Abstract
Aim:
evaluating the impact of screening programmes on colorectal cancer (CRC) in Italy.
Methods:
we studied 1292 patients with colorectal cancer. Data were collected from January 2004 through December 2015 in Parma University Hospital. We compared clinophatological features to evaluate the real impact of screening programmes on detecting early stage colorectal cancers in target population.
Results:
screening programmes with fecal occult blood test (FOBT) and colonoscopy covered only patients from 50 to 69. In our study we reported that the 52,3% of patients with CRC were over 70 and out of screen time, while only 47,7% were under 70. Early detection seems to be related to early stage of CRC and to an improved overall survival.
Conclusion:
The importance of early detection in colorectal cancers represents the most important outcome for OS. The risk of colorectal cancer is increased in elderly. Actual screening programmes cover less than 50% of population with colorectal cancer. Screening should be considered for patients over 70, due to the high number of new diagnosis in symptomatic disease and worst prognosis, in accordance with advanced cancer stage and comorbidities in elderly. (www.actabiomedica.it)
Keywords: colorectal cancer, screening programmes, elderly, FOBT, colonoscopy, survival
Introduction
Colorectal cancer (CRC) is a common and lethal disease.
The majority of CRC develops slowly from adenomatous polyps or adenomas (1). The risk of developing CRC is influenced by both environmental and genetic factors (2, 3).
CRC is the third for incidence and second for cancer deaths in 2015.
CRC incidence and mortality rates vary markedly around the world. Globally, CRC is the second most common cancer in females and the third one in males, with 1.65 million new cases and almost 835000 deaths in 2015. In Europe there were 447136 new cases of CRC in 2012 and 214866 deaths (12.2% of the total number of cancer deaths, 2nd most common cause of cancer related deaths). The 5-year prevalence of CRC in 2012 was estimated at 1203943 in Europe. In 2012, the cumulative risk of CRC in people aged under 75 was 1.95% worldwide and 3.51% in Europe (4, 5). In Italy there were 52000 new cases in 2016 and 18756 deaths in 2013. The 5-year survival rate is 60,8% for colon cancer and 58,3 for rectal cancer (6, 7).
During the last decades the develop of minimally invasive techniques and the amelioration of surgical strategy (8, 9) contributed to an overall increase in postoperative outcomes, but poorly affecting overall survival.
In Italy, before 1999, only one screening programme had been activated (10). The value of screening programmes has been accredited by various international societies. In Italy a structured screening programme started in 2005. Nowadays, screening programmes with fecal occult blood test (FOBT) every two years and colonoscopy only with positive FOBT are reserved to people from 50 to 69.
In Italy people’s compliance for CRC screening programmes with FOBT increases every year with an adherence of 43% in 2015 (6, 7, 11).
Study Protocol
We retrospectively collected data from a total of 1292 CRC patients who underwent curative surgery at Parma University Hospital from January 2005 through December 2015.
In our study we included: 1. Patients with primary CRC; 2. Colorectal cancers screen detected, non-screen detected; 3. Patients who underwent curative surgery with laparoscopic or laparotomic approach.
We divided patients into three subgroups according to the time of surgery (2004-2007; 2008-2011; 2012-2015) to evaluate the impact of screening programmes through the years. After curative surgery, all patients were followed through the years or until their death. The follow up of all patients in this study was completed in December 2017.
Statistical Methods
According to the Kaplan-Meier method and compared by log-rank test, the survival analysis and curves were calculated observing postoperative survival time. The chi-square test was used to evaluate the statistical significance of differences. Cox proportional hazard model was used for multivariate analyses. Kruskal-Wallis test was used to compare two or more independent samples, equal or different in sizes.
All factors regarded statically significant present a P values <0,05.
Results
Patient characteristics
Among 1292 patients with colorectal cancer, 439 died during the follow-up. 686 (56,7%) were male while 524 (43,3%) were female (Tab. 1).
Table 1.
Sex distribution
| Gender | N | Deaths |
| Male | 733 | 266 |
| Female | 559 | 173 |
In our study, 611 patients (47,7%) were younger than 69, 670 (52,3%) were older than 70, out of screen time (Tab. 2).
Table 2.
