Abstract
The inter-relationship between chronic respiratory disease and reflux disease in the airway reflux paradigm is extremely complex and remains poorly characterised. Reflux disease is reported to cause or contribute to the severity of a number of respiratory tract diseases including laryngeal disorders, sinusitis, chronic cough, asthma, COPD, idiopathic pulmonary fibrosis, cystic fibrosis, bronchiectasis and bronchiolitis obliterans post lung transplant. It is now appreciated that reflux disease is not simply caused by liquid acid reflux but rather by a variety of chemical refluxates originating from the stomach and duodenum due to a number of different mechanisms. Reflux disease can be challenging to diagnose, particularly proving its role in the causation of direct respiratory epithelial damage. Significant advances in oesophageal assessment and gastric biomarkers have emerged in recent years as our understanding increases. There are a number of treatments available for reflux disease, both medical and surgical, but there is a paucity of large randomised trials to evaluate their efficacy in the setting of chronic respiratory disease. Everyday clinical practice, however, informs us that treatment failure in reflux disease is common. This clinical review summarises associations between reflux disease in the setting of chronic respiratory diseases and examines available evidence regarding potential therapeutic strategies.
Short abstract
Gastro-oesophageal reflux disease is prevalent among patients with chronic respiratory disease. A number of medical and surgical treatment options are available for GORD. This review examines available evidence in the setting of chronic lung disease. https://bit.ly/34TcMJS
Introduction
Gastro-oesophageal reflux (GOR) is a normal physiological event in healthy individuals, referring to the involuntary passage of gastric contents into the oesophagus [1, 2]. Gastro-oesophageal reflux disease (GORD) comprises symptoms or end-organ complications resulting from the reflux of gastric contents into the oesophagus, or beyond into the oral cavity, larynx or lung – a process termed extra-oesophageal reflux (EOR) [3]. The classical definition of GORD refers to liquid acid reflux defined by 24-h pH monitoring with most epidemiological studies of GORD referring to this phenomenon.
Typical GORD has been shown to affect up to a third of the normal population causing symptoms, mucosal damage and potentially malignant transformation of the epithelium in the oesophagus [4]. Oesophageal symptoms include epigastric pain, heartburn, odynophagia, gaseous reflux, acid and non-acid tasting reflux, dysphagia, epigastric pain and sleep disturbance [3, 5, 6]. Therefore, it is necessary to establish temporal relationships between GORD symptoms with food, posture and stress [7]. The prevalence of GORD could also be increasing due to the obesity epidemic, eating larger meals, greater ingestion of reflux-provoking food-stuffs (e.g. carbonated drinks, chocolate, caffeine, spiced foods and alcohol), an increase in the prevalence of hiatal hernias (HH) and an increasingly aged population [4]. Symptoms from EOR are frequently not inquired about by physicians or offered by patients and can include peri-prandial or persistent cough (laryngeal irritation), dysphonia, globus, laryngitis, sinusitis, metallic taste, dental caries and halitosis [8].
In recent years, however, the concept of airways reflux, which consists of neither acid nor liquid reflux but rather a gaseous mist containing mainly non-acid components, has become widely established, with 24-h pH–impedance studies now the gold standard investigation of choice for the same. pH impedance quantifies the type, number, phase, duration and proximal extent of each reflux episode [9–11]. Airways reflux may be entirely asymptomatic, and gaseous or mixed reflux may be as pathogenic to the oesophagus, oropharynx and upper and lower respiratory tract as liquid acid reflux [6, 9, 12–15]. It is also increasingly recognised that the refluxate may also be from the duodenum and contain bile acids, which again can be very pro-inflammatory and have been associated with changes in the gut microbiome [16].
The nomenclature remains confusing with GOR considered to be a normal physiological process and GORD a disease caused by pathological GOR. Does GOR refer only to the involuntary passage of liquid acid contents or does it encompass all potential gastric contents? Should airways reflux be considered under the same umbrella term of GORD if it contributes to a disease process comprising symptoms or end-organ complications? Airways reflux is more likely to contribute to extra-oesophageal reflux disease (EORD) caused by EOR, which can consist of liquid acid reflux (typical GORD) or gaseous non-acid reflux (airways reflux). In this review, therefore, reflux disease is the overarching term that refers to symptoms or end-organ complications resulting from the reflux of gastric contents into the oesophagus, or beyond, into the oral cavity, larynx or lung by any mechanism including typical GORD, airways reflux and micro-aspiration.
In the last decade there has been a huge interest in the role of reflux disease in the pathogenesis of a number of chronic airway and parenchymal lung diseases. Given the potential for reflux disease and chronic respiratory disease to act in a bidirectional manner with reflux disease driving respiratory disease and respiratory mechanics contributing to reflux disease, it is important to better understand the relationship and possible consequences of these conditions coexisting. The purpose of this review is to provide a summary of what is currently known about aerodigestive disease in terms of what causes reflux disease, individual respiratory diseases linked with reflux disease, and treatment of reflux disease with a proposed diagnostic and management approach. Very little of our current clinical practice in this area is evidence-based, and there is therefore inevitably a degree of informed speculation.
What causes reflux disease?
In health, reflux is prevented through the combined action of the components of the anti-reflux barrier comprising the lower oesophageal sphincter (LOS), the crural diaphragm and the anatomical flap valve [5]. Initial research suggested that the most common cause of reflux was an excess of transient relaxations of the LOS, although it has since been demonstrated that patients with reflux disease are more likely to have acid reflux associated with these transient relaxations. Reflux disease is viewed as a multifactorial disorder with risk factors including genetic predisposition, lifestyle, body habitus, anatomical variation and presence of comorbid conditions and their treatment [1, 5, 17].
The strongest risk factor for reflux disease is the presence of a hiatal hernia where the integrity of the LOS is lost, and the acid pocket normally seen in the gastric fundus sits directly below the LOS [18]. A critical function of the LOS is to prevent reflux when recumbent. The presence of a hiatal hernia compromises this essential function promoting GORD, EOR and potentially micro-aspiration. Recent data suggest that the presence and size of a hiatal hernia influence clinical presentation, oesophageal function, reflux profile and the degree of mucosal injury [18]. Hiatal hernias are more common with age, probably due to connective tissue change and, in particular, in centrally obese subjects due to raised gastric pressure. It is likely that the failure of multiple anatomical or physiological protective anti-reflux mechanisms, rather than one single process, results in progressive incompetence of the anti-reflux barrier, with compromise of each protective mechanism increasing the frequency and duration of reflux events, potentially leading to pathological damage to the oesophagus and extra-oesophageal organs [1, 19].
Respiratory diseases linked with GORD
Most of the conditions linked with reflux disease are due to EOR where there is direct contact of the respiratory system with gastric refluxate, whether by typical liquid acid GORD, gaseous airways reflux or micro-aspiration of either. An increase in cough responsiveness observed on instilling hydrochloric acid into the distal oesophagus in seven patients with bronchial asthma suggesting a vagal reflex response [20]. Moreover, in patients with chronic cough and asthma with distal typical GORD on 24-h oesophageal pH monitoring, higher levels of tachykinin were seen in induced sputum in asthmatics compared with chronic cough controls without distal reflux suggesting neurogenic inflammation [21]. Postulated EOR-related diseases can be summarised and mapped from the larynx to the lung parenchyma (figure 1). Somewhat surprisingly, the proximal upper airway can also be affected potentially by gaseous reflux in the form of sinusitis.
FIGURE 1.
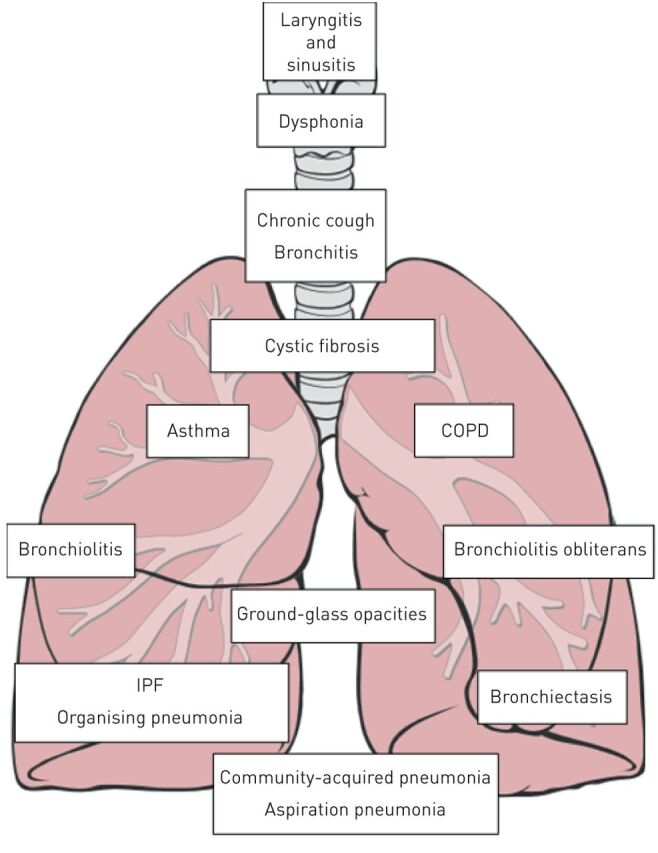
Diseases associated with gastro-oesophageal reflux disease.
A number of reflux disease-related conditions predominate in later life such as chronic cough, COPD, bronchiectasis and idiopathic pulmonary fibrosis (IPF). Why EOR can be both associated with airway disease and severe parenchymal lung disease remains unexplained. The magnitude of the reflux volume, its frequency and the constituents of the refluxate (pH, gastric or duodenal predominant, microbiology, food particles) may play a role along with genetic variation. What is inflammatory to one person's respiratory tract may not be to another individual. Evidence of this variation is demonstrated in daily clinical practice with, for instance, susceptibility of smokers to developing COPD or patients developing occupational asthma or post-viral cough syndrome.
Reflux disease and chronic respiratory disease – is it a bidirectional process?
One tends to think of the respiratory tract as a passive recipient of noxious refluxate, but it is very likely that chronic respiratory diseases can worsen or precipitate reflux disease through a number of mechanisms setting up a potential vicious cycle of damage. Patients with obstructive lung disease such as symptomatic asthma, COPD, cystic fibrosis (CF) and bronchiectasis are hyperinflated with descent of the diaphragm, thus lowering the resting pressure of the LOS and predisposing to reflux. There may also be a greater pressure gradient across the LOS after eating if there is hyperinflation as seen by the early satiety of patients with severe COPD. With more severe airflow obstruction, a greater negative intra-thoracic pressure has to be created in order to inspire, and this may also have a siphoning effect of gastric contents into the oesophagus.
Coughing also involves sudden dynamic contracture of the abdominal muscles with an associated spike in intra-abdominal pressure which could provoke reflux. Inhaled anti-cholinergic agents may have a negative effect on oesophageal motility and gastric emptying. A lowering of the pressure of the LOS has also been demonstrated with salbutamol, theophylline and steroids. It is also interesting to speculate on the role played by the length of the oesophagus which, in hyperinflated patients, will be longer, and in patients with progressive restriction, such as IPF, will be shortened. A shorter oesophagus possibly has a lower resting pressure and more proximal reflux may occur in these patients.
It seems intuitive that patients with chronic cough are more likely to develop a hiatal hernia. Interestingly, an increased prevalence of hiatal hernia with worse disease outcomes has been demonstrated in IPF, bronchiectasis and, more recently, asthma patients [22–24]. These conditions have the most end-organ damage of the EOR-related diseases possibly due to greater refluxate associated with a hiatal hernia and, in all, cough is a very dominant symptom. Lengthening of the oesophagus in hyperinflation may also create a traction force on the stomach leading to a hiatal hernia. Patients with airways obstruction are also exposed to high-dose inhaled and oral corticosteroid which may contribute to tissue laxity and subsequent development of a hiatal hernia.
Treatment of reflux disease
Proton pump inhibitors (PPIs) have been dramatically successful at ameliorating oesophageal and some extra-oesophageal symptoms of reflux disease and healing oesophageal mucosa. It is also now clear, however, that PPIs are not a panacea for reflux disease, and weakly acidic or non-acid reflux can continue or worsen without causing any local symptoms, and EOR-related respiratory tract damage via airways reflux can continue unabated [25]. PPIs are generally more effective and promote faster healing than H2-receptor antagonists, but long-term use may be associated with a variety of adverse events including osteoporosis and increased infections including community-acquired pneumonia [26]. However, whether or not this observed link is likely due to protopathic bias and confounding by indication remains a question of debate [27]. Prokinetic therapy with domperidone and metoclopramide are often trialled to speed up gastric emptying, limiting exposure of the oesophagus to acid. Prokinetic effects of macrolides have yet to be evaluated in this setting, although azithromycin has been shown to reduce hiatal hernia size and acid pocket position, thereby reducing acid reflux episodes [28]. Azithromycin is a panacea in numerous randomised controlled trials of a variety of airway diseases in successfully reducing exacerbation frequency and time to first exacerbation, and has been shown separately to act as agonists of the gut hormone motilin, so it is reasonable to hypothesise that some of the benefit of azithromycin may be related to its promotility effects [29]. Indeed, the success of azithromycin points to the importance of non-acid reflux as an important potential contributor of airways disease. Aside from lung transplant where patients taking azithromycin were found to have less objective GORD and bile acid aspiration thought to be due to enhanced oesophageal motility and accelerated gastric emptying, there is little direct evidence supporting the promotile effect of azithromycin as the potential mechanism of action in reducing exacerbations of chronic lung disease; therefore, further studies are greatly needed to confirm or refute these findings [30].
There is also increasing interest in endoscopic treatment and anti-reflux surgeries usually reserved for patients with persistent reflux disease [31]. A successful Nissen's fundoplication in select candidates with IPF and post transplant has been associated with improvements in symptoms, quality of life (QoL) and lung function decline attenuation [32–34]. Endoscopic treatments, such as the LINX or Stretta therapy, may not offer the same degree of relief provided by surgery, but might represent viable alternatives for non-surgical patients seeking relief from lifelong dependence on pharmacological therapy, its cost, associated side effects and long-term adverse outcomes [6].
A summary of the published literature on the relationship between reflux disease and chronic respiratory diseases is described below.
