Abstract
Introduction:
The most accurate way of assessing kidney function is the measurement of the glomerular filtration rate (GFR). Since, we do not have good formulae to estimate GFR in elderly, in this study we evaluate the accuracy of the most commonly used formulas for the estimation of GFR in comparison with direct measurement in elderly.
Materials and Methods:
85 patients (51 males and 34 females), with an average age of 76.2 ± 4.4 years, 42% already diagnosed with chronic kidney disease (CKD) were investigated. Two plasma samples were collected between 60-90 and 165-195 minutes after injection of 99mTc-DTPA, and the GFR was calculated applying Charles D. Russell’s two-sample method.
Results:
When comparing the GFR values obtained from the various formulae by creatinine levels with the GFR values obtained by measuring 99mTc-DTPA residue, the following concordance values emerged: (1) MDRD: 57.5 ± 9.59 %; (2) Cockroft-Gault: 48.33 ± 24.93; (3) CKD-EPI: 49.40 ± 26.30; (4) BIS1: 58 ± 6.79.
Conclusion:
Our data shows a greater concordance between the GFR values calculated with the Russell’s method and the estimated values of GFR when the latter are calculated using the MDRD or BIS1 formulae. (www.actabiomedica.it)
Keywords: CKD, eGFR, CKD-EPI, CKD-MDRD
Introduction
Chronic kidney disease (CKD) is an impending important problem in public health systems in western countries and in the near future even in developing ones. It is well known that CKD is associated with age-related decline in renal function and, owing to the demographic evolution, it is likely that the overall prevalence of CKD in the general population will increase in the coming years [1]. CKD progression is strongly related to diseases such as hypertension, diabetes, obesity and is conditioned by primary renal disorders. At the same time, CKD is a well-known independent cardiovascular risk factor [2]. In fact, a low glomerular filtration rate (GFR) is associated with increasing mortality, cardiovascular events, hospitalizations and costs. According to epidemiological reports, the age-standardized global prevalence of CKD stages 1–5 in adults was 10.4% in men (95% confidence interval [CI] 9.3–11.9) and 11.8% in women (95% CI 11.2–12.6). These values differed based on the population’s GDP (Gross Domestic Product), ranging from 8.6% in men (95% CI 7.3–9.8) and 9.6% in women (95%CI 7.7–11.1) in high-income countries to 10.6% in men ( 95% CI 9.4–13.1) and 12.5% in women (95% CI 11.8–14.0) in low- and middle-income countries [3].
The aim of our study was to evaluate the accuracy of the most commonly used formulas for the estimation of GFR in comparison with direct measurement in the elderly population; among 186 patients, we randomly selected 85 aged >70 yrs needing GFR measurement and renal scintigraphy for various clinical problems after obtaining their informed consent to participate in a study using GFR measurement based on the 99mTc-DTPA method. Diethethylenetriaminopenta-acetic acid (DTPA), a 99mTc-labelled analog of EDTA worldwide available, is routinely used in nuclear imaging (isotopic nephrogram) e.g. to measure the function of the right and left kidney separately. Advantages of 99mTc-DTPA include a short half-life (6 h) that minimizes radiation exposure, high counting efficiency of 99mTc, and high availability in most nuclear medicine departments. 99mTc-DTPA is thought to be freely filtered at the glomerulus, with minimal tubular reabsorption.
Materials and Methods
Patients
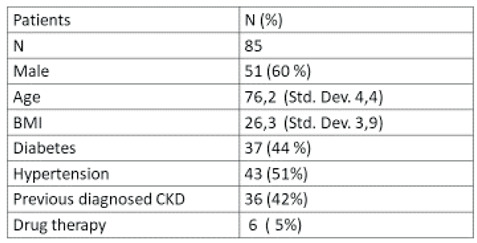
Our sample includes a total of 85 patients, of which 51 males and 34 females, with an average age of 76.2 ± 4.4 years. 51% have high blood pressure and 44% suffer from diabetes. Of the 85 total patients, 36 (42%) had already been diagnosed with CKD (Table 1).
Table 1.
Patient characteristics.
 |
The most recent creatinine values available for each patient were considered, and their levels were determined in our analysis laboratory; the average creatinine values is 1.52 ± 0.74, with a maximum of 4.2 and a minimum of 0.57. With these values, the GFR was calculated using the different formulas available: (1) MDRD: GFR 49.24 ± 20.85 ml/min; (2) Cockroft-Gault: 39.60 ± 14.60 ml/min; (3) CKD-EPI: 48.87 ± 21.09 ml/min; (4) BIS1: 45.40 ± 15.25 ml/min.