Age distribution
| Frequency | % | Valid % | Cumulative % | |
| Age | ||||
| <=60 | 251 | 19.4 | 19.6 | 19.6 |
| 60-70 | 360 | 27.9 | 28.1 | 47.7 |
| >70 | 670 | 51.9 | 52.3 | 100.0 |
| Total | 1281 | 99.1 | 100.0 | |
| Missing | 11 | 0.9 | ||
| Total | 1292 | 100.0 | ||
The most performed procedure was right emicolectomy (522) followed by left emicolectomy (335); anterior rectal resection (RAR) (238), sigmoidectomy (120), transverse colon resection (51) and abdominoperineal resection (APR) (26).
The median age at the time of surgery was higher for right emicolectomy thane left emicolectomy (Tab. 3, 4).
Table 3.
Surgical procedure
| Surgical procedure | Total N | Deaths |
| Right emicolectomy | 522 | 179 |
| Left emicolectomy | 335 | 92 |
| Transverse colon resection | 51 | 23 |
| Sigmoidectomy | 120 | 48 |
| RAR | 238 | 88 |
| APR | 26 | 9 |
| Overall | 1292 | 439 |
Table 4.
Median age distribution for cancer site and surgery
| Surgical procedure | Median age |
| Right emicolectomy | 72.67 |
| Left emicolectomy | 67.60 |
| Transverse colon resection | 71.79 |
| Sigmoidectomy | 69.01 |
| RAR | 68.21 |
| APR | 70.42 |
According to TNM staging system we found:
T1 stage: 108; T2: 240; T3: 774; T4a: 112; T4b:58
N0: 779; N1a-b: 280; N2a-b: 233.
Statistical analysis
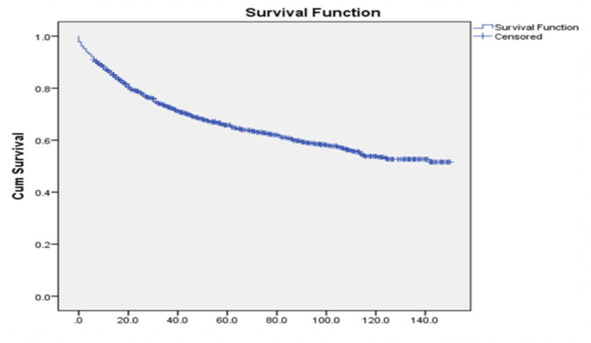
In our study 5-year OS was 70%. (Fig. 1).
Figure 1.
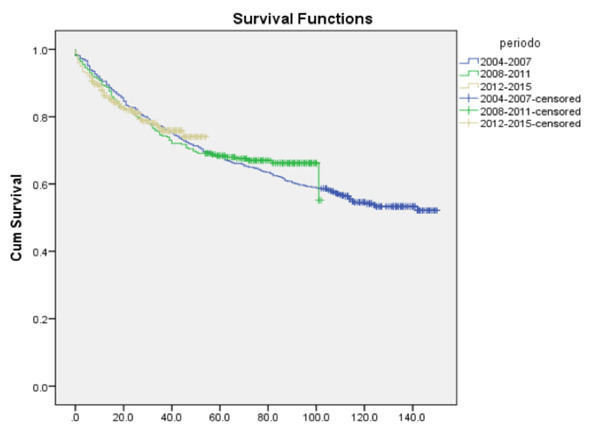
On the three periods on examination we found a non-statistically significant stackable OS. (P>00,5) (Fig. 2).
Figure 2.
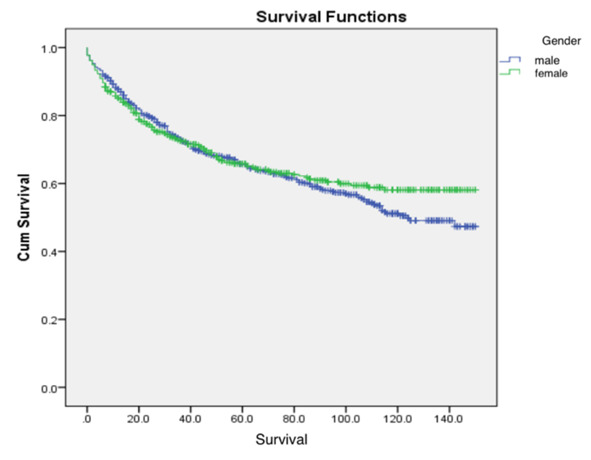
OS differences in male and female was not statistically significant (P>0.05) (Tab. 5, Fig. 3).
