Abstract
Background and aim of the work:
The incidence of long bone non-unions has been estimated to range between 5-10%. Nonunion of fracture is a delayed complication of fracture. A large bone resection, associated with Ilizarov’s osteo-distraction technique, is commonly used in these cases. The war experience was very important for dealing with these injuries. The purpose of this study is to report whether the use of Platelet Rich of Plasma(PRP) or Hyperbric Oxygen Therapy(HOT) as an adjuvant to the osteogenic distraction of Ilizarov with respect to the classical method has advantages.
Methods:
From 183 tibial non union, we enrolled 50 patients suffering by Type B according ASAMI non union classification. We divided the patients into two groups. The first group was a retrospective group of patient treated by Ilizarov Tecnique plus PRP. Instead the second group, patients were treated by Ilizarov Tecnique associated with HOT. The chosen criteria to evaluate the two groups during the clinical and radiological follow-up were: the complication after the surgery in the two groups; the duration of surgery; the objective quality Bone results and functional results were evaluated according to ASAMI classification while the subjective quality of life correlated with Ilizarov frame function by the Short Form 12 Health Survey (SF-12); The correlation between bone regenerate/bone healing and X-rays. The evaluation endpoint was set at 12 months from the remotion of Ilizarov’s frame for both groups.
Results:
In comparing the complications of the two populations, there were a significant statistically difference(p<0.05) in the local skin inflammation and Dockin Point Skin retraction for HOT group while in refracture p<0.05 was for group PRP. From the SF-12 we discovered not statistically differences p<0.05. The average correlation between Bone Regenerate-Bone Healing/ X-rays is absolutely in the PRP as in the HOT, p>0.05. The average Time for remove Ilizarov’s Frame in months was 15.37(±7.34; range 9–32) in PRP while in HOT was15.22(± 7.83; range 9–31), p>0.05.
Conclusions:
From our study we can conclude that the association of HOT and PRP with the Ilizarov technique does not improve the functional outcomes but allows a more rapid healing of the regenerated bone and therefore an early removal of the device and a corresponding improvement in the quality of life. (www.actabiomedica.it)
Keywords: Tibial Nonunion, Ilizarov, Paltlet Rich Plasma, Hyperbaric Oxigen Therapy, Outcomes, ASAMI, Limb Reconstruction, Limb Savage
Introduction
The epidemiology of fractures of the tibial shaft has been addressed in a number of studies (1–8). The incidence of tibial shaft fractures is reported in the literature with variation over years and between different countries and cultures (1). From our trauma database, in South Italy, Tibial fracture is one of the most common in the long bone of the body and high-energy collisions, such as road traffic accidents or motorcycle crashes and gunshot injuries, are common causes of tibial shaft fractures. Non-union or delayed union is a common complication of tibial fracture and indicates that the fracture did not heal in a timely fashion(2,3). Nonunion rates in tibial shaft nonunion were >10%, Tibia (14%), than others long bones(4). Univariate analysis assumes that the response variable is influenced only by one other factor, while multivariate analysis assumes that the response variable is influenced by multiple factors or combinations of these factors(5). There are local or general factor because a fracture don’t not heal(3). Non-unions are difficult to treat and have a high financial impact(3). Indirect costs, such as productivity losses, are the key driver for the overall costs in fracture and non-union patients(3). The Ilizarov method is the one most commonly used for the treatment of aseptic nonunion(3). According to the diamond concept(6), the use of biological stimulants such as platelet-rich plasma (PRP) (7) and hyperbaric oxygen therapy(HOT)(8) can be diaphanous for rapid healing. The purpose of the study is to compare the use of PRP with HOT combined with the Ilizarov Method in treating aseptic tibial shaft nonunions.
Materials and Methods
From January 2006 to December 2017, at the six Trauma Level I Center: Vito Fazzi Hospital, Lecce, Italy; Italy; Department of Orthopaedics and Traumatology, University Hospital “Gaetano Martino” Messina, Italy, AO G Rummo, Benevento, Italy; Santa Maria della Misericordia, Perugia, Italy; Clinic of Traumatology, University Hospital Clinical Center Banja Luka, Bosnia and Herzegovina; University of Valencia, “La Ribera” Hospital, Valencia, Spain Division of Orthopedics and Trauma Surgery; we treated 183 tibial non union. From 183 tibial non union, we enrolled 50 patients suffering by Type B according ASAMI non union classification (9).
Exclusion criteria included: hematological or oncological patients; Acute or Chronicle infections; ASAMI non union classification’s type A and C; not Ilizarov technique; not use of PRP or HOT; other treatments to treat aseptic nonunions; patients who did not adhere to a minimum follow-up of 12 months after the remotion of Ilizarov Frame.