GFR calculation based on the 99mTc-DTPA method
The body handles intravenously injected 99mTc-DTPA according to a bi-compartment model: the chelate mixes between the vascular and extravascular space in the body while being cleared from the plasma by glomerular filtration in the kidneys. This model generates a bi-exponential plasma clearance curve following the initial mixing phase of 99mTc-DTPA in plasma. It possible to approximate bi-exponential plasma clearance curves to a mono-exponential plasma clearance curve; assuming that clearance is only by glomerular filtration, the GFR would be described as follows:
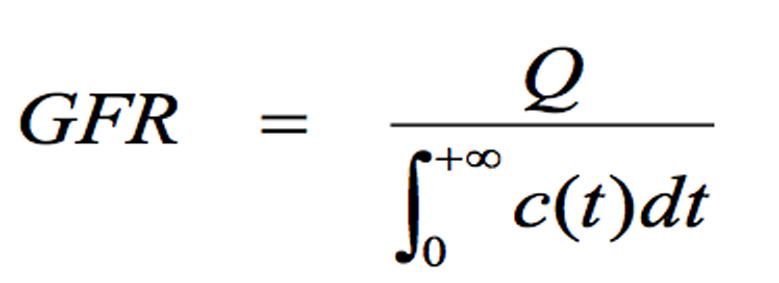
where Q is the amount of 99mTc-DTPA injected and c(t) its plasma concentration [11].
99mTc-DTPA (TechneScan®DTPA, Mallinckrodt) was prepared in accordance with the European Pharmacopoeia, Monograph 642, and quality control of radiochemical purity, performed by ITLC-SG chromatography, always gave a value >95%. The needle of a butterfly infusion set was placed in a peripheral vein. About 180 MBq of 99mTc--DTPA were injected. Residual activity in the syringe was less than 2% of the dose. Two EDTA blood samples were collected, the first between 60 and 90 minutes and the second between 165 and 195 minutes post- injection, using a vein other than that used for the injection. After centrifugation at 1500 g, duplicate samples of plasma were pipetted, counted in a gamma counter (COBRA auto gamma, Packard), cross calibrated weekly with a dose calibrator (PET-DOSE Comecer, Italy).
The GFR was calculated in accordance with the Russell two-sample method [12] and expressed as ml/min/1.73 m2. Body surface area was calculated using the DuBois & DuBois formula [13].
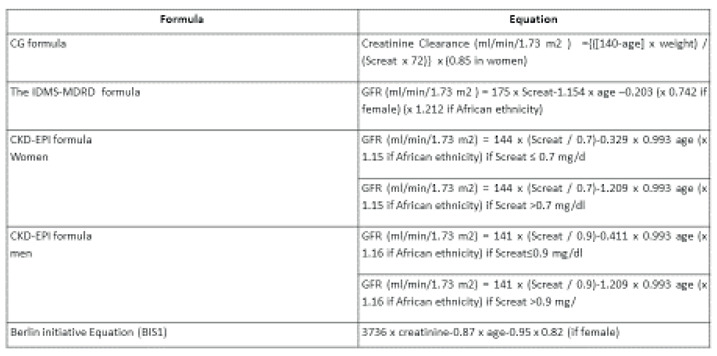
Serum creatinine determination and creatinine-based formulae
Serum creatinine (Screat, mg/dl) was measured at the time of the scintigraphic examination using an automatic system, Vitros 5600 (Roche Diagnostic GmbH, Mannheim), by peroxidase-catalysed oxidation, with a method standardized to IDMS (Isotope Dilution Mass Spectrometry). 99mTc-DTPA GFR values were compared with the GFR values measured using the following Screat-based formulae: CG formula, IDMS-MDRD formula, CKD-EPI formula, Berlin initiative Equation (BIS1) [14;15] (Table 2).
Table 2.