Reflux disease and chronic cough
It is through the clinical observation of patients with chronic cough that the nature and associations of airway reflux as a causal mechanism of respiratory disease have been elucidated [35]. The prevalence of reflux, oesophageal dysmotility and aspiration in chronic cough has been estimated from 0 to almost 100% [36]. A low incidence, poor temporal relationship and poor response with PPIs versus placebo using acid reflux criteria alone has been found [37, 38]. The suggestion of non-acid reflux as a potential aetiological factor is difficult to confirm with existing technologies, and diagnosis relies primarily on the clinical history supported by validated questionnaires [36]. The picture is also complicated by the observation that there is a high prevalence of oesophageal dysmotility in patients with chronic cough and thus oesophago-larngo-pharyngeal reflux rather than GORD may be the problem [39]. Many of the signs and symptoms associated with chronic cough are explicable by reflux and aspiration and this is very important to consider in anyone presenting with these symptoms. Recent chronic cough guidelines have highlighted the different treatable traits in chronic cough with an emphasis on non-acid reflux being treated with promotility agents rather than anti-acid drugs [36].
Reflux disease and asthma
Estimates of the prevalence of reflux disease among patients with asthma has varied from 25 to 80% [40]. A significant association between the presence of reflux disease and an increased frequency of exacerbations (OR 4.9 (95% CI1.4–17.8)) and hospitalisations in asthmatic patients has been noted [41, 42]. Impedance studies in asthma have shown acid and non-acid reflux to occur with equal frequency [43]. Manometric studies have confirmed a lower LOS pressure in asthmatic patients compared to healthy controls that correlates with low forced expiratory volume in 1 s (FEV1) and may contribute to deterioration of spirometry in asthmatics [44].
There has been a paucity of research looking at the role of gastro-oesophageal biomarkers and associations with disease severity in asthma. A recent study of 78 patients with asthma of varying severity stratified according to Global INitiative for Asthma (GINA) guidelines showed detectable bronchoalveolar lavage (BAL) pepsin in 59% patients. However, no significant associations between pepsin level and disease severity, measures of asthma control, lung function, QoL or exacerbation frequency were noted, suggesting that the importance of aspiration on asthma outcomes may be overstated [45].
Numerous studies and randomised clinical trials (RCTs) examining the potential of PPIs to improve airways disease in asthma have demonstrated mixed findings (table 1) [16, 46–81]. A multicentre, double-blind RCT in adult patients with moderate-to-severe persistent asthma and symptoms of GORD showed that treatment with lansoprazole 30 mg twice daily for 24 weeks significantly reduced asthma exacerbations and improved QoL, particularly in the subset of patients on multiple medication types. However, treating GORD did not improve symptoms directly related to asthma, nor was there any effect on pulmonary function or reduction in rescue medication use [58]. In a larger RCT of 770 participants assigned to either esomeprazole 40 mg twice daily or placebo for 16 weeks, no overall significant improvement in morning peak expiratory flow rates (PEFR) over placebo was noted. Interestingly, an improvement in PEFR in asthmatic subjects with symptoms of GORD and nocturnal respiratory symptoms was observed [61].
TABLE 1.
Studies of gastro-oesophageal reflux treatment in asthma
|
First author [ref] Study type |
n | Treatment | Asthma symptoms | Exacerbations | FEV1 | Other outcomes |
| H2RAs | ||||||
| Goodall [46] RCT crossover |
18 | Cimetidine 200 mg 5 times a day for 6 weeks | Improvement in nocturnal asthma symptom score | N/A | Unchanged | Improvement in evening PEFR |
| Nagel [47] RCT crossover |
14 | Ranitidine 400 mg four times daily for 1 week | N/A | N/A | Unchanged | No change in use of asthma medications |
| Ekstrom [48] RCT crossover |
48 | Ranitidine 150 mg twice daily for 4 weeks | Improvement in nocturnal asthma symptom score | N/A | Unchanged | N/A |
| Larrain [49] RCT placebo or surgery parallel |
27 | Cimetidine 300 mg four times daily for 6 months | N/A | N/A | Minor improvement in FEV1 after 6 months | N/A |
| PPIs | ||||||
| Meier RCT crossover [50] |
15 | Omeprazole 20 mg twice daily for 6 weeks | N/A | N/A | 27% asthma patients with GORD had a ≥20% net improvement in FEV1 after treatment | N/A |
| Teichtahl [51] RCT crossover |
20 | Omeprazole 40 mg once daily for 4 weeks versus placebo | Unchanged | N/A | N/A | Improvement in evening but not morning PEFR; improved reflux symptoms |
| Harding [52] RCT crossover |
30 | Omeprazole 20–60 mg four times daily for 12 weeks | Improved | N/A | Improved FEV1 and FVC | Improved PEFR; improved reflux symptoms |
| Levin [16] RCT crossover |
9 | Omeprazole 20 mg once daily for 8 weeks | Improved | N/A | Trend toward higher FEV1 (mean difference 15.6%) | Improved Asthma Quality of Life Score (AQLS) including sutwice dailyomains of activity limitation, symptoms and emotions |
| Boeree [53] RCT crossover |
36 | Omeprazole 40 mg b for 12 weeks versus placebo | Unchanged | N/A | Unchanged | Improved reflux symptom scores and proportion of time with pH<4; no effect on peak flow or reversibility |
| Kiljander [54, 55] RCT crossover |
107 | Omeprazole 40 mg once daily for 8 weeks versus placebo | Improved nocturnal asthma symptoms | N/A | Improved | No effect on peak flow; 18 (35%) patients had improved pulmonary symptom scores while receiving omeprazole |
| Tsugeno [56] Prospective observational |
Rabeprazole 20 mg once daily for 8 weeks | Unchanged | N/A | N/A | Improved PEFR; improved reflux symptoms |
|
| Jiang [57] RCT |
30 | Omeprazole 20 mg once daily plus domperidone 10 mg three times daily for 6 weeks versus usual care | N/A | N/A | Improved | Improved PEFR and bronchial hyperresponsiveness |
| Littner [58] RCT |
207 | Lansoprazole 30 mg once daily for 24 weeks versus placebo | Unchanged | N/A | Unchanged | Improved AQLS emotional function; no change in PEFR or use of asthma rescue medications |
| Stordal [59] RCT |
38 | Omeprazole 20 mg for 12 weeks versus placebo | Unchanged | N/A | Unchanged | Improved quality of life; improved reflux scores on pH; no change in asthma rescue medications |
| Shimizu [60] RCT |
30 | Lansoprazole 30 mg·day−1 for 8 weeks versus roxatidine (H2RA), 150 mg·day−1 | Improved | N/A | Unchanged | Improved peak flow and ACQ score |
| Kiljander [61] RCT |
770 | Esomeprazole 40 mg twice daily versus placebo for 16 weeks | Unchanged | N/A | Unchanged | Improved PEFR in patients with GORD and nocturnal symptoms only; no safety concerns noted |
| Wong [62] Prospective observational |
30 | Lansoprazole 30 mg once daily | Improved | N/A | Unchanged | No effect on PEFR; improved pulmonary symptom scores |
| Sharma [63] RCT |
Omeprazole 20 mg twice daily plus domperidone 10 mg three times daily versus placebo for 16 weeks | Improved day and night-time symptom scores | N/A | Improved FEV1 and FVC | Improved reflux symptom scores; improved PEFR; reduction in asthma rescue medications |
|
| Khorasani [64] RCT Adolescents |
36 | Omeprazole 20 mg twice daily for 6 weeks versus placebo | N/A | N/A | Improved FEV1 and FVC | Improved reflux symptoms |
| Mastronarde [65] RCT |
412 | Esomeprazole 40 mg twice daily for 24 weeks versus placebo | Unchanged | N/A | Unchanged | No effect on airway reactivity, asthma control, asthma symptom scores, nocturnal awakening or quality of life; no increase in adverse events compared to placebo |
| Bucknall [66] Prospective observational |
51 | Omeprazole up to 80 mg daily | N/A | N/A | N/A | Improved GORD symptoms and pH readings with increased therapy dose |
| Kiljander [67] RCT |
828 | Esomeprazole 40 mg once/twice daily for 26 weeks | Unchanged | N/A | Improved FEV1 in 40 mg TWICE DAILY group after 26 weeks compared to control | No effect on PEFR; improved AQLS score in both treatment groups compared to control |
| Adamko [68] Infants RCT |
19 | Combined omeprazole 10 mgonce daily plus bethanacol versus either treatment alone versus placebo | Improved daytime coughing and respiratory symptom scores | N/A | N/A | Improved GORD symptoms and GORD measured by pH; no adverse events noted |
| Holbrook [69] Children RCT |
306 | Lansoprazole 15 mg·day−1 if <30 kg or 30 mg·day−1 if ≥30 kg versus placebo | Improved | N/A | Unchanged | Improved ACQ score but no effect on asthma-related quality of life or rates of episodes of poor asthma control; in the subgroup with a positive pH study, no treatment effect was observed for any asthma outcome; increased respiratory infections noted in treatment group |
| Sandur [70] Prospective observational |
28 | Omeprazole 40 mgonce daily for 3 months; increased to 60 mgonce daily at 2 months if pH study remained abnormal | Improved pulmonary symptom and night-time asthma symptom scores | N/A | Improved FEV1 | Improved reflux symptom score and peak flow readings |
| Yamaji [71] RCT |
60 | Omeprazole 10 mgonce daily plus mosapride 5 mg three times daily versus omeprazole alone for 4 weeks | N/A | N/A | N/A | No additional amelioration of GORD symptoms when combined |
| Surgery | ||||||
| Perrin-Fayolle [73] Prospective observational |
44 | Nissen fundoplication | Improved | N/A | N/A | Pulmonary improvement classified as total cure 25%, marked improvement 16%, moderate improvement 25%, no improvement 34% 95% long-term improved reflux symptoms |
| Larrain [49] RCT |
26 | Nissen fundoplication | Improved | N/A | N/A | Clinical improvement and reduced use of asthma rescue medications |
| Spivak [74] Prospective observational |
39 | Nissen fundoplication (median follow-up 2.7 years) | Improved | N/A | N/A | Improved asthma scores; reduction in use of systemic steroids |
| Ekstrom [75] Prospective observational |
13 | Transabdominal/ laparoscopic fundoplication | N/A | N/A | Unchanged | N/A |
| Sontag [76] RCT |
62 | Antacids p.r.n. versus ranitidine 150 mg three times daily versus Nissen fundoplication for follow-up of 2 years | Surgery improves asthma symptoms | N/A | Unchanged | No effect of PEFR, rescue medications or survival |
| Khoshoo [77] Children Prospective observational |
18 | Medical treatment (lifestyle changes, proton pump inhibitors and prokinetics) or surgical treatment (Nissen fundoplication) |
Improved | N/A | N/A | Reduction in need for rescue medications |
| Khoshoo [78] Children Prospective observational |
44 | Esomeprazole plus metoclopraminde 10 mg three times daily versus ranitidine versus Nissen fundoplication | N/A | Increased exacerbations in ranitidine group compared to other treatment groups | N/A | N/A |
| Kiljander [79] Prospective observational |
69 | Esomeprazole 40 mg twice daily versus Nissen fundoplication after 3 months | Improved cough and dyspnoea with both treatment groups | N/A | Unchanged | Improved SGRQ quality of life after fundoplication |
| Silva [80] Retrospective observational |
30 | Nissen fundoplication | Improved | N/A | N/A | Improvement in daily crises of asthma |
| Hu [81] Prospective observational |
137 | Stretta radiofrequency (n=82) or laparoscopic Nissen fundoplication (n=55) | Improved | N/A | N/A | Improved reflux, respiratory and ENT symptoms in both groups, better in Nissen fundoplication group at both 1 and 5 years follow-up |
Abbreviations: FEV1: forced expiratory volume in 1 s; H2RAs: histamine-2 receptor antagonists; PEFR: peak expiratory flow rate; RCT: randomised controlled trial; GORD: gastro-oesophageal reflux; FVC: forced vital capacity; AQLS: Asthma Quality of Life Score; ACQ: Asthma Control Questionnaire; SGRQ: St. George's Respiratory Questionnaire; ENT: ears, nose and throat; N/A: not available.
A further study by the same group indicated that esomeprazole 40 mg once or twice daily in patients with moderate-to-severe asthma and GORD may improve pulmonary function and asthma-related QoL scores, but these improvements were minor and of limited clinical significance [67]. Mastronarde et al. [65] highlighted that while asymptomatic reflux amongst patients with poorly controlled asthma is highly prevalent, treatment with a PPI did not improve asthma control, perhaps suggesting that asymptomatic reflux is not a likely cause of poorly controlled asthma, or that PPI's simply do not prevent non-acidic reflux in this population. The benefit of PPI treatment has been questioned by many, with the most recent RCT for uncontrolled asthma and treatment with lansoprazole finding that the addition of lansoprazole, compared with placebo, improved neither symptoms nor lung function but was associated with increased respiratory infections [69].
Surgical targeting looking at the effect of laparoscopic Nissen's fundoplication in children with evidence of severe reflux disease and steroid-dependent asthma showed a 91% subjective improvement in symptoms, a reduction in both oral steroid and inhaler use and an increase in FEV1 in the immediate post-operative period [82]. Similar results were observed in a smaller retrospective adult series [74]. Thus, although there is no clear evidence on the optimal management of GORD in asthma until further RCT results are available, the option of fundoplication may be considered in a carefully selected subpopulation of steroid-refractory asthma patients.
Reflux disease and COPD
Reflux disease is a comorbidity in COPD with a reported prevalence of 17–54% using symptoms and questionnaires and 19–78% using oesophageal pH testing [7]. Numerous studies have reported associations with reflux disease and COPD severity, particularly in relation to increased exacerbations and hospitalisations and reduced QoL. Because lung function is not regained, exacerbations are pivotal events in COPD progression and other chronic lung diseases. In an influential study by Hurst et al. [83], the frequency and associations of exacerbation in 2138 patients enrolled in the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) study were evaluated in a multivariate model. This included an exacerbation during the previous year (OR 5.72 (95% CI 4.47–7.31)), supporting the hypothesised “frequent exacerbator phenotype”. The second-best independent predictor in this model was typical GORD (OR 2.07 (95% CI 1.58–2.72)). A secondary analysis of the ECLIPSE cohort identified self-reported GORD in 26% patients: self-reported GORD and/or use of gastric suppression medication were associated with an increased risk of moderate-to-severe and hospitalised exacerbations [84].