We divided the patients into two groups. The first group was a retrospective group of patient treated by Ilizarov Tecnique plus PRP(PRP). Instead the second group, patients were treated by Ilizarov Tecnique associated with HOT(HOT). Patient division was done through the free choice of patients to adhere to one of the relative and absolute contraindications and treatments for hyperbaric therapy.
The population of the PRP group at the time of the nonunion had a mean age of 42.86 (±6.23;range 16-72), the relation between the sexes (M:F) was 2.57 (18:7). All patients had a closed tibial shaft fracture. The Type of closed Fracture according AO’s classification(1) were: A1 in 1(4%) patient; A2 in 1(4%) patient; A3 in 3(12%) patients; B1in 2(8%) patients; B2 in 6(24%) patients; B3 in 4(16%) patients; C1 in 2(8%) patients; C2 in 3(12%) patients; C3 in 3(12%) patients. The orthopedic trauma devices for the treatment of fractures were: Axial External Fixation in 8(32%) patients; Circular external Fixation in 3(12%) patients; Intramedullary nail in 10(40%) patients; Plate in 4(16%) patients.
The mean in months of nonunion after the trauma was 7.23(±1.58; range 4-8). The Type of nonunions according ASAMI’s classification were: B1 in 9(36%) patients; B2 in 7(28%)patients; B3 in 9(36%) patients.
To understand and study the capacity of bone healing in patients, we used the Non-Union Scoring System (NUSS) in retrospective mode (3). The average point of the NUSS in Norm was 48.23(±7.45; range 36-72).
The population of the HOT group at the time of the nonunion had a mean age of 42.79 (±6.33;range 16-71), the relation between the sexes (m: f) was 2.12 (17:8). All patients had a closed tibial shaft fracture. The Type of closed Fracture according AO’s classification(1) were: A1 in 1(4%) patient; A2 in 1(4%) patient; A3 in 3(12%) patients; B1in 2(8%) patients; B2 in 5(20%) patients; B3 in 5(20%) patients; C1 in 2(8%) patients; C2 in 3(12%) patients; C3 in 3(12%) patients. The orthopedic trauma devices for the treatment of fractures were: Axial External Fixation in 7(28%) patients; Circular external Fixation in 4(16%) patients; Intramedullary nail in 9(36%) patients; Plate in 5(20%) patients.
The mean in months of nonunion after the trauma was 7.21(±1.49; range 4-8). The Type of nonunions according ASAMI’s classification were: B1 in 9(36%) patients; B2 in 8(32%) patients; B3 in 8(32%) patients.
To understand and study the capacity of bone healing in patients, we used the Non-Union Scoring System (NUSS) in retrospective mode (3). The average point of the NUSS in Norm was 48.62(±7.39; range 35-74).
All patients were informed in a clear and comprehensive way of the two types of treatment and other possible surgical and conservative alternatives. Patients were treated according to the ethical standards of the Helsinki Declaration and were invited to read, understand and sign the informed consent form.
All patients of the two groups. They have undergone the same pre operative and post operative protocol according their treatment (see Patient case management).
The chosen criteria to evaluate the two groups during the clinical and radiological follow-up were: the complication after the surgery in the two groups; the duration of surgery; the objective quality Bone results and functional results were evaluated according to Association for the Study and Application of the Method of Ilizarov (ASAMI) classification(10) while the subjective quality of life correlated with Ilizarov frame function by the Short Form 12 Health Survey (SF-12)(11); The correlation between bone regenerate/bone healing and X-rays.
The evaluation endpoint was set at 12 months from the remotion of Ilizarov’s frame for both groups.
Statistical analysis
Descriptive statistics were used to summarize the characteristics of the study group and subgroups, including means and standard deviations of all continuous variables. The t test was used to compare continuous outcomes. The Fisher, in this groups are smaller than 10 patients, exact test were used to compare Categorical variables. The statistical significance was defined as p<0.05. We used Pearson correlation coefficient (r) was used to compare the predictive score of outcomes and quality of life. Statistical analyses were performed with SPSS v.15.0 (SPSS Inc., an IBM Company, Chicago, IL, USA). Mean ages (and their standard deviations) of the patients were rounded at the closest year. The predictive score of outcomes and quality of life and their standard deviations were approximated at the first decimal while at the second decimal was approximated Pearson correlation coefficient (r). The reliability and validity of the correlation between bone regenerate/bone healing and X-rays were determined by the Cohen’s kappa(k).
Patient Managements
Preoperative Evaluation and Planning
All patients were assessed in a multidisciplinary clinic, comprising orthopaedic and plastic surgeons, radiologist, anesthesiologist, hematologic phycisins, and a specialist Ilizarov nurse practitioner. A preoperative plan was performed by drawing on paper or on radiographic plate.