Formulae and related equations for GFR estimation.
 |
Statistical Analysis
All differences were tested against each other for significance using the t-test (a two-tailed P<0.05 was considered significant) and the square of Pearson’s correlation coefficient (R2). To compare the four alternative methods used for patient classification, we performed three different statistical tests. The first simply computes agreement as the percentage of exact agreements observed in the data set. The second considers the statistical procedure of Bland and Altman [16] and was used to compare the four alternative methods with 99mTc-DTPA. The limits of agreement between two different methods were defined as the mean ±1.96 SD of the difference between the methods. The third, a more refined method, computes the k value, which considers the agreement in excess of the amount of agreement expected by chance
Results
When comparing the GFR values obtained from the various formulae by creatinine levels with the GFR values obtained by measuring 99mTc-DTPA residue, the following concordance values emerged: (1) MDRD: 57.5 ± 9.59 %; (2) Cockroft-Gault: 48.33 ± 24.93; (3) CKD-EPI: 49.40 ± 26.30; (4) BIS1: 58 ± 6.79 (Table 3).
Table 3.
Concordance between formulae-estimated GFR and 99mTc-DTPA-measured GFR.
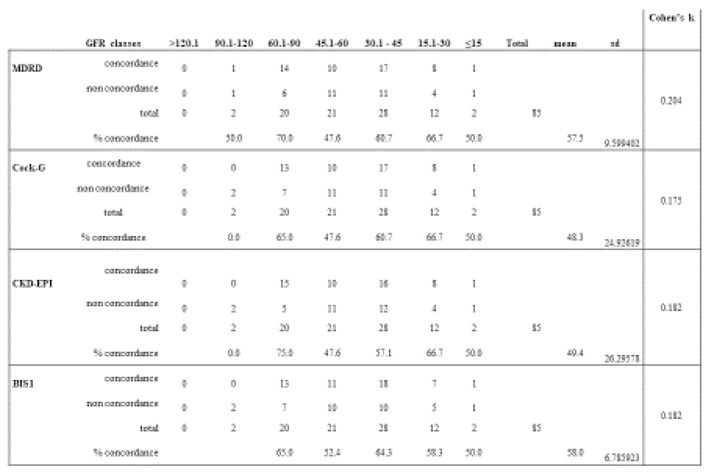 |
There appears to be a lower percentage of agreement between the GFR measured with the formulae and the one measured with the 99mTc-DTPA in a CKD stage between 45.1 and 60 ml/min.
Overall, the greatest concordance results from the use of MDRD and BIS1; however the latter is less in agreement for GFR values between 30 and 15 ml/min and lower than 15 ml/min (respectively 58.3% for GFR between 30-15 ml/min and 50% for GFR less than 15 ml/min). Although the agreement of MDR for GFR values <15 ml/min is equivalent to BIS1, in the range between 15-30 ml/min MDRD has a higher concordance than BIS1, 66.7%. In consideration of the possible relevance of the actual GFR in the clinical management of patients at a non-dialysis stage, the use of the MDRD formula is advisable compared to the others, as it is more consistent with the real GFR measured by 99mTc-DTPA.
We have studied how our GFR values differ from those estimated with the available formulae, if it is a difference tending to higher or lower GFR values. For each formula, about half of the patients remain in the same GFR class both with 99mTc-DTPA and with the use of formulae:
MDRD: the formula detects a worse GFR for 23.6% of patients compared to the values obtained with 99mTc-DTPA; in particular, 22.4% of these are in a lower stage of IRC, 1.2% two stages lower. On the contrary, the formula overestimates GFR for 16.5% of patients, 9.4% of whom have CKD at a more advanced stage, 7.1% CKD at two advanced stages (fig. 1)
Figure 1.
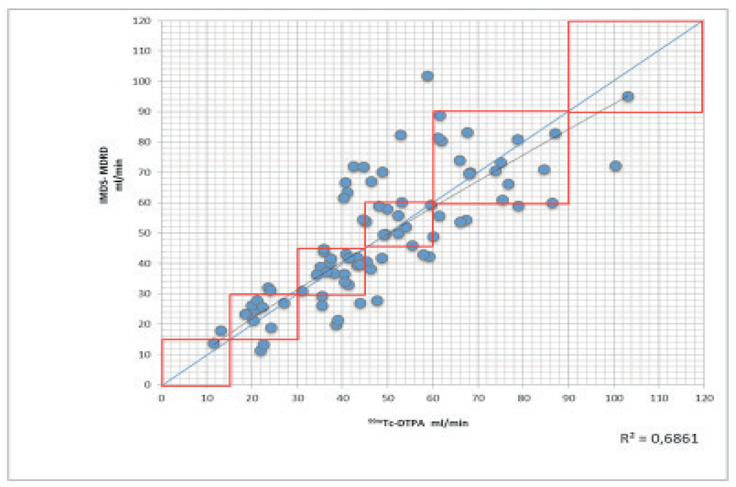
99mTc-DTPA vs. creatinine clearanceIMDS-MDRD. The rectangles represent the clinical levels of GFR (see text). GFR, glomerular filtration rate; IMDS-MDRD, isotope dilution mass spectrometry-modification of diet in renal disease; 99mTc-DTPA, 99mTcdiethylene triamine pentaacetic acid.
