Abstract
Clinicians who care for patients infected with coronavirus disease 2019 (COVID-19) must wear a full suite of personal protective equipment, including an N95 mask or powered air purifying respirator, eye protection, a fluid-impermeable gown, and gloves. This combination of personal protective equipment may cause increased work of breathing, reduced field of vision, muffled speech, difficulty hearing, and heat stress. These effects are not caused by individual weakness; they are normal and expected reactions that any person will have when exposed to an unusual environment. The physiologic and psychologic challenges imposed by personal protective equipment may have multiple causes, but immediate countermeasures and long-term mitigation strategies can help to improve a clinician’s ability to provide care. Ultimately, a systematic approach to the design and integration of personal protective equipment is needed to improve the safety of patients and clinicians.
Experience from the COVID-19 pandemic has shown how personal protective equipment degrades the performance of individual clinicians and teams. This experience can be improved with a systematic approach to collectively managing these stressors.
Clinicians around the world use personal protective equipment while caring for patients affected by the coronavirus disease 2019 (COVID-19) pandemic. Physicians of all specialties perform aerosol-generating procedures (including tracheal intubation and extubation), administer treatments that generate aerosols (e.g., bilevel positive airway pressure ventilation and high-flow nasal cannulas), or must simply stand within two meters of an infectious patient. Personal protective equipment required for the care of these patients includes an N95 mask with a face shield or powered air-purifying respirator, a gown, and gloves. This combination of personal protective equipment causes increased work of breathing, reduced field of vision, reduced tactile sensation, and heat stress.1–4 Additional problems include ill-fitting equipment and shortages that result in constant changes in the type and availability of equipment that healthcare professionals must use. Each of these challenges has the potential to impair a clinician’s ability to care for his or her patients.
In the past, medical equipment was designed with the expectation that the user will adapt his or her workflow to the device. Instead, the device should be designed to accommodate the needs of the user. Advances in human factors engineering lead to equipment design that will enhance, rather than impair performance. Although a single piece of equipment (e.g., an N95 mask) may cause only a minor degradation in performance, multiple items used in combination have additive effects which may significantly impair a clinician’s ability to provide care.5 The authors have personally experienced this effect before the current pandemic but dismissed it as a mildly unpleasant, short-term problem. The COVID-19 pandemic requires that clinicians make continuous use of personal protective equipment for longer periods of time, exacerbating its effects on human performance. There is a paucity of information on the effects of prolonged use of the personal protective equipment required to care for COVID-19 patients, but at least one study has concluded that personal protective equipment produces negative effects on both the physical and mental health of healthcare workers.4
The diverse array of personal protective equipment worn by healthcare workers varies by location and availability and may also change over time. This lack of standardization can prevent clinicians from developing proficiency in its use and may negatively affect their ability to provide care.6 One possible advancement would be for health care systems, the government (e.g., National Institute for Occupational Safety and Health), and organizations with expertise to align and insist on higher and universal manufacturer standards for design, fit, and performance, which would allow for preemptive universal training, possibly translating to improved clinician safety and performance. This review will discuss how personal protective equipment can impair performance and propose immediate and long-term solutions for wearable, functional, and comfortable personal protective equipment in the patient care environment.
Human Performance: Impact and Countermeasures
When wearing personal protective equipment, factors such as thermal stress, limitations on hearing and vision, and restriction of movement exacerbate physical and attentional fatigue. The stressors placed on healthcare professionals through their work environment and the added burden of wearing personal protective equipment are cumulative.7 The “Task-Taxon-Task” method can be used to develop a predictive model of how physiologic and psychologic stressors can interact to impair a practitioner’s ability to function in the clinical environment.7 This model assumes that each task uses a measurable set of skills taxons, and environmental stressors cause a decrement in each skill by a measurable amount.7 The decrease in performance can be predicted by rating the impact of the stressor on each skill, assigning each skill a proportion related to its importance to the task, then summing the total.7 For example, the Task-Taxon-Task method can be used to show that physical fatigue, impacting motor skills, is additive to sleep deprivation, impairing cognition. Figure 1 uses this methodology to illustrate how impairment caused by wearing personal protective equipment is cumulative.