Surgical Management and Microbiologic Sampling
Surgical excision and tissue sampling were performed according to a previously described protocol(Figure 1, Figure 2). The medullary canal were reamed. The excision was complete when only healthy bleeding bone remained. After debridement, an assessment of the stability of the nonunion was made. The nonunion was regarded as “stiff” if it had angular bending of less than 7 degrees and axial movement of less than 5 mm on manual testing.
Figure 1.
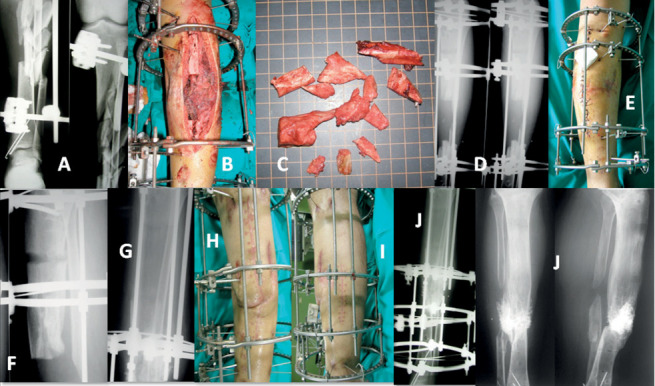
The X-rays of a 52-year-old man 42C3 according AO of closed tibial shaft fracture, treated with axial external fixator at 4 months from trauma(A; B). Bone tumor resection(C) and Ilizarov’s frame(D and E) implantation. X-ray showed the start of bone transport(F) and proximal bone regenerated after 6 months of Ilizarov Treatment(G). Skin Complication at the docking point site(H), and its resolution(I). X-ray showed the Docking point state before the platelet rich plasma’s injection. Bone healing at the removal of the Iizarov’s Frame, X-rays showed the hypercalculation(bone metallization effect) of docking point site due to PRP
Figure 2.
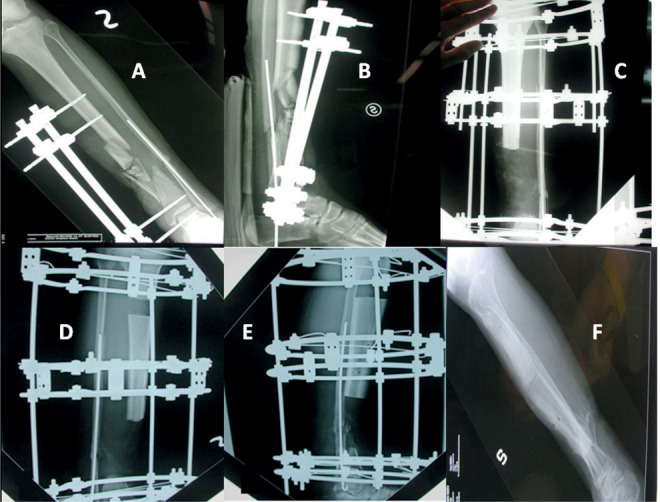
The X-rays of a 34-year-old woman with a closed tibial shaft fracture 42C3 according AO, treated with an axialexternal fixator and K-wire in the fibula, 7-month after the trauma(A;B). Tumor-type resection and Ilizarov frame(C) implant. X-ray showed the start of bone transport(D, E) and after hyperbaric oxygen therapy protocol. X-ray showed excellent results post removal Ilizarov’s frame(F).
Stabilization and Realignment
Monofocal distraction: performed in cases with stiff nonunions with no major bone loss. A 4-ring frame was used, and a distal fibular osteotomy was made. Hinges were used to gradually correct angular deformity if present. Distraction was commenced at 1 mm per day for 2 weeks, or until deformity was corrected.
Postoperative Care
Vancomycin and meropenem were given intraoperatively, Samples and cultures were did on bone resection used to detect possible infections, all of which were negative. Knee and Ankle Joints mobilization were started on day 2 and early full-weight-bearing encouraged. Radiographs were reviewed every 2 weeks during the distraction period and monthly during the consolidation period. The Ilizarov external fixator was removed when radiographs showed solid docking-site union and the regenerate area had a minimum of three complete cortices.
Platelet Rich Plasma Injection Protocol
For each patient in the PRP Group, 60 ml of whole blood was drawn from an antecubital vein. The 30-ml syringe was primed with 8 ml of anticoagulant citrate dextrose solution(ACD-A) before 52 ml of whole blood was obtained from each patient using standard phlebotomy procedures. On reaching the final volume of 60 ml, the syringe was loaded into centrifuge. The centrifuge was programmed to produce 6 ml of PRP from the 60 ml volume. The local injection of PRP was done on the docking site at first day of docking point compression.
