Abstract
Reorganization of healthcare resources due to COVID-19 pandemic has led to an unintentional neglect of essential care, especially for paediatric emergencies. This phenomenon has been observed also for type 1 diabetes patients at onset, and surveys from different countries have shown an increased number of diabetic ketoacidosis during lock-down period. We report the case of two patients admitted late at our emergency care service for type-1 diabetes at onset with ketoacidosis, for reasons related to COVID-19 pandemic outbreak. Case report 1: A 5 years old boy, presented with a severe diabetic ketoacidosis, requiring admission in Intensive Care Unit, prolonged intravenous insulin infusion and enteral nutrion via nasogastric tube. Case report 2: A 10 years old girl presented in the emergency department with a history respiratory distress, due to Kussmaul’s breathing, and severe dehydration. Laboratory findings were consistent with a diagnosis of moderate diabetic ketoacidosis. We have further analyzed the experience of our Centre regarding new onset type 1 diabetes patients during lock-down period: we observed a reduction of admissions for type 1 diabetes onset during lock-down period compared to same period of 2019, with a higher prevalence of moderate and severe diabetic ketoacidosis. We conclude highlighting the upcoming necessity, due to the emerging of a ‘second wave’ of the pandemic, that public opinion and healthcare practitioners provide correct information regarding access to paediatric services, in particular for children with newly onset symptoms, in order to avoid late access to emergency department in critical situations and to prevent avoidable morbidity and mortality. (www.actabiomedica.it)
Keywords: COVID-19, diabetic ketoacidosis, type 1 diabetes
Introduction
The COVID-19 pandemic is a major health emergency that is impacting the behaviour of entire populations creating an environment of strong emotions in the community, especially fear. Many clinicians have highlighted the problem of access to and utilisation of services. The reasons are presumed to be a combination of factors related to patients and doctors as well as the health care system and its management during the peak of the COVID-19 crisis. Although control measures are effective at containing the spread of disease, and undoubtedly contribute to preserving services from collapsing, they are expected to have also negative effects in delaying diagnosis and treatment for some patients during the COVID-19 pandemic.
Italy saw an exponential growth in COVID-19 cases from the day the first patient was identified in the north of Italy until the 9th of March, when the Italian government imposed the national lock-down.
By the time of this commentary more than 358.499 cases of COVID-19 and 36,233 deaths have been reported in Italy. Only 7,3% of these cases occurred in paediatric age (0-19 years) (1).
Castagnoli et al. highlighted that children also are susceptible to COVID-19 but with a more benign course compared to adults and a study conducted with over 2000 paediatric subjects showed that 89,7 % children had low-moderate severity disease and 4.4% were asymptomatic (2).
Despite few cases and mild clinical symptoms on the paediatric population, COVID-19 pandemic in Italy has indirectly affected the quality of care in paediatrics.
During the lock-down period paediatric first aid facilities have organised special paths to limit the possibility of infection but the fear of contracting COVID-19 has led many parents to delay access to the paediatric first aid despite children’s impaired health conditions.
In addition, temporary restructuring of the health system to deal with pandemic has caused the closure of peripheral paediatrics facilities making access to care even more difficult.
Data on first aid access in five paediatric hospitals in Italy from 1 to 27 March 2020 showed that paediatric emergency department visits have been reduced by 73% and 88% compared to the same periods in 2019 and 2018 respectively (3).
According to Roberton et al. (4), the redistribution of healthcare resources for COVID-19 pandemic has led to an unintentional neglect of essential care.
In this way, children with the onset of COVID-19 non-related disease during the pandemic had a higher risk of developing adverse events.
Newly diagnosed diabetic children were reported to rapidly progress to diabetic ketoacidosis because of a delayed treatment, increasing the risk of morbidity and mortality (5).
We describe 2 patients admitted late to our hospital with moderate to severe DKA during lock-down period.
Case 1
A 5 years old boy, living 1 hour away from Parma Children Hospital, was admitted to the emergency room with a one-week history of weight loss (about 4 kg) and respiratory distress. The parents were from Tunis.