Fig. 1.

To accomplish an intubation, a clinician needs cognitive, visual, and motor skills. Wearing personal protective equipment may additively impair all three of these skills. Mitigating impairment in any domain may therefore improve performance. Based on the Task-Taxon-Task (T3) Method.7
Respiratory Effects
The N95 mask protects the wearer from droplets or aerosol that contains infectious agents (e.g., Mycobacterium tuberculosis, severe acute respiratory syndrome coronavirus 2). It is defined as a negative pressure respirator because the pressure inside the mask is lower than ambient pressure during inspiration, which increases work of breathing. An N95 mask increases inspiratory flow resistance by 126%, increases expiratory flow resistance by 122%, and decreases the volume of air exchanged by 37%.1 Dead-space carbon dioxide is increased and dead-space oxygen is decreased.8 Interim guidance from U.S. Centers for Disease Control and Prevention currently recommends that if exposure to bodily fluids is anticipated, a face shield should be worn and the respirator should be covered with a surgical mask to facilitate extended use. This technique increases the resistance to inhalation and exhalation.9 Humidity from exhaled air accumulates in an N95 mask over time, further increasing the work of breathing. The effect of full-face respirators is similar to that of N95 masks.10 Increased resistance to breathing is a physiologic stressor9 and can cause dyspnea, fatigue of the respiratory muscles, and changes in lung volumes and ventilation.11 A person who is unfamiliar with this sensation may respond with either hypo- or hyperventilation.12 These physiologic stressors, even in physically fit individuals, can lead to “‘hypoxia-like’ incidents characterized by short periods of confusion and cognitive impairment.”13
Ill-fitting or uncomfortable industrial respirators have been shown to cause psychologic stress, especially in workers with claustrophobia or anxiety.14 The increased work of breathing from an N95 mask may cause anxiety in some individuals. Clinicians with asthma may experience an anxiety related dyspnea.15 This same anxiety can trigger a positive feedback cycle of hyperventilation and hyperventilation that causes an increased sensation of dyspnea.16 Half-facepiece respirators can cause more anxiety than N95 respirators in some healthcare workers.17 In spite of this, many practitioners prefer half-facepiece respirators for prolonged wear, because they have an expiratory valve that mitigates the associated increased work of breathing.18
All clinicians should be aware of the potential for hyperventilation or hypoventilation while wearing a respirator and may need to consciously control the depth or rate of breathing. Clinicians should be aware of the common symptoms of hypoventilation, which include anxiety and shortness of breath, and of hyperventilation, which include light-headedness and tingling fingers. U.S. Air Force Aerospace Physiologists teach high altitude operators to regulate breathing rate and depth by deliberately speaking out loud in long sentences. This forces a person to breathe at a normalized rate and depth, as hyperventilation is nearly impossible when talking. Teaching healthcare workers to focus on taking slow, regular breaths using their diaphragm as the predominant respiratory muscle can also help to alleviate dysfunctional breathing.19 Anecdotal reports from our colleagues suggest that powered air-purifying respirators may be more comfortable, particularly if a clinician is performing a physically demanding task.
Tight-fitting respirators can deform and stretch the skin, causing discomfort and eventually pressure injury. Absorbent foam wound dressing material (e.g., Mepilex Lite, Mölnlycke Corp., Sweden) has been reported to reduce the risk of injury and to improve comfort in patients who are required to wear tight-fitting masks for noninvasive ventilation.20 After applying this material and before entering a patient care environment, the clinician should undergo a fit check to ensure that the respirator maintains a proper seal.