Hyperbaric Oxygen Therapy Protocol
For patients in the HOT treatment group, the aim was for them to receive a total of 20 HOT sessions over approximately 20 days in 4 weeks. HOT treatment was provided using pressure/time schedules selected in hyperbaric oxygenation for 2 hours daily, beginning on the first day of docking point compression, aimed at delivering a dose approximately bioequivalent to 90 min of oxygen breathing at 2.5 atmospheres absolute pressure.
Results
Null hypothesis between the two populations was rejected.
The mean Follow up in years were in PRP 2.1(±0.62; range 1-5) as in HOT 1.62.2(±0.58; range 1-5), p>0.05.
The average duration of surgical time in the PRP group was 126.1 (±33.2; range 89-169) minutes; in the HOT group was 126.6(±28.7; range 87-172) with a p> 0.05.
The average bone resection in cm in the PRP group was 6.3(±1.75; range 3.6-10.9)as in the HOT group was 6.5(±1.72; range 3.8-11.2)with a p> 0.05.
The average Time of bone transport took in days was 92.7(±9.27; range 69-92) in the PRP while in HOT was 92.4(±9.31; range 67-90), p>0.05.
The average External Fixation Index in months/cms was 0.88(±0.47; range 0.52–1.88) in the PRP while in HOT was 0.86(±0.53; range 0.48–1.86), p>0.05.
At the end of the treatment the complication in PRP were: Blood Loss was average 937±164.38 mls; Intra Operative Fracture in 0 patient; Loosening of wires or pins in 4(16%) patients; Local Skin inflammation in 8(32%) patients; Docking point skin retraction in 7(28%)patients; Retard to consolidation of bone regenerate in 2(8%) patients; Refracture in 0. while in the group HOT: Blood Loss was average 942±157.46 mls; Intra Operative Fracture in 0 patient; Loosening of wires or pins in 3(12%) patients; Local Skin inflammation in 4(16%) patients; Docking point skin retraction in 3(12%) patients; Retard to consolidation of bone regenerate in 2(8%) patients; Refractures in 2(8%) fractures.
In comparing the complications of the two populations, there were a significant statistically difference(p<0.05) in the local skin inflammation and Dockin Point Skin retraction for HOT group while in refracture p<0.05 was for group PRP.
The average correlation between Bone Regenerate-Bone Healing/ X-rays is absolutely in the PRP k=0.812204±0.099677 (Figure 1) as in the HOT 0.812208±0.065343, p>0.05 (Figure 3).
Figure 3.
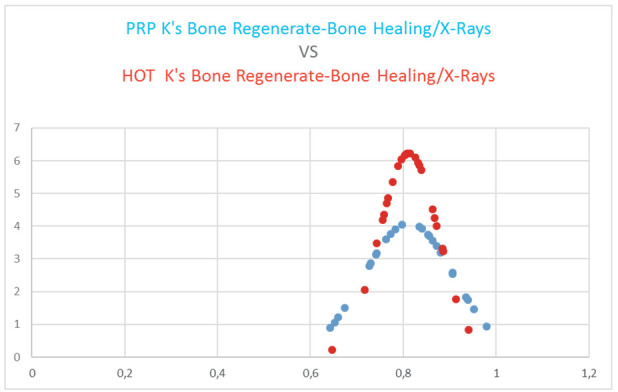
Comparison between the two Gaussian distributions. At the endpoint there was not statistically differences between the two groups, p>0.05.
The average Time for remove Ilizarov’s Frame in months was 15.37(±7.34; range 9–32) in PRP while in HOT was15.22(± 7.83; range 9–31), p>0.05.
In comparing the outcomes of the two populations, there were not a significant statistically difference(p>0.05).
According the ASAMI outcomes classification we had some different results in both two groups were: in PRP excellent results were in 9(36%) patients while in HOT 10(40%), p>0.05; patients in PRP good results were in 9(36%) patients while in HOT 8(32%)patients, p>0.05; fair results were 7(28%) in both groups, p=1; poor results in both groups in 0 patients, p=1.
The subjective quality of PRP’ life before the tibial shaft fracture, measured by SF-12, was about 92.3 points (range 82-100) while the quite quality of life before the tibial shaft fracture, measured by SF-12, was about 92.4 points (range 84-100) in HOT, p>0.05 (Figure 4). After Discovery of Non union the SF-12 score was in 68.3 (range 26-82) points in PRP and 67.7 (range 28-78) in HOT, (p>0.05). After 1 month of applied Ilizarov’s Frame the SF-12 score in PRP was 39.7 (range 24-68) points while in HOT was 39.6, p>0.05 (Figure 4). At the moment of total weigh bearing the SF-12 score in PRP was 66.3 (range 40-84) while 66.4(range 40-84) in HOT, p>0.05 (Figure 4). When started each protocol group the SF-12 score was in 67.2 (range 28-74) points in PRP and 67.5 (range 28-72) in HOT, p>0.05 (Figure 4). When ended each protocol group the SF-12 score was in 70.5 (range 52-90) while 70(50-92) in HOT, p>0.05 (Figure 4).
