs. In addition, we correlated the radiological changes with the clinical severity of the disease.
Patients and Methods
A retrospective study was conducted in several COVID-19 designated facilities Centers in Qatar [Al Hazm Mebaireek General Hospital (HMGH), Communicable Disease Center (CDC), Mesaieed Hospital (MGH), Ras Laffan Hospital (RLH), and the main health care provider of Hamad Medical Corporation (HMC)]. The study was approved by the Institutional Review Board in HMC [MRC-05-104].
Adult symptomatic patients with confirmed COVID-19 admitted to any of the designated facilities Centers, between January 2, 2020 and June 2, 2020 were studied. All patients were diagnosed based on the WHO recommendations for cases who had a positive PCR test for SARS-CoV-2 (11). WHO guidelines for clinical management were utilized to categorize COVID-19 patients accordingly (12).
We recorded the clinical presentations and radiological findings (CXR) of all affected patients. Recovery was defined as the resolution of clinical symptoms assessed by clinicians, such as no fever for more than three days, improved respiratory symptoms with reduced oxygen requirement, and no further need for hospital care. The severity and outcome of the disease included clinical manifestations (fever, cough, dyspnea), Intensive Care Unit (ICU) admission, need for oxygen therapy and/or mechanical ventilation and mortality.
Based on CXR changes we suggested a simple scoring system for evaluation of the severity of lung affection that can be used to triage patients accordingly. Each chest radiograph was analyzed for several items as showed in table 1. The scoring system and the degree of involvement (CO X-RADS) are summarized in tables 2 and 3.
Table 1.
Items studied in the chest X- ray analysis of patients with Covid 19. (From: https://doi.org/10.1038/s41598-020-66895)
Each chest radiograph was analyzed for the following items
|
Table 2.
The proposed scoring system (CO X-RADS) for the analysis of chest X-ray severity
| Score | Description |
| 0 | Normal lung vascularity and hilar shadows, clear lung fields, clear pleural reflections |
| 1 | Prominent central linear lung shadowing (mainly vascular shadowing) |
| 2 | 1+ accentuated hilar shadows + increased fine linear interstitial shadowing (thick interstitium) |
| 3 | 2+ fine soft tissue micronodular like (micro-beaded like appearance) possible perivascular/peribronchial micro-infiltrates and or end on prominent tiny vessels (more basal and peripheral). |
| 4 | 3+ Short relatively thick linear shadows mainly peripheral (septal lines i.e. Kerley’s lines) + or- fine honeycomb pattern, haziness of hilum, haziness of vascular markings or all. |
| 5 | 3+ one or few small ill-defined patches of diminished aeration (alveolar shadowing -GGO) mainly peripherally oriented and involving 1 or 2 lobes. |
| 6 | 3+multiple variable sized ill-defined patches of alveolar shadowing more peripheral involving more than 2 lobes. |
| 7 | 6+ one or few small patches of relatively denser consolidation involving 1 lobe. |
| 8 | 6+ few or multiple variable sized patches of consolidation (confluent or discreet) involving 2 lobes. |
| 9 | 6+ multiple variable sized areas of consolidations (confluent or discreet) involving more than 2 lobes |
| 10 | 8 or 9 + relatively thick peripheral linear shadowing (atelectatic/fibrotic band/s, + septal lines, Kerley’s B and or A &C lines) or 8 or 9 + pleural effusion, 8 or 9 + enlarged hilar shadows. |
Table 3.
Degree of radiological lung involvement according to our proposed scoring (CO X-RADS)
| CO X –RADS | Scoring | Degree of Chest X ray involvement |
| 0 | 0 | No chest involvement |
| I | 1,2,3 and 4 | Mild chest involvement |
| II | 5 and 6 | Moderate chest involvement |
| III | 7,8 and 9 | Sever chest involvement |
| IV | 10 | Severest form |
In the current proposed scoring system, patches of ill-defined alveolar shadowing which correspond to pulmonary ground glass opacities (GGO) in CT was considered positive when the degree of density of the pulmonary veiling (alveolar shadowing) was less than the adjacent ribs with no superimposition similar or less than the vascular shadowing with no superimposition. The consolidations were considered positive when the alveolar shadowing density was more than the adjacent rib with no superimposition with or without air bronchogram. Thick linear shadowing was considered positive when the thickness of the fibrotic strand was more than 3mm and was considered thin linear shadowing when its thickness is less than 3 mm.