Other studies have also consistently demonstrated this positive relationship, noting a higher rate of hospitalisation or emergency room visits among those with COPD and reflux disease [85–95]. One study with a 5-year follow-up found that those who experience both nocturnal and daytime symptoms experienced more exacerbations, with a higher risk in those who did not use regular acid inhibitory treatment (hazard ratio (HR) 2.7 (95% CI 1.3–5.4)) [94]. In a South Korean study, symptoms of laryngopharyngeal reflux (LPR) in patients with COPD were significant predictors for severe acute exacerbation of COPD, associated with diffuse oedema, erythema, and hyperaemia on laryngeal examination. The potential interest of this finding is that LPR symptoms are a potential precursor to aspiration [95]. A subsequent systematic review and meta-analyses clearly identified GORD as a risk factor for COPD exacerbations (RR 7.57 (95% CI 3.84–14.94)), with an increased mean number of exacerbations per year (mean difference: 0.79 (95% CI 0.22–1.36)). The prevalence of GORD was significantly higher in patients with COPD than in those without (RR 13.06 (95% CI 3.64–46.87); p<0.001) [96].
Although several small studies have reported minimal impact on disease-specific QoL among those with moderate-to-severe COPD, those with a greater sample size have reported a poorer QoL reflected in disease-specific and generic questionnaires as well as greater levels of anxiety and depression and a poorer perception of physical health [86, 88, 97, 98]. The effect of reflux disease on pulmonary function decline is less clear. One study reported more frequent typical GORD symptoms in COPD patients with FEV1 <50% compared to those with FEV1 >50%, with another showing typical GORD symptoms to be associated with a reduced inspiratory capacity among patients with COPD [99, 100]. However, other studies have reported no correlation between reflux disease and lung function [101].
As impedance has yet to be performed in this patient population, the majority of these studies focus on “acid reflux” or typical GORD, which may underestimate overall reflux disease in COPD [102]. Non-acid components of reflux, such as pepsin and bile, are potentially aspirated, but are not necessarily denoted by symptoms associated with acid reflux [103]. Pepsin has been detected in sputum and exhaled breath condensate (EBC) in up to 60% of patients with COPD [101, 104]. A potential issue is that the reported association might overemphasise the role of anti-acid therapy, which may relieve symptoms associated with acid reflux but be less effective on overall reflux disease [105].
Unlike in asthma, there is a paucity of research into treatment options of reflux disease in the context of COPD (table 2) [33, 94, 106–112]. In a Japanese RCT, treatment with PPI in COPD patients without symptomatic typical GORD significantly lowered the number of exacerbations/year compared to the placebo group (OR 0.23 (95% CI 0.08–0.62)) [108]. However, these results may be related to a reduction in rhinovirus infections when taking lansoprazole through its effect on intercellular adhesion molecule (ICAM)-1, as opposed to its effect on GORD. A small observational study from Turkey showed improvement in COPD and LPR symptoms and LPR examination findings following 2 months of treatment with PPI symptomatic LPR-positive COPD patients [109]. Nissen fundoplication pre- and post-transplant COPD has showed significant improvements in FEV1 [33, 110]. Longitudinal observational studies assessing the effect of long-term anti-reflux treatment on COPD exacerbations and disease progression are conflicting [111, 112].
TABLE 2.
Studies of gastro-oesophageal reflux treatment in COPD
|
First author [ref] Study type |
n | Treatment | COPD symptoms | Exacerbations | FEV1 | Other outcomes |
|
Mokhlesi [106] Prospective observational |
100 | Antacids (43%) PPI (28%) H2RA (6%) Treatment duration not specified |
Resolution of chronic cough in 2% of patients | N/A | Unchanged | Resolution of GORD symptoms in 2% of patients |
|
Hasanoglu [107] Prospective observational |
30 | Ranitidine 50 mg intravenous, 2-h measurement | N/A | N/A | Unchanged | N/A |
|
Sasaki [108] RCT single-blind |
100 | Lansoprazole (15 mg·day−1) versus usual care | N/A | Fewer exacerbations (0.34 versus 1.18, p=0.03); fewer patients experienced >1 exacerbation (24% versus 52%; p=0.004); PPI therapy independently reduced risk of exacerbation (OR 0.23, 95% CI 0.08–0.62) |
N/A | Trend toward fewer common colds (1.22 versus 2.04) and less frequent common colds <3 per year) with PPI therapy compared to control |
|
Eryuksel [109] Prospective observational |
30 | Anti-reflux therapy (2 months) PPI therapy |
Reduced COPD symptoms (p<0.01) | N/A | N/A | Reduction in laryngopharyngeal reflux symptoms (p<0.01); improved laryngeal examinations (p<0.001) |
|
Hartwig [33] Prospective observational |
20 | Following bilateral lung transplantation, Nissen fundoplication (<365 days post-transplant) undertaken in selected patients |
Unchanged | N/A | FEV1 greater at 1 year with fundoplication compared to no fundoplication (8.8% difference) | N/A |
|
Hoppo [110] Retrospective observational |
11 | Pre-transplant Nissen fundoplication | Unchanged | N/A | Improved FEV1 and FVC % pred in overall group (separate outcomes for COPD not reported) | N/A |
|
Lee [111] Prospective observational |
17 498 | Acid suppressive medication (PPI or H2RA) | N/A | N/A | N/A | Higher incidence rate ratio of pneumonia |
|
Ingebrigtsen [94] Prospective observational |
1259 | Daily use of acid inhibitory therapy | N/A | Unchanged | N/A | N/A |
|
Su [112] Prospective observational |
17 423 | Acid suppressive therapy (PPI or H2RA) | N/A | N/A | N/A | Lower risk of acute exacerbation (HR 0.31, 95% CI 0.20–0.50, p<0.0001) and mortality (HR 0.36, 95% CI 0.20–0.65, p=0.0007) with PPIs; no significant benefit observed for H2RAs |
Abbreviations: FEV1: forced expiratory volume in 1 s; PPI: proton pump inhibitor; H2RA: histamine-2 receptor antagonist; GORD: gastro-oesophageal reflux; RCT: randomised controlled trial; FVC: forced vital capacity; HR: hazard ratio.
Reflux disease and cystic fibrosis
Reflux disease occurs frequently in children and adults with CF and estimates of prevalence range from 19 to 90%, depending on the modality used to define reflux disease [113]. Patients with CF are predisposed to reflux as a result of both primary and secondary mechanisms, particularly abnormal gastrointestinal motility manifesting as lower oesophageal pressures, delayed gastric emptying and an increased number of transient LOS relaxations [113–117]. Impedance studies in CF patients demonstrate increased numbers of total reflux episodes with a higher proportion of reflux episodes extending to the proximal oesophagus [115]. Several studies have suggested that patients with CF and reflux disease have more severe lung disease with lower pulmonary function and increased numbers of respiratory exacerbations [118–121].
The European Epidemiologic Registry of Cystic Fibrosis reported that patients with CF and GORD had a 5–10% lower FEV1 than those without GORD [122]. In a retrospective series of children with CF and evidence of both acid and non-acid reflux, a higher incidence of Pseudomonas aeruginosa in the lungs was noted compared to those who did not have reflux, and an inverse correlation between reflux burden and FEV1 as well as total number of reflux events and FEV1 was noted [118]. Similarly, van der Doef and colleagues [123] showed that GORD was associated with reduced pulmonary function and earlier acquisition of P. aeruginosa and Staphylococcus aureus, two major pathogens in CF lung disease. In their study, patients receiving treatment with gastric acid suppression had a significantly smaller yearly decline in maximal expiratory flow at 50% and maximal expiratory flow between 25 and 75% of forced vital capacity (FVC) compared with those not being treated with acid suppressors [123]. There are also suggestions in the literature that people with CF have an increased risk of Barrett's oesophagus and gastrointestinal-related cancers, which become more marked following lung transplantation [124, 125]. While a direct causative effect of reflux disease in promoting worse lung and gastrointestinal health in the majority of these studies is not demonstrated, the results remain compelling.
Duodeno-gastro-oesophageal reflux and subsequent micro-aspiration of bile acids may be an under-recognised contributor to airway injury in CF lung disease. High levels of pepsin have been described in BAL samples from children with CF with corresponding high interleukin (IL)-8 levels, confirming active reflux and micro-aspiration, not suppressed by PPI therapy [126, 127]. Consistent with these observations, high concentrations of bile acids have been described in saliva, sputum and BAL of both adults and children with CF, although there is evidence to suggest that some assays used were not of sufficient sensitivity [114, 128–131]. Concentration of bile acids correlated with neutrophil elastase concentration in sputum, degree of lung function impairment and need for intravenous antibiotic treatment [130]. The markedly reduced biodiversity and increased colonisation by dominant proteobacterial CF-associated pathogens observed in the sputum of bile-aspirating patients suggest that bile may play a major role in disease progression in CF [132]. Although initial evidence suggested that bile acids were observed in patients with homozygous DF508 genotype, subsequent studies demonstrated similar bile acid concentrations in patients with a range of CF mutations [114, 130]. A recent study in patients with the G551D mutation showed that treatment with ivacaftor was associated with a significant reduction of EOR symptoms denoted by the reflux symptom index and Hull airway reflux questionnaire [133].
Therapeutic targeting of reflux disease in CF patients is generally with high-dose PPIs and/or surgical intervention (table 3) [123, 133–139]. Use of PPIs in CF has increased consistently in recent years, initiated for a variety of reasons including improved efficacy of pancreatic enzymes in a higher pH environment, steatorrhoea, reflux symptoms, and treatment of cough or other respiratory or gastrointestinal complaints believed to be caused by GORD [140, 141]. A prospective RCT in adult patients with CF showed a trend towards shorter time to first exacerbation and increased number of exacerbations over a 6-month period in patients receiving esomeprazole compared with placebo, but the small sample size of this study precludes generalisability of the results [138]. Recent observational studies of PPIs in CF have shown an increased frequency of exacerbations and hospitalisations in patients with PPIs, but determining whether this increase is a genuine side effect of PPI treatment or a result of an increase in weakly acidic reflux events due to acid suppression remains to be determined [142, 143]. Challenge of primary bronchial epithelial cells (PBECs) cultured from CF lungs with physiologically achievable levels of primary and secondary bile acids led to increased release of the key pro-neutrophilic mediators IL-8 and IL-17 [129]. Stimulation of PBECs of one patient with CF and one healthy patient using gastric juice of 22 CF patients on and off PPIs showed higher pH and higher endotoxin levels in the gastric juice of CF patients treated with PPIs than those off treatment, resulting in a significantly enhanced inflammatory effect on CF PBECs in culture [144]. If chronic PPI treatment in CF results in a paradoxically increased inflammatory effect in the airways, alternative anti-reflux therapies need to be explored.
TABLE 3.
Studies of gastro-oesophageal reflux treatment in cystic fibrosis and bronchiectasis
|
First author [ref] Study type |
n | Treatment | CF symptoms | Exacerbations | FEV1 | Other outcomes |
| Cystic fibrosis | ||||||
| Malfroot [134] Prospective observational |
16 | Cisapride therapy | Improved weight gain and improved cough and wheeze | N/A | N/A | N/A |
| Brodzicki [135] Prospective observational |
19 | Cisapride or cisparide with ranitidine for 3 months | N/A | N/A | N/A | Improved GORD outcomes on pH analysis: decrease in reflux index, longest episode duration and the no. of episodes >5 min; improvement of endoscopic picture post-treatment |
| van der Doef [123] Prospective observational |
218 | Gastric acid inhibition (proton pump inhibitors or histamine-2 receptor antagonists) for fat malabsorption or GORD | N/A | N/A | GORD was associated with significantly reduced FEV1 and FVC Patients with gastric acid inhibition had a significantly smaller yearly decline of MEF50 and MEF25–75% |
GORD was associated with an earlier acquisition of P. aeruginosa and S. aureus |
| Tran [136] Children Prospective observational |
15 | Lansoprazole 15 mg daily for 3 months | Improved faecal steatorrhoea | N/A | N/A | Significant improvements in fat mass nutritional status and bone mineral content |
| Hendriks [137] Prospective observational |
14 | Lansoprazole 30 mg daily for 1 year | Improved faecal steatorrheoa | N/A | Improved TLC, RV and inspiratory muscle capacity | Improved BMI, decreased fat losses and improved total body fat |
| Dimango [138] RCT |
17 | PPI (esomeprazole 40 mg BD) for 36 weeks | N/A | Trend to earlier exacerbation and more frequent exacerbations in esomeprazole group | FEV1 unchanged | No change in Gastroesophageal Symptom Assessment Score or CF Quality of Life score between the two groups |
| Zeybel [133] Prospective observational |
12 | Ivacaftor (CF patients with G511D mutations) | N/A | N/A | Baseline FEV1 lower in patients with extra-oesophageal reflux symptoms | Improved extra-oesophageal reflux symptoms using the Reflux Symptom Index and the Hull Airways Reflux Questionnaire |
| Boesch [139] Children Prospective observational |
25 | Nissen fundoplication | N/A | N/A | No change in FEV1 or body mass index after fundoplication; children who had an FEV1 <60% predicted at time surgery had significantly improved FEV1 compared to those with FEV1 <60% |
No mortality associated with fundoplication, but 12% had complications that required a subsequent surgical procedure |
| Fathi [145] Prospective observational |
6 | Nissen fundoplication | N/A | 50% reduction in exacerbations 2 years post-operatively | Small but significant improvement in FEV1 and FVC 2 years post-operatively | Improved cough symptoms using the Leicester Cough Questionnaire |
| Sheikh [146] Retrospective observational |
Nissen fundoplication | Increased weight gain | Fewer pulmonary exacerbations | Slower decline in FEV1 2 years post-operatively | Better pulmonary and nutritional outcomes were noted among patients with milder lung disease compared to those with severe lung disease; no mortality associated with surgery |
|
| Bronchiectasis | ||||||
| Ahn [159] Prospective observational |
257 | PPI therapy (any type) for 6 months | N/A | N/A | Unchanged Subgroup analyses showed significant improvement in lung function in patients with high BMI related to the severity of obesity |
N/A |
| Hu [160] Prospective observational |
7 | Stretta radiofrequency (SRF) n=2 Laparoscopic fundoplication with or without hiatal hernia repair n=4 Combined n=1 |
Improved | Improved exacerbations Improved hospitalisations |
N/A | Improved GORD symptoms |
Abbreviations: CF: cystic fibrosis; FEV1: forced expiratory volume in 1 s; GORD: gastro-oesophageal reflux; FVC: forced vital capacity; MEF50: maximal expiratory flow at 50 % of FVC; MEF25–75%: mean expiratory flow at 25–75% of FVC; TLC: total lung capacity; RV: residual volume; BMI: body mass index; RCT: randomised controlled trial; PPI: proton pump inhibitor.