Figure 4.
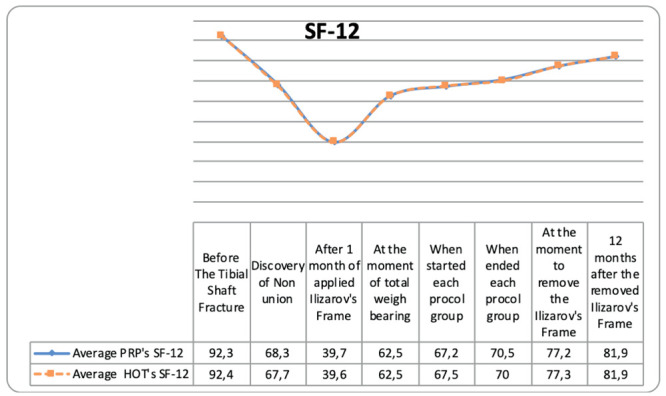
Trend of Subjective quality of life misured by Short Form 12 Health Survey (SF-12) from the healthy life to all surgical treatments. At the moment to remove the Ilizarov’s Frame and 12 months after the removed Ilizarov’s Frame, there was not a statistically differences(p>0.05).
At the moment to remove the Ilizarov’s Frame the SF-12 was 77.2(range 66-92) point in PRP while in HOT was 77.3(range 66-94), p>0.05 (Figure 4).
At 12 months after the removed Ilizarov’s Frame we had SF-12 score in PRP of 81.9(range 64-92) as in HOT was 8.9 (range 64-92) points, p>0.05 (Figure 4).
From the SF-12 it is shown that the pain, the stiffness of the knee and /or the ankle have affected the patients quality life.
The SF-12 psychological scores show that women in the patients of both groups were the most affluent people. At the end of the therapeutic protocol for each group, we did not show any placebo effect or increase in anxiety and depression states for any re-interventions to free the docking site or prescription for antibiotic therapy for inflammation of the skin.
From a functional point of view, women complained about the size of the Iizarov Frame in both groups while in the Hot Group they underwent five times a week for 4 weeks for 2 hours per day at hyperbaric therapy.
The men complained that they did not immediately have an effective benefit that could make them work for the work, sports and hobbies that they did before the trauma.
Discussion
Fracture healing is a dynamic process governed by cellular and biochemical agents. Despite the investigation of many factors that may affect this process and the achieved progress on this issue, there are still problems in fracture healing(13). The basic principles of atrophic nonunion treatment involve resection of nonviable bone, autogenous grafting, and skeletal stabilization(3,14-16). However, extensive surgical approaches further endanger an already impaired blood flow at the nonunion site(3,14-16). The biomechanical properties inherent to circular external fixation and the techniques of compression-distraction and internal bone transport are important innovations that will help surgeons meet the challenges of this difficult problem(3-16). Cellular evidence of the potential applications of HOT therapy in fracture healing has previously been investigated. Wu et al. suggested that HOT enhances the differentiation of osteoblasts towards the osteogenic phenotype in vitro(17). Milovanova et al.(18) showed that HOT stimulated vasculogenic stem cell growth and differentiation in vivo. According two systematic reviews(19,20) failed to locate any relevant clinical evidence to support or refute the effectiveness of HOT for the management of delayed union or established non-union of bony fractures. Good quality clinical trials are needed to define the role, if any, of HOT in the treatment of atrorphic non union. There are three randomised controlled trials provide some relevant clinical evidence to address this issue(21-23). Fracture union is promoted by the removal of non-viable bone through subperiosteal corticotomy and intermittent compression-distraction in most cases(3,14-16). However, this technique remains controversial due to the disadvantages of prolonged framing time, the need for good patient tolerance, the fact that frame application is a technically demanding procedure, and the need for close followup and frequent frame adjustment(11,12,14-16). Therefore, adjunctive HOT therapy can enhance fracture healing in an atrophic tibial nonunions in patients and can therefore be used as supplementary therapy. From the Tenth European Consensus Conference on Hyperbaric Medicine, the HOT is Strongly recommending treatment for traumatic bone ischaemias as the aseptic non union(24).
Two papers have reported that PRP can enhance the healing process in bone injuries(25,26). The bone regenerative effects of PRP have also been reported at early phases of distraction osteogenesis (27,28). Some research has indicated that the addition of MSC into a PRP scaffold would be beneficial for increased new bone formation, mineralization, and mechanical property (29,30).