COCKROFT-GAULT: the formula detects a worse GFR for 29.4% of patients compared to the values obtained with 99mTc-DTPA; in particular, 28.2% is in a lower stage of CKD, 1.2% two stages lower. On the contrary, the formula overestimates GFR for 13% of patients, 10.6% of whom have CKD at a more advanced stage, 2.4% CKD two stages higher.
CKD-EPI: the formula detects a worse GFR for 24.7% of patients compared to the values obtained with 99mTc-DTPA; in particular, 23.5% are in a lower stage of CKD, 1.2% two stages lower. On the contrary, the formula overestimates GFR for 16.5% of patients, 10.6% of whom have CKD at a more advanced stage, 5.9% IRC two stages higher.
BIS1: the formula detects a worse GFR for 24.8% of patients compared to the values obtained with 99mTc-DTPA; in particular, 22.4% is in a lower stage of CKD, 2.4% two stages lower. On the contrary, the formula overestimates GFR for 16.5% of patients, all with CKD at a more advanced stage. (Table 4) (fig. 2)
Table 4.
Overstimation and understimation of GFR in different formulae.
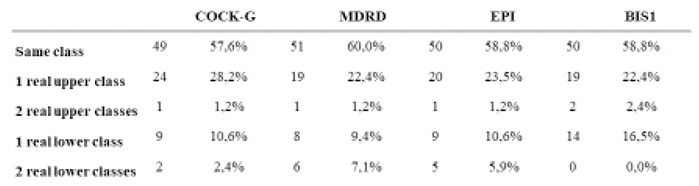 |
Figure 2.
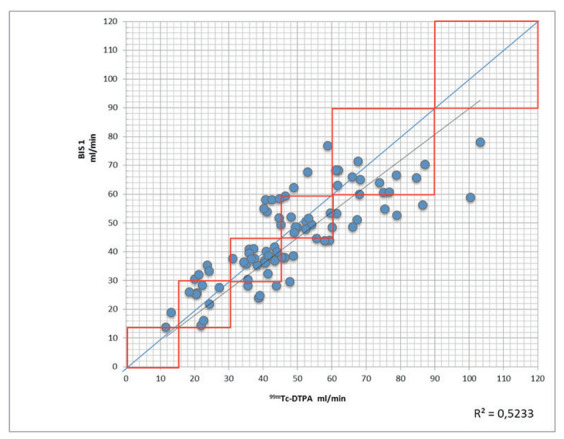
99mTc-DTPA vs. BIS1. The rectangles represent the clinical levels of GFR (see text). 99mTc-DTPA, 99mTc-diethylene triamine pentaacetic acid.
Bland Altman’s and k value analysis shows that in all the methods analyzed there is a bias and that no method can be used as equally valid compared to the 99mTc-DTPA
Discussion
Our data shows a greater concordance between the GFR values calculated with the Russell’s method and the estimated values of GFR when the latter are calculated using the MDRD or BIS1 formulae. However, the second one proves to be less reliable for filtrate values between 30 and 15 ml/min, a range in which, on the contrary, MDRD obtains the best concordance results.
From the data emerged from our study, the MDRD formula seems to be the most reliable for the category of patients we considered, contrary to what emerged from the previous study [9]. According to the current data, the MDRD formula seems to be the preferable one as it is more reliable in guaranteeing an optimal clinical management of patients.
In agreement with our previous study, we found a lower percentage of agreement between the GFR measured with the formulae and the one measured with the 99mTc-DTPA in the CKD stage between 45.1 and 60 ml/min.
The non-concordance between estimated and actually measured GFR raise the question not only of the reliability of formulas for certain categories of patients, but also of clinical management of such patients; in fact, as emerged from the reported data, for some patients the actual GFR values were different from the formulae, resulting in a different renal failure stage, one or even twice higher or lower.
This consideration can be of fundamental importance for the clinical management of certain categories of patients, for which knowing the exact filtrate value is decisive for a certain therapy to be undertaken in place of another: under these circumstances it is essential to know the exact glomerular filtration rate and one cannot simply rely on the estimates provided by the formulae commonly used by clinicians, in view of their lack of full reliability for certain classes of patients, as described above,.