A recent limited literature has advocated fundoplication in CF. A retrospective study of the effect of Nissen fundoplication in patients with CF and GORD showed a significant decline in pulmonary exacerbation rate and improvement of FEV1 and FVC during the 2 years after surgery compared with the 2 years preceding surgery [145]. In 48 patients with CF and evidence of uncontrolled reflux disease despite optimal medical management, fundoplication slowed decline in lung function and need for intravenous antibiotics for at least 1 year after surgery. Improvement in FEV1 was lost by the end of the second year of follow-up in patients with an FEV1 <60% at baseline. Therefore, patients with milder disease demonstrated the greatest benefit [146]. Fundoplication in children with CF has also been undertaken, but results have been varied [139].
Although some of these studies suggest that treatment of reflux disease might result in improved lung function or exacerbation rates, prospective studies have not been conducted in CF to determine whether reducing gastric pH or surgically reducing reflux has a beneficial effect on pulmonary exacerbations or other health-related outcomes.
Reflux disease and bronchiectasis
The reported prevalence of reflux disease in bronchiectasis ranges from 34 to 74% using symptoms and questionnaires and from 11 to 75% using oesophageal pH monitoring [23, 101, 104, 147–158]. The confirmed presence of asymptomatic reflux in 42–73% of bronchiectasis patients emphasises the importance of objective confirmation of reflux disease in certain individuals [101, 150]. Three large prospective observational cohort studies suggest that typical GORD is associated with increased symptoms, increased exacerbations and hospitalisations, increased radiological severity, increased bacterial colonisation rates, reduced lung function and reduced QoL in bronchiectasis patients [23, 155, 156]. An increase in mortality has been described in two studies, a single centre study of 212 patients and a multicentre study of 986 patients [156, 157].
An increase in the prevalence of hiatal hernias has also been noted in bronchiectasis patients [23]. Increased radiological disease extent with typical GORD has been reported in bronchiectasis patients with coexisting non-tuberculous mycobacteria (NTM) [150]. The increased prevalence of typical GORD in bronchiectasis and NTM has also been observed among patients in the US bronchiectasis registry [158]. A correlation between symptoms of nocturnal reflux and distal reflux on pH monitoring has also been noted, which suggests that reflux disease may influence nocturnal respiratory status in some patients. Two case–control studies of reflux disease in bronchiectasis failed to observe any association with reduced lung function or other markers of disease severity. However, these studies were significantly underpowered to detect such effects, and a single dimension of time may be insufficient to accurately reflect the relationship between reflux disease and bronchiectasis [101, 104]. These studies also looked at pepsin as a marker of aspiration, detected in 26–70% of individuals with mild to moderate disease [101, 104].
Very few studies have assessed potential treatment strategies for reflux disease in bronchiectasis (table 3) [159, 160]. A retrospective comparison of 27 patients treated with long-term PPIs compared to 230 without showed no significant differences in lung function after 6 months [159]. A review of the clinical outcomes of seven patients with GORD-related bronchiectasis showed that anti-reflux treatment with Stretta radiofrequency and/or laparoscopic fundoplication resulted in significant improvements in exacerbations, respiratory and typical GORD symptoms over a 1- to 5-year follow-up [160]. Routine interrogation for reflux disease and RCTs of anti-reflux therapy in this patient population are urgently needed.
Reflux disease and IPF
An association between IPF and reflux disease was demonstrated in an early study which noted an increased prevalence of hiatal hernias among IPF patients [161]. The limited available research has demonstrated, through pH monitoring, that reflux disease is significantly increased in patients with IPF as compared to normal subjects but may be clinically occult [162]. This has been confirmed by Raghu et al. [163], demonstrating liquid acid GORD on 24-hour pH monitoring in 87% of their subjects. A recent systematic review, however, indicated that the prevalence of abnormal GORD in 23 studies ranged from 0 to 94% [164]. Patient selection, however, probably accounted for the results at the extremes.
Patients with IPF can experience acute exacerbations in their respiratory status leading to loss of lung function, morbidity and mortality. Occult aspiration of gastric contents has been proposed as a possible mechanism. BAL pepsin levels have been shown to correlate with clinical features and disease course in IPF, but this was not an independent predictor of survival [165]. Combining reflux disease testing by pH–impedance and BAL markers of aspiration was evaluated in a study by Savarino et al. [166]. IPF patients were found to have higher levels of reflux disease in terms of proximal reflux events and BAL bile acids and pepsin than non-IPF patients and healthy volunteers.
Recently, lung disease severity in IPF has been found to be strongly associated with impedance measures of bolus reflux than pH parameters of acid reflux alone in a retrospective study of 45 patients undergoing assessment pre-transplant [167]. Some patients with IPF have marked asymmetry of their lung disease on high-resolution CT (HRCT), potentially suggestive of aspiration [168]. These patients showed an increased prevalence of acute exacerbations, with increased reflux symptoms.
Studies of anti-reflux treatment in IPF are lacking (table 4) [169–181]. An influential retrospective study of 204 patients showed that reflux disease therapy, consisting of PPIs and surgery, was associated with longer survival in IPF and a lower radiological fibrosis score, emphasising the need for further careful study [172]. Similar findings in an analysis of data from three RCTs have also been reported whereby, after adjustment for sex and baseline lung function, patients taking anti-acid treatment had a smaller decrease in FVC at 30 weeks compared to those not taking anti-acid treatment [172, 176, 177]. Recent meta-analyses of randomised trials and observational case–control studies of reflux disease in IPF suggest that pharmacological treatment of reflux disease may be associated with a reduction in IPF-related (adjusted HR 0.45 (0.24–0.84)) but not overall mortality and that the observed association with reflux disease may be confounded by smoking [177, 182, 183]. The most recently reported trials of PPIs and surgical fundoplication in IPF suggest non-significant reductions in FVC decline with both treatment entities, with a small increase in respiratory-related infections with twice-daily omeprazole use [34, 179].
TABLE 4.
Studies of gastro-oesophageal reflux treatment in interstitial pulmonary fibrosis
|
First author [ref] Study type |
n | Treatment | IPF symptoms | Exacerbations | FEV1 | Other outcomes |
| Medications | ||||||
| Bradford [169] Retrospective observational |
262 | Chronic anti-reflux medications (>6 months non-p.r.n. use of any antacid, sucralfate, H2RA or PPI) versus non-users (<6 months of use or none) | N/A | N/A | Unchanged | Increased risk of hospitalisation and respiratory hospitalisation in chronic anti-reflux medication users; no effect on mortality |
| Gribbin [170] Retrospective case–control |
920 | Anti-reflux medications (H2RA or PPI) | N/A | N/A | N/A | IPF diagnosis significantly associated with anti-reflux therapy (OR 2.20, 95% CI 1.88–2.58) |
| Lee [171] Retrospective observational |
204 | Anti-reflux medications (H2RA or PPI) | N/A | N/A | N/A | Anti-reflux medications were an independent predictor of longer survival time; anti-reflux medications were associated with a lower radiological fibrosis score |
| Lee [172] Retrospective observational |
242 | Anti-reflux medications (H2RA or PPI) | N/A | N/A | Unchanged | Patients taking anti-reflux medications at baseline had a smaller decrease in FVC at 30 weeks (−0.06 L, 95% CI −0.11 to −0.01) compared to those not taking anti-reflux medications (−0.12 L, 95% CI −0.17 to −0.08; difference 0.07 L, 95% CI 0–0.14; p=0.05). No change in all-cause mortality |
| Kilduff [173] Prospective observational |
18 | Anti-reflux medications (H2RA or PPI) undergoing oesophageal pH–impedance | N/A | N/A | N/A | Significant decrease in the number of acid reflux events (p=0.02), but an increase in the number of non-acid reflux events (p=0.01); no change in cough frequency (p=0.70) |
| Ghebremariam [174] Prospective observational |
215 | PPI therapy >12 months | N/A | N/A | N/A | Use of PPIs was associated with a significant reduction in the number of patients with lung transplantation or death (p=0.025) and a 1.4-year increase in longevity (median survival of 3.4 versus 2 years; p<0.001) |
| Raghu [181] Prospective observational |
406 | Anti-reflux medications (H2RA or PPI) with and without nintedanib | N/A | N/A | N/A | Anti-reflux medication use at baseline did not influence the treatment effect of nintedanib on reducing decline in FVC in patients with IPF |
| Lee [176] Retrospective observational |
786 | PPI any type (mean follow-up 2.6 years) | N/A | N/A | N/A | Patients administered PPI >4 months had a lower IPF-related mortality rate than patients on PPI <4 months; younger age, higher initial FVC and longer duration of PPI use, but not a diagnosis of GORD, were significantly associated with lower IPF-related mortality |
| Kreuter [177] Pooled analysis |
291 | Anti-reflux medications (H2RA or PPI) For 52 weeks follow-up |
N/A | Overall and pulmonary infections higher in patients with advanced IPF treated with anti-reflux medications compared to those not treated | Unchanged | No difference in overall or IPF-related mortality between groups; no difference in hospitalisations between groups |
| Kreuter [178] Post hoc RCT analysis |
623 | Anti-reflux medications (H2RA or PPI) with and without pirfenidone | N/A | Severe pulmonary infections higher in patients treated with anti-reflux medications compared to those not treated; no difference in all-cause hospitalisation rate | Unchanged | No significant differences in disease progression, all-cause mortality rate IPF-related mortality rate or mean change in percent FVC between groups; severe gastrointestinal adverse events were more frequent with anti-reflux medications |
| Dutta [179] RCT |
45 | PPI (omeprazole) | N/A | Small excess of lower respiratory tract infection in omeprazole-treated group | Small reduction in FEV1 in omeprazole-treated group | Non-significant reduction in geometric mean cough frequency at the end of treatment, adjusted for baseline in the omeprazole group compared with placebo; omeprazole was well tolerated and adverse event profiles were similar in both groups; non-significant reduction in FVC associated with omeprazole |
| Surgery | ||||||
| Linden [180] Prospective observational |
19 | Nissen fundoplication (15-month follow-up) | N/A | N/A | Unchanged | Unchanged exercise capacity; stable oxygen requirements compared to IPF patients without fundoplication on transplant list |
| Raghu [181] Retrospective observational |
27 | Nissen fundoplication | N/A | N/A | Unchanged | Improvement in mean DeMeester scores from 42 to 4 (p<0.01); trend toward stabilisation in observed FVC No 90-day deaths |
| Raghu (WRAP-IPF trial) [34] RCT |
58 | Nissen fundoplication | N/A | Non-significant reduction in exacerbations & respiratory hospitalisations in surgery-treated group | N/A | Non-significant reduction in rate of change of FVC (p=0.28) and mortality over 48 weeks |
Abbreviations: IPF: interstitial pulmonary fibrosis; FEV1: forced expiratory volume in 1 s; H2RA: histamine-2 receptor antagonist; PPI: proton pump inhibitor; FVC: forced vital capacity; GORD: gastro-oesophageal reflux; RCT: randomised controlled trial.
Due to the older age and multimorbidity of IPF patients, lung and non-lung surgical procedures have a high degree of risk, indicating the need for very careful patient selection. The Newcastle group have pioneered the role of the aerodigestive multidisciplinary team and have shown that fundoplication is only suitable in a minority of IPF patients following an integrated approach due to the presence of oesophageal dysmotility and multiple comorbidities [184]. It is of potential concern that the current literature includes increasing numbers of statements supporting surgical treatment for IPF despite a lack of evidence from clinical trials [164]. Importantly, evidence-based guidelines for treatment of IPF approved conditional recommendation of PPIs for all patients with IPF regardless of their reflux disease status [185]. This could potentially limit the number of IPF patients enrollable in future treatment efficacy studies.
Reflux disease and lung transplant
Reflux disease post lung transplantation is now identified as a major risk factor for the development of bronchiolitis obliterans syndrome (BOS), which is the commonest cause of late graft failure. Increased total proximal and distal reflux episodes on pre-transplant impedance and pH testing have also been associated with decreased time to early allograft injury after lung transplantation [186]. Damage to the vagal nerves is also common during the lengthy complex surgery. Calcineurin inhibitors to prevent rejection also significantly suppress oesophageal and gastric peristalsis. Up to 75% of post-transplant patients have demonstrable reflux disease with impedance or biomarker presence following lung transplantation [187–190]. Recent studies suggest that oesophageal dysmotility and impaired clearance of swallowed bolus or refluxed contents are also important risk factors in the development of lung allograft dysfunction [191]. A retrospective review of persistent PPI therapy in 188 patients post lung transplant demonstrated that PPIs are protective against rejection, independent of other clinical predictors including body mass index, suggesting that PPIs may have anti-reflux or anti-inflammatory effects in enhancing allograft protection [192]. Anti-reflux surgery has also been associated with an increased survival and improved lung function [33]. In particular, fundoplication within 3 months or, as has more recently been demonstrated, within 1 month of transplant may result in a significant reduction in the incidence of BOS [193]. Studies have also shown a potential therapeutic benefit of azithromycin post lung-transplant in improving FEV1 in patients with BOS, but whether this is due to its immunomodulatory effect on small airways or prokinetic effect on the upper gut is unclear [194].
Diagnosis and treatment of reflux disease in chronic respiratory diseases
Diagnosing GORD in respiratory patients can be very challenging, as there is a paucity of randomised trials to direct appropriate therapy. The authors recommend the following approach.
Very detailed history taking, nuanced also for the presence of EOR. Validated questionnaires for GORD and EOR could be very helpful. Reflux disease symptoms, however, may be entirely absent in some patients.
If reflux disease is suspected, lifestyle modification, particularly weight loss if obese, avoidance of late-night meals or food triggers and elevating the head of the bed should be trialled.
