Abstract
This study aimed at the identification of the settings linked to SARS-CoV-2 transmission through the analysis of clusters and small outbreaks detected by the Lombardy Region surveillance system during the second epidemic wave. Comparing the data before and after the introduction of restrictive measures (night curfew, partial closure of schools and businesses, smart working), we observed a significant decrease of infections in workplaces, social gatherings, coffee shops, restaurants, and sports centers; contagion in schools decreased from 9.8% to 3.4%, in hospitals environments and nursing homes from 5.2% to 2%; domestic infections increased instead from 72.8% to 92.7%. These results suggest that containment measures have been effective in controlling virus circulation in the community but not at the household level and might inform future interventions, including the establishment of structures (Covid Hotels) for the isolation infected people. At the same time, they raise awareness on the risk of transmission among family members and during households social gatherings. (www.actabiomedica.it)
Keywords: SARS-CoV-2, transmission, household, containment
Introduction
The route of transmission and the setting of the contagion of an infectious disease are relevant aspects for the management of an epidemic and should guide containment and control strategies (1). In the case of SARS-Cov-2, infection transmission initially occurred at the hospital-level and in crowded social and healthcare settings such as nursing homes. However, at the start of the epidemic there was no reliable systematic collections of single outbreaks’ data (2, 3), with the exception of an estimate issued by the Italian National Institute of Health (INH) which categorized settings of infection for COVID-19 cases during the first epidemic wave – when a strict lockdown was imposed at the national level (4). During summer 2020 clubs, coffee shops, restaurants and other places for young generations’ gathering were identified as places at high risk of infection transmission, as reflected by the average age of infection which dropped from 70 years to about 40 years at that time (5). Household-level transmission, more frequent during lockdown periods, is intended not only as contagion between cohabitants, but also as contagion between members of the same family in other circumstances; therefore it includes gatherings for events such as birthday parties, funerals and other family gatherings. Determinants of household contagion are various, and include housing quality and population density, socio-demographic and cultural factors (6, 7).
Methods
In order to better monitor the dynamics of the pandemic, the Lombardy Region started, at the end of September 2020, a systematic collection of single outbreaks’ data in the context of the regional COVID-19 surveillance system. This has made it possible to collect data from all 8 Local Health Authorities (ATS) on the origin of new outbreaks and insert them in the weekly reports available to the Regional COVID-19 regional Task Force (Comitato Tecnico-Scientifico, CTS). Single outbreaks were defined as two or more new COVID-19 cases attributable to the same chain of infection after an epidemiological investigation. In the current analysis we compare single outbreaks’ data in the Lombardy region, collected before (19-25th October 2020) and after (2-8th November 2020) the introduction of “regional-level” containment measures on 22nd October 2020, during the second epidemic wave of COVID-19, and analyse the reported setting of transmission. These measures included nighttime curfew from 11pm to 5am, distance learning (for high schools), increase of smart working and closure of non-essential businesses and preceded those adopted by the Italian government by about 10 days (8)(9). Data from the Lombardy region are compared, as far as possible, with the estimates carried out by the INH in the spring of 2020, during the first epidemic wave.
Results
The comparison between the pre- and post-control measures adoption period showed a significant decrease in the proportion of infections acquired in the workplace (downward from 4.7% to 0.6%), during community social gatherings (from 3.3% to 0.6%), in bars and restaurants (from 0.8% to 0.2%), and during sports activities (from 2.2% to 0.2%). Contagion in schools decreased from 9.8% to 3.4%; in hospitals and other healthcare settings from 0.7% to 0.1% and in nursing homes from 4.5% to 1.9%. Overall, nosocomial transmission dropped from 5.2% to 2%, while household-level transmission increased from 72.8% to 92.7%. As reported in Figure 1, as the number of outbreaks increased over time in Lombardy, a proportional increase in the number of household-level outbreaks was also reported. In the two periods analyzed the number of new cases was stable (approximately 55,000 per week). Comparisons with national-level estimates during the first wave indicate a greater proportion of household-level transmission (from 24.7% to almost 93%) and a decreased contribution of healthcare-level transmission (from 54.9% to less than 5%, Table 1).
