To the Editor,
The additional arguments supported by Sukhomlin (1) in the letter above could represent an essential aid in comprehending COVID infection and constitute important support in developing and deepening iron metabolism interaction in this affection.
The first impression we can get reading the commentary seems to contrast with our observations about hepcidin.
The ancestral role of hepcidin has the function to preserve from bacterial infection, reducing the availability of free iron outside the cell; thus, the bacteria minimize replication capability. The same effect is present in macrophages that incorporate iron and expel it as ferritin (2). Also, in pneumocytes, the effect exerted by direct production of Interleukine-6 and hepcidin is to reduce intralveolar iron; in fact, ferroportin is expressed on the alveolar surface (3,4) (see Figure 1 for better explanation).
Figure 1.
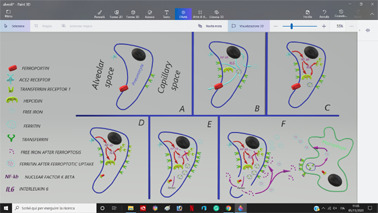
A) Pneumocytes distribution of Ace2 Receptor, ferroportin and transferrin receptors; B) Intracellular iron movements; C) Ace2 receptor stimulation and activation of NF-κB pathway with implementation of hepcidin, IL-6 and transferrin receptors; D) Ferroportin internalization trough hepcidin action and transferrin receptor exposition; E) Transferrin internalization with labile iron pool accumulation and initial Fenton chemistry; F) Excess of intracellular iron and consequent ferroptosis with free iron delivery and Macrophage iron capitation.
In the commentary proposed by Hirano (5), the Sars-Cov-2 virus links the ACE2 receptor of the alveolar cell by activating the NF-κB factor for its replication. The NF-κB requires iron for its activation by the complex IKK - IκB - NF-κB (6). The consequence of NF-kb activation stimulates hepcidin and IL-6 production (7). IL-6 also stimulates hepcidin and transferrin receptor 1 with consequent transferrin internalization (8) and iron accumulation in the alveolar cell. The intracellular iron persists the NF-κB activation (6). When this sequence is too accelerated, it causes an overcharge of intracellular iron and consequent ferroptosis (9). Ferroptosis itself and IL-6 production maintain hepcidin expression in macrophages, with the aim of iron sequestration, converting it to ferritin (2). Disruption of alveolar epithelium by ferroptosis releases several pro-inflammatory, procoagulant molecules and free iron ions in the blood torrent (10).
The consequence of all these processes is the contemporary use of hepcidin as a viral helper in replication and a defense immunity activator, consisting of a “Hepcidin paradox and an iron storm”. Understanding if cytokine storm could be restricted to an iron storm could be a target to address our treatments.
Several authors (11,12) previously observed the same conclusion, underlining the NF-κB pathway’s simultaneous use for viral replication and immunity reaction. A better comprehension of these two distinct phases could be useful in understanding COVID infection.
Conclusion
In her letter, the demonstrations reported by Sukhomlin added to our clinical observations suggest considering iron metabolism and the adverse effects promoted by non-transferrin bound iron, a topic to be deepened in the understanding and treating COVID infection.
Conflict of interest
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Sukhomlin T. Hepcidin is a friend rather than a foe in COVID19-induced complication. Acta Biomed. 2020;91(4):e2020138. doi: 10.23750/abm.v91i4.10768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nairz M, Theurl I, Swirski FK, Weiss G. “Pumping iron”-how macrophages handle iron at the systemic, microenvironmental, and cellular levels. Pflugers Arch. 2017 Apr;469(3-4):397–418. doi: 10.1007/s00424-017-1944-8. doi: 10.1007/s00424-017-1944-8. Epub 2017 Mar 1. PMID: 28251312; PMCID: PMC5362662.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang V, Nemeth E, Kim A. Iron in Lung Pathology. Pharmaceuticals (Basel) 2019 Feb 15;12(1):30. doi: 10.3390/ph12010030. doi: 10.3390/ph12010030. PMID: 30781366; PMCID: PMC6469192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim J, Wessling-Resnick M. The Role of Iron Metabolism in Lung Inflammation and Injury. J Allergy Ther. 2012;3(Suppl 4):004. doi: 10.4172/2155-6121.S4-004. doi: 10.4172/2155-6121.S4-004. Epub 2012 Jan 25. PMID: 29226014; PMCID: PMC5718378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirano T, Murakami M. COVID-19: A New Virus, but a Familiar Receptor and Cytokine Release Syndrome. Immunity. 2020 May 19;52(5):731–733. doi: 10.1016/j.immuni.2020.04.003. doi: 10.1016/j.immuni.2020.04.003. Epub 2020 Apr 22. PMID: 32325025; PMCID: PMC7175868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiong S, She H, Takeuchi H, Han B, Engelhardt JF, Barton CH, et al. Signaling role of intracellular iron in NF-kappaB activation. J Biol Chem. 2003 May 16;278(20):17646–54. doi: 10.1074/jbc.M210905200. doi: 10.1074/jbc.M210905200. Epub 2003 Mar 11. PMID: 12637578. [DOI] [PubMed] [Google Scholar]
- 7.Liao RX, Sun JG, Zhong XL, Zhou JX, Wang YZ. [Experimental study on transcription regulation of mouse hepcidin gene by NF-kB] Zhonghua Gan Zang Bing Za Zhi. 2006 Feb;14(2):118–23. Chinese. PMID: 16494782. [PubMed] [Google Scholar]
- 8.Kobune M, Kohgo Y, Kato J, Miyazaki E, Niitsu Y. Interleukin-6 enhances hepatic transferrin uptake and ferritin expression in rats. Hepatology. 1994 Jun;19(6):1468–75. PMID: 8188178. [PubMed] [Google Scholar]
- 9.Tao N, Li K, Liu J. Molecular Mechanisms of Ferroptosis and Its Role in Pulmonary Disease. Oxid Med Cell Longev. 2020 Jun 26 doi: 10.1155/2020/9547127. 2020:9547127. doi: 10.1155/2020/9547127. PMID: 32685102; PMCID: PMC7338975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kell DB, Pretorius E. Serum ferritin is an important inflammatory disease marker, as it is mainly a leakage product from damaged cells. Metallomics. 2014 Apr;6(4):748–73. doi: 10.1039/c3mt00347g. doi: 10.1039/c3mt00347g. PMID: 24549403. [DOI] [PubMed] [Google Scholar]
- 11.Zhao J, He S, Minassian A, Li J, Feng P. Recent advances on viral manipulation of NF-κB signaling pathway. Curr Opin Virol. 2015 Dec;15:103–11. doi: 10.1016/j.coviro.2015.08.013. doi: 10.1016/j.coviro.2015.08.013. Epub 2015 Sep 15. PMID: 26385424; PMCID: PMC4688235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santoro MG, Rossi A, Amici C. NF-kappaB and virus infection: who controls whom. EMBO J. 2003 Jun 2;22(11):2552–60. doi: 10.1093/emboj/cdg267. doi: 10.1093/emboj/cdg267. PMID: 12773372; PMCID: PMC156764. [DOI] [PMC free article] [PubMed] [Google Scholar]