In patients with reflux disease and/or suspected reflux disease-exacerbated lung disease, start treatment trial twice daily PPI for up to 8 weeks. If good response, continue PPI and reduce to the minimum beneficial dose. If poor response, check compliance (PPI should be taken 30–60 min pre-meal).
Response to treatment may be difficult to determine, but a reduction in exacerbation frequency of airway diseases, or clinical and radiological improvement in bronchiolitis and other infiltrative disorders would be encouraging and long-term PPI treatment advocated.
As yet, there is no evidence to support the addition of prokinetic drugs such as domperidone, metaclopramide or macrolides.
In non-responders with suspected reflux disease-exacerbated lung disease, again check compliance. If satisfactory, further investigation should be considered with oesophageal manometry to exclude achalasia or oesophageal spasm and determine presence and size of a hiatal hernia, and 24-h oesophageal pH and impedance monitoring to determine non-adequate suppression of acid, non-acid or gaseous reflux and its proximal extent.
In those with persistent oesophageal symptoms, particularly dysphagia, despite PPI, an oesophago-gastro-duodenoscopy (OGD) would be warranted to exclude persistent erosive disease, Barrett's oesophagus or malignancy, functional heartburn, oesophageal stricture or eosinophilic oesophagitis.
Detection of biomarkers such as pepsin and bile acids in BAL, EBC, induced sputum or saliva is not yet validated but may be promising as absolute proof of reflux disease.
In patients proven to be refluxing despite PPI with significant oesophageal and extra-oesophageal disease, anti-reflux surgery should be considered. Oesophageal physiology studies including dysmotility and pH–impedance studies should be performed to inform the risk:benefit ratio. All patients being considered for surgery should be discussed at an aerodigestive multidisciplinary team meeting with lung and gastroenterology representation. A Nissen's fundoplication is the most commonly performed surgical procedure, consisting of a complete 360° wrap to create an anti-reflux valve at the fundus of the stomach that inhibits the regurgitation of gastric contents into the oesophagus. Anecdotal successes abound, but there have been no randomised trials of its effect in reflux disease-related respiratory syndromes.
RCTs of anti-reflux medications and surgery are needed across the spectrum of chronic lung disease to determine effects of treatment and control for confounding and protopathic bias.
Conclusion
Aerodigestive disease is a rapidly growing field within respiratory medicine with reflux disease suspected of having an adverse role in a number of chronic respiratory diseases, therefore our index of suspicion should remain high. A vicious cycle of worsening reflux disease and lung disease may ensue. If the patient has typical GORD or suggestible EOR symptoms, an 8-week trial of PPIs is indicated followed by prokinetics after reviewing the potential benefits versus known risks. Lack of response warrants further investigation with oesophageal manometry, 24-h pH–impedance monitoring and an oesophageal mucosal inspection. If reflux disease is still suspected, anti-reflux surgery may be considered.
Footnotes
Conflict of interest: M.J. McDonnell reports grants from Health Research Board Ireland and the European Respiratory Society during the conduct of the study.
Conflict of interest: E.B. Hunt reports grants from University College Cork during the conduct of the study.
Conflict of interest: C. Ward has nothing to disclose.
Conflict of interest: J.P. Pearson has nothing to disclose.
Conflict of interest: D. O'Toole reports grants from Health Research Board Ireland and Science Foundation Ireland during the conduct of the study.
Conflict of interest: J.G. Laffey has nothing to disclose.
Conflict of interest: D.M. Murphy reports a UCC Translational Research Access Programme Award during the conduct of the study; personal fees and nonfinancial support from AstraZeneca and Novartis, personal fees from Teva, personal fees from Boehringer Ingelheim and GSK, and personal fees and nonfinancial support from Menarini and Bayer, outside the submitted work.
Conflict of interest: R.M. Rutherford has nothing to disclose.
Support statement: M.J. McDonnell acknowledges grant funding from the Health Research Board, Ireland (NSAFP-2013-1) and is a past recipient of a European Respiratory Society Fellowship (LRTF-42-2012). E.B. Hunt has received a Denis O'Sullivan Fellowship award from University College Cork. D.M. Murphy has been awarded an Alimentary Pharmabiotic Centre grant from University College Cork, is the past recipient of a European Respiratory Society Fellowship and has been awarded a Translational Research Access Programme award from University College Cork. J.G. Laffey was funded by Science Foundation Ireland (16/FRL/3845) under their Future Research Leaders Programme.
References
- 1.Kahrilas PJ. GERD pathogenesis, pathophysiology, and clinical manifestations. Cleve Clin J Med 2003; 70: Suppl. 5, S4–19. doi: 10.3949/ccjm.70.Suppl_5.S4 [DOI] [PubMed] [Google Scholar]
- 2.Shi G, Bruley des Varannes S, Scarpignato C, et al. Reflux related symptoms in patients with normal oesophageal exposure to acid. Gut 1995; 37: 457–464. doi: 10.1136/gut.37.4.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vakil N, van Zanten SV, Kahrilas P, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006; 101: 1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x [DOI] [PubMed] [Google Scholar]
- 4.El-Serag HB, Sweet S, Winchester CC, et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2014; 63: 871–880. doi: 10.1136/gutjnl-2012-304269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bredenoord AJ, Pandolfino JE, Smout AJ. Gastro-oesophageal reflux disease. Lancet 2013; 381: 1933–1942. doi: 10.1016/S0140-6736(12)62171-0 [DOI] [PubMed] [Google Scholar]
- 6.Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 2013; 108: 308–328. doi: 10.1038/ajg.2012.444 [DOI] [PubMed] [Google Scholar]
- 7.Lee AL, Goldstein RS. Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis 2015; 10: 1935–1949. doi: 10.2147/COPD.S77562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hungin APS, Raghunath AS, Wiklund I. Beyond heartburn: a systematic review of the extra-oesophageal spectrum of reflux-induced disease. Fam Pract 2005; 22: 591–603. doi: 10.1093/fampra/cmi061 [DOI] [PubMed] [Google Scholar]
- 9.Castell DO, Vela M. Combined multichannel intraluminal impedance and pH-metry: an evolving technique to measure type and proximal extent of gastroesophageal reflux. Am J Med 2001; 111: Suppl. 8A, 157S–159S. doi: 10.1016/S0002-9343(01)00826-9 [DOI] [PubMed] [Google Scholar]
- 10.Sifrim D, Holloway R, Silny J, et al. Acid, nonacid, and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenterology 2001; 120: 1588–1598. doi: 10.1053/gast.2001.24841 [DOI] [PubMed] [Google Scholar]
- 11.Kahrilas PJ, Sifrim D. High-resolution manometry and impedance-pH/manometry: valuable tools in clinical and investigational esophagology. Gastroenterology 2008; 135: 756–769. doi: 10.1053/j.gastro.2008.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tutuian R, Castell DO. Review article: complete gastro-oesophageal reflux monitoring – combined pH and impedance. Aliment Pharmacol Ther 2006; 24: Suppl. 2, 27–37. doi: 10.1111/j.1365-2036.2006.03039.x [DOI] [PubMed] [Google Scholar]
- 13.Jamieson JR, Stein HJ, DeMeester TR, et al. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am J Gastroenterol 1992; 87: 1102–1111. [PubMed] [Google Scholar]
- 14.Johnson LF, DeMeester TR. Development of the 24-hour intraesophageal pH monitoring composite scoring system. J Clin Gastroenterol 1986; 8: Suppl. 1, 52–58. doi: 10.1097/00004836-198606001-00008 [DOI] [PubMed] [Google Scholar]
- 15.Johnson LF, Demeester TR. Twenty-four-hour pH monitoring of the distal esophagus. A quantitative measure of gastroesophageal reflux. Am J Gastroenterol 1974; 62: 325–332. [PubMed] [Google Scholar]
- 16.Levin TR, Sperling RM, McQuaid KR. Omeprazole improves peak expiratory flow rate and quality of life in asthmatics with gastroesophageal reflux. Am J Gastroenterol 1998; 93: 1060–1063. doi: 10.1111/j.1572-0241.1998.329_q.x [DOI] [PubMed] [Google Scholar]
- 17.Kahrilas PJ, McColl K, Fox M, et al. The acid pocket: a target for treatment in reflux disease? Am J Gastroenterol 2013; 108: 1058–1064. doi: 10.1038/ajg.2013.132 [DOI] [PubMed] [Google Scholar]
- 18.Schlottmann F, Andolfi C, Herbella FA, et al. GERD: presence and size of hiatal hernia influence clinical presentation, esophageal function, reflux profile, and degree of mucosal injury. Am Surg 2018; 84: 978–982. [PubMed] [Google Scholar]
- 19.Pacheco-Galván A, Hart SP, Morice AH. Relationship between gastro-oesophageal reflux and airway diseases: the airway reflux paradigm. Arch Bronconeumol 2011; 47: 195–203. doi: 10.1016/S1579-2129(11)70046-5 [DOI] [PubMed] [Google Scholar]
- 20.Wu DN, Yamauchi K, Kobayashi H, et al. Effects of esophageal acid perfusion on cough responsiveness in patients with bronchial asthma. Chest 2002; 122: 505–509. doi: 10.1378/chest.122.2.505 [DOI] [PubMed] [Google Scholar]
- 21.Patterson RN, Johnston BT, Ardill JE, et al. Increased tachykinin levels in induced sputum from asthmatic and cough patients with acid reflux. Thorax 2007; 62: 491–495. doi: 10.1136/thx.2006.063982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tossier C, Dupin C, Plantier L, et al. Hiatal hernia on thoracic computed tomography in pulmonary fibrosis. Eur Respir J 2016; 48: 833–842. doi: 10.1183/13993003.01796-2015 [DOI] [PubMed] [Google Scholar]
- 23.McDonnell MJ, Ahmed M, Das J, et al. Hiatal hernias are correlated with increased severity of non-cystic fibrosis bronchiectasis. Respirology 2015; 20: 749–757. doi: 10.1111/resp.12522 [DOI] [PubMed] [Google Scholar]
- 24.Li ZT, Ji F, Han XW, et al. Contribution of hiatal hernia to asthma in patients with gastroesophageal reflux disease. Clin Respir J 2018; 12: 1858–1864. doi: 10.1111/crj.12748 [DOI] [PubMed] [Google Scholar]
- 25.Tsoukali E, Sifrim D. The role of weakly acidic reflux in proton pump inhibitor failure, has dust settled? J Neurogastroenterol Motil 2010; 16: 258–264. doi: 10.5056/jnm.2010.16.3.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schnoll-Sussman F, Katz PO. Clinical implications of emerging data on the safety of proton pump inhibitors. Curr Treat Options Gastroenterol 2017; 15: 1–9. doi: 10.1007/s11938-017-0115-5 [DOI] [PubMed] [Google Scholar]
- 27.Filion KB. Proton pump inhibitors and community acquired pneumonia. BMJ 2016; 355: i6041. doi: 10.1136/bmj.i6041 [DOI] [PubMed] [Google Scholar]
- 28.Rohof WO, Bennink RJ, de Ruigh AA, et al. Effect of azithromycin on acid reflux, hiatus hernia and proximal acid pocket in the postprandial period. Gut 2012; 61: 1670–1677. doi: 10.1136/gutjnl-2011-300926 [DOI] [PubMed] [Google Scholar]
- 29.Broad J, Sanger GJ. The antibiotic azithromycin is a motilin receptor agonist in human stomach: comparison with erythromycin. Br J Pharmacol 2013; 168: 1859–1867. doi: 10.1111/bph.12077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mertens V, Blondeau K, Pauwels A, et al. Azithromycin reduces gastroesophageal reflux and aspiration in lung transplant recipients. Dig Dis Sci 2009; 54: 972–979. doi: 10.1007/s10620-009-0725-4 [DOI] [PubMed] [Google Scholar]
- 31.Hershcovici T, Fass R. Gastro-oesophageal reflux disease: beyond proton pump inhibitor therapy. Drugs 2011; 71: 2381–2389. doi: 10.2165/11597300-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 32.Robertson AGN, Krishnan A, Ward C, et al. Anti-reflux surgery in lung transplant recipients: outcomes and effects on quality of life. Eur Respir J 2012; 39: 691–697. doi: 10.1183/09031936.00061811 [DOI] [PubMed] [Google Scholar]
- 33.Hartwig MG, Anderson DJ, Onaitis MW, et al. Fundoplication after lung transplantation prevents the allograft dysfunction associated with reflux. Ann Thorac Surg 2011; 92: 462–468. doi: 10.1016/j.athoracsur.2011.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raghu G, Pellegrini CA, Yow E, et al. Laparoscopic anti-reflux surgery for the treatment of idiopathic pulmonary fibrosis (WRAP-IPF): a multicentre, randomised, controlled phase 2 trial. Lancet Respir Med 2018; 6: 707–714. doi: 10.1016/S2213-2600(18)30301-1 [DOI] [PubMed] [Google Scholar]
- 35.Morice AH. Airway reflux as a cause of respiratory disease. Breathe 2013; 9: 256. doi: 10.1183/20734735.000513 [DOI] [Google Scholar]
- 36.Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020; 55: 1901136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Irwin RS, French CL, Curley FJ, et al. Chronic cough due to gastroesophageal reflux. Clinical, diagnostic, and pathogenetic aspects. Chest 1993; 104: 1511–1517. doi: 10.1378/chest.104.5.1511 [DOI] [PubMed] [Google Scholar]
