Abstract
Coronavirus Disease (COVID-19), first emerged in Wuhan, China, in December 2019 and has now become a worldwide health emergency. The symptoms of Coronavirus vary from anosmia, fever, and cough to severe complications such as acute respiratory distress syndrome, which often require intubation and subsequent ventilation. Procedures such as these are aerosol-generating, and this adds additional challenges due to the risks posed to staff. In this brief article, we discuss the need for ventilation, risks raised to healthcare staff in this context, and ways to potentially mitigate these risks. We also discuss emerging themes, including phenotypes of COVID-19 and the role of prone positioning. (www.actabiomedica.it)
Keywords: COVID-19, critical care, anesthesiology, ventilation, intubation
Introduction
Coronavirus Disease (COVID-19), which is caused by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2), first emerged in Wuhan, China, in December 2019 as a cluster of pneumonia cases (1, 2). It has since spread at a remarkable speed and has been declared by the World Health Organisation (WHO) as a pandemic (3). As of 3rd May 2020, there have been 1,384,641 cases in the US, with 78,409 deaths. Worldwide, there have been more than 3 million confirmed cases of COVID-19 with 238,628 deaths (4). SARS-CoV-2, which causes COVID-19, is similar to the coronaviruses responsible for severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) (5). It is without a doubt that healthcare systems across the globe now face an unprecedented challenge dealing with COVID-19. There are many reasons for this, including its highly infectious nature, which can lead to infection rates of around 60-80% in a population (6). In addition, there is a multitude of clinical presentations from mild symptoms to severe illness and mortality, particularly in those with other comorbidities (7). Apart from supportive management, there are currently no definitive treatments available. There are also risks to healthcare professionals due to its human-to-human transmission (8). Anaesthetic and intensive care staff are at particularly high risk from aerosol-generating procedures such as intubation and extubation.
While our knowledge of COVID-19 is still emerging, this brief article will discuss the novel challenges faced by staff in managing this unique set of patients.
Need for intubation and invasive ventilation in COVID-19 patients
In a meta-analysis of 43 studies, including 3600 COVID-19 patients, fever was present in 83.3% of patients, cough present in 60.3%, and fatigue in 38% of patients. 25.6% of cases were severe, and the case fatality rate (CFR) was found to be 3.6% (9). The most common complication was acute respiratory distress syndrome (ARDS) (15.7%), and the incidence of this was significantly higher in older patients. Another study also found those aged over 65, those who had comorbidities and ARDS were at increased risk of death (10).
ARDS is a life-threatening acute inflammatory syndrome resulting in pulmonary edema of non-cardiac origin with associated hypoxia and pulmonary infiltrates (11).
Most patients with acute respiratory distress syndrome (ARDS) in the context of COVID-19 will require intubation and mechanical ventilation (12). In the meta-analysis by Fu et al., invasive mechanical ventilation was required in 22.2% of patients (9). However, this figure increases in those who are admitted to intensive care units (ICU). A study by Wang et al. showed this to be 47% in those admitted to an ICU in Wuhan (13), and Yang et al. reported this to be at 42% at their center (14). Therefore, it is evident that there is a demand for intubation and invasive ventilation in severely unwell COVID-19 patients.
Intubation and ventilation of COVID-19 patients present a unique challenge to anesthetists and staff working in critical care departments across the globe. Although many centers have cancelled their elective surgical lists and repurposed their theatres to prepare for the care of COVID-19 patients, there are still emergency procedures that need to occur. COVID-19, therefore, places additional pressures on already overstretched healthcare systems. It is therefore paramount that the decision to intubate and ventilate is one considered carefully by exploring patient factors, prognosis, availability of skilled staff, and risks posed to the workforce.