Figure 1.
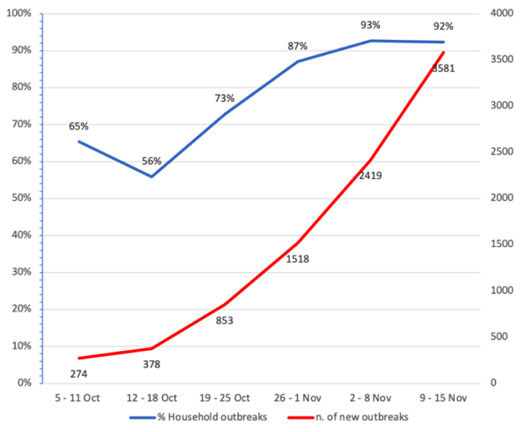
Trend of outbreaks and number of householding outbreaks in Lombardy Region 5th October-15th November 2020 (from Lombardy Region surveillance system)
Table 1.
Settings linked to SARS-CoV-2 transmission in Italy and in the Lombardy region
(source: (1) and Lombardy Region COVID-19 Surveillance systems)
| Settings | LOMBARDY 19-25th October 2020 | LOMBARDY 2-8th November 2020 | Estimate for Italy, June 2020 (5) | |||
| Outbreaks (n.) | % | Outbreaks (n.) | % | (%) | ||
| Hospitals | 6 | 0.7% | 3 | 0.1% | 10.8% | |
| Nursing Homes | 39 | 4.5% | 46 | 1.9% | 44.1% | |
| Household | 621 | 72.8% | 2,243 | 92.7% | 24.7% | |
| Schools | 83 | 9.8% | 83 | 3.4% | 0%* | |
| Workplaces | 40 | 4.7% | 15 | 0.6% | 4.2% | |
| Sport settings | 19 | 2.2% | 6 | 0.2% | ° | |
| Bar / Restaurants | 7 | 0.8% | 5 | 0.2% | ° | |
| Social gathering | 28 | 3.3% | 15 | 0.6% | ° | |
| Religious and other communities | 5 | 0.6% | 0 | 0% | 1.9% | |
| Cruise ships | 0 | 0% | 0 | 0% | 1.4% | |
| Centers for refugees | 2 | 0.2% | 1 | 0.1% | 0.2% | |
| Others | 2 | 0.2% | 2 | 0.1% | 12.8% | |
| Total | 853 | 100.0% | 2,419 | 100.0% | 100.0% | |
*Schools were closed in that period of time; °Included in category “others”
Possible bias
Our data are based on what reported by COVID-19 cases to healthcare workers during contact tracing and epidemic surveillance and therefore transmission occurred in some settings might be underestimated because of recall bias or lack of identification of specific modalities of infection (i.e. public transports, public areas, ets). An overestimation of household transmissions in the data presented cannot therefore be excluded. However, the comparison between pre- and post-intervention, showing a significant increase in household infections in this phase of the pandemic, is consistent with data from other international studies (10-12). A further matter of concern is that epidemiological investigations were carried out only in 50.6% of cases (5); however, there is no reason to believe that this under-reporting may have caused selection bias that would influence the main conclusions of this study.
Conclusion
The data here presented underline that almost all COVID-19 infections currently occur at the household-level. In the Lombardy Region this proportion increased after the adoption of restrictive measures. The second setting at high risk of contagion are schools, in a period during which about half of the students were still on distance learning. This supports the idea that school environments are still a place at risk. The very high number of household infections is to be considered while planning future prevention initiatives for the containment of COVID-19 pandemic. First of all, a part of these infections certainly occurred by infected or sick people in house fiduciary isolation. This fact underlines the need to identify different solutions for asymptomatic or paucisymptomatic COVID-19 cases, such as “Covid Hotels”. It is also believed that some of the infections occurred, even unconsciously, due to contacts with family members who contracted the infection before the diagnostic test was performed. In this case, poor preventive measures at home may have been cause the infection. However, it is essential that at this stage the importance of domestic risk is emphasized also in communication campaigns. Behaviors like sharing the same room and the same bed, sharing dishes, cutlery, glasses and bottles, excessive effusions, failure to respect safe distances, sharing telephones, bath towels and other objects that may come into contact with “droplets” of infected patients (even if asymptomatic) or sharing buildings’ lift are risky behaviors. The faster and better control of the COVID-19 pandemic also depends on the monitoring and control of such behaviors through effective preventive and educational interventions.