Vision Restrictions
Personal protective equipment can impair vision by reducing field of view and field of regard. Field of view is the width of the visual angle that can be viewed instantaneously within the visual field. Field of regard is the total area that can be seen when moving the head, eyes, and body.21 Field of view is reduced by the way that the head is positioned in the protective equipment and field of regard is reduced by the limited range of motion from side to side. In one study, the field of view was reduced in all of the 12 military combat eye protection devices evaluated.22 Similar vision restrictions are almost certainly created by much of the personal protective equipment employed in healthcare, and especially by powered air-purifying respirators. People use peripheral vision to orient themselves in space relative to the view they are focusing on. A person who has impaired peripheral vision may compensate with an altered posture and gait, increasing the likelihood of falls. Plastic face shields can become fogged or scratched and may also distort vision, further decreasing visual acuity and making procedures more difficult.23
The most effective countermeasures for restricted vision include changes to the environment that facilitate situation awareness. Personal protective equipment does not appear to affect a clinician’s ability to intubate using direct laryngoscopy or through a laryngeal mask airway. If, however, a fiberoptic bronchoscope is required and a video monitor is unavailable, it may be difficult use an optical eyepiece.24 Some countermeasures that improve a pilot’s ability to function in restricted vision situations may also be applicable to the clinician. When possible, the most critical equipment should be arranged so that it is in the clinician’s field of view. Clinicians should remember to turn their heads and look left and right periodically to monitor objects that are not seen due to reduced peripheral vision. Because the field of regard is reduced, clinicians should be trained to understand that their vision will be limited. Clinicians may need to turn their head slowly, however, to avoid becoming dizzy, especially because they also may be experiencing heat retention. Moving the head in only one axis at a time (e.g., up and down or left and right) may help to avoid disorientation. Smooth, deliberate movements will help the clinician to maintain balance using the vestibular system of the inner ear when visual cues are decreased.
As new personal protective equipment is developed, its impact on breathing, vision, hearing, physical movement, and anxiety should be considered during design and certification, particularly if the device is to be widely used. Readily available, inexpensive respirators may be developed that allow delivery of oxygen to the clinician25 and measurements of inspired and expired Po2 and partial pressure of carbon dioxide that could be monitored by a safety officer.13 Personnel who chronically hyperventilate while wearing a respirator, such as those individuals with asthma, may benefit from a mask that can be adjusted to allow for partial rebreathing when necessary.26
Impaired Communication
Respirators such as N95 face masks and powered air purifying respirators can muffle speech, making communication difficult or impossible.27,28 Clinicians should therefore look directly at the person to whom they are speaking, speak slowly and distinctly, and plan to repeat critical information.29 Using a colleague’s name at the beginning of a conversation may help to attract his or her attention. It is essential to verify critical communication (e.g., drug doses). Closed loop communication with verbal readbacks are therefore especially important in this environment. Because of the aforementioned vision restrictions, it may be difficult or impossible to see a coworker’s gestures or nonverbal communication, further emphasizing the importance of closed-loop communication.30 The suite of personal protective equipment used during the current pandemic has also made it difficult to identify or distinguish healthcare professionals from each other. One potential solution is for each clinician to write his or her name and title in bold letters on 3-inch tape placed over the front and back of the uniform; others have taped a photograph onto a visible part of his or her gown.31
Decreased Manual Dexterity
Clinicians will experience a decrease in manual dexterity caused by movement restrictions or the decreased tactile feedback provided by multiple layers of gloves.32 One study comparing intravenous with intraosseous vascular access with the provider wearing personal protective equipment and a mannequin with or without personal protective equipment concluded that vascular access was established more rapidly by the intraosseous route (14 vs. 46 s).33 Intravenous access took 90 s longer than intraosseous access in a simulated disaster scenario in which participants wore personal protective equipment.3 Data from the military corroborate that when wearing chemical protective clothing, it takes more time to finish a task.34 These studies highlight the fact that some procedures requiring a high degree of manual dexterity can take longer and might be more difficult when wearing personal protective equipment.
Clinicians should expect that procedures such as endotracheal intubation and vascular access may take longer than expected. If help is needed, assistants will need to don personal protective equipment before entering the patient care area, so clinicians should call for help earlier, especially if a patient is developing respiratory failure and may need an emergency intubation. For intraoperative procedures, clinicians should also set a lower threshold for establishing vascular access, securing the airway, or calling for extra equipment that may be needed during surgery. Although this does not appear to have been studied in healthcare professionals, practicing procedures using double gloves before performing them on an infected patient may help clinicians to compensate for any reduction in manual dexterity.