Dehghan et al. (30) in their canine animal study reported a 30% lengthening of the left tibia (mean distraction distance: 60.8 mm) was performed in ten adult male dogs by callus distraction after osteotomy and application of an Ilizarov fixator. Autologous bone marrow mesenchymal stem cells (BM-MSCs) and PRP as the treatment group (n=5) or PRP alone (control group, n=5) were injected into the distracted callus at the middle and end of the distraction period. At the end of the consolidation period, the dogs were sacrificed after which computerized tomography (CT) and histomorphometric evaluations were performed; From the radiographic evaluationsrevealed that the amount and quality of callus formations were significantly higher in the treatment group (P<0.05). As measured by CT scan, the healing parametersin dogs of the treatment group were significantly greater (P<0.05). New bone formation in the treatment group was significantly higher (P<0.05). Their conclusione the transplantation of BM-MSCs and PRP positively affects early bony consolidation in osteogenic distraction and their use might allow a shortened period of consolidation and therefore permit earlier device removal. The use of platelet-rich plasma (PRP) can augment the healing process of soft tissues following surgical interventions(31). Rodriguez-Collazo and Urso(31) used of DBM saturated with cBMA PRP and in combination with the Ilizarov technique to treat distal tibial fracture in patients with non union’s high rates. Their results in an 85 % healing rate in approximately 4 months (31). Their conclude this strategy is safe, reliable, and effective with good clinical outcomes for the treatment for complex fractures in patients with significant comorbidities and nonunion rates(31).
If we compare to the meta-analysis and literature reviews of ordinary Ilizarov’s treatment with our results for outcomes, prognosis, complications, they do not differ but our data are better in the early removal of the device.
From our study we can conclude that the association of HOT and PRP with the Ilizarov technique does not improve the functional outcomes but allows a more rapid healing of the regenerated bone and therefore an early removal of the device and a corresponding improvement in the quality of life.
Limitations In Investigational Methodology
The limits of the current study was the limited number of patients, non-probability sample of convenience, due to few centric sample, Level 1 Trauma Center.
Another limit’s it’s is retrospective study.
Disadvantages of retrospective studies: inferior level of evidence compared with prospective studies; subject to confounding (other risk factors may be present that were not measured) ;cannot determine causation, only association; some key statisitics cannot be measured.
Selection of patients may be biased, making generalization of results difficult. It may be unclear whether the confluence of findings is merely a chance occurrence or is truly characteristic of a new disease or syndrome.Another limitation was that the measurements and intervention were made without randomization of the researcher to the experimental groups, which have potential for bias. Finally other limiting factors of the study acknowledged by the authors can be: the potential for regression to the mean, the presence of temporal confounders and the mention of subjective score.
Human and animal right
For this type of study is not required any statement relating to studies on humans and animals. All patients gave the informed consent prior being included into the study. All procedures involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
Conflict of Interest
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Larsen P, Elsoe R, Hansen SH, Graven-Nielsen T, Laessoe U, Rasmussen S. Incidence and epidemiology of tibial shaft fractures. Injury. 2015;46(4):746–50. doi: 10.1016/j.injury.2014.12.027. doi: 10.1016/j.injury.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 2.Al Shahrani AA, Tedla JS, Ahmad I. Effectiveness of Ilizarov frame fixation on functional outcome in aseptic tibial non-union cases at Abha, Kingdom of Saudi Arabia: An experimental study. Journal of Taibah University Medical Sciences. 2015;10(2):216–221. Doi: https://doi.org/10.1016/j.jtumed.2014.09.002. [Google Scholar]