Table 5.
Sex distribution through the years
| Period | Total | |||||
| 2004-2007 | 2008-2011 | 2012-2015 | ||||
| Gender | Male | Count | 340 | 207 | 186 | 733 |
| % within gender | 46.5% | 28.1% | 25.4% | 100.% | ||
| % within period | 60,3% | 56.3% | 51.5% | 56.7% | ||
| Female | Count | 224 | 160 | 175 | 559 | |
| % within gender | 40.1% | 28.6% | 31.3% | 100.0% | ||
| % within period | 39.7% | 43.7% | 48.5% | 43.3% | ||
| Total | Count | 564 | 367 | 351 | 1292 | |
| % within gender | 43.7% | 28.3% | 27.9% | 100.0% | ||
| % within period | 100.0% | 100.0% | 100.0% | 100.0% | ||
Figure 3.
We found that only 47.7% of colorectal cancers were detected in screen time. In patients over 70 the incidence of CRC was higher, with an increased number of new diagnosis out of screening programmes and a worst prognosi. (Tab. 2, 6, 7).
Table 6.
Age distribution through the years
| Period | Total | |||||
| 2004-2007 | 2008-2011 | 2012-2015 | ||||
| Age | <60 | Count | 129 | 55 | 67 | 251 |
| % within age | 51.5% | 21.7% | 26.8% | 100.0% | ||
| % within period | 23.0% | 15.1% | 18.6% | 19.6% | ||
| 60-70 | Count | 173 | 108 | 79 | 360 | |
| % within age | 48.3% | 29.9% | 21.8% | 28.7% | ||
| % within period | 31.6% | 30.6% | 22.2% | 100.0% | ||
| >70 | Count | 256 | 197 | 217 | 670 | |
| % within age | 38.3% | 29.5% | 32.2% | 100.0% | ||
| % within period | 45.3% | 54.3% | 59.2% | 51.7% | ||
| Total | Count | 558 | 360 | 363 | 1281 | |
| % within age | 43.8% | 28.1% | 28.2% | 100.0% | ||
| % within period | 100.0% | 100.0% | 100.0% | 100.0% | ||
Table 7.
Vital status by age
| Vital Status | Total | ||||
| Alive | Deaths | ||||
| Age | <60 | Count | 201 | 50 | 251 |
| % within age | 80.2% | 19.8% | 100.% | ||
| 60-70 | Count | 240 | 120 | 360 | |
| % within age | 66.6% | 33.3% | 100.0% | ||
| >70 | Count | 401 | 269 | 670 | |
| % within age | 59.8% | 40.2% | 100.0% | ||
| Total | Count | 842 | 439 | 1281 | |
| % within age | 65.7% | 34.3 | 100.0% | ||
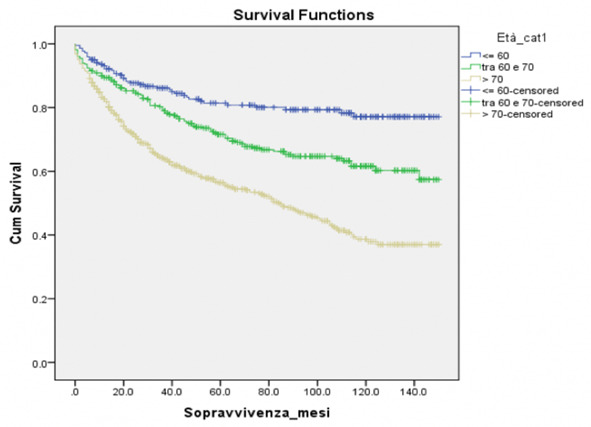
Lower overall survival for patients over 70 was statistically significant (P=0.032) (Tab. 7, Fig. 4).
Figure 4.
Discussion
Japan, where the incidence of CRC is one of the highest compared to Europe, shows a lower incidence of mortality and this is due to the highly effective screening programmes (17, 18). These observations imply that screening has a significant impact on reducing CRC death rate.
A screening test must be well accepted in order to get a highly successful screening programme. The adherence to the screening programme is extremely important for the efficacy of the screening test itself, nevertheless, in practice, adherence to CRC screening is quite variable.