Risks to staff
It is known that certain procedures are more likely to generate aerosols and droplets, promoting the spread of respiratory pathogens. These procedures include the use of positive pressure non-invasive ventilation, including bilevel positive airway pressure (BiPAP) and continuous positive airway pressure (CPAP), endotracheal intubation, suction of the airway, and bronchoscopy (15). Case-control studies during previous outbreaks have shown severe acute respiratory syndrome (SARS) transmission to healthcare staff during intubation and ventilation (16, 17). A systematic review by Tran et al. showed those who performed tracheal intubations had an increased risk of being infected with SARS (odds ratio 6.6) (18). This is of relevance as a recent study showed that out of those hospitalized with COVID-19 at a single hospital in Wuhan, 29% were healthcare staff (13).
Organizations and hospitals have released new guidelines on the routine care of patients, high-risk procedures, and transfer of patients (19, 20, 21). Among these recommendations include regular handwashing, use of HEPA filters, personal protective equipment, use of video laryngoscopy, and rapid sequence induction (RSI). Extubation is also an aerosol-generating procedure requiring contact with the anesthetic team. It is likely that some individuals requiring intubation may still be infectious at the time of extubation. D’Silva et al. produced guidelines for mask-over tube extubation to help reduce the risk to staff (22). Others have recommended the use of lidocaine to help reduce coughing in these patients (23). This is supported by a systematic review that has shown fewer airway complications, including cough and sore throat, with the use of intravenous (IV) lidocaine (24). A summary of these recommendations can be seen in Figure 1.
Figure 1.
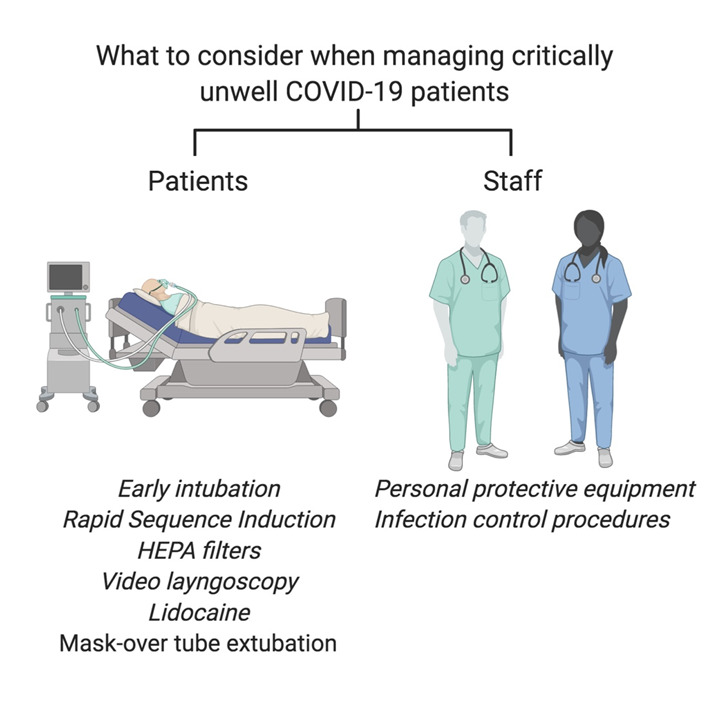
Factors to consider when managing a COVID-19 patient
Considerations for Intubating COVID-19 patients
Criteria for intubation
The decision to intubate patients with COVID-19 is complex and dependent on many factors. However, recommendations for the clinical criteria to intubate have emerged from around the world.
The Chinese Society of Anaesthesiology Task Force on Airway Management recommended that intubation be done in patients that show no improvement in respiratory distress and tachypnoea (respiratory rate greater than 30 breaths per minute), and those with poor oxygenation defined as a partial pressure of oxygen (PaO2) to fraction of inspired oxygen (FiO2) ratio less than 150 mmHg after 2 hours of high-flow oxygen therapy or non-invasive ventilation (NIV) (25). These recommendations are similar to those given in guidelines offered by the Surviving Sepsis organization who recommend that intubation be carried out when acute hypoxemic failure worsens despite conventional oxygen therapy, high flow nasal cannula (HFNC), and a trial of nasal intermittent positive pressure ventilation (26). WHO guidelines suggest that endotracheal intubation should be carried out in patients with hypoxemic respiratory failure in ARDS who continue to have increased work of breathing or hypoxemia despite standard oxygen therapy (27).