Physical and Mental Fatigue
Personal protective equipment imposes restrictions on movement and increases the difficulty of tasks requiring physical exertion, such as chest compressions during cardiopulmonary resuscitation. In addition to a decrease in the percentage of adequate compressions, rescuers exhibited an increase in heart rate, arterial blood pressure, and subjective fatigue.35 Tolerance to aerobic exercise is decreased when a person is not adequately hydrated; this effect exacerbates the progressive dehydration that occurs during exercise.36 Full-face, negative pressure respirators can impair performance on cognitive tasks,37 and it seems reasonable to assume that other respirators (such as half-face respirators) may have similar effects. Mental fatigue is also exacerbated by personal protective equipment, and the task-taxon-task model suggests that aggregate effects of stress can worsen cognitive impairment.7 This mental fatigue can present as anxiety, which impairs working memory as a result of processing of extraneous information.38
Specific countermeasures to mitigate physical and mental stress include adequate hydration and personal protective equipment that minimizes heat accumulation and enables physiologic regulation of body temperature. Healthcare professionals who wear impermeable protective equipment should drink at least 0.7 l per hour to mitigate the effects of dehydration39 and remove sweaters or warm-up jackets to prevent overheating. When clinically feasible, dividing strenuous tasks may decrease the fatigue associated with wearing protective equipment. Powered air purifying respirators do not seem to offer a significant improvement in respiratory function over N95 masks but may be more comfortable, particularly if a clinician is performing a physically demanding task for an extended period of time. Team leaders should ensure that clinicians receive adequate breaks, nutrition, and sleep whenever feasible. Clinicians can reduce the strain on prospective memory by making a list of critical tasks that must be performed in the future (e.g., antibiotic administration, redosing heparin during vascular procedures) and by using a cognitive aid during critical and off-nominal events.40
Thermoregulation
Surgical masks, N95 masks, and powered air-purifying respirators must comply with National Institute for Occupational Safety and Health regulations. Similar regulations apply to head covers, isolation gowns, fluid impermeable gowns, and gloves. Each of these regulations focuses primarily on how the personal protective equipment is used. Personal protective equipment is designed to be impermeable to fluids such as sweat, trapping hot air between the clinician’s clothing and body, and limits heat transfer by radiation and convection. Obstructions to airflow, such as fitted arm or leg cuffs, can reduce or eliminate a path for hot air to escape or cool air to enter. This results in a micro-climate of hot, humid air that inhibits the evaporation of moisture such as sweat. Wearing extensive personal protective equipment, particularly in a warm environment (such as a pediatric operating room), may therefore cause heat stress in healthcare workers.41
Clinicians can mitigate some of the effects of heat stress by minimizing layers of clothing (e.g., surgical scrubs) under the personal protective equipment. Prescription eyeglasses can be secured to the face so that they do not slip as a result of perspiration,42 possibly with an elastic band. A clinician who is sweating should resist the temptation to adjust his or her eyeglasses while wearing personal protective equipment. If the patient is not at risk for hypothermia, the room should be cooled. Loose-fitting and tight-fitting half-face powered air purifying respirators ameliorate exercise-induced increases in facial skin temperature when compared to an N95 mask. This can lead to a hazardous situation in which the wearer may feel a normal face and head temperature while his or her core temperature is increasing.43 Clinicians should consider measuring their temperature regularly and ensure that they are well hydrated if required to wear personal protective equipment for an extended period of time.4
Difficulty of Donning and Doffing Personal Protective Equipment
Donning and doffing personal protective equipment is more difficult to perform than many clinicians expect, and failure to remove personal protective equipment correctly represents a significant safety hazard. Self-assessment of proficiency is a poor predictor of a clinician’s ability to correctly don and doff personal protective equipment.44 Self-contamination can be common for clinicians who are unfamiliar with this task. In one study, for example, protocol deviations prior to training occurred in 27% of healthcare workers doffing personal protective equipment.45 Another study found that 79% of healthcare workers contaminated themselves in at least one area while doffing personal protective equipment.6 The authors of this study concluded that the errors with the highest risk were those related to hand hygiene and mishandled or compromised personal protective equipment (especially exposed hands and wrists).46 In less experienced personnel, the potential for contamination is even greater. Only 41% of medical students reported receiving personal protective equipment training, and none had received training to a demonstrated level of proficiency.47 The same study showed that 93% of trainees had one or more lapses in technique during simulation and 44% contaminated their skin with a fluorescent lotion.47 This suggests that strategies to improve donning and doffing of personal protective equipment should be implemented before the need for use. Potential strategies include procedural changes, optimization of the environment, and training.
