Abstract
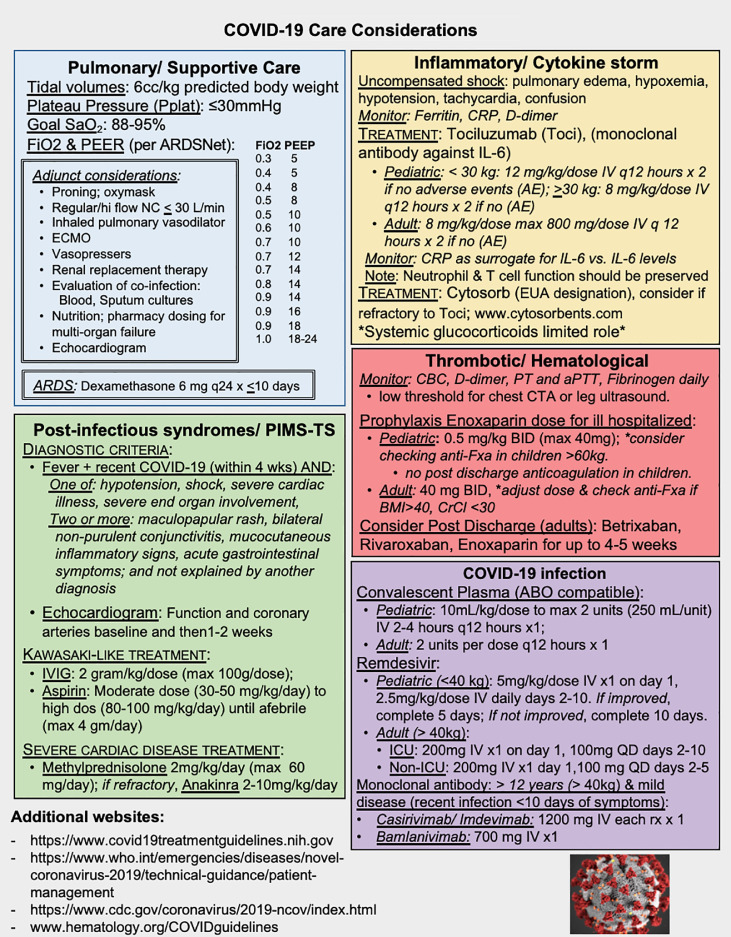
As we pass the nearly 9 month mark of the coronavirus virus disease 2019 (COVID-19) pandemic in the United States, we sought to compile a brief multi-disciplinary compendium of COVID-19 information learned to date. COVID-19 is an active viral pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that confers high morbidity and mortality. COVID-19 has been associated with: pulmonary compromise and acute respiratory distress syndrome, thrombotic events, inflammation and cytokine, and post-infectious syndromes. Mitigation of these complications and expeditious therapy are a global urgency; this is brief summary of current data and management approaches synthesized from publications, experience, cross-disciplinary expertise (Figure 1).
Key Words: COVID-19, compendium, treatment guidance
Pulmonary and Supportive Care
Progressive COVID-19 requires critical care. Priorities include appropriate personal protective equipment, negative-pressure rooms, and minimization of particle aerosolization: regular- or high-flow nasal cannula (limited to ≤30 L/minute), oxygen mask, and in very select cases a trial of noninvasive ventilation [1]. Progressive failure necessitates safe endotracheal intubation by experienced providers and lung-protective mechanical ventilation (high positive end-expiratory pressure and low tidal volumes), with adjunct therapies including proning, inhaled pulmonary vasodilators, extracorporeal membrane oxygenation, vasopressors, nutrition, and renal replacement therapy. Safe and expedient extubation must be prioritized in patients with successful spontaneous breathing trials [1]. Adult respiratory distress syndrome (ARDS) is a life-threatening complication, with data suggesting that low-dose, short-term dexamethasone therapy may have a critical role [2]. Cardiac complications, including myocarditis, heart failure, and arrhythmias, are being increasingly recognized in COVID-19; thus, cardiac evaluation is recommended in children and adults with severe disease. Additional risks of ulcers, thrombi, and fluid overload should be minimized. Evaluation for coinfections is warranted, as data have shown that bacterial and fungal pathogens contribute to mortality, and some have suggested therapy with empiric antimicrobials [1].
Figure 1.
COVID-19 care considerations.
COVID-19 Treatment
Two therapies continue to show promise for primary treatment of COVID-19. Convalescent plasma—plasma containing antibodies to SARS-CoV-2, obtained from individuals who have recovered from COVID-19—has a good safety record, data to suggest efficacy in severe disease, and recently received emergency use authorization (EUA) from the Food and Drug Administration for use in COVID-19 [3]. Studies in children and adults are ongoing, with the best results anticipated in patients who receive products with high neutralization titers. To date, the most encouraging antiviral agent is remdesivir, with some data linking it to decreased time to recovery in adults [4]. Antiviral treatment is likely most effective earlier in the illness (days 0 to 7) when there is active viral replication. It has been given emergency use authorization for the treatment of SARS-Co-V-2 in hospitalized adult and pediatric patients with severe disease. Emerging data suggests that monoclonal antibody therapy to SARS-COV2 may mitigate severe disease in outpatients early in the disease process, with either casirivimab and imdevimab or bamlanivimab (under an EUA) [5,6].