Results
The clinical and radiographic data of 459 male patients and 41 female patients with mean age of 39 ± 11 years were recorded and analyzed.
Most of our patients (86.8%) had mild and moderate clinical manifestations. These included: mild headache, fever, dryness of mouth and throat or cough. Only 13.2% of patients had severe manifestations including severe dry cough, shortness of breath, dyspnea, abdominal and generalized body pains and diarrhea.
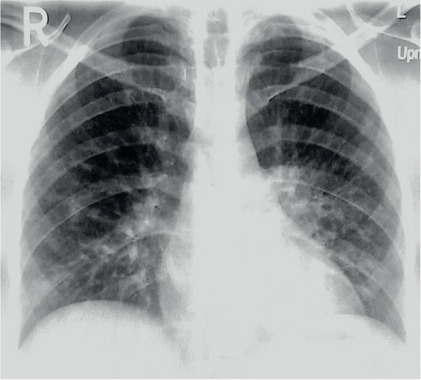
The CXR of patients with minimal symptoms were mainly clear (Figure 1). The most frequent finding of CXR in symptomatic patients were the prominent central linear lung shadowing, mainly vascular shadowing, and increased fine linear interstitial shadowing with secondary fine lace like appearance and prominent hilar shadows. These changes occurred in 94.2% of patients (Figures 2 and 3).
Figure 1.
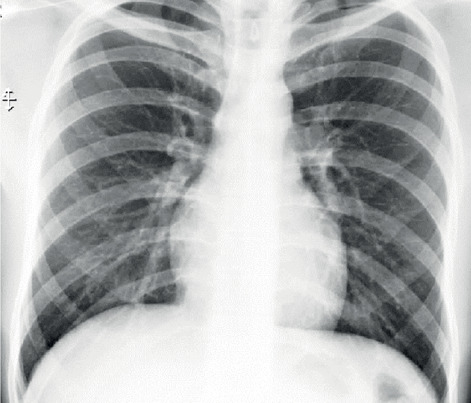
Plain X ray chest showing clear lungs (Pt. is covid 19 positive), appearance corresponding to score 0.
Figure 2.
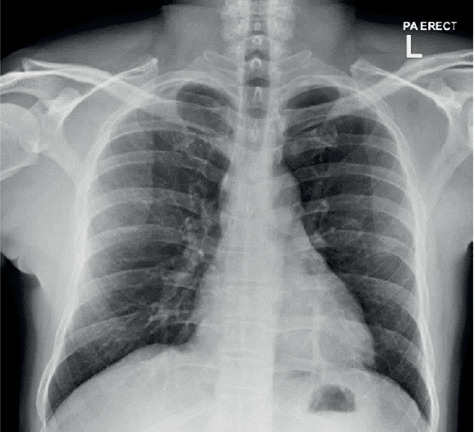
Plain X ray chest showing mild prominent central linear lung shadowing (mainly vascular shadows) corresponding to score 1.
Figure 3.
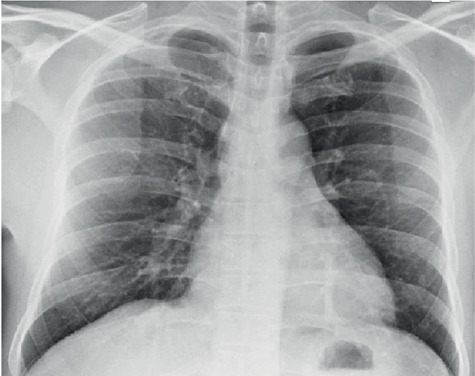
Plain X ray chest: Prominent central linear lung shadowing mainly vascular shadowing with increased fine linear interstitial shadowing (corresponding to score 2).