Glomerular filtration rate (GFR) is accepted as the best indicator of kidney function and is commonly estimated in clinical and epidemiological settings from serum creatinine (SCr) based equations [4]. Assessment of glomerular filtration rate (GFR) is essential in the clinical practice; it is crucial for interpreting symptoms, signs and laboratory abnormalities that may be indicators of kidney disease, for drug dosing, and for detecting, managing and estimating the progression and the prognosis of chronic kidney disease. Therefore, early detection of at-risk populations with decreased kidney function is important for both acute kidney injury and chronic kidney disease (CKD). Measuring GFR is considered to be the more precise method for determining the kidney function and is therefore frequently referred to as the “gold standard” using clearance methods. Urinary inulin clearance, the classic method for measuring GFR described by Smith [5], is too difficult to be used in the clinical practice and for clinical research purposes; consequently, alternative filtration markers and clearance methods are used to measure GFR. The one that is still most often used in the clinical setting is the creatinine clearance [6]. Creatinine clearance procedure needs urine to be collected over a certain period of time — usually 24 or 12 hours — to measure the urinary creatinine concentration [7]. In addition, it is necessary to determinate the serum creatinine concentration at end of the collection period as well. This method, widely used for a long time and still in use in the clinical practice is extremely error-prone owing to two main factors: improper urine collection (especially outpatients) and creatinine behavior (tubular secretion when plasma levels are high).
The ideal marker for measuring GFR should have these features: (I) its production and plasma concentration must be constant if GFR does not change; (II) it must be free in plasma (not binding to protein) and must be freely and fully filtrated through the glomerulus; (III) neither secreted nor absorbed by renal tubules; (IV) inert and not toxic; (V) its excretion must be exclusively done by kidneys; (VI) it must be easily measured in both plasma and urine
Other more accurate methods have been introduced consisting in the intravenous infusion of exogenous filtration marker, with subsequent measurement of its plasma clearance such as Iothalamate, Iohexol, chromium ethylenediaminetetraacetate 51Cr-EDTA, diethylenetriaminepentaacetic acid 99mTc-DTPA.
In the clinical practice, GFR is most commonly estimated from serum creatinine using mathematical formulae [8]. In the last years different groups have been working to optimize GFR assessment, which has led to many papers about GFR estimation or measurement. In an attempt to get as close as possible to the true GFR, several novel GFR estimation formulae (eGFR) have been developed as CG (Cockcroft-Gault formula), MDRD (modification of diet in renal disease), CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) and, more recently, the Berlin Initiative Study 1 (BIS1) equation.
Once universally accepted that plasma creatinine value could not represent a unique valid endogenous marker for the evaluation of renal function or CKD progression, cystatin C has been analyzed extensively in terms of its performance in GFR assessing. However, none of these methods except the BIS1 equation has been validated in a large population of elderly patients, leading to the following question: what is the best method, applicable in ambulatory practice, to evaluate kidney function in the elderly? [3]
In a recent study, the authors evaluated kidney function in two groups of patients, <70 years and aged over 70 years, using different methods, including the 99mTc-DTPA method, to establish which creatinine-based formula produces the best measurement of renal function [9]. The results seem to show that the level of concordance between 99mTc-DTPA and clinical formulae was greater in patients younger than 70 years than in those aged 70 and above. Moreover, the authors noticed that the MDRD and CKD-EPI equations cannot be considered for estimating GFR in individuals older than 70 years.
In the study of Huang et al. the authors compared the performance of 99mTc-DTPA, renal dynamic imaging (RDI), MDRD equation and CKD EPI equation to estimate GFR [10]. The authors enrolled 551 subjects, including CKD patients and healthy individuals, and they found that RDI and the MDRD equation underestimated GFR and that CKD EPI overestimated it. They concluded that RDI should not be recommended as a reference standard against which other GFR measurement methods are assessed, except for individuals with eGFR between 30 and 59 ml/min/1.73 m2; in this group of patients, in fact, RDI provides a better estimate for GFR and could be helpful to distinguish stage 3a and 3b CKD.
In this regard, it is necessary to underline the importance of performing renal scintigraphy, a relatively inexpensive, simple and non-invasive examination, which exposes to very low radiation doses, and which allows to obtain a reliable value of renal function. It is therefore important to make clinicians aware of the method in order to correctly assess renal function and ensure that patients have the best therapeutic path, which may become as personal as possible.
