Abstract
As the coronavirus disease 2019 pandemic continues to impact hospital systems both in the United States and throughout the world, it is important to understand how the pandemic has impacted the volume of hospital admissions. Using the Vizient Inc (Chicago, IL) clinical databases, we analyzed inpatient hospital discharges from the general medicine service and its subspecialty services including cardiology, neonatology, pulmonary/critical care, oncology, psychiatry, and neurology between December 2019 and July 2020. We compared baseline discharge data to that of the first six months of the pandemic, from February to July 2020. We set the baseline as discharges by specialty from February 2019 through January 2020, averaged over the 12 months. Compared to baseline, by April 2020 the volume of general medicine hospital discharge was reduced by -20.2%, from 235,581 to 188,027 discharges. We found that while overall the number of discharges decreased from baseline, with a nadir in April 2020, pulmonary/critical care services had an increase in hospital discharge volume throughout the pandemic, from 7534 at baseline to 15,792 discharges in April. These findings are important for understanding health care use during the pandemic and ensuring proper allocation of resources and funding throughout the coronavirus disease 2019 pandemic.
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019
The coronavirus disease 2019 (COVID-19) pandemic continues to be a global threat. At the height of the pandemic in the United States, there was a widespread reduction in emergency department visits and hospitalization for medical and surgical services.1 The aim of this study was to determine the impact of the pandemic on the volume of hospital discharges from general medicine and its subspecialty services.
Methods
The Vizient Inc (Chicago, IL) clinical database was analyzed for inpatient hospital discharges from the general medicine service and its subspecialty services including cardiology, neonatology, pulmonary/critical care, oncology, psychiatry, and neurology between February 2019 and July 2020. The Vizient clinical database is comprised of administrative, clinical, and financial inpatient information of index hospitalizations at academic centers and their affiliates in the United States. Hospital discharge volumes and patient demographics were analyzed at baseline and monthly thereafter during the pandemic, beginning February 1, 2020. Baseline data were defined as the mean hospital discharge volumes among services from February 2019 through January 2020. Using International Classification of Diseases, Tenth Revision, Clinical Modification diagnosis code for COVID-19 (U07.1), the proportion of hospital discharges related to COVID-19 was calculated for the general medicine and pulmonary/critical care services. Analysis was performed using χ2 tests to compare demographic factors related to lower volume of hospitalization. Approval for the use of the Vizient patient-level data in this study was obtained from Vizient, as well as approval and waiver of consent from the Institutional Review Board of the University of California, Irvine Medical Center, as exempted status for this analysis of a de-identified national database.
Results
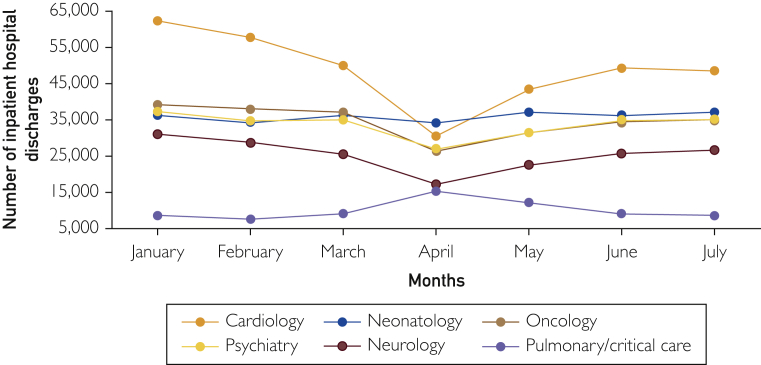
Our search resulted in discharge information from 615 US academic centers and their affiliates across 50 states. Volume of hospital discharges from general medicine and its subspecialty services decreased from baseline beginning in March 2020 with the maximum reduction in April 2020. Compared to baseline, by April 2020, the volume of general medicine hospital discharge was reduced by 20.2%, from 235,581 to 188,027 discharges (Table 1). For medicine subspecialty services, cardiology and neurology had the greatest reduction of hospital discharges, -49.4% and -42.9%, respectively; oncology and psychiatry had a moderate reduction in discharge volumes, -20.3% and -26.8%, respectively; and neonatology was the least impacted at -7.7% (Figure). However, pulmonary/critical care service had an increase in hospital discharge volume from 7534 at baseline to 15,792 discharges in April (+52.3%). For the month of April, 59.9% of the hospital discharges from pulmonary/critical care service and 27.6% of the discharges from general medicine service were for COVID-19 treatments. Demographic factors contributing to a lower volume of hospitalization during the pandemic include female gender and white ethnicity (P<.05) (Table 2). All medicine services had a recovery of discharge volume toward baseline starting in the month of May. By July 2020, the volume of hospital discharge for pulmonary critical care was +19.0% of baseline whereas cardiology and neurology discharge volume still lagged behind at -15.5% and -9.8%, respectively.