Fine beaded like appearance (likely formed by prominent end-on tiny pulmonary vascularity with possible perivascular thickening) occurred in 21.4% of patients (Figure 4) and was associated with thick septal lines, perivascular haziness, peribronchial cuff and hilar haziness in another 26.8% of patients (Figure 5).
Figure 4.
Plain X ray chest showing slightly thick fine interstitial shadowing with fine soft tissue micronodular like shadows (micro-beaded appearance) (arrows) more distributed basal and peripheral (corresponding to score 3).
Figure 5.
Plain X ray chest showing accentuated hilar shadows, increased fine linear lung shadowing, micro-beaded appearance, haziness of the fine vascular shadowing, fine honey comb like appearance and short relatively thick (still less than 3mm in thickness) linear shadows mainly peripheral (arrows), corresponding to score 4.
Variable sized patchy soft tissue infiltrates (ground glass opacities GGO), mainly peripherally oriented, occurred in 28% of patients. In 14.8% of them were not associated with consolidations. 8.2% patients showed one or more GGO involving one or two lobes (Figure 6). Multiple GGO involving more than 2 lobes occurred in 6.6% of patients (Figure 7). GGO associated with consolidations occurred in 13.2% of patients.
Figure 6.
Plain chest X-ray showing few small ill-defined patches of diminished aeration (alveolar shadowing-GGO) mainly peripherally oriented and involving 2 lobes (arrows) together with prominent hilar shadows and increased fine linear lung shadowing with haziness of fine arterial linear shadowing, corresponding to score 5.
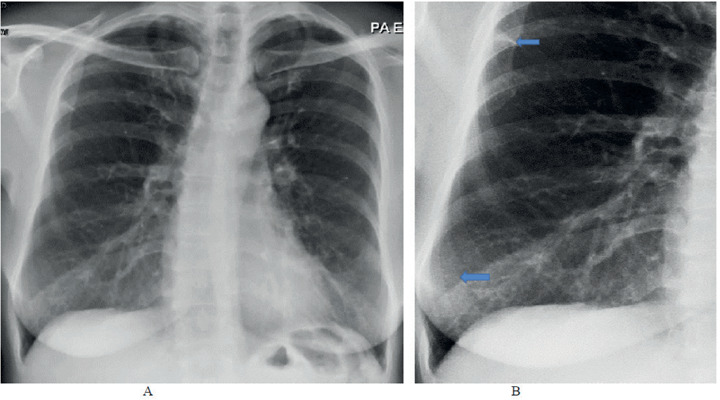
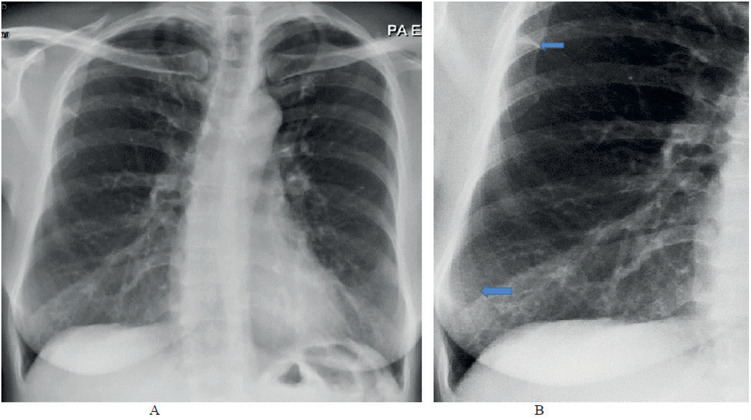
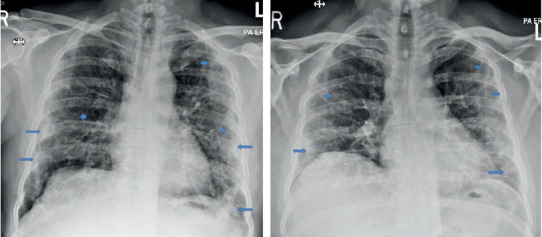
Figure 7.