Overall, although the parameters used for definitions may differ, the consensus is to intubate in cases of acute hypoxemic respiratory failure in ARDS due to COVID-19 worsening despite standard oxygen therapy or NIV. Recommendations are, however, mostly empirical as there is little supporting evidence.
Timing of Intubation
There is little literature that addresses the timing of endotracheal intubation, but recommendations favor early intubation over late intubation. This may be, in part, explained by the fact that with disease progression in COVID-19, patients lose respiratory reserve and exhaust compensatory mechanisms (28). Yao et al. reported that intubation should be performed early on in the disease to avoid having to intubate patients with severe hypoxemia and to avoid the increased risk of cardiovascular collapse during intubation, both of which may ultimately help to reduce mortality (29). Similar recommendations were given by clinicians based in Brazil and China (30, 31). While there has been no formal evaluation of early versus late intubation in COVID-19 in comparative trials, there is evidence that supports early intubation in the case of ARDS. A prospective observational study analyzing clinical outcomes in adults with ARDS showed that late intubation was associated with a significantly higher 60-day mortality rate when compared to early intubation (56% vs. 36%, P<0.03) (32). It is thus possible that similar results would be seen in the context of intubation in COVID-19 patients.
Early intubation may also be beneficial for clinicians performing intubations who would be doing them on an elective basis rather than on an emergent basis. Given the aerosol transmission of COVID-19, intubation poses a risk to healthcare workers performing it as discussed previously. Emergent or late intubation may create an increased time pressure for clinicians that makes mistakes donning personal protective equipment (PPE) more likely, thus making the timing of intubation an issue essential both for patient and staff safety. Overall, guidance favors early intubation over late intubation both to reduce patient mortality and to ensure the safety of healthcare workers (Figure 1). However, there remains a lack of clarity over what exactly constitutes “early.”
Emerging themes
COVID-19 Pneumonia phenotypes
It is emerging that there may be different phenotypes of COVID-19. Gattinoni et al. present COVID-19 as distinct types, type L and type H. During the early phase, they report patients present with type L disease. This is characterized by low elastance, low ventilation-to-perfusion (V/Q) ratio, low lung weight, and low lung recruitability. These patients may or may not progress to become type H patients. Type H is characterized by high elastance, high right-to-left shunt, high lung weight due to ARDS progression, and high lung recruitability (33). The authors recommend identifying type L and type H patients with the use of computerized tomography (CT) scanning. Type L patients should then be treated with non-invasive options, including HFNC and CPAP. Measuring oesophageal pressure swings should be done and the need for intubation evaluated. They recommend type H patients to be treated as severe ARDS and using higher positive end-expiratory pressure (PEEP) alongside prone position and extracorporeal support (33).
Ventilatory types
To date, there has been no randomized trial comparing non-invasive ventilation (NIV) to mechanical ventilation in coronavirus related severe pneumonia. Early studies show that up to 50% of patients with COVID-19 admitted to the ICU did not subsequently require mechanical ventilation (34). It has also emerged that patients with severe disease can avoid intubation with the use of NIV (13). It is important to note that the key manifestation of such severe viral infections is the development of ARDS and the use of NIV is not usually recommended for pneumonia but may improve the oxygenation at the initial phase. Therefore, its use in COVID-19 patients remains controversial. Some studies in previous pandemics have suggested that NIV use is associated with a 92% chance of requiring intubation and mechanical ventilatory support (35). It is important to remember that there is no clear consensus supported with data from large centers and intensive care unit, and therefore modified settings should be applied on an individual basis.