In Spain, Quintero in his study reported adherence of 34% for the initial FOBT and 25% for colonoscopy (19). In Italy the participation rates to screening programmes in 2015 was the 43% of target population, 5,1% of them had positive FOBT and 79,6% with positive result accepted colonoscopy. During the same period coloscopic screening programmes showed a worst compliance with only 24% of adhesions in 2016 (6, 7, 11).
When the screening programmes started in Italy, the study IMPATTO, including people from 40 to 79 through 2000 to 2008, showed only a little reduction of incidence with remarkable differences among the North-Centre, the South and the Islands (20).
Nowadays, improved screening programmes show a reduction of mortality of 13-22% in screen detected areas vs non-screen detected areas, with early stage at the time of diagnosis and better overall survival (21, 22).
In Emilia Romagna, screening programme with FOBT started in 2005 (23). Until 2007 adherence to FOBT was only 47,6% of target population (24) with 5,5% of positive FOBT. The 80,2% with positive FOBT accepted colonoscopy.
During 2008-2011 the 99,5% of resident population were invited and only 51,6% accepted FOBT. Colonoscopy was performed in 82,6% of the patients with positive FOBT (4,7%) (25).
In the last period (2012-2015) in Emilia-Romagna there was an adherence of 50,3% to screening programmes with FOBT, though only 85,4% of the 5,2% with positive FOBT underwent colonoscopy (26).
Moreover, based on the results of our study, a 52,3% of patients with CRC were over 70 and out of screen time, presenting a worst prognosis.
Conclusion
Despite the outstanding effect on early stage detection and overall survival, a majority of patients who may benefit from the screening is excluded for age cutoff. Data of our study suggest the possibility to extended the screening programme to patients over 70, in consideration to the increase in life expectancy. Elderly patients in good health and with an expectation of long remaining lifespan, might greatly get benefit from the screening programmes (27). Extending the screening programme until 79 in patients in good health seems to be highly reccomendable, in order to improve early stage CRC detection and OS.
Conflict of interest:
None to declare
References
- 1.Levine JS, Ahnen DJ. Clinical practice. Adenomatous polyps of the colon. The New England journal of medicine. 2006;355(24):2551–2557. doi: 10.1056/NEJMcp063038. [DOI] [PubMed] [Google Scholar]
- 2.Costi R, Azzoni C, Marchesi F, et al. Repeated anastomotic recurrence of colorectal tumors: genetic analysis of two cases. World J Gastroenterol. 2011 Aug 28;17(32):20–21. doi: 10.3748/wjg.v17.i32.3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarli L, Bottarelli L, Azzoni C, et al. Loss of p27 expression and microsatellite instability in sporadic colorectal cancer. Surg Oncol. 2006 Aug;15(2):97–20. doi: 10.1016/j.suronc.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 5.Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. Jama Oncol. 2017 Apr 1;3(4):20–21. doi: 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Associazione Italiana di Oncologia Medica – AIOM. [Google Scholar]
- 7. Associazione Italiana Registri Tumori – AIRTUM. [Google Scholar]
- 8.Marchesi F, Pinna F, Percalli L, et al. Totally laparoscopic right colectomy: theoretical and practical advantages over the laparo-assisted approach. J Laparoendosc Adv Surg Tech A. 2013 May;23(5):418–20. doi: 10.1089/lap.2012.0420. [DOI] [PubMed] [Google Scholar]
- 9.Cecchini S, Azzoni C, Bottarelli L, et al. Surgical treatment of multiple sporadic colorectal carcinoma. Acta Biomed. 2017 Apr 28;88(1):20–21. doi: 10.23750/abm.v88i1.6031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zorzi M, Barca A, Falcini F, et al. Screening for colorectal cancer in Italy: 2005 survey. Epidemil Prev. 2007 Mar-Jun;31(2-3 Suppl 2):49–60. [PubMed] [Google Scholar]
- 11.Osservatorio Nazionale Screening. 2016 [Google Scholar]
- 12.Shin-ei Kudo, Tayoki Kudo. The necessity of colorectal cancer screening for elderly patients. Transl. Gastroenterol Hepatol. 2017;2:19. doi: 10.21037/tgh.2017.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]