Table 1.
Number of In-Patient Hospital Discharges and Percentage Change From Baseline (February 2019 Through February 2020 Averaged Over 12 Months) for March Through July 2020 for General Medicine and its Subspecialty Servicesa
| Medicine service line | Pre-pandemic baseline | Pandemic |
||||
|---|---|---|---|---|---|---|
| March |
April |
May |
June |
July |
||
| n (% change) | n (% change) | n (% change) | n (% change) | n (% change) | ||
| General medicine, n | 235,581 | 221,622 (-5.9) | 188,027 (-20.2) | 195,506 (-17.0) | 201,819 (-14.3) | 220,379 (-6.5) |
| Cardiology, n | 60,501 | 51,284 (-15.2%) | 30,605 (-49.4%) | 43,246 (-28.5%) | 49,097 (-18.8%) | 51,182 (-15.5%) |
| Oncology, n | 39,350 | 37,337 (-5.1) | 31,365 (-20.3) | 31,518 (-19.9) | 34,393 (-12.6) | 36,232 (-7.9) |
| Psychiatry, n | 37,529 | 35,897 (-4.3) | 27,479 (-26.8) | 31,489 (-16.1) | 34,929 (-6.9) | 36,361 (-3.1) |
| Neonatology, n | 37,502 | 37,066 (-1.1) | 34,602 (-7.7) | 37,033 (-1.3) | 35,969 (-4.1) | 39,900 (+6.0) |
| Neurology, n | 31,052 | 26,168 (-15.7) | 17,739 (-42.9) | 22,513 (-27.5) | 25,753 (-17.1) | 27,996 (-9.8) |
| Pulmonary/critical care, n | 7,534 | 9,398 (+19.8) | 15,792 (+52.3) | 12,076 (+37.6) | 9075 (+17.0) | 9301 (+19.0) |
| Mortality | 2.6% | 3.0% (+0.4) | 5.8% (+3.2) | 3.5% (+0.9) | 2.6% (+0) | 2.6% (+0) |
| COVID-19 cases | 0 (0%) | 0 (0)b | 51,879 (+27.6) | 30,305 (+15.5) | 17,795 (+8.8) | 27,442 (+12.5) |
COVID-19, coronavirus disease 2019.
COVID-19 testing availability was very limited in March 2020.
Figure.
Inpatient hospital discharges from medicine subspecialty services at US academic centers and their affiliates according to months before and during the pandemic, excluding general medicine service.
Table 2.