He was in severe clinical conditions with a reduced state of consciousness (Glasgow Coma Scale 7/15), polypnea and dyspnea due to Kussmaul’s breathing and severe dehydration with hypothermia. Heart rate was 140 ppm, oxygen saturation was 100%. He was severely underweight and showed an important abdominal distension and stiffness with absent peristalsis (figure 1). His weight was 14,5 kg (-2,37 SDS) and body mass index (BMI) was 11,8 kg/m2 (-5,11 SDS).
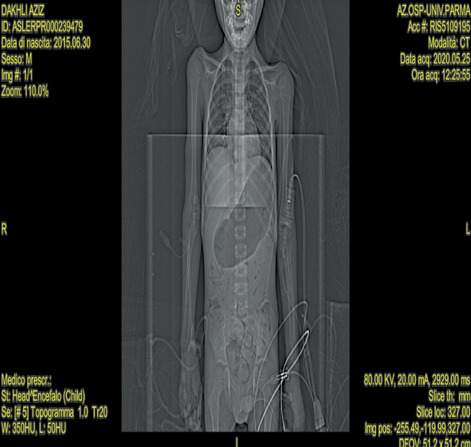
Figure 1.

Clinical conditions of the child, showing severe underweight status, upon arrival in Intensive Care Unit
Laboratory findings on admission are summarized in Table 1, consistent with a diagnosis of severe diabetic ketoacidosis (DKA).
Table 1.
Laboratory findings on admission for patient 1
| Parameter | Vale |
| Blood glucose mg/dl | 756 |
| pH | 6,8 |
| HCO3- mmol/l | 5,4 |
| B-OH-butirrate mmol/l | 5,9 |
| Corrected sodium mmol/l | 164 |
| Corrected potassium mmol/l | 2,5 |
He was then referred to the intensive care unit and intravenous fluids, insulin and potassium replacement were started according to the local protocol for the management of DKA (6).
Acidosis, hyperglycaemia, electrolytes disorders and respiratory symptoms started to improve 24 hours after initiating the treatment and DKA correction was finally achieved more than 48 hours after treatment was started. However, the child presented persistently reduced consciousness state and started vomiting. Brain TC scan was normal and abdomen CT scan revealed a paralytic ileus secondary to the acidosis and electrolyte unbalance (Figure 2).
Figure 2.
Abdomen CT scan showing gastric distension and paralytic ileus secondary to the acidosis and electrolyte unbalance.
Repeated enemas and placement of nasogastric tube were therefore necessary to restore bowel function and to start enteral feeding. Full neurological recovery occurred on the third day after the admission. Oral feeding and subcutaneous insulin treatment were started 3 days after admission.
Patient and caregiver had nasopharyngeal and oropharyngeal swab sampling, testing SARS-CoV-2 nucleic acid using reverse-transcriptase quantitative PCR assay, and resulted negative. Positive anti-GAD65 and anti-IA2 antibodies confirmed the diagnosis of type 1 diabetes.
Parents reported polydipsia, polyuria, and constipation two weeks before admittance.
The delay in hospitalization was related to the impossibility of leaving one’s home and to reach both the doctor’s office and the hospital during COVID19 lock-down.
Case 2
A 10 years old girl presented in the emergency department with a history respiratory distress since the last few days and polyuria, polydipsia and nocturia for 2 weeks. Recent medical history revealed fatigue with onset since at least one month, and a weight loss of 4 kg in the last 2 months. Moreover, the child was treated with topic antimycotic agent for genital candidiasis with poor response one month before the admission.
On examination, she presented with polypnea and dyspnea due to Kussmaul’s breathing and severe dehydration (skin pallor, sunken eyes, dry mucous membrane, cold extremities, capillary refill time about 3 seconds). Her heart rate was 111 ppm, her blood pressure 123/79 mmHg.
Laboratory findings on admission are summarized in Table 2 consistent with a diagnosis of moderate diabetic ketoacidosis (DKA).