Another factor to consider during ventilatory support is the recruitment of the collapsed lung due to the severity of infection, and this can be achieved through the mechanical ventilation using appropriate PEEP level. The main factor that contributes to provision of appropriate oxygenation is the mean airway pressure and therefore the appropriate level of pressure can help in reducing breathing workload, thus improving oxygenation. Some reports noted that use of a PEEP of 10 cmH2O or higher can achieve adequate oxygenation and recruitment of the lung (36). One of the larger studies including 1591 patients reported a requirement of 88% for mechanical ventilatory support with a mean PEEP of 14 (12-16) cmH2O, while only 11% achieved satisfactory oxygenation and pO2 level with NIV (37). The optimal PEEP level is still under debate. Gattinoni et al. recommend high PEEP in type H patients with high lung recruitability (33). On the other hand, Pan et al. found that patients had low recruitability with high PEEP levels (38). Similarly, a study by Roesthuis et al. reported lung compliance decreasing with higher PEEP levels. The authors propose that high PEEP may cause hyperinflation of compliant parts of the lungs as COVID-19 lesions are not recruited. Overall, they promote the use of proning and applying lower PEEP (39).
Prone positioning
The use of prone positioning has also been discussed. Prone positioning increases end-expiratory lung volume, increases chest wall elastance and improves tidal volume (40). A previous meta-analysis has shown a reduction in mortality when performed early on in the disease and recommended this to be done at least 12 hours a day (41). A more recent study evaluating the use of self-proning in awake, non-intubated patients in an emergency department showed median oxygen saturation (SpO2) at triage to be 80% and increasing to 84% with additional oxygen. This increased to 94% after 5 minutes of proning (p=0.001) (42).
COVID-19 is indeed a novel challenge and therefore, the long-term effects of proning on disease severity and mortality need to be determined.
Future Perspectives
Until the management for COVID-19 moves beyond only being conservative, it remains essential that supportive therapy is optimized to minimize mortality as much as possible. As ARDS is the most common and severe complication in patients with COVID-19, optimization of ventilatory support, in particular, is imperative (10). Current guidelines for indications and timing for intubation are based on empirical evidence; thus, there is a need for more research to be carried out. There is little information on when to extubate or stop ventilatory support in general, highlighting an additional requirement for research that can inform anaesthesiology and critical care guidelines. In the midst of this, it is also vital that the safety of healthcare workers be maintained by ensuring that as guidelines evolve in line with emerging evidence that staff safety continues to be prioritized. It is also emerging that there may be different phenotypes of COVID-19 pneumonia. This is an area which requires further study as the differences in pathophysiology should determine timing and specifics of treatment. In addition, the role of proning requires further investigation with clearer indications and timings determined for intensivists and other healthcare professionals to guide treatment.
Conclusion
Coronavirus has created unprecedented challenges for healthcare systems across the globe. This is more evident in critical care settings with older patients and those with comorbidities as these patients are more likely to have severe disease requiring admission to intensive care units. Choice of appropriate ventilatory setting and airway pressure support is crucial to provide safe care and to optimize patient outcomes. It is promising to see guidelines produced, which detail how to manage these patients medically. However, further work needs to be done to elucidate phenotypes of COVID-19 pneumonia to help guide treatment.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.World Health Organization. Pneumonia of unknown cause – China. 2020 https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ [Google Scholar]
- 2.Huang C, Wang Y, Li X, et al. Clinical Features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO pandemic WHO Director-General’s opening remarks at the media briefing on COVID19 -March 2020 [Google Scholar]