Plain X ray chest PA view (A and B are two different patients) showing multiple variable sized discrete (fine arrow) and conglomerate (thick arrows) faint ground glass opacity (GGO) infiltrates involving both lungs (more than two lobes) mainly within the Rt lung and more peripherally oriented corresponding to score 6.
Few or multiple, small or conglomerate consolidations involving one lobe occurred in 5.4% of patients (Figure 8). An involvement of two or more lobes occurred in 3% (Figure 9) and 2.2%, respectively (Figure 10). Multiple consolidations with atelectatic bands occurred in 2.6% of patients (Figure 11). Associated pleural effusion (Figure 12) occurred in 1.5% and hilar enlargement (Figure 13) occurred only in 1% of patients.
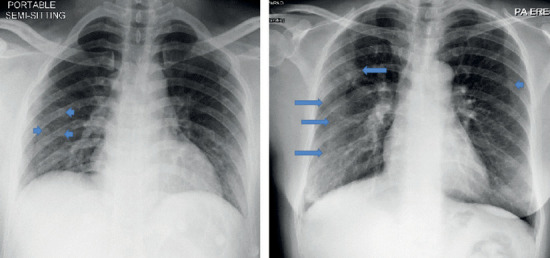
Figure 8.
Plain X ray: Chest PA view (A) and (B) magnified view for Rt lower lung zone Showing small patches of relatively denser consolidation within Rt middle lung zone (arrow) on top of the multiple small patchy ill-defined ground glass opacities (GGO) (short arrows) and increased linear lung shadowing with haziness of fine lung vascularity, corresponding to score 7.
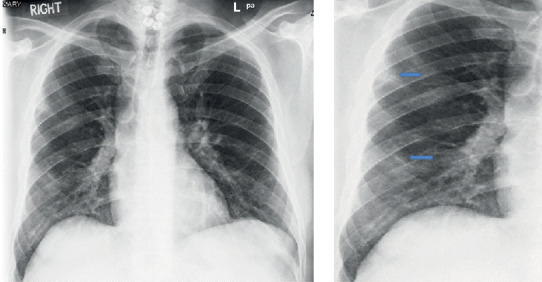
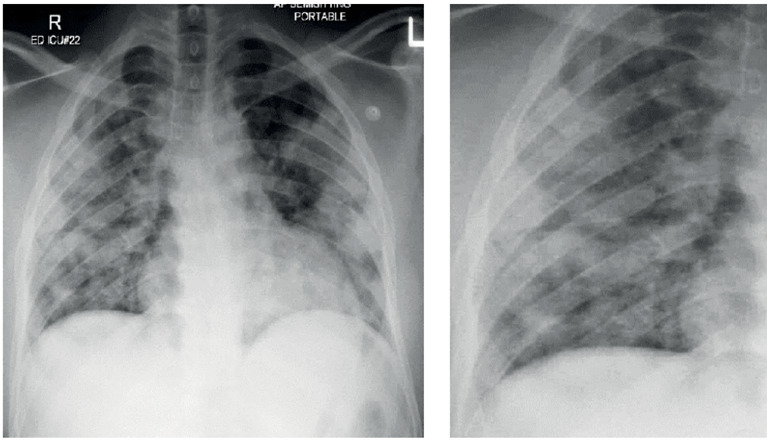
Figure 9.
Plain chest X-ray: Chest PA view (A) and (B) (two different patients) showing small patches of relatively denser consolidation within Rt and left lower and lung lobes more peripherally oriented (arrows) on top (merged with) of the multiple small patchy and conglomerate ill-defined ground glass opacities (GGO) which scattered in all lobes (short arrows) and increased linear lung shadowing with haziness of fine lung vascularity more basal and midzonal regions, corresponding to score 8.