Improved procedures and workspace design can improve the safety of personal protective equipment and reduce the risk of contamination. Clear, detailed instructions and the use of visual cognitive aids can help to improve the safety of donning and doffing personal protective equipment.48 Personnel who are developing donning and doffing procedures should evaluate potential failure modes and design procedures to include an extra margin of safety.48 Workspace design should include mirrors (to allow the clinician to see possible contamination sites), handrails, prominent disposal bins, readily available gloves and hand sanitizer, and clear demarcation of “clean” and “dirty” zones.49 A trained safety coach instructing the clinician step by step how to don and doff the equipment has been shown to help ease healthcare worker anxiety and decrease errors resulting in self contamination. A checklist may assist the safety coach.40
Training personnel in the setting in which they will work may be of benefit. Subjects can recall information more effectively in the environment in which it was originally learned,50 especially if that workspace contains signage and design cues to facilitate high level performance.51 It may also be beneficial to train healthcare workers to perform procedures and manage critical events while wearing personal protective equipment. This could be done, for example, outside an empty operating room or in the anteroom to an intensive care unit room. A simulation center can also be configured to emulate these spaces. This physical space would not only give environmental cues but also emulate the restricted space in these areas. Another measure to improve donning and doffing of personal protective equipment is to focus on error-prone steps46 and to practice multiple times. The philosophy to repeat training “not until you get it right, but until you never get it wrong” may be applicable in this setting and should be employed by clinical leaders who are responsible for reserving time to train for what may be perceived as infrequently used skills.
Psychologic Issues: Interpreting Physical Discomfort as Stress
Extended use of personal protective equipment may cause discomfort from restricted movement, weight, and heat. This can increase anxiety and stress and lower tolerance for pain and discomfort.52,53 Anxiety has been shown to decrease working memory and impair performance across a wide variety of tasks54 and could conceivably exacerbate the errors that a clinician might make while donning or doffing personal protective equipment. Setting the expectation that some amount of discomfort is normal when wearing personal protective equipment may improve healthcare workers’ tolerance to it. One study found that that participants had increased tolerance to pain after reading a positive statement and concluded that the subjective threat associated with pain was mediated by the participants’ viewpoints.52 Clinicians who are required to wear personal protective equipment may benefit from counseling as to its safety and the fact that some amount of discomfort is normal (e.g., a slightly increased work of breathing while wearing an N95 mask indicates a proper seal).
Teaching clinicians coping skills can also help to improve their tolerance to discomfort. A mindfulness training program developed for the United States military is designed to mitigate the stress caused by training and subsequent deployment and teaches personnel to develop attentional control and tolerance to challenging experiences such as harsh environmental conditions, anxiety, and discomfort. The program teaches specific skills that use concepts from psychotherapy to enhance resilience and enable complex decision making. United States Marines who participated in this program were found to have significantly lower physiologic markers associated with stress and an improved response to stress.55 A game-based educational program teaches deployed service members how to conduct brief interventions for their colleagues, including cognitive restructuring, breathing exercises, and muscle relaxation techniques.56 This technology has been demonstrated in the clinical environment: A mindfulness program developed to help surgeons manage burnout and fatigue was shown to improve wellbeing and executive function.57 Programs such as these are readily adaptable to the current clinical environment and could be introduced rapidly.