- 38.Kahrilas PJ, Howden CW, Hughes N, et al. Response of chronic cough to acid-suppressive therapy in patients with gastroesophageal reflux disease. Chest 2013; 143: 605–612. doi: 10.1378/chest.12-1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith JA, Houghton LA. The oesophagus and cough: laryngo-pharyngeal reflux, microaspiration and vagal reflexes. Cough 2013; 9: 12. doi: 10.1186/1745-9974-9-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mastronarde JG. Is there a relationship between GERD and asthma? Gastroenterol Hepatol (NY) 2012; 8: 401–403. [PMC free article] [PubMed] [Google Scholar]
- 41.ten Brinke A, Sterk PJ, Masclee AA, et al. Risk factors of frequent exacerbations in difficult-to-treat asthma. Eur Respir J 2005; 26: 812–818. doi: 10.1183/09031936.05.00037905 [DOI] [PubMed] [Google Scholar]
- 42.Diette GB, Krishnan JA, Dominici F, et al. Asthma in older patients: factors associated with hospitalization. Arch Intern Med 2002; 162: 1123–1132. doi: 10.1001/archinte.162.10.1123 [DOI] [PubMed] [Google Scholar]
- 43.Condino AA, Sondheimer J, Pan Z, et al. Evaluation of gastroesophageal reflux in pediatric patients with asthma using impedance-pH monitoring. J Pediatr 2006; 149: 216–219. doi: 10.1016/j.jpeds.2006.03.022 [DOI] [PubMed] [Google Scholar]
- 44.Dua S, Mohan L. Lower esophageal sphincter pressures in patients of bronchial asthma and its correlation with spirometric parameters: a case-control study. J Asthma 2016; 53: 289–294. doi: 10.3109/02770903.2015.1088548 [DOI] [PubMed] [Google Scholar]
- 45.Hunt EB, Ward C, Power S, et al. The potential role of aspiration in the asthmatic airway. Chest 2017; 151: 1272–1278. doi: 10.1016/j.chest.2017.03.005 [DOI] [PubMed] [Google Scholar]
- 46.Goodall RJ, Earis JE, Cooper DN, et al. Relationship between asthma and gastro-oesophageal reflux. Thorax 1981; 36: 116–121. doi: 10.1136/thx.36.2.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nagel RA, Brown P, Perks WH, et al. Ambulatory pH monitoring of gastro-oesophageal reflux in “morning dipper” asthmatics. BMJ 1988; 297: 1371–1373. doi: 10.1136/bmj.297.6660.1371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ekstrom T, Lindgren BR, Tibbling L. Effects of ranitidine treatment on patients with asthma and a history of gastro-oesophageal reflux: a double blind crossover study. Thorax 1989; 44: 19–23. doi: 10.1136/thx.44.1.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Larrain A, Carrasco E, Galleguillos F, et al. Medical and surgical treatment of nonallergic asthma associated with gastroesophageal reflux. Chest 1991; 99: 1330–1335. doi: 10.1378/chest.99.6.1330 [DOI] [PubMed] [Google Scholar]
- 50.Meier JH, McNally PR, Punja M, et al. Does omeprazole (Prilosec) improve respiratory function in asthmatics with gastroesophageal reflux? A double-blind, placebo-controlled crossover study. Dig Dis Sci 1994; 39: 2127–2133. doi: 10.1007/BF02090360 [DOI] [PubMed] [Google Scholar]
- 51.Teichtahl H, Kronborg IJ, Yeomans ND, et al. Adult asthma and gastro-oesophageal reflux: the effects of omeprazole therapy on asthma. Aust N Z J Med 1996; 26: 671–676. doi: 10.1111/j.1445-5994.1996.tb02938.x [DOI] [PubMed] [Google Scholar]
- 52.Harding SM, Richter JE, Guzzo MR, et al. Asthma and gastroesophageal reflux: acid suppressive therapy improves asthma outcome. Am J Med 1996; 100: 395–405. doi: 10.1016/S0002-9343(97)89514-9 [DOI] [PubMed] [Google Scholar]
- 53.Boeree MJ, Peters FT, Postma DS, et al. No effects of high-dose omeprazole in patients with severe airway hyperresponsiveness and (a)symptomatic gastro-oesophageal reflux. Eur Respir J 1998; 11: 1070–1074. doi: 10.1183/09031936.98.11051070 [DOI] [PubMed] [Google Scholar]
- 54.Kiljander TO, Salomaa ER, Hietanen EK, et al. Gastroesophageal reflux in asthmatics: a double-blind, placebo-controlled crossover study with omeprazole. Chest 1999; 116: 1257–1264. doi: 10.1378/chest.116.5.1257 [DOI] [PubMed] [Google Scholar]
- 55.Kiljander T, Salomaa ER, Hietanen E, et al. Asthma and gastro-oesophageal reflux: can the response to anti-reflux therapy be predicted? Respir Med 2001; 95: 387–392. doi: 10.1053/rmed.2001.1055 [DOI] [PubMed] [Google Scholar]
- 56.Tsugeno H, Mizuno M, Fujiki S, et al. A proton-pump inhibitor, rabeprazole, improves ventilatory function in patients with asthma associated with gastroesophageal reflux. Scand J Gastroenterol 2003; 38: 456–461. doi: 10.1080/00365520310002490 [DOI] [PubMed] [Google Scholar]
- 57.Jiang SP, Liang RY, Zeng ZY, et al. Effects of antireflux treatment on bronchial hyper-responsiveness and lung function in asthmatic patients with gastroesophageal reflux disease. World J Gastroenterol 2003; 9: 1123–1125. doi: 10.3748/wjg.v9.i5.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Littner MR, Leung FW, Ballard ED 2nd, et al. Effects of 24 weeks of lansoprazole therapy on asthma symptoms, exacerbations, quality of life, and pulmonary function in adult asthmatic patients with acid reflux symptoms. Chest 2005; 128: 1128–1135. doi: 10.1378/chest.128.3.1128 [DOI] [PubMed] [Google Scholar]
- 59.Stordal K, Johannesdottir GB, Bentsen BS, et al. Acid suppression does not change respiratory symptoms in children with asthma and gastro-oesophageal reflux disease. Arch Dis Child 2005; 90: 956–960. doi: 10.1136/adc.2004.068890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shimizu Y, Dobashi K, Kobayashi S, et al. A proton pump inhibitor, lansoprazole, ameliorates asthma symptoms in asthmatic patients with gastroesophageal reflux disease. Tohoku J Exp Med 2006; 209: 181–189. doi: 10.1620/tjem.209.181 [DOI] [PubMed] [Google Scholar]
- 61.Kiljander TO, Harding SM, Field SK, et al. Effects of esomeprazole 40 mg twice daily on asthma: a randomized placebo-controlled trial. Am J Respir Crit Care Med 2006; 173: 1091–1097. doi: 10.1164/rccm.200507-1167OC [DOI] [PubMed] [Google Scholar]
- 62.Wong CH, Chua CJ, Liam CK, et al. Gastro-oesophageal reflux disease in 'difficult-to-control' asthma: prevalence and response to treatment with acid suppressive therapy. Aliment Pharmacol Ther 2006; 23: 1321–1327. doi: 10.1111/j.1365-2036.2006.02888.x [DOI] [PubMed] [Google Scholar]
- 63.Sharma B, Sharma M, Daga MK, et al. Effect of omeprazole and domperidone on adult asthmatics with gastroesophageal reflux. World J Gastroenterol 2007; 13: 1706–1710. doi: 10.3748/wjg.v13.i11.1706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Khorasani EN, Fallahi GH, Mansouri F, et al. The effect of omeprazole on asthmatic adolescents with gastroesophageal reflux disease. Allergy Asthma Proc 2008; 29: 517–520. [DOI] [PubMed] [Google Scholar]
- 65.Mastronarde JG, Anthonisen NR, Castro M, et al. Efficacy of esomeprazole for treatment of poorly controlled asthma. N Engl J Med 2009; 360: 1487–1499. doi: 10.1056/NEJMoa0806290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bucknall C, Stanton A, Miller G, et al. The impact of normalization of esophageal acid profile by incremental protein pump inhibitors dosing in difficult asthma patients with proven gastro-esophageal acid reflux. J Asthma 2009; 46: 506–511. doi: 10.1080/02770900902866784 [DOI] [PubMed] [Google Scholar]
- 67.Kiljander TO, Junghard O, Beckman O, et al. Effect of esomeprazole 40 mg once or twice daily on asthma: a randomized, placebo-controlled study. Am J Respir Crit Care Med 2010; 181: 1042–1048. doi: 10.1164/rccm.200910-1537OC [DOI] [PubMed] [Google Scholar]
- 68.Adamko DJ, Majaesic CM, Skappak C, et al. A pilot trial on the treatment of gastroesophageal reflux-related cough in infants. Transl Pediatr 2012; 1: 23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Holbrook JT, Wise RA, Gold BD, et al. Lansoprazole for children with poorly controlled asthma: a randomized controlled trial. JAMA 2012; 307: 373–381. doi: 10.1001/jama.2011.2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sandur V, Murugesh M, Banait V, et al. Prevalence of gastro-esophageal reflux disease in patients with difficult to control asthma and effect of proton pump inhibitor therapy on asthma symptoms, reflux symptoms, pulmonary function and requirement for asthma medications. J Postgrad Med 2014; 60: 282–286. doi: 10.4103/0022-3859.138754 [DOI] [PubMed] [Google Scholar]
- 71.Yamaji Y, Isomura Y, Yoshida S, et al. Randomized controlled trial comparing the efficacy of mosapride plus omeprazole combination therapy to omeprazole monotherapy in gastroesophageal reflux disease. J Dig Dis 2014; 15: 469–476. doi: 10.1111/1751-2980.12167 [DOI] [PubMed] [Google Scholar]
- 72.Tang M, Blake KV, Lima JJ, et al. Genotype tailored treatment of mild symptomatic acid reflux in children with uncontrolled asthma (GenARA): rationale and methods. Contemp Clin Trials 2019; 78: 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Perrin-Fayolle M, Gormand F, Braillon G, et al. Long-term results of surgical treatment for gastroesophageal reflux in asthmatic patients. Chest 1989; 96: 40–45. doi: 10.1378/chest.96.1.40 [DOI] [PubMed] [Google Scholar]
- 74.Spivak H, Smith CD, Phichith A, et al. Asthma and gastroesophageal reflux: fundoplication decreases need for systemic corticosteroids. J Gastrointest Surg 1999; 3: 477–482. doi: 10.1016/S1091-255X(99)80100-0 [DOI] [PubMed] [Google Scholar]
- 75.Ekstrom T, Johansson KE. Effects of anti-reflux surgery on chronic cough and asthma in patients with gastro-oesophageal reflux disease. Respir Med 2000; 94: 1166–1170. doi: 10.1053/rmed.2000.0944 [DOI] [PubMed] [Google Scholar]
- 76.Sontag SJ, O'Connell S, Khandelwal S, et al. Asthmatics with gastroesophageal reflux: long term results of a randomized trial of medical and surgical antireflux therapies. Am J Gastroenterol 2003; 98: 987–999. [DOI] [PubMed] [Google Scholar]
- 77.Khoshoo V, Le T, Haydel RM Jr, et al. Role of gastroesophageal reflux in older children with persistent asthma. Chest 2003; 123: 1008–1013. doi: 10.1378/chest.123.4.1008 [DOI] [PubMed] [Google Scholar]
- 78.Khoshoo V, Haydel R Jr. Effect of antireflux treatment on asthma exacerbations in nonatopic children. J Pediatr Gastroenterol Nutr 2007; 44: 331–335. doi: 10.1097/MPG.0b013e31802fe89c [DOI] [PubMed] [Google Scholar]
- 79.Kiljander T, Rantanen T, Kellokumpu I, et al. Comparison of the effects of esomeprazole and fundoplication on airway responsiveness in patients with gastro-oesophageal reflux disease. Clin Respir J 2013; 7: 281–287. doi: 10.1111/crj.12005 [DOI] [PubMed] [Google Scholar]
- 80.Silva AP, Tercioti-Junior V, Lopes LR, et al. Laparoscopic antireflux surgery in patients with extra esophageal symptoms related to asthma. Arq Bras Cir Dig 2014; 27: 92–95. doi: 10.1590/S0102-67202014000200002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hu Z, Wu J, Wang Z, et al. Outcome of Stretta radiofrequency and fundoplication for GERD-related severe asthmatic symptoms. Front Med 2015; 9: 437–443. doi: 10.1007/s11684-015-0422-y [DOI] [PubMed] [Google Scholar]
- 82.Rothenberg S, Cowles R. The effects of laparoscopic Nissen fundoplication on patients with severe gastroesophageal reflux disease and steroid-dependent asthma. J Pediatr Surg 2012; 47: 1101–1104. doi: 10.1016/j.jpedsurg.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 83.Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363: 1128–1138. doi: 10.1056/NEJMoa0909883 [DOI] [PubMed] [Google Scholar]
- 84.Benson VS, Mullerova H, Vestbo J, et al. Associations between gastro-oesophageal reflux, its management and exacerbations of chronic obstructive pulmonary disease. Respir Med 2015; 109: 1147–1154. doi: 10.1016/j.rmed.2015.06.009 [DOI] [PubMed] [Google Scholar]
- 85.Terada K, Muro S, Sato S, et al. Impact of gastro-oesophageal reflux disease symptoms on COPD exacerbation. Thorax 2008; 63: 951–955. doi: 10.1136/thx.2007.092858 [DOI] [PubMed] [Google Scholar]
- 86.Martinez CH, Okajima Y, Murray S, et al. Impact of self-reported gastroesophageal reflux disease in subjects from COPDGene cohort. Respir Res 2014; 15: 62. doi: 10.1186/1465-9921-15-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rogha M, Behravesh B, Pourmoghaddas Z. Association of gastroesophageal reflux disease symptoms with exacerbations of chronic obstructive pulmonary disease. J Gastrointestin Liver Dis 2010; 19: 253–256. [PubMed] [Google Scholar]
- 88.Rascon-Aguilar IE, Pamer M, Wludyka P, et al. Role of gastroesophageal reflux symptoms in exacerbations of COPD. Chest 2006; 130: 1096–1101. doi: 10.1378/chest.130.4.1096 [DOI] [PubMed] [Google Scholar]