Coagulopathy and Bleeding Diathesis
SARS-CoV-2 infection predisposes patients to venous and arterial thrombosis, due to excessive inflammation, platelet activation, endothelial dysfunction and stasis [7]. Venous thromboembolism incidence risk is associated with disease severity, ≤70% in intensive care patients [7]. Bleeding diatheses also occur in up to 5% of patients with COVID-19 and can be accompanied by hypofibrinogemia [7]. To risk stratify, follow coagulation and hematology labs daily. Intermediate dose prophylaxis should be considered in ill patients, using anti-FXa to evaluate resistance and adjust dosage, including those on therapeutic dosing [7]. Careful consideration of changing renal function, thrombocytopenia, and impact of BMI on dosing of anticoagulation. Consider a very low threshold for chest computer tomography angiography, venous ultrasound. In ill adults, post-discharge thromboembolism prophylaxis could be considered for up to 4-5 weeks.
Inflammation/Cytokine Storm
Severe COVID-19 may present with life-threatening, uncompensated shock similar to cytokine release or macrophage activation syndromes with elevated ferritin, C-reactive protein, and d-dimers. Hallmarks include lymphopenia, elevated IL-6, and TNF-α. Tociluzumab, an IL-6 antagonist, has shown survival benefit in the treatment of COVID-19 without affecting viral clearance [8]. This may be especially important for immunocompromised patients, such as after cellular transplantation [9]. In contrast, the risks of secondary infections have cautioned against systemic steroids in patients who do not have ARDS. For patients refractory to tocilizumab, a method for in-line cytokine removal, CytoSorb, has received an EUA for adults, although data remain limited.
Postinfectious Syndromes
Postinfectious syndromes such as Guillain-Barré and a severe multisystem disease inflammatory syndrome in children (MIS-C; also called pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2) are emerging. MIS-C is characterized by fever with one of the following: hypotension or shock, severe cardiac illness, and severe end-organ involvement; or 2 or more of the following: maculopapular rash, bilateral nonpurulent conjunctivitis, mucocutaneous inflammatory signs, acute gastrointestinal symptoms; and not explained by another diagnosis [10]. Echocardiography should be performed at presentation and repeated in 1 to 2 weeks. Treatment includes supportive care along with consideration of immunomodulation with, for example, steroids and i.v. immunoglobulin, with uncommon use of IL-1 and Il-6 inhibitors, and anticoagulation [10].
This perspective is not a guideline but provides a brief summary of current considerations for the care of patients with COVID-19, including details of pulmonary and intensive care management, and specific treatments for severe disease, coagulopathy, dysregulated inflammation, and postinfectious syndromes. The care of COVID-19 patients is a rapidly evolving field that will require continued collaborations across disciplines and age groups to best care for these patients and improve outcomes, as highlighted by the patient synopsis.
ACKNOWLEDGMENTS
Financial disclosure: There is no funding to report.
Conflict of interest statement: All authors have no relevant conflict of interest for this work. A.L.A. has served as an HIV expert on the scientific advisory board of Gilead Sciences and on an expert advisory panel and as a consultant for Merck Pharmaceuticals for HIV therapies. Searches for institutional funding from Gilead (remdesivir) and Roche (Tociluzumab) revealed only that Emory University received a COMPASS grant from Gilead for HIV therapies. No known monetary compensation from industry related to COVID-19 is forthcoming to the hospitals/authors listed herein.
Authorship statement: All authors contributed to the generation of the manuscript, editing, and final review. K.M.W. initially crafted the outline of the manuscript and the panel of individuals to be included, which was further broadened by those individuals’ subsequent invitations. .J.H.-C. and A.L.A. contributed equally to this work.
Footnotes
Financial disclosure: See Acknowledgments on page 474.e3.
REFERENCES
- 1.Poston JT, Patel BK, Davis AM. Management of critically ill adults with COVID-19. JAMA. 2020;323:1839–1841. doi: 10.1001/jama.2020.4914. [DOI] [PubMed] [Google Scholar]
- 2.Horby P, Lim WS, Emberson JR, RECOVERY Collaborative Group Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li L, Zhang W, Hu Y, et al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial. JAMA. 2020;324:460–470. doi: 10.1001/jama.2020.10044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19: final report. N Engl J Med. 2020;383:1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gottlieb RL, Nirula A, Chen P, et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA. 2021;325:632–644. doi: 10.1001/jama.2021.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinreich DM, Sivapalasingam S, Norton T, et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med. 2021;384:238–251. doi: 10.1056/NEJMoa2035002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Samkari H, Karp Leaf RS, Dzik WH, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020;136:489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salama C, Han J, Yau L, et al. Tocilizumab in patients hospitalized with Covid-19 pneumonia. N Engl J Med. 2021;384:20–30. doi: 10.1056/NEJMoa2030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma A, Bhatt NS, St Martin A, et al. Clinical characteristics and outcomes of COVID-19 in haematopoietic stem-cell transplantation recipients: an observational cohort study. Lancet Haematol. 2021;8:185–193. doi: 10.1016/S2352-3026(20)30429-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem inflammatory syndrome in US children and adolescents. N Engl J Med. 2020;383:334–346. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]