- 3.Calori GM, Colombo M, Mazza EL, Mazzola S, Malagoli E, Marelli N, Corradi A. Validation of the Non-Union Scoring System in 300 long bone non-unions. Injury. 2014;45(Suppl 6):S93–7. doi: 10.1016/j.injury.2014.10.030. doi: 10.1016/j.injury.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 4.Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, Della Rocca GJ, Mehta S, McKinley T, Wang Z, Steen RG. Epidemiology of Fracture Nonunion in 18 Human Bones. JAMA Surg. 2016;151(11):e162775. doi: 10.1001/jamasurg.2016.2775. doi: 10.1001/jamasurg.2016.2775. [DOI] [PubMed] [Google Scholar]
- 5.Hak DJ. Editorial on “Epidemiology of fracture nonunion in 18 human bones”. Ann Transl Med. 2017;5(Suppl 1):S19. doi: 10.21037/atm.2017.03.86. doi: 10.21037/atm.2017.03.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: the role of the biological chamber. Injury. 2011;42(11):1191–3. doi: 10.1016/j.injury.2011.04.016. doi: 10.1016/j.injury.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez-Collazo ER, Urso ML. Combined use of the Ilizarov method, concentrated bone marrow aspirate (cBMA), and platelet-rich plasma (PRP) to expedite healing of bimalleolar fractures. Strategies Trauma Limb Reconstr. 2015;10(3):161–6. doi: 10.1007/s11751-015-0239-x. doi: 10.1007/s11751-015-0239-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martel’ II, Dolganova TI, Nikolaĭchuk, Sazonova NV, Dolganov DV. Hyperbaric oxygenation in the treatment regimen using Ilizarov technique in patients with open fractures. Vestn Khir Im I I Grek. 2003;162(6):35–9. [PubMed] [Google Scholar]
- 9.Yin P, Zhang L, Li T, Zhang L, Wang G, Li J, Liu, Zhou J, Zhang Q, Tang P. Infected nonunion of tibia and femur treated by bone transport. J Orthop Surg Res. 2015;10:49. doi: 10.1186/s13018-015-0189-5. doi: 10.1186/s13018-015-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kindwall E, Whelan H. Hyperbaric Medicine Practice. In: Flagstaff AZ, editor. 2nd ed. Best Publishing Company; 2004. chap 1, 18, 19, 20, 25, 29, 30. [Google Scholar]
- 11.Yin P, Zhang Q, Mao Z, Li T, Zhang L, Tang P. The treatment of infected tibial nonunion by bone transport using the Ilizarov external fixator and a systematic review of infected tibial nonunion treated by Ilizarov methods. Acta Orthop Belg. 2014;80(3):426–35. [PubMed] [Google Scholar]
- 12.Iliopoulos E, Morrissey N, Cho S, Khaleel A. Outcomes of the Ilizarov frame use in elderly patients. J Orthop Sci. 2017;22(4):783–786. doi: 10.1016/j.jos.2017.03.002. doi: 10.1016/j.jos.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Demirtaş A, Azboy I, Bulut M, Uçar BY, Alemdar C, Alabalık U, Akpolat V, Yıldız I, Ilgezdi S. The effect of hyperbaric oxygen therapy on fracture healing in nicotinized rats. Ulus Travma Acil Cerrahi Derg. 2014;20(3):161–6. doi: 10.5505/tjtes.2014.52323. doi: 10.5505/tjtes.2014.52323. [DOI] [PubMed] [Google Scholar]
- 14.Grubor P, Grubor M, Meccariello L. Use of external fixation and bone graft vs ao plates and bone graft in fractures of tibial shaft during the war in bosnia. Med&CH Orto. 2013;4:60–68. [Google Scholar]
- 15.Grubor P, Falzarano G, Grubor M, Piscopo A, Franzese R, Meccariello L. Treatment of the chronic war tibial osteomyelitis, Gustilo type IIIB and Cierny-Mader IIIB, using various methods. A Retrospective study. EMBJ. 2014;9(2):7–18. Doi: 10.3269/1970.5492.2014.9.2. [Google Scholar]
- 16.Grubor P, Milicevic S, Grubor M, Meccariello L. Treatment of Bone Defects in War Wounds: Retrospective Study. Med Arh. 2015;69(4):260–264. doi: 10.5455/medarh.2015.69.260-264. doi: 10.5455/medarh.2015.69.260–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu D, Malda J, Crawford R, Xiao Y. Effects of hyperbaric oxygen on proliferation and differentiation of osteoblasts from human alveolar bone. Connect Tissue Res. 2007;48:206–13. doi: 10.1080/03008200701458749. DOI: 10.1080/03008200701458749. [DOI] [PubMed] [Google Scholar]
- 18.Milovanova TN, Bhopale VM, Sorokina EM, Moore JS, Hunt TK, Hauer-Jensen M, Velazquez OC, Thom SR. Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo. J Appl Physiol. 2009;106:711–28. doi: 10.1152/japplphysiol.91054.2008. DOI:10.1152/japplphysiol.91054.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bennett MH, Stanford RE, Turner R. WITHDRAWN: Hyperbaric oxygen therapy for promoting fracture healing and treating fracture non-union. Cochrane Database Syst Rev. 2012;14(3):CD004712. doi: 10.1002/14651858.CD004712.pub3. doi: 10.1002/14651858.CD004712.pub3. [DOI] [PubMed] [Google Scholar]