Summary of Demographics and Characteristics of Hospitalized Patients Pre-Pandemic (April–June 2019) and During the Pandemic (April–June 2020)a
| Demographics and characteristics | Pre-pandemic (n=703,357) | Pandemic (n=585,352) | P∗ |
|---|---|---|---|
| Sex | |||
| Male | 339,347 (48.2) | 295,228 (50.4) | <.001 |
| Female | 363,982 (51.7) | 290,087 (49.6) | <.001 |
| Age group, years | |||
| ≤65 | 392,648 (55.8) | 329,440 (56.3) | <.001 |
| >65 | 310,709 (44.2) | 255,912 (43.7) | <.001 |
| Race/ethnicity | |||
| Caucasian | 470,187 (66.8) | 366,195 (62.6) | <.001 |
| African American | 141,927 (20.2) | 129,667 (22.2) | <.001 |
| Asian | 16,924 (2.4) | 14,618 (2.5) | <.001 |
| Other | 74,319 (10.6) | 74,872 (12.8) | <.001 |
Values shown are n (%).
Discussion
The COVID-19 pandemic led to a precipitous reduction in the volume of hospitalization through the general medicine and its subspecialty services. The peak of this reduction occurred in the month of April. The reason for this decline has been shown to be attributed to reduction in hospitalizations and COVID-19–related fear, which prohibits patients from obtaining treatment or hospitalization for their medical conditions.2 Of the medicine subspecialties, cardiology was most impacted whereas neonatology was the least impacted, likely related to continued medical necessity for hospitalization for care of the neonates. We can surmise that the down-trend in discharges from pulmonary critical care subspecialty after the April peak is related to 1) increase in contribution to the care of COVID-19 patients from general hospitalist team; and 2) the downward trend in acute critical care COVID-19 patients after the initial surge. Reduction in hospitalization and avoidance of medical care during the pandemic has been shown to be detrimental with an excess of cardiovascular deaths including heart disease and diabetes and a negative financial impact on the US healthcare system.3, 4, 5, 6 In this study, factors associated with reduction in hospitalization during the pandemic included female gender and white ethnicity.
Conclusion
In contrast to all other medicine subspecialties, volume of hospital discharges for the pulmonary/critical care service almost doubled that of baseline during the height of the pandemic as general medicine and pulmonary/critical care were the main two services caring for hospitalized COVID-19 patients. Not only did the reduction in hospitalization during the pandemic lead to a detrimental impact on patients requiring urgent and timely care, it has also led to a negative financial impact on the health care system in the United States.
Acknowledgment
The information contained in this article was based on the Vizient Inc clinical database. This study received no funding.
Footnotes
Potential Competing Interests: Dr Amin reported serving as principal investigator or co-investigator of clinical trials sponsored by NIH/NIAID, NeuroRx Pharma, Pulmotect, Blade Therpeutics, Novartis, Takeda, Humanigen, Eli Lilly, PTC Therapeutics, Octapharma, Fulcrum Therapeutics, Alexion; and he has served as speaker and/or consultant for BMS, Pfizer, BI, Portola, Sunovion, Mylan, Salix, Alexion, AstraZeneca, Novartis, Nabriva, Paratek, Bayer, Tetraphase, Achogen LaJolla, Millenium, Ferring, PeraHealth, HeartRite, Aseptiscope, and Sprightly. Dr Nguyen reported serving as a speaker for Olympus and Endogastric Solutions.
The remaining authors report no potential competing interests.
References
- 1.Hartnett K.P., Kite-Powell A., DeVies J., et al. Imapct of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Czeisler M.E., Marynak K., Clarke K.E.N., et al. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu J., Mamas M.A., Mohamed M.O., et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107(2):113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 4.Woolf S.H., Chapman D.A., Sabo R.T., et al. Excess deaths from COVID-19 and other causes, March–April 2020. JAMA. 2020;324(5):510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Best M.J., McFarland E.G., Anderson G.F., Srikumaran U. The likely economic impact of fewer elective surgical procedures on US hospitals during the COVID-19 pandemic. Surgery. 2020;168(5):962–967. doi: 10.1016/j.surg.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khullar D., Bond A.M., Schpero W.L. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127–2128. doi: 10.1001/jama.2020.6269. [DOI] [PubMed] [Google Scholar]