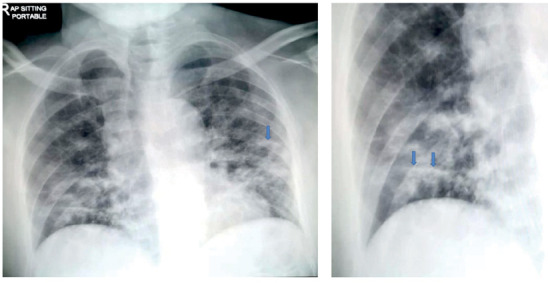
Figure 10.
Plain chest X-ray: PA view (A) and magnified view for Rt base (B) showed numerous areas of relatively dense consolidations involving both lungs nearly all lobes with relative sparing of Lt upper zone, corresponding to score 9.
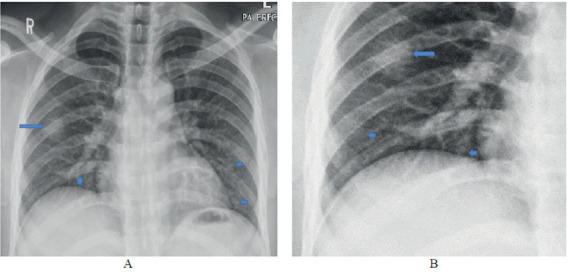
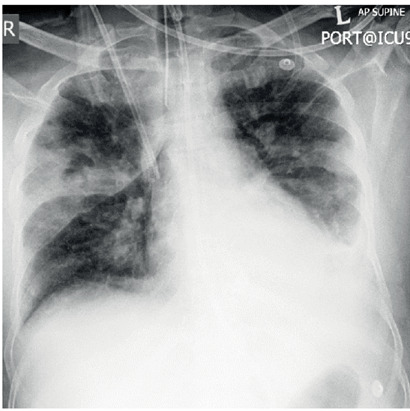
Figure 11.
Plain chest X-ray: PA view (A) and magnified view of the Rt long lung (B) showing multiple areas of denser consolidations on top of other patchy ground glass opacities (GGO) and thick atelectatic bands at Rt med to lower lung zone and left midzonal region (arrows), corresponding to score 10.
Figure 12.
Pleural effusion with lung changes (GGO, Consolidation and fibrotic strands) corresponding to score 10.
Figure 13.
Hilar enlargement with lung changes (ground glass opacities-CGO, Consolidation and thin fibrotic strands), corresponding to score 10.
Consolidation and associated pulmonary nodular shadows were identified in 3 patients (two of them were secondary to subsequent staphylococcal abscesses formation (Figure 14) and one with previous pulmonary nodule identified in older X-rays before COVID-19. Based on the radiological scoring system (0 to 10) and according to suggested CO X-RADS our patients are distributed as in Table 4 and 5.
Figure 14.
Plain chest X-ray: Large abscess cavities within both lungs secondary to staphylococcal abscesses formation (on top of ground glass opacities-GGO, consolidation and fibrotic strands), corresponding to score 10.
Table 4.
Distribution of patients according to our radiological severity score
| Score | No. of Pt. | % | Score | No of Pt. | % |
| 0 | 5 | 1% | 6 | 33 | 6.6% |
| 1 | 32 | 6.4% | 7 | 27 | 5.4% |
| 2 | 82 | 16.4% | 8 | 15 | 3.0% |
| 3 | 107 | 21.4% | 9 | 11 | 2.2% |
| 4 | 134 | 26.6% | 10 | 13 | 2.6% |
| 5 | 41 | 8.2% | 500 | 100% |
Table 5.
Distribution of our patients according to CO X-RADS
| CO X-RADS | No of Pt. | % |
| 0 | 5 | 1% |
| I | 355 | 71% |
| II | 74 | 14.8% |
| III | 53 | 10.6% |
| IV | 13 | 2.6% |
Clinical-radiological correlations
Patients with mild clinical manifestations showed low scoring in CXR (score 0 up to 4, CO X-RADS 0 and I) and they represented 72% of our patients. Patients with moderately severe clinical manifestations showed mainly GGO (scoring 5 and 6, CO X-RADS II) represented about 14.8% of patients. Patients presented with severe clinical manifestations had obvious lung consolidations at the time of presentation with CXR (scoring system ≥ 7, CO X-RADS III and IV) and represented about 13.2% of patients (Table 6).