- 89.Shimizu Y, Dobashi K, Kusano M, et al. Different gastoroesophageal reflux symptoms of middle-aged to elderly asthma and chronic obstructive pulmonary disease (COPD) patients. J Clin Biochem Nutr 2012; 50: 169–175. doi: 10.3164/jcbn.11-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Takada K, Matsumoto S, Kojima E, et al. Prospective evaluation of the relationship between acute exacerbations of COPD and gastroesophageal reflux disease diagnosed by questionnaire. Respir Med 2011; 105: 1531–1536. doi: 10.1016/j.rmed.2011.03.009 [DOI] [PubMed] [Google Scholar]
- 91.Terada K, Muro S, Ohara T, et al. Abnormal swallowing reflex and COPD exacerbations. Chest 2010; 137: 326–332. doi: 10.1378/chest.09-0482 [DOI] [PubMed] [Google Scholar]
- 92.Ozyilmaz E, Kokturk N, Teksut G, et al. Unsuspected risk factors of frequent exacerbations requiring hospital admission in chronic obstructive pulmonary disease. Int J Clin Pract 2013; 67: 691–697. doi: 10.1111/ijcp.12150 [DOI] [PubMed] [Google Scholar]
- 93.Lin YH, Tsai CL, Chien LN, et al. Newly diagnosed gastroesophageal reflux disease increased the risk of acute exacerbation of chronic obstructive pulmonary disease during the first year following diagnosis: a nationwide population-based cohort study. Int J Clin Pract 2015; 69: 350–357. doi: 10.1111/ijcp.12501 [DOI] [PubMed] [Google Scholar]
- 94.Ingebrigtsen TS, Marott JL, Vestbo J, et al. Gastro-esophageal reflux disease and exacerbations in chronic obstructive pulmonary disease. Respirology 2015; 20: 101–107. doi: 10.1111/resp.12420 [DOI] [PubMed] [Google Scholar]
- 95.Jung YH, Lee DY, Kim DW, et al. Clinical significance of laryngopharyngeal reflux in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2015; 10: 1343–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sakae TM, Pizzichini MMM, Teixeira PJZ, et al. Exacerbations of COPD and symptoms of gastroesophageal reflux: a systematic review and meta-analysis. J Bras Pneumol 2013; 39: 259–271. doi: 10.1590/S1806-37132013000300002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Niklasson A, Strid H, Simren M, et al. Prevalence of gastrointestinal symptoms in patients with chronic obstructive pulmonary disease. Eur J Gastroenterol Hepatol 2008; 20: 335–341. doi: 10.1097/MEG.0b013e3282f2d0ec [DOI] [PubMed] [Google Scholar]
- 98.Ajmera M, Raval AD, Shen C, et al. Explaining the increased health care expenditures associated with gastroesophageal reflux disease among elderly Medicare beneficiaries with chronic obstructive pulmonary disease: a cost-decomposition analysis. Int J Chron Obstruct Pulmon Dis 2014; 9: 339–348. doi: 10.2147/COPD.S59139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Phulpoto MA, Qayyum S, Rizvi N, et al. Proportion of gastroesophageal reflux symptoms in patients with chronic obstructive pulmonary disease. J Pak Med Assoc 2005; 55: 276–279. [PubMed] [Google Scholar]
- 100.Liang BM, Feng YL. Association of gastroesophageal reflux disease symptoms with stable chronic obstructive pulmonary disease. Lung 2012; 190: 277–282. doi: 10.1007/s00408-011-9365-5 [DOI] [PubMed] [Google Scholar]
- 101.Lee AL, Button BM, Denehy L, et al. Proximal and distal gastro-oesophageal reflux in chronic obstructive pulmonary disease and bronchiectasis. Respirology 2014; 19: 211–217. doi: 10.1111/resp.12182 [DOI] [PubMed] [Google Scholar]
- 102.Ward C, Ryan V, Pearson J. Susceptibility to exacerbation in COPD. N Engl J Med 2010; 363: 2671. [DOI] [PubMed] [Google Scholar]
- 103.Perng DW, Chang KT, Su KC, et al. Exposure of airway epithelium to bile acids associated with gastroesophageal reflux symptoms: a relation to transforming growth factor-beta1 production and fibroblast proliferation. Chest 2007; 132: 1548–1556. doi: 10.1378/chest.07-1373 [DOI] [PubMed] [Google Scholar]
- 104.Lee AL, Button BM, Denehy L, et al. Exhaled breath condensate pepsin: potential noninvasive test for gastroesophageal reflux in COPD and bronchiectasis. Respir Care 2015; 60: 244–250. doi: 10.4187/respcare.03570 [DOI] [PubMed] [Google Scholar]
- 105.Jones R, Pearson J, Ward C. Functional dyspepsia. N Engl J Med 2016; 374: 895. doi: 10.1056/NEJMc1515497 [DOI] [PubMed] [Google Scholar]
- 106.Mokhlesi B, Morris AL, Huang CF, et al. Increased prevalence of gastroesophageal reflux symptoms in patients with COPD. Chest 2001; 119: 1043–1048. doi: 10.1378/chest.119.4.1043 [DOI] [PubMed] [Google Scholar]
- 107.Hasanoglu HC, Yildirim Z, Hasanoglu A, et al. Effects of ranitidine on pulmonary function tests of patients with chronic obstructive pulmonary disease. Pharmacol Res 2003; 47: 535–539. doi: 10.1016/S1043-6618(03)00012-4 [DOI] [PubMed] [Google Scholar]
- 108.Sasaki T, Nakayama K, Yasuda H, et al. A randomized, single-blind study of lansoprazole for the prevention of exacerbations of chronic obstructive pulmonary disease in older patients. J Am Geriatr Soc 2009; 57: 1453–1457. doi: 10.1111/j.1532-5415.2009.02349.x [DOI] [PubMed] [Google Scholar]
- 109.Eryuksel E, Dogan M, Olgun S, et al. Incidence and treatment results of laryngopharyngeal reflux in chronic obstructive pulmonary disease. Eur Arch Otorhinolaryngol 2009; 266: 1267–1271. doi: 10.1007/s00405-009-0922-y [DOI] [PubMed] [Google Scholar]
- 110.Hoppo T, Jarido V, Pennathur A, et al. Antireflux surgery preserves lung function in patients with gastroesophageal reflux disease and end-stage lung disease before and after lung transplantation. Arch Surg 2011; 146: 1041–1047. doi: 10.1001/archsurg.2011.216 [DOI] [PubMed] [Google Scholar]
- 111.Lee SW, Lien HC, Chang CS, et al. The impact of acid-suppressing drugs to the patients with chronic obstructive pulmonary disease: a nationwide, population-based, cohort study. J Res Med Sci 2015; 20: 263–267. [PMC free article] [PubMed] [Google Scholar]
- 112.Su VY, Liao HF, Perng DW, et al. Proton pump inhibitors use is associated with a lower risk of acute exacerbation and mortality in patients with coexistent COPD and GERD. Int J Chron Obstruct Pulmon Dis 2018; 13: 2907–2915. doi: 10.2147/COPD.S157761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pauwels A, Sifrim D, Dupont L. Gastroesophageal reflux in cystic fibrosis and non-CF bronchiectasis. In: Meyer KC, Raghu G, eds. Gastroesophageal Reflux and the Lung. New York, NY, Springer New York, 2013; pp. 153–174. [Google Scholar]
- 114.Blondeau K, Dupont LJ, Mertens V, et al. Gastro-oesophageal reflux and aspiration of gastric contents in adult patients with cystic fibrosis. Gut 2008; 57: 1049–1055. doi: 10.1136/gut.2007.146134 [DOI] [PubMed] [Google Scholar]
- 115.Pauwels A, Blondeau K, Dupont LJ, et al. Mechanisms of increased gastroesophageal reflux in patients with cystic fibrosis. Am J Gastroenterol 2012; 107: 1346–1353. doi: 10.1038/ajg.2012.213 [DOI] [PubMed] [Google Scholar]
- 116.Hauser B, De Schepper J, Malfroot A, et al. Gastric emptying and gastro-oesophageal reflux in children with cystic fibrosis. J Cyst Fibros 2016; 15: 540–547. doi: 10.1016/j.jcf.2015.12.015 [DOI] [PubMed] [Google Scholar]
- 117.Woodley FW, Machado RS, Hayes D Jr, et al. Children with cystic fibrosis have prolonged chemical clearance of acid reflux compared to symptomatic children without cystic fibrosis. Dig Dis Sci 2014; 59: 623–630. doi: 10.1007/s10620-013-2950-0 [DOI] [PubMed] [Google Scholar]
- 118.Palm K, Sawicki G, Rosen R. The impact of reflux burden on Pseudomonas positivity in children with cystic fibrosis. Pediatr Pulmonol 2012; 47: 582–587. doi: 10.1002/ppul.21598 [DOI] [PubMed] [Google Scholar]
- 119.Gustafsson PM, Fransson SG, Kjellman NI, et al. Gastro-oesophageal reflux and severity of pulmonary disease in cystic fibrosis. Scand J Gastroenterol 1991; 26: 449–456. doi: 10.3109/00365529108998565 [DOI] [PubMed] [Google Scholar]
- 120.Button BM, Roberts S, Kotsimbos TC, et al. Gastroesophageal reflux (symptomatic and silent): a potentially significant problem in patients with cystic fibrosis before and after lung transplantation. J Heart Lung Transplant 2005; 24: 1522–1529. doi: 10.1016/j.healun.2004.11.312 [DOI] [PubMed] [Google Scholar]
- 121.Ledson MJ, Wilson GE, Tran J, et al. Tracheal microaspiration in adult cystic fibrosis. J R Soc Med 1998; 91: 10–12. doi: 10.1177/014107689809100104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Navarro J, Rainisio M, Harms HK, et al. Factors associated with poor pulmonary function: cross-sectional analysis of data from the ERCF. European Epidemiologic Registry of Cystic Fibrosis. Eur Respir J 2001; 18: 298–305. doi: 10.1183/09031936.01.00068901 [DOI] [PubMed] [Google Scholar]
- 123.van der Doef HP, Arets HG, Froeling SP, et al. Gastric acid inhibition for fat malabsorption or gastroesophageal reflux disease in cystic fibrosis: longitudinal effect on bacterial colonization and pulmonary function. J Pediatr 2009; 155: 629–633. doi: 10.1016/j.jpeds.2009.06.040 [DOI] [PubMed] [Google Scholar]
- 124.Knotts RM, Solfisburg QS, Keating C, et al. Cystic fibrosis is associated with an increased risk of Barrett's esophagus. J Cyst Fibros 2019; 18: 425–429. [DOI] [PubMed] [Google Scholar]
- 125.Maisonneuve P, Marshall BC, Knapp EA, et al. Cancer risk in cystic fibrosis: a 20-year nationwide study from the United States. J Natl Cancer Inst 2013; 105: 122–129. doi: 10.1093/jnci/djs481 [DOI] [PubMed] [Google Scholar]
- 126.McNally P, Ervine E, Shields MD, et al. High concentrations of pepsin in bronchoalveolar lavage fluid from children with cystic fibrosis are associated with high interleukin-8 concentrations. Thorax 2011; 66: 140–143. doi: 10.1136/thx.2009.130914 [DOI] [PubMed] [Google Scholar]
- 127.Reder NP, Davis CS, Kovacs EJ, et al. The diagnostic value of gastroesophageal reflux disease (GERD) symptoms and detection of pepsin and bile acids in bronchoalveolar lavage fluid and exhaled breath condensate for identifying lung transplantation patients with GERD-induced aspiration. Surg Endosc 2014; 28: 1794–1800. doi: 10.1007/s00464-013-3388-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hallberg K, Fandriks L, Strandvik B. Duodenogastric bile reflux is common in cystic fibrosis. J Pediatr Gastroenterol Nutr 2004; 38: 312–316. doi: 10.1097/00005176-200403000-00016 [DOI] [PubMed] [Google Scholar]
- 129.Aseeri A, Brodlie M, Lordan J, et al. Bile acids are present in the lower airways of people with cystic fibrosis. Am J Respir Crit Care Med 2012; 185: 463. doi: 10.1164/ajrccm.185.4.463 [DOI] [PubMed] [Google Scholar]
- 130.Pauwels A, Decraene A, Blondeau K, et al. Bile acids in sputum and increased airway inflammation in patients with cystic fibrosis. Chest 2012; 141: 1568–1574. doi: 10.1378/chest.11-1573 [DOI] [PubMed] [Google Scholar]
- 131.Parikh S, Brownlee IA, Robertson AG, et al. Are the enzymatic methods currently being used to measure bronchoalveolar lavage bile salt levels fit for purpose? J Heart Lung Transplant 2013; 32: 418–423. doi: 10.1016/j.healun.2012.12.008 [DOI] [PubMed] [Google Scholar]
- 132.Reen FJ, Woods DF, Mooij MJ, et al. Aspirated bile: a major host trigger modulating respiratory pathogen colonisation in cystic fibrosis patients. Eur J Clin Microbiol Infect Dis 2014; 33: 1763–1771. doi: 10.1007/s10096-014-2133-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zeybel GL, Pearson JP, Krishnan A, et al. Ivacaftor and symptoms of extra-oesophageal reflux in patients with cystic fibrosis and G551D mutation. J Cyst Fibros 2017; 16: 124–131. doi: 10.1016/j.jcf.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Malfroot A, Dab I. New insights on gastro-oesophageal reflux in cystic fibrosis by longitudinal follow up. Arch Dis Child 1991; 66: 1339–1345. doi: 10.1136/adc.66.11.1339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Brodzicki J, Trawinska-Bartnicka M, Korzon M. Frequency, consequences and pharmacological treatment of gastroesophageal reflux in children with cystic fibrosis. Med Sci Monit 2002; 8: CR529–CR537. [PubMed] [Google Scholar]
- 136.Tran TM, Van den Neucker A, Hendriks JJ, et al. Effects of a proton-pump inhibitor in cystic fibrosis. Acta Paediatr 1998; 87: 553–558. doi: 10.1111/j.1651-2227.1998.tb01503.x [DOI] [PubMed] [Google Scholar]
- 137.Hendriks HJ, van Kreel B, Forget PP. Effects of therapy with lansoprazole on intestinal permeability and inflammation in young cystic fibrosis patients. J Pediatr Gastroenterol Nutr 2001; 33: 260–265. doi: 10.1097/00005176-200109000-00006 [DOI] [PubMed] [Google Scholar]
- 138.Dimango E, Walker P, Keating C, et al. Effect of esomeprazole versus placebo on pulmonary exacerbations in cystic fibrosis. BMC Pulm Med 2014; 14: 21. doi: 10.1186/1471-2466-14-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Boesch RP, Acton JD. Outcomes of fundoplication in children with cystic fibrosis. J Pediatr Surg 2007; 42: 1341–1344. doi: 10.1016/j.jpedsurg.2007.03.030 [DOI] [PubMed] [Google Scholar]
- 140.Heijerman HG, Lamers CB, Bakker W. Omeprazole enhances the efficacy of pancreatin (pancrease) in cystic fibrosis. Ann Intern Med 1991; 114: 200–201. doi: 10.7326/0003-4819-114-3-200 [DOI] [PubMed] [Google Scholar]