Fundings:
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 101003562.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet (London, England) 2020;395(10223):514–23. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Odone A, Delmonte D, Scognamiglio T, Signorelli C. COVID-19 deaths in Lombardy, Italy: data in context. The Lancet Public health. 2020;5(6):e310. doi: 10.1016/S2468-2667(20)30099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Signorelli C, Scognamiglio T, Odone A. COVID-19 in Italy: impact of containment measures and prevalence estimates of infection in the general population. Acta bio-medica : Atenei Parmensis. 2020;91(3-s):175–9. doi: 10.23750/abm.v91i3-S.9511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DPCM, 8 marzo 2020. Gazz Uff della Repubb Ital. “Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19.” [Google Scholar]
- 5. Istituto Superiore Di Sanita. Available at: https://www.iss.it/coronavirus . [accessed: 20.11.2020] [Google Scholar]
- 6.Amerio A, Brambilla A, Morganti A, Aguglia A, Bianchi D, Santi F, et al. COVID-19 Lockdown: Housing Built Environment’s Effects on Mental Health. International journal of environmental research and public health. 2020;17(16) doi: 10.3390/ijerph17165973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Odone A, Lugo A, Amerio A, Borroni E, Bosetti C, Carreras G, et al. COVID-19 lockdown impact on lifestyle habits of Italian adults. Acta bio-medica : Atenei Parmensis. 2020;91(9-s):87–9. doi: 10.23750/abm.v91i9-S.10122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DPCM, del 3 novembre 2020. Gazz Uff della Repubb Ital. “Ulteriori disposizioni attuative del decreto-legge 25 marzo 2020, n. 19, convertito, con modificazioni, dalla legge 25 maggio 2020, n. 35, recante «Misure urgenti per fronteggiare l’emergenza epidemiologica da COVID-19», e del decreto-legge 16 maggio 2020, n. 33, convertito, con modificazioni, dalla legge 14 luglio 2020, n. 74, recante «Ulteriori misure urgenti per fronteggiare l’emergenza epidemiologica da COVID-19».” [Google Scholar]
- 9.Ordinanza n. 623 Regione Lombardia. del 21/10/2020. Link: https://www.regione.lombardia.it/wps/wcm/connect/b52df501-feae-4103-b514-1038a5747d46/Ordinanza+623+del+21+ottobre.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-b52df501-feae-4103-b514-1038a5747d46-nlc7zJB. [utlimo accesso 20/11/2020] [Google Scholar]
- 10.Grijalva CG, Rolfes MA, Zhu Y, McLean HQ, Hanson KE, Belongia EA, et al. Transmission of SARS-COV-2 Infections in Households - Tennessee and Wisconsin, April-September 2020. MMWR Morbidity and mortality weekly report. 2020;69(44):1631–4. doi: 10.15585/mmwr.mm6944e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haroon S, Chandan JS, Middleton J, Cheng KK. Covid-19: breaking the chain of household transmission. BMJ (Clinical research ed) 2020;370:m3181. doi: 10.1136/bmj.m3181. [DOI] [PubMed] [Google Scholar]
- 12.Del Brutto OH, Costa AF, Mera RM, Recalde BY, Bustos JA, García HH. Household Clustering of SARS-CoV-2 in Community Settings: A Study from Rural Ecuador. The American journal of tropical medicine and hygiene. 2020;103(3):1207–10. doi: 10.4269/ajtmh.20-0688. [DOI] [PMC free article] [PubMed] [Google Scholar]