Table 2.
Laboratory findings on admission for patient 2
| Parameter | Value |
| Blood glucose mg/dl | 564 |
| pH | 7,1 |
| HCO3- mmol/l | 9,4 |
| B-OH-butirrate mmol/l | 6,7 |
| Corrected sodium mmol/l | 149 |
| Corrected potassium mmol/l | 3,7 |
Intravenous fluids, insulin and potassium replacement were started according to the local protocol for the management of DKA (6).
DKA correction was achieved within 12 hours after treatment was commenced and she was the started on insulin subcutaneous treatment with a basal-bolus regimen.
Patient and caregiver had nasopharyngeal and oropharyngeal swab sampling, testing SARS-CoV-2 nucleic acid using reverse-transcriptase quantitative PCR assay, and resulted negative. Positive anti-GAD65 and anti-IA2 antibodies confirmed the diagnosis of type 1 diabetes.
Parents admitted that the danger and fear of contracting SARS-CoV-2 pandemic outbreak was responsible for the delay in the access to medical services.
Discussion
DKA represents a major cause of morbidity and mortality in young people with of type 1 diabetes at onset (7).
Despite public health interventions organised in order to prevent DKA, epidemiological data showed that its prevalence remains remarkable both in Italy and in other European countries (8, 9).
Italian data pointed out that prevalence of DKA at the onset of type 1 diabetes increased in the last few years compared to early 2010s, and that younger patients are at higher risk compared to school age children and adolescents (10).
During COVID-19 pandemic access to medical services became difficult for facilities re-organization due to conversion of some hospitals to ‘COVID hospital’ and for the reduction of public transport and related services.
Moreover, public alerts discouraged in person access to emergency departments and to general practitioner’s clinics; the majority of medical consultations were delivered by tele-medicine technology support (e.g. on the phone, via e-mail) with significative limitations for people with low socio-economic conditions or linguistic difficulties.
Reviewing the admission data of our hospital we observed a significative reduction in the number of accesses to paediatric emergency service during lock-down period compared to the same period of time in 2019, and a higher rate of hospitalizations among patients who attended paediatric emergency service, suggesting that children who were evaluated during this period presented with complex or severe conditions and required inpatient care (Table 3).
Table 3.
Number of accesses to pediatric emergency department and hospitalization rate: comparison between lock-down period and same period in 2019.
| N° of accesses 01/03/2019-31/05/2019 | N° of accesses 01/03/2020-31/05/2020 | Delta (%) |
| 5103 | 1288 | -75% |
| Hospitalization rate | Hospitalization rate | Delta (%) |
| 11,6% | 23,9% | +48,5% |
When we consider type 1 diabetes onset patients, we observed a reduction of admissions for type 1 diabetes onset during lock-down period compared to same period of 2019, with a higher prevalence of DKA.
Moreover, we did not observe any further DKA at type 1 diabetes onset in the following 3 months (Table 4).
Table 4.
Data regarding type 1 diabetes onset and DKA at onset of type 1 diabetes: comparison between lock-down period/post lock-down period in 2019 and 2020.
| Total | DKA | |
| T1D onset 01/03/19-31/05/19 | 3 | 0 |
| T1D onset 01/06/19-31/08/19 | 1 | 0 |
| T1D onset 01/03/20-31/05/20 | 2 | 2 |
| T1D onset 01/06/20-31/08/20 | 2 | 0 |
Our experience is consistent with reports from other groups (5, 10-12).
In conclusion, difficulties in transportation, fear of contracting COVID-19 and reluctance in seeking medical attention may determine a delayed access to pediatric emergency facilities. The cases herein described also underline the utmost importance of medical assessment as the parents on their own are not able to adequately discriminate the severity of a clinical condition. In the current sanitary emergency, telemedicine has suggested as a valid alternative for a first evaluation of certain conditions. However, we believe that this modality should be employed with extreme care, as the physical examination remains crucial for a correct and timely evaluation. Therefore, access to first-level healthcare in the territory should be ensured, enhanced and promoted, even for apparently “benign symptoms”, which may eventually suggest the need for an urgent hospital admission.