- 4.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report – 104. 2020 https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200427-sitrep-98-covid-19.pdf?sfvrsn=90323472_4 . [Google Scholar]
- 5.Xu J, Zhao S, Teng T, et al. Systematic Comparison of Two Animal-to-Human Transmitted Human Coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses. 2020;12(2):244. doi: 10.3390/v12020244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flahault A. Has China faced only a herald wave of SARS-CoV-2. Lancet. 2020;395:947. doi: 10.1016/S0140-6736(20)30521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kakodkar P, Kaka N, Baig MN. A Comprehensive Literature Review on the Clinical Presentation, and Management of the Pandemic Coronavirus Disease 2019 (COVID-19) Cureus. 2020;12(4):e7560. doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Military Med Res. 2020;7:11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect. 2020 March 15 doi: 10.1016/j.jinf.2020.03.041. (Epub ahead of print). https://doi.org/10.1016/j.jinf.2020.03.041 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 February 24 doi: 10.1016/S2213-2600(20)30079-5. (Epub ahead of print). https://doi.org/10.1016/S2213-2600(20)30079-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Umbrello M, Formenti P, Bolgiaghi L, Chiumello D. Current Concepts of ARDS: A Narrative Review. Int J Mol Sci. 2016;18(1):e64. doi: 10.3390/ijms18010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahase E. Covid-19: most patients require mechanical ventilation in first 24 hours of critical care. BMJ. 2020 doi: 10.1136/bmj.m1201. 368:m1201. [DOI] [PubMed] [Google Scholar]
- 13.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020 February 24 doi: 10.1016/S2213-2600(20)30079-5. (Epub ahead of print). https://doi.org/10.1016/S2213-2600(20)30079-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odor PM, Neun M, Bampoe S, et al. Anaesthesia and COVID-19: infection control. Br J Anaesth. 2020 March 30 doi: 10.1016/j.bja.2020.03.025. (Epub ahead of print). https://doi.org/10.1016/j.bja.2020.03.025 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raboud J, Shigayeva A, McGeer A, et al. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PLoS One. 2010;5(5):e10717. doi: 10.1371/journal.pone.0010717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fowler RA, Guest CB, Lapinsky SE, et al. Transmission of severe acute respiratory syndrome during intubation and mechanical ventilation. Am J Respir Crit Care Med. 2004;169(11):1198–202. doi: 10.1164/rccm.200305-715OC. [DOI] [PubMed] [Google Scholar]
- 18.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol Generating Procedures and Risk of Transmission of Acute Respiratory Infections to Healthcare Workers: A Systematic Review. PLoS One. 2012;7(4):e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Association of Anaesthetists. Anaesthetic Management of Patients During a COVID-19 Outbreak. 2020 https://anaesthetists.org/Home/Resources-publications/Anaesthetic-Management-of-Patients-During-a-COVID-19-Outbreak . [Google Scholar]
- 20.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth/J Can Anesth. 2020;67:568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brewster DJ, Chrimes NC, Do TBT, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust. 2020 April 1 doi: 10.5694/mja2.50598. (Epub ahead of print). https://www.mja.com.au/journal/2020/consensus-statement-safe-airway-society-principles-airway-management-and-tracheal . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D’Silva DF, McCulloch TJ, Lim JS, Smith SS, Carayannis D. Extubation of patients with COVID-19. Br J Anaesth. 2020 March 16 doi: 10.1016/j.bja.2020.03.016. (Epub ahead of print). https://doi.org/10.1016/j.bja.2020.03.016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aminnejad R, Salimi A, Saeidi M. Lidocaine during intubation and extubation in patients with coronavirus disease (COVID-19) Can J Anesth/J Can Anesth. 2020 March 16 doi: 10.1007/s12630-020-01627-2. (Epub ahead of print). https://doi.org/10.1007/s12630-020-01627-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang SS, Wang NN, Postonogova T, et al. Intravenous lidocaine to prevent postoperative airway complications in adults: a systematic review and meta-analysis. Br J Anaesth. 2020;124:314–23. doi: 10.1016/j.bja.2019.11.033. [DOI] [PubMed] [Google Scholar]
