To the Editor,
The SARS-CoV-2 coronavirus pandemic, which emerged in Wuhan1 (China) several months ago, has led to the collapse of health care in many countries around the world, including Spain. Since the beginning of the pandemic, Spanish dermatologists have been warning of the risk of a delay in the diagnosis of melanomas as a consequence of the lockdown following the state of alarm.2, 3 The objective of this study was to evaluate the impact of the pandemic on the detection and early diagnosis of new cases of melanoma, as well as identifying the differential clinical presentation characteristics compared to the pre-COVID period.
A retrospective cross-sectional study was carried out in which the new cases of primary cutaneous melanoma (PCM) registered during the period from April to August 2020 diagnosed at the Costa del Sol Hospital were compared with the same period of the previous year. Data were extracted from the anatomical pathology skin cancer registry. Epidemiological (sex, age) and clinicopathological (location, tumour thickness, ulceration, mitosis) characteristics were evaluated. A descriptive analysis was performed using location measurements and frequency distribution. The Chi-square test and the Mann–Whitney U test were used to compare differences. Significant primary outcome variables were expressed as odds ratio (OR) with their respective 95% confidence intervals (95% CI). The level of statistical significance was established in p < 0.05.
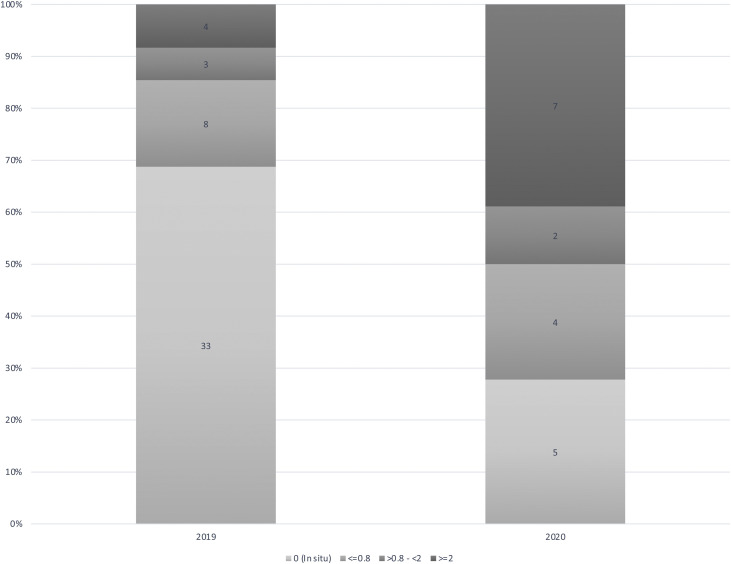
During the period from April to August 2019, 48 new cases of PCM were identified, which represents a cumulative incidence of 28 per 100,000 inhabitants (95% CI: 23.2–33.7), compared to 18 cases diagnosed in the same period of months in 2020, which means a cumulative incidence of 10.2 per 100,000 inhabitants (95% CI: 7.4–13.8), with significant differences between both periods (p < 0.001). There were no differences between periods in relation to sex, nor differences in relation to age. The most common anatomical location of melanomas diagnosed in 2019 was the trunk (45.8%), while in 2020 the most common location was the head (47.4%) (p = 0.089). In terms of the histopathological characteristics of the tumours, in 2019, 68.8% of the cases were melanomas in situ and 8.3% were melanomas over 2 mm in thickness, while in the same period of 2020, 27.8% were melanomas in situ and 38.9% melanomas over 2 mm in thickness (p = 0.001) (Fig. 1 ). The risk of presenting a thick melanoma in 2020 patients compared to 2019 obtained a odds ratio of 7 (95% CI: 1.7–28.2). When analysing other histopathological findings, 7.1% of melanomas showed ulceration in the 2019 period compared to 21.4% during the 2020 period (p = 0.596) and 42.9% showed mitosis in the 2019 period compared to 75% during the 2020 period (p = 0.209).
Fig. 1.
In 2019, 33 cases were melanomas in-situ and 4 melanomas over 2 mm in thickness, while in 2020, 5 cases were melanomas in-situ and 7 were melanomas over 2 mm in thickness.
The main finding observed is the significant decrease in new diagnoses of PCM during the pandemic, compared to the same period in 2019 (62%). This decline in diagnosis has rested primarily on in situ. There has also been an exponential increase in the diagnosis of thick melanoma compared to the same period in 2019, with a 7-fold increased risk of having a thick melanoma during the pandemic (OR: 7). Thick melanoma also carries with it the presence of other predictors of poor prognosis, such as location on the head, ulceration, and the presence of mitosis, although there was no statistical significance when comparing these findings with those of the 2019 period. This increase in the diagnosis of thick melanomas has implications not only for survival, but also for the associated healthcare costs, which include imaging tests for staging and follow-up, as well as adjuvant treatment.
The compulsory lockdown of the population throughout the national territory during the state of alarm, the fear of contagion and the difficulties of access to primary care as a result of the collapse of health services have likely been determining factors causing patients not to go to hospital or to do so with delay. Therefore, it is essential to restore face-to-face primary care and reduce accessibility barriers to the specialist using effective and efficient telematic tools such as teledermatology.4, 5
Footnotes
Please cite this article as: Fernández Canedo MI, de Troya Martín M, Rivas Ruíz F. Impacto de la pandemia SARS-CoV-2 en el diagnóstico precoz del melanoma. Med Clin (Barc). 2021;156:356–357.
References
- 1.Phelan A., Katz R., Gostin L. The novel coronavirus originating in Wuhan, China: challenges for Global Health Governance. JAMA. 2020;323:709. doi: 10.1001/jama.2020.1097. [DOI] [PubMed] [Google Scholar]
- 2.Tejera A., Nagore E. Estimated effect of COVID-19 lockdown on melanoma thickness and prognosis: a rate of growth model. J Eur Acad Dermatology Venereol. 2020;34:351–352. doi: 10.1111/jdv.16555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tejera A., Cañueto J., Toll A., Santos-Juanes J., Jaka A., Ferrándiz C., et al. Estimación del efecto en el tamaño y la supervivencia de los tumores cutáneos debido al confinamiento por COVID-19: modelo basado en un crecimiento exponencial. Actas Dermosifiliogr. 2020;111:629–638. doi: 10.1016/j.ad.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moreno D., Ferrándiz L., Nieto A., Carrasco R., Moreno P., Galdeano R., et al. Store-and-forward teledermatology in skin cancer triage. Experience and evaluation of 2009 teleconsultations. Arch Dermatol. 2007;143:479–484. doi: 10.1001/archderm.143.4.479. [DOI] [PubMed] [Google Scholar]
- 5.Millán J.F., Herrera R., Rivas F., García P., García P., Pozo F., et al. Impact of a community intervention for early skin cancer diagnosis implementing teledermatology. Acta Dermatovenerol Croat. 2020;28:75–79. [PubMed] [Google Scholar]