- 20.Bennett MH, Stanford RE, Turner R. Hyperbaric oxygen therapy for promoting fracture healing and treating fracture non-union. Cochrane Database Syst Rev. 2012;11:CD004712. doi: 10.1002/14651858.CD004712.pub4. doi: 10.1002/14651858.CD004712.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karamitros AE, Kalentzos VN, Soucacos PN. Electric stimulation and hyperbaric oxygen therapy in the treatment of nonunions. Injury. 2006;37(Suppl 1):S63–73. doi: 10.1016/j.injury.2006.02.042. DOI: 10.1016/j.injury.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 22.Barilaro G, Francesco Masala I, Parracchini R, Iesu C, Caddia G, Sarzi-Puttini P, Atzeni F. The Role of Hyperbaric Oxygen Therapy in Orthopedics and Rheumatological Diseases. Isr Med Assoc J. 2017;19(7):429–434. [PubMed] [Google Scholar]
- 23.Millar IL, McGinnes RA, Williamson O, Lind F, Jansson KÅ, Hajek M, Smart D, Fernandes T, Miller R, Myles P, Cameron P. Hyperbaric Oxygen in Lower Limb Trauma (HOLLT); protocol for a randomised controlled trial. BMJ Open. 2015;6:e008381. doi: 10.1136/bmjopen-2015-008381. doi: 10.1136/bmjopen-2015-008381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mathieu D, Marroni A, Kot J. Tenth European Consensus Conference on Hyperbaric Medicine: recommendations for accepted and non-accepted clinical indications and practice of hyperbaric oxygen treatment. Diving Hyperb Med. 2017;47(1):24–32. doi: 10.28920/dhm47.1.24-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wroblewski AP, Mejia HA, Wright VJ. Application of platelet-rich plasma to enhance tissue repair. Oper Tech Orthop. 2010;20(2):98–105. [Google Scholar]
- 26.Jiang ZQ, Liu HY, Zhang LP, Wu ZQ, Shang DZ. Repair of calvarial defects in rabbits with platelet-rich plasma as the scaffold for carrying bone marrow stromal cells. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(3):327–333. doi: 10.1016/j.tripleo.2011.03.026. DOI: 10.1016/j.tripleo.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 27.Hernandez-Fernandez A, Velez R, Soldado F, Carlos Saenz-Ríos J, Barber I, Aguirre-Canyadell M. Effect of administration of platelet-rich plasma in early phases of distraction osteogenesis: an experimental study in an ovine femur model. Injury. 2013;44(7):901–907. doi: 10.1016/j.injury.2012.10.018. DOI: 10.1016/j.injury.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 28.Latalski M, Elbatrawy YA, Thabet AM, Gregosiewicz A, Raganowicz T, Fatyga M. Enhancing bone healing during distraction osteogenesis with platelet-rich plasma. Injury. 2011;42(8):821–824. doi: 10.1016/j.injury.2011.03.010. DOI: http://dx.doi.org/10.1016/j.injury.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 29.Hwang YJ, Choie JY. Addition of mesenchymal stem cells to the scaffold of platelet-rich plasma is beneficial for the reduction of the consolidation period in mandibular distraction osteogenesis. J Oral Maxillofac Surg. 2010;68(5):1112–1124. doi: 10.1016/j.joms.2008.08.038. doi: 10.1016/j.joms.2008.08.038. [DOI] [PubMed] [Google Scholar]
- 30.Dehghan MM, Baghaban Eslaminejad M, Motallebizadeh N, Ashrafi Halan J, Tagiyar L, Soroori S, Nikmahzar A, Pedram M, Shahverdi A, Kazemi Mehrjerdi H, Izadi S. Transplantation of Autologous Bone Marrow Mesenchymal Stem Cells with Platelet-Rich Plasma Accelerate Distraction Osteogenesis in A Canine Model. Cell J. 2015;17(2):243–52. doi: 10.22074/cellj.2016.3724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodriguez-Collazo ER, Urso ML. Combined use of the Ilizarov method, concentrated bone marrow aspirate (cBMA), and platelet-rich plasma (PRP) to expedite healing of bimalleolar fractures. Strategies Trauma Limb Reconstr. 2015;10(3):161–6. doi: 10.1007/s11751-015-0239-x. doi: 10.1007/s11751-015-0239-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papakostidis C, Bhandari M, Giannoudis PV. Distraction osteogenesis in the treatment of long bone defects of the lower limbs: effectiveness, complications and clinical results; a systematic review and meta-analysis. Bone Joint J. 2013;95-B(12):1673–80. doi: 10.1302/0301-620X.95B12.32385. doi: 10.1302/0301-620X.95B12.32385. [DOI] [PubMed] [Google Scholar]
- 33.Yin P, Ji Q, Li T, Li J, Li Z, Liu J, Wang G, Wang S, Zhang L, Mao Z, Tang P. A Systematic Review and Meta-Analysis of Ilizarov Methods in the Treatment of Infected Nonunion of Tibia and Femur. PLoS One. 2015;10(11):e0141973. doi: 10.1371/journal.pone.0141973. doi: 10.1371/journal.pone.0141973. [DOI] [PMC free article] [PubMed] [Google Scholar]