Table 6.
The correlation between CO X-RADS score and clinical manifestations
| CO X-RADS | Clinical manifestation |
| 0 | Mild fever |
| I | Mild fever and cough |
| II | Fever, Cough and aches |
| III | Fever, cough, dyspnea requesting O2, tiredness |
| IV | Severe cough, dyspnea required assisted ventilation |
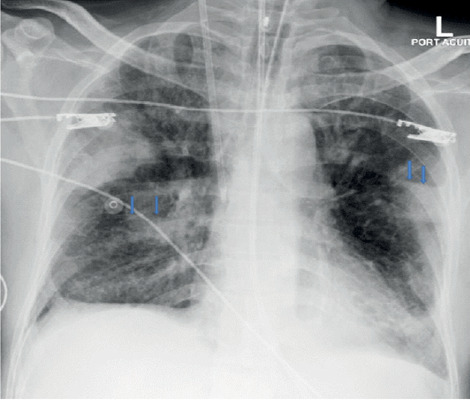
The clinical and radiological course of the disease
86 % of patients (n= 430) with mild and moderate symptoms improved clinically within 7-14 days and were not radiologically followed, 70 patients were radiologically followed because had a stationary or progression of symptoms. Table 7 shows the outcome of the patients in the course of radiologic follow- up (Figures 15 and 16).
Table 7.
The recorded changes of scoring CO X-RADS during the chest X-ray follow-up [Follow up was done only for the patients with deterioration or stationary clinical condition (N.70), 1 E= Deceased]
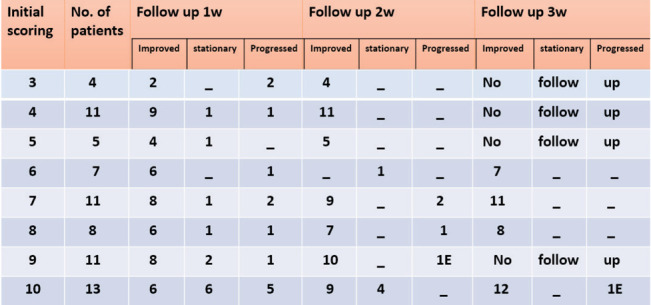 |
Figure 15.
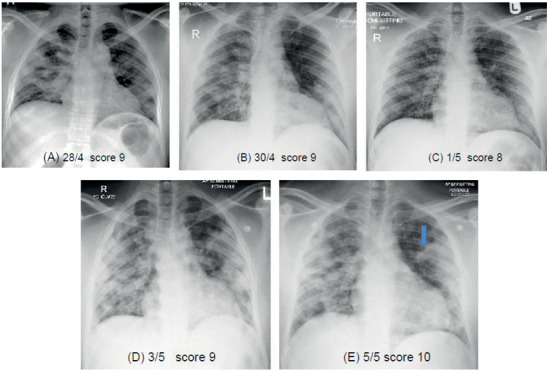
Serial chest radiographs for the same patient (follow up). A demonstrating initial scoring of the chest 9, the clinical condition of the patient showed no improvement and 2nd follow up radiograph (B) showed nearly no change of scoring still 9 but the degree of density of the consolidations are relatively less, clinically the patient improves and (C )is the 2nd follow up radiograph which showed change of scoring to 8, then the patient starts to deteriorate clinically and 3rd follow up radiograph (D) showed increased in number and density of consolidations and scoring is changed to 9, patient clinically deteriorate more and the 4rd follow up radiograph (E) showed starting of atelectatic bands (arrow) denoting scoring of 10.
Figure 16.