Bibliography
- 1.Zhang QL, Rothenbacher D. Prevalence of chronic kidney disease in population-based studies: systematic review. BMC Public Health. 2008;8:117. doi: 10.1186/1471-2458-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cozzolino M, Mangano M, Stucchi A, Ciceri P, Conte F, Galassi A. Cardiovascular disease in dialysis patients. Nephrol Dial Transplant. 2018 Oct 1;33(suppl_3) doi: 10.1093/ndt/gfy174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mills KT, Xu Y, Zhang W, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88:950–957. doi: 10.1038/ki.2015.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Pottelbergh G, van Heden L, Matheï C, Degryse J. Methods to evaluate renal function in elderly patients: a systematic literature review. Age Ageing. 2010 Sep;39(5):542–20. doi: 10.1093/ageing/afq091. [DOI] [PubMed] [Google Scholar]
- 5.Levey A, Inker L, Coresh J. GFR estimation: from physiology to public health. Am J Kidney Dis. 2014 May;63(5):820–20. doi: 10.1053/j.ajkd.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pottel H, Hoste L, Dubourg L, Ebert N, Schaeffner E, Eriksen BO, Melsom T, Lamb EJ, Rule AD, Turner ST, Glassock RJ, de Souza V, Selistre L, Mariat C, Martens F, Delanaye P. An estimated glomerular filtration rate equation for the full age spectrum. Nephrol Dial Transplant. 2016 May;31(5):798–20. doi: 10.1093/ndt/gfv454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaeffner E. Determining the Glomerular Filtration Rate-An Overview. J Ren Nutr. 2017 Nov;27(6):375–380. doi: 10.1053/j.jrn.2017.07.005. doi: 10.1053/j.jrn.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Ji M, Lee YH, Hur M, Kim H, Cho HI, Yang HS, Navarin S, Di Somma S. GREAT Network. Comparing Results of Five Glomerular Filtration Rate-Estimating Equations in the Korean General Population: MDRD Study, Revised Lund-Malmö, and Three CKD-EPI Equations. Ann Lab Med. 2016 Nov;36(6):521–20. doi: 10.3343/alm.2016.36.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maioli C, Cozzolino M, Gallieni M, Del Sole A, Tagliabue L, Strinchini A, Gaito S, Lecchi M, Cusi D, Lucignani G. Evaluation of renal function in elderly patients: performance of creatinine-based formulae versus the isotopic method using 99mTc-diethylene triamine pentaacetic acid. Nucl Med Commun. 2014 Apr;35(4):416–20. doi: 10.1097/MNM.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 10.Huang Q, Chen Y, Zhang M, Wang S, Zhang W, Cai G, Chen X, Sun X. Comparative evaluation of technetium-99m-diethylenetriaminepentaacetic acid renal dynamic imaging versus the Modification of Diet in Renal Disease equation and the Chronic Kidney Disease Epidemiology Collaboration equation for the estimation of GFR. Int Urol Nephrol. 2018 Apr;50(4):733–20. doi: 10.1007/s11255-018-1811-3. [DOI] [PubMed] [Google Scholar]
- 11.Fleming JS, Wilkinson J, Oliver RM, Ackery DM, Blake GM, Waller DG. Comparison of radionuclide estimation of glomerular filtration rate using technetium 99m diethylenetriaminepentaacetic acid and chromium 51 ethylenediaminetetraacetic acid. Eur J Nucl Med. 1991;18:391–395. doi: 10.1007/BF02258429. [DOI] [PubMed] [Google Scholar]
- 12.Russell CD, Bischoff PG, Kontzen FN, Rowell KL, Yester MV, Lloyd LK, et al. Measurement of glomerular filtration rate: single injection plasma clearance method without urine collection. J Nucl Med. 1985;26:1243–1247. [PubMed] [Google Scholar]
- 13.DuBois D, DuBois EF. A formula to estimate the approximate surface area if height and weight are known. Ann Intern Med. 1916;17:863–871. [Google Scholar]
- 14.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 15.Fliser D, Ritz E. Serum cystatin C concentration as a marker of renal dysfunction in the elderly. Am J Kidney Dis. 2001;37:79–83. doi: 10.1053/ajkd.2001.20628. [DOI] [PubMed] [Google Scholar]
- 16.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurements. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]