In addition, it is necessary, even during a pandemic outbreak, to restore educational programs addressed both to healthcare providers and to parents and caregivers regarding symptoms of type 1 diabetes onset with particular attention to infants and pre-school children who are at increased risk of DKA.
Moreover, considering the emerging possibility of a ‘second wave’ of COVID-19 pandemic, it is necessary that public opinion and healthcare practitioners provide correct information regarding access to paediatric services, in particular for children with newly onset symptoms, in order to avoid late access to emergency department in critical situations and to prevent avoidable morbidity and mortality.
Disclosure:
the Authors report no conflict of interest. For figure 1, the Authors got the parents’ permission for the inclusion of the picture of their child.
Conflict of interest
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1. Task force COVID-19 del Dipartimento Malattie Infettive e Servizio di Informatica, Istituto Superiore di Sanità. Epidemia COVID-19, Aggiornamento nazionale: 13 ottobre 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_13-ottobre-2020.pdf . [Google Scholar]
- 2.Castagnoli R, Votto M, Licari A, et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review. JAMA Pediatr. 2020;174:882–889. doi: 10.1001/jamapediatrics.2020.1467. [DOI] [PubMed] [Google Scholar]
- 3.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e901–e908. doi: 10.1016/S2214-109X(20)30229-1. doi: 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elbarbary NS, Dos Santos TJ, de Beaufort C, Agwu JC, Calliari LE, Scaramuzza AE. COVID-19 outbreak and pediatric diabetes: Perceptions of health care professionals worldwide. Pediatr Diabetes. 2020 doi: 10.1111/pedi.13084. 10.1111/pedi.13084. doi: 10.1111/pedi.13084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vanelli M, Chiarelli F. Treatment of diabetic ketoacidosis in children and adolescents. Acta Biomed. 2003;74:59–68. [PubMed] [Google Scholar]
- 7.Wolfsdorf JI, Glaser N, Agus M, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes. 2018;19:155–177. doi: 10.1111/pedi.12701. [DOI] [PubMed] [Google Scholar]
- 8.Cherubini V, Skrami E, Ferrito L, et al. High frequency of diabetic ketoacidosis at diagnosis of type 1 diabetes in Italian children: a nationwide longitudinal study, 2004-2013. Sci Rep. 2016;6:38844. doi: 10.1038/srep38844. doi: 10.1038/srep38844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Große J, Hornstein H, Manuwald U, Kugler J, Glauche I, Rothe U. Incidence of Diabetic Ketoacidosis of New-Onset Type 1 Diabetes in Children and Adolescents in Different Countries Correlates with Human Development Index (HDI): An Updated Systematic Review, Meta-Analysis, and Meta-Regression. Horm Metab Res. 2018;50:209–222. doi: 10.1055/s-0044-102090. [DOI] [PubMed] [Google Scholar]
- 10.Rabbone I, Maltoni G, Tinti D, et al. Diabetic ketoacidosis at the onset of disease during a national awareness campaign: a 2-year observational study in children aged 0-18 years. Arch Dis Child. 2020;105:363–366. doi: 10.1136/archdischild-2019-316903. [DOI] [PubMed] [Google Scholar]
- 11.Cherubini V, Gohil A, Addala A, et al. Unintended Consequences of Coronavirus Disease-2019: Remember General Pediatrics. J Pediatr. 2020;223:197–198. doi: 10.1016/j.jpeds.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Power BD, Power RF, Twomey J, Afridi Z, Neylon OM. PANDEMIC: Presentation of non-Covid cases - Delay in emergencies in children. J Paediatr Child Health. 2020 doi: 10.1111/jpc.15059. 10.1111/jpc.15059. doi: 10.1111/jpc.15059. [DOI] [PMC free article] [PubMed] [Google Scholar]