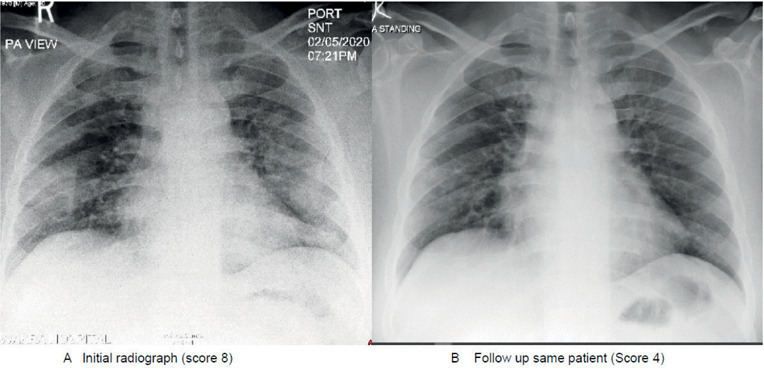
Plain chest X-ray: (A) initial radiograph of patient resented presenting severe clinical presentation with scoring 8 of the chest radiograph that did not improve (stationary) for 4 days then started to improve and (B) the follow-up radiograph, after one week before discharging, the patient showed considerable improvement with scoring changes to 4.
Discussion
Based on the analyses of the radiological and clinical data of our 500 patients with COVID19 we proposed a scoring and reading system for assessment of the severity of chest involvement (summarized in tables 2 and 3). In our patients this score proved to correlate generally with the clinical severity (symptoms and signs as well as requirement for oxygen and assisted ventilation).
Most of the chest X-ray findings in mild clinical cases showed mild lung changes, nonspecific for COVID-19. These included prominent hilar shadows, accentuated lung vascularity and fine linear parahilar and para cardiac lung reticulations. A specific finding in this mild group category was the micro-beaded like appearance, probably due to perivascular/peribronchial micro-infiltrates and/or end on prominent tiny lung vessels, mainly distributed in basal and peripheral lung zones.
The moderate chest involvement group was characterized by the identification of ground glass opacities (GGO) due to patchy alveolar shadowing/veiling. The distribution and extent of GGO increased according to the severity of lung involvement. In support with our findings, a previous report endorsed that the GGO pattern, identified by CT, was the most common finding in COVID-19. Zhou et al.(12) reported that GGO starts as unifocal lesion; most located in the inferior lobe, that later progressed to a multifocal, bilateral, and peripheral positions.
In our classification, the severe X-ray lung changes were identified by the presence of consolidation within the lungs which increased in density and distribution with expanding lung involvement and was coupled with more rigorous clinical manifestations. The severest form of lung involvement was indicated by the appearance of atelectatic bands that represented pulmonary infarctions secondary to pulmonary vascular thrombosis on top of consolidations. Super added pleural effusion, hilar enlargement and lung abscesses formation were very infrequent in our series and considered as severe complications.
Other investigators using CT imaging support our radiological findings in severe cases, reporting increased frequencies of GGO plus a reticular pattern, fibrotic streaks, air-bronchogram and pleural effusion as a manifestations of severe chest involvement (12-15).
The radiological manifestations of COVID-19 pneumonia are related to its pathophysiological basis. Since the diameter of SARS-CoV-2 is about 60–140 nm, and the size of the alveolar pores is about 10–15 μm, after inhaled through the respiratory tract, SARS-CoV-2 invades the bronchioles, mainly involving the interstitium around bronchioles at the end of lobular bronchioles, causing bronchiolitis and peri-bronchitis, and spreads to the distal end. Therefore, the lesion originates from a round-like nodule in the core of the secondary lung lobule, which were usually shown as round ground-glass opacity at first, and then extends to the whole secondary pulmonary lobules, forming lobular patchy imaging. SARS-CoV-2 mainly invades the interlobular interstitium, resulting in the appearance of prominent linear interstitial shadowing. Inflammatory stimulation leads to thickening of blood vessels in the lesion, which results in a corresponding alteration on imaging (16, 17). This pathophysiological sequences can explain our observation and scoring of severity as a part of the pathological progression of viral infection.
These scenarios of chest changes categorized according to radiological score fitted well with the clinical status of the patients at presentation and during the follow-up. Collectively, these data indicated that the proposed radiological score is a useful guide in the diagnosis and follow-up of symptomatic patients with COVID-19.