- 141.Robinson NB, DiMango E. Prevalence of gastroesophageal reflux in cystic fibrosis and implications for lung disease. Ann Am Thorac Soc 2014; 11: 964–968. doi: 10.1513/AnnalsATS.201401-044FR [DOI] [PubMed] [Google Scholar]
- 142.McCrory BE, Harper HN, McPhail GL. Use and incidence of adverse effects of proton pump inhibitors in patients with cystic fibrosis. Pharmacotherapy 2018; 38: 725–729. [DOI] [PubMed] [Google Scholar]
- 143.Ayoub F, Lascano J, Morelli G. Proton pump inhibitor use is associated with an increased frequency of hospitalization in patients with cystic fibrosis. Gastroenterology Res 2017; 10: 288–293. doi: 10.14740/gr917w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Pauwels A, Verleden S, Farre R, et al. The effect of gastric juice on interleukin-8 production by cystic fibrosis primary bronchial epithelial cells. J Cyst Fibros 2013; 12: 700–705. doi: 10.1016/j.jcf.2013.03.006 [DOI] [PubMed] [Google Scholar]
- 145.Fathi H, Moon T, Donaldson J, et al. Cough in adult cystic fibrosis: diagnosis and response to fundoplication. Cough 2009; 5: 1. doi: 10.1186/1745-9974-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sheikh SI, Ryan-Wenger NA, McCoy KS. Outcomes of surgical management of severe GERD in patients with cystic fibrosis. Pediatr Pulmonol 2013; 48: 556–562. doi: 10.1002/ppul.22630 [DOI] [PubMed] [Google Scholar]
- 147.Ahmed I, Tran J, Hind C, et al. Simultaneous oesophageal and tracheal pH monitoring in bronchiectasis. Thorax 1995; 50: A23–A50. doi: 10.1136/thx.50.Suppl_2.A23 [DOI] [Google Scholar]
- 148.Chen HC, Liu CY, Cheng HF, et al. Chest physiotherapy does not exacerbate gastroesophageal reflux in patients with chronic bronchitis and bronchiectasis. Changgeng Yi Xue Za Zhi 1998; 21: 409–414. [PubMed] [Google Scholar]
- 149.Sweet MP, Herbella FA, Leard L, et al. The prevalence of distal and proximal gastroesophageal reflux in patients awaiting lung transplantation. Ann Surg 2006; 244: 491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Koh WJ, Lee JH, Kwon YS, et al. Prevalence of gastroesophageal reflux disease in patients with nontuberculous mycobacterial lung disease. Chest 2007; 131: 1825–1830. doi: 10.1378/chest.06-2280 [DOI] [PubMed] [Google Scholar]
- 151.Banjar HH. A review of 151 cases of pediatric noncystic fibrosis bronchiectasis in a tertiary care center. Ann Thorac Med 2007; 2: 3–8. doi: 10.4103/1817-1737.30354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fortunato GA, Machado MM, Andrade CF, et al. Prevalence of gastroesophageal reflux in lung transplant candidates with advanced lung disease. J Bras Pneumol 2008; 34: 772–778. doi: 10.1590/S1806-37132008001000004 [DOI] [PubMed] [Google Scholar]
- 153.Zaid AA, Elnazir B, Greally P. A decade of non-cystic fibrosis bronchiectasis 1996–2006. Ir Med J 2010; 103: 77–79. [PubMed] [Google Scholar]
- 154.Lee AL, Denehy L, Wilson JW, et al. Upright positive expiratory pressure therapy and exercise: effects on gastroesophageal reflux in COPD and bronchiectasis. Respir Care 2012; 57: 1460–1467. doi: 10.4187/respcare.01498 [DOI] [PubMed] [Google Scholar]
- 155.Mandal P, Morice AH, Chalmers JD, et al. Symptoms of airway reflux predict exacerbations and quality of life in bronchiectasis. Respir Med 2013; 107: 1008–1013. doi: 10.1016/j.rmed.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 156.McDonnell MJ, O'Mahony M, Breen DP, et al. Increased disease severity and mortality associated with the Bronchiectasis-GORD phenotype. Eur Respir J 2015; 46: Suppl. 59, PA366. [Google Scholar]
- 157.McDonnell MJ, Aliberti S, Goeminne PC, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med 2016; 4: 969–979. doi: 10.1016/S2213-2600(16)30320-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Aksamit TR, O'Donnell AE, Barker A, et al. Adult bronchiectasis patients: a first look at the United States Bronchiectasis Research Registry. Chest 2017; 151: 982–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Ahn B, Lee DH, Lee CM, et al. Effect of proton pump inhibitors in bronchiectatic patients with gastroesophageal reflux disease. Korean J Gastroenterol 2016; 68: 10–15. doi: 10.4166/kjg.2016.68.1.10 [DOI] [PubMed] [Google Scholar]
- 160.Hu ZW, Wang ZG, Zhang Y, et al. Gastroesophageal reflux in bronchiectasis and the effect of anti-reflux treatment. BMC Pulm Med 2013; 13: 34. doi: 10.1186/1471-2466-13-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mays EE, Dubois JJ, Hamilton GB. Pulmonary fibrosis associated with tracheobronchial aspiration. A study of the frequency of hiatal hernia and gastroesophageal reflux in interstitial pulmonary fibrosis of obscure etiology. Chest 1976; 69: 512–515. doi: 10.1378/chest.69.4.512 [DOI] [PubMed] [Google Scholar]
- 162.Tobin RW, Pope CE 2nd, Pellegrini CA, et al. Increased prevalence of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 1998; 158: 1804–1808. doi: 10.1164/ajrccm.158.6.9804105 [DOI] [PubMed] [Google Scholar]
- 163.Raghu G, Freudenberger TD, Yang S, et al. High prevalence of abnormal acid gastro-oesophageal reflux in idiopathic pulmonary fibrosis. Eur Respir J 2006; 27: 136–142. doi: 10.1183/09031936.06.00037005 [DOI] [PubMed] [Google Scholar]
- 164.Raghu G, Amatto VC, Behr J, et al. Comorbidities in idiopathic pulmonary fibrosis patients: a systematic literature review. Eur Respir J 2015; 46: 1113–1130. doi: 10.1183/13993003.02316-2014 [DOI] [PubMed] [Google Scholar]
- 165.Lee JS, Song JW, Wolters PJ, et al. Bronchoalveolar lavage pepsin in acute exacerbation of idiopathic pulmonary fibrosis. Eur Respir J 2012; 39: 352–358. doi: 10.1183/09031936.00050911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Savarino E, Carbone R, Marabotto E, et al. Gastro-oesophageal reflux and gastric aspiration in idiopathic pulmonary fibrosis patients. Eur Respir J 2013; 42: 1322–1331. doi: 10.1183/09031936.00101212 [DOI] [PubMed] [Google Scholar]
- 167.Gavini S, Borges LF, Finn RT, et al. Lung disease severity in idiopathic pulmonary fibrosis is more strongly associated with impedance measures of bolus reflux than pH parameters of acid reflux alone. Neurogastroenterol Motil 2017; 29: e13001. doi: 10.1111/nmo.13001 [DOI] [PubMed] [Google Scholar]
- 168.Tcherakian C, Cottin V, Brillet PY, et al. Progression of idiopathic pulmonary fibrosis: lessons from asymmetrical disease. Thorax 2011; 66: 226–231. doi: 10.1136/thx.2010.137190 [DOI] [PubMed] [Google Scholar]
- 169.Bradford WZ, Brown KK, Noble PW, et al. Chronic use of anti-gastroesophageal reflux (GER) medications in patients with idiopathic pulmonary fibrosis (IPF). Chest 2004; 126: 772S. [Google Scholar]
- 170.Gribbin J, Hubbard R, Smith C. Role of diabetes mellitus and gastro-oesophageal reflux in the aetiology of idiopathic pulmonary fibrosis. Respir Med 2009; 103: 927–931. doi: 10.1016/j.rmed.2008.11.001 [DOI] [PubMed] [Google Scholar]
- 171.Lee JS, Ryu JH, Elicker BM, et al. Gastroesophageal reflux therapy is associated with longer survival in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011; 184: 1390–1394. doi: 10.1164/rccm.201101-0138OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lee JS, Collard HR, Anstrom KJ, et al. Anti-acid treatment and disease progression in idiopathic pulmonary fibrosis: an analysis of data from three randomised controlled trials. Lancet Respir Med 2013; 1: 369–376. doi: 10.1016/S2213-2600(13)70105-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kilduff CE, Counter MJ, Thomas GA, et al. Effect of acid suppression therapy on gastroesophageal reflux and cough in idiopathic pulmonary fibrosis: an intervention study. Cough 2014; 10: 4. doi: 10.1186/1745-9974-10-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ghebremariam YT, Cooke JP, Gerhart W, et al. Pleiotropic effect of the proton pump inhibitor esomeprazole leading to suppression of lung inflammation and fibrosis. J Transl Med 2015; 13: 249. doi: 10.1186/s12967-015-0614-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Raghu G, Crestani B, Bailes Z, et al. Effect of anti-acid medication on reduction in FVC decline with nintedanib. Eur Respir J 2015; 46: Suppl. 59, OA4502. [Google Scholar]
- 176.Lee CM, Lee DH, Ahn BK, et al. Protective effect of proton pump inhibitor for survival in patients with gastroesophageal reflux disease and idiopathic pulmonary fibrosis. J Neurogastroenterol Motil 2016; 22: 444–451. doi: 10.5056/jnm15192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kreuter M, Wuyts W, Renzoni E, et al. Antacid therapy and disease outcomes in idiopathic pulmonary fibrosis: a pooled analysis. Lancet Respir Med 2016; 4: 381–389. doi: 10.1016/S2213-2600(16)00067-9 [DOI] [PubMed] [Google Scholar]
- 178.Kreuter M, Spagnolo P, Wuyts W, et al. Antacid therapy and disease progression in patients with idiopathic pulmonary fibrosis who received pirfenidone. Respiration 2017; 93: 415–423. doi: 10.1159/000468546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Dutta P, Funston W, Mossop H, et al. Randomised, double-blind, placebo-controlled pilot trial of omeprazole in idiopathic pulmonary fibrosis. Thorax 2019; 74: 346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Linden PA, Gilbert RJ, Yeap BY, et al. Laparoscopic fundoplication in patients with end-stage lung disease awaiting transplantation. J Thorac Cardiovasc Surg 2006; 131: 438–446. doi: 10.1016/j.jtcvs.2005.10.014 [DOI] [PubMed] [Google Scholar]
- 181.Raghu G, Morrow E, Collins BF, et al. Laparoscopic anti-reflux surgery for idiopathic pulmonary fibrosis at a single centre. Eur Respir J 2016; 48: 826–832. doi: 10.1183/13993003.00488-2016 [DOI] [PubMed] [Google Scholar]
- 182.Fidler L, Sitzer N, Shapera S, et al. Treatment of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis: a systematic review and meta-analysis. Chest 2018; 153: 1405–1415. doi: 10.1016/j.chest.2018.03.008 [DOI] [PubMed] [Google Scholar]
- 183.Bedard Methot D, Leblanc E, Lacasse Y. Meta-analysis of gastroesophageal reflux disease and idiopathic pulmonary fibrosis. Chest 2019; 155: 33–43. doi: 10.1016/j.chest.2018.07.038 [DOI] [PubMed] [Google Scholar]
- 184.Jones R, Krishnan A, Zeybel GL, et al. Reflux in idiopathic pulmonary fibrosis: treatment informed by an integrated approach. ERJ Open Res 2018; 4: 00051–02018. doi: 10.1183/23120541.00051-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Raghu G, Rochwerg B, Zhang Y, et al. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An update of the 2011 clinical practice guideline. Am J Respir Crit Care Med 2015; 192: e3–e19. doi: 10.1164/rccm.201506-1063ST [DOI] [PubMed] [Google Scholar]
- 186.Lo WK, Burakoff R, Goldberg HJ, et al. Pre-transplant impedance measures of reflux are associated with early allograft injury after lung transplantation. J Heart Lung Transplant 2015; 34: 26–35. doi: 10.1016/j.healun.2014.09.005 [DOI] [PubMed] [Google Scholar]
- 187.Robertson AG, Griffin SM, Murphy DM, et al. Targeting allograft injury and inflammation in the management of post-lung transplant bronchiolitis obliterans syndrome. Am J Transplant 2009; 9: 1272–1278. doi: 10.1111/j.1600-6143.2009.02648.x [DOI] [PubMed] [Google Scholar]
- 188.Stovold R, Forrest IA, Corris PA, et al. Pepsin, a biomarker of gastric aspiration in lung allografts: a putative association with rejection. Am J Respir Crit Care Med 2007; 175: 1298–1303. doi: 10.1164/rccm.200610-1485OC [DOI] [PubMed] [Google Scholar]
- 189.Vos R, Blondeau K, Vanaudenaerde BM, et al. Airway colonization and gastric aspiration after lung transplantation: do birds of a feather flock together? J Heart Lung Transplant 2008; 27: 843–849. doi: 10.1016/j.healun.2008.05.022 [DOI] [PubMed] [Google Scholar]
- 190.Ward C, Forrest IA, Brownlee IA, et al. Pepsin like activity in bronchoalveolar lavage fluid is suggestive of gastric aspiration in lung allografts. Thorax 2005; 60: 872–874. doi: 10.1136/thx.2004.036426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Tangaroonsanti A, Lee AS, Crowell MD, et al. Impaired esophageal motility and clearance post-lung transplant: risk for chronic allograft failure. Clin Transl Gastroenterol 2017; 8: e102. doi: 10.1038/ctg.2017.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Lo WK, Goldberg HJ, Boukedes S, et al. Proton pump inhibitors independently protect against early allograft injury or chronic rejection after lung transplantation. Dig Dis Sci 2018; 63: 403–410. doi: 10.1007/s10620-017-4827-0 [DOI] [PubMed] [Google Scholar]
- 193.Brodlie M, Aseeri A, Lordan JL, et al. Bile acid aspiration in people with cystic fibrosis before and after lung transplantation. Eur Respir J 2015; 46: 1820–1823. doi: 10.1183/13993003.00891-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Corris PA, Ryan VA, Small T, et al. A randomised controlled trial of azithromycin therapy in bronchiolitis obliterans syndrome (BOS) post lung transplantation. Thorax 2015; 70: 442–450. doi: 10.1136/thoraxjnl-2014-205998 [DOI] [PMC free article] [PubMed] [Google Scholar]