- 25.Zuo M, Huang Y, Ma W, et al. Chinese Society of Anesthesiology Task Force on Airway Management: Expert Recommendations for Tracheal Intubation in Critically ill Patients with Noval Coronavirus Disease 2019. Chin Med Sci J. 2020 February 27 doi: 10.24920/003724. (Epub ahead of print). https://doi.org/10.24920/003724 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poston JT, Patel BK, Davis AM. Management of Critically Ill Adults With COVID-19. JAMA. 2020 March 26 doi: 10.1001/jama.2020.4914. (Epub ahead of print). https://doi.org/10.1001/jama.2020.4914 . [DOI] [PubMed] [Google Scholar]
- 27.World Health Organisation (WHO) Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim Guidance. 2020 https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf . [Google Scholar]
- 28.Meng L, Qui H, Wan L, et al. Intubation and Ventilation amid the COVID-19 Outbreak: Wuhan’s Experience. Anesthesiology. 2020 March 26 doi: 10.1097/ALN.0000000000003296. (Epub ahead of print). https://doi.org/10.1097/ALN.0000000000003296 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yao W, Wang T, Jiang B, et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J of Anaesth. 2020 March 31 doi: 10.1016/j.bja.2020.03.026. (Epub ahead of print). https://doi.org/10.1016/j.bja.2020.03.026 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mendes JJ, Mergulhão P, Froes F, Paiva JA, Gouveia J. Recommendations from the Sociedade Portuguesa de Cuidados Intensivos and Infection & Sepsis Group for intensive care approach to COVID-19. Rev Bras Ter Intensive. 2020;32(1):2–10. doi: 10.5935/0103-507X.20200002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheung JCH, Ho LT, Cheng JV, Cham EYK, Lam KN. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020;8(4):e19. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kangelaris KN, Ware LB, Wang CY, et al. Timing of Intubation and Clinical outcomes in Adults with ARDS. Crit Care Med. 2016;44(1):120–129. doi: 10.1097/CCM.0000000000001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06033-2. https://doi.org/10.1007/s00134-020-06033-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meng L, Qiu H, Wan L, et al. Intubation and ventilation amid the COVID-19 outbreak: wuhan’s experience. Anesthesiol. 2020 doi: 10.1097/ALN.0000000000003296. published online March 26. DOI:10.1097/ALN.0000000000003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alraddadi BM, Qushmaq I, Al-Hameed FM, et al. Non-invasive ventilation in critically ill patients with the Middle East respiratory syndrome. Influenza Other Respir Viruses. 2019;13:382–390. doi: 10.1111/irv.12635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McEnery T, Gough C, Costello RW. COVID-19: Respiratory support outside the intensive care unit [published online ahead of print, 2020 Apr 9] Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30176-4. S2213-2600(20)30176-4. doi:10.1016/S2213-2600(20)30176-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grasselli G, Zangrillo A, Zanella A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy [published online ahead of print, 2020 Apr 6] JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. doi:10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pan C, Chen L, Lu C, Zhang W, Xia JA, Sklar MC, Du B, Brochard L, Qiu H. Lung Recruitability in SARS-CoV-2 Associated Acute Respiratory Distress Syndrome: A Single-center, Observational Study. Am J Respir Crit Care Med. 2020 doi: 10.1164/rccm.202003-0527LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roesthuis L, van den Berg M, van der Hoeven H. Advanced Respiratory Monitoring in COVID-19 Patients: Use Less PEEP! Preprints. 2020 doi: 10.1186/s13054-020-02953-z. 2020040275 (doi: 10.20944/preprints202004.0275.v1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kallet R. A Comprehensive Review of Prone Position in ARDS. Respiratory Care. 2015;60(11):1660–1687. doi: 10.4187/respcare.04271. [DOI] [PubMed] [Google Scholar]
- 41.Mora-Arteaga J, Bernal-Ramírez O, Rodríguez S. The effects of prone position ventilation in patients with acute respiratory distress syndrome A systematic review and metaanalysis. Medicina Intensiva (English Edition) 2015;39(6):359–72. doi: 10.1016/j.medin.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 42.Caputo N, Strayer R, Levitan R. Early Self-Proning in Awake, Non-intubated Patients in the Emergency Department: A Single ED’s Experience during the COVID-19 Pandemic. Academic Emergency Medicine. 2020 doi: 10.1111/acem.13994. doi:10.1111/acem.13994. [DOI] [PMC free article] [PubMed] [Google Scholar]