The CT CO-RADS classification did not discuss the severity of the chest involvement and only pointed to the possibility that the chest manifestations could be due to COVID-19 or not (16-19). Our CO X-RADS classification is mainly quantifying the degree of chest involvement in proved COVID-19 and appears to be useful in triaging patients at presentation and in monitoring them during hospital stay.
We encourage other centers to test this scoring system and its correlation with the clinical status of patients to confirm its diagnostic efficacy.
Declaration of interest
The authors report no conflicts of interest.
References
- 1.Rubin GD, Ryerson CJ, Haramati LB, et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology. 2020;296:172–180. doi: 10.1148/radiol.2020201365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raptis CA, Hammer MM, Short RG, et al. Chest CT and Coronavirus Disease (COVID-19): A Critical Review of the Literature to Date. AJR Am J Roentgenol. 2020;215:1–4. doi: 10.2214/AJR.20.23202. [DOI] [PubMed] [Google Scholar]
- 3.Wong HYF, Lam HYS, Fong AH, et al. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology. 2020;296:E72–E78. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection | American College of Radiology. https://www. acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection . Accessed March 22, 2020. [Google Scholar]
- 5.Rodrigues JCL, Hare SS, Edey A, et al. An update on COVID-19 for the radiologist - A British society of Thoracic Imaging statement. Clin Radiol. 2020;75:323–325. doi: 10.1016/j.crad.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ACR Recommendations for the Use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection.” American College of Radiology, 11 Mar. 2020 [Google Scholar]
- 7.Canadian Society of Thoracic Radiology and Canadian Association of Radiologists’ Statement on COVID -19 - CAR - Canadian Association of Radiologists”. CAR - Canadian Association of Radiologists, 2020 [Google Scholar]
- 8.Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296:E115–E117. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dutch Association for Radiology (Nederlandse Vereniging voor Radiologie, NVvR). https://www.radiologen.nl/secties/netwerk-covid-19/documenten/handreiking-standaardverslag-ct-thorax-covid-inclusief-co-rads . (in Dutch) [accessed 14 April 2020] [Google Scholar]
- 10.Prokop M, van Everdingen W, van Rees Vellinga T, et al. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19-Definition and Evaluation. Radiology. 2020;296:E97–E104. doi: 10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS) and common lexicon: a proposal based on the imaging data of 37 studies. Eur Radiol. 2020;30:4930–4942. doi: 10.1007/s00330-020-06863-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou S, Wang Y, Zhu T, Xia L. CT Features of Coronavirus Disease 2019 (COVID-19) Pneumonia in 62 Patients in Wuhan, China. AJR Am J Roentgenol. 2020;214:1287–1294. doi: 10.2214/AJR.20.22975. [DOI] [PubMed] [Google Scholar]
- 13.Liu X, Zhou H, Zhou Y, et al. Temporal radiographic changes in COVID-19 patients: relationship to disease severity and viral clearance. Sci Rep. 2020;10(1):10263. doi: 10.1038/s41598-020-66895-w. Published 2020 Jun 24 doi:10.1038/s41598-020-66895-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ooi GC, Khong PL, Müller NL, et al. Severe acute respiratory syndrome: temporal lung changes at thin-section CT in 30 patients. Radiology. 2004;230:836–844. doi: 10.1148/radiol.2303030853. [DOI] [PubMed] [Google Scholar]
- 15.Prokop M, van Everdingen W, van Rees Vellinga T, et al. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19-Definition and Evaluation. Radiology. 2020;296(2):e97–e104. doi: 10.1148/radiol.2020201473. doi:10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nicholls JM, Poon LL, Lee KC, et al. Lung pathology of fatal severe acute respiratory syndrome. Lancet. 2003;361(9371):1773–1778. doi: 10.1016/S0140-6736(03)13413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meng H, Xiong R, He R, et al. CT imaging and clinical course of asymptomatic cases with COVID-19 pneumonia at admission in Wuhan, China. J Infect. 2020;81:e33–e39. doi: 10.1016/j.jinf.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32–E40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296:E115–E117. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]