Conclusions
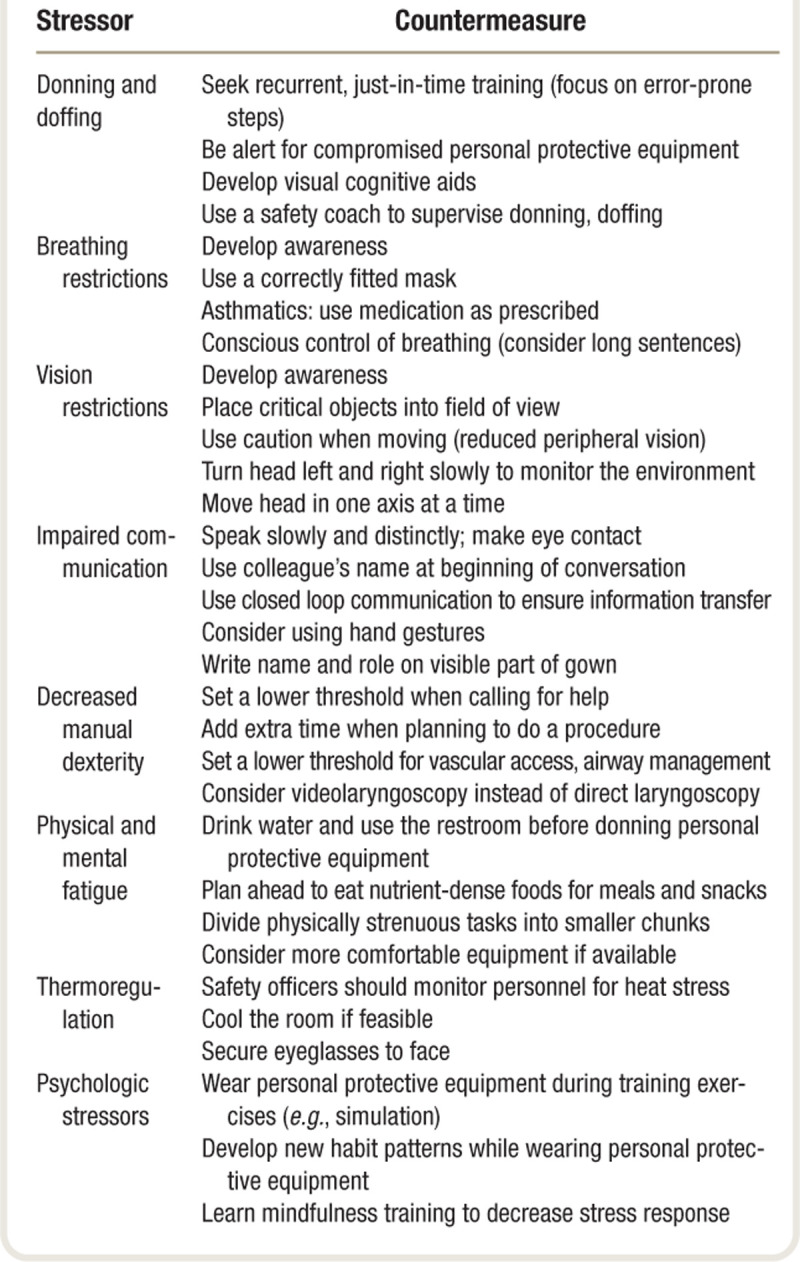
The COVID-19 pandemic reinforces the critical role that clinicians play in caring for patients and managing resources during local, regional, and global disasters. Clinicians are frequently on the front line of the response and are thus at an increased risk for infection. The personal protective equipment that is routinely used to protect clinicians imposes a variety of physiologic and psychologic stressors that may impair their performance. Modern medical personal protective equipment protects healthcare professionals but is often difficult to don and doff, is uncomfortable, and may impair a clinician’s ability to care for his or her patients. This article offers immediate countermeasures that can help to mitigate these effects and provide some relief to clinicians who must wear personal protective equipment (table 1).
Table 1.
A Summary of Countermeasures That May Help Clinicians Who Wear Personal Protective Equipment
Improving the design of personal protective equipment can help to preserve a clinician’s performance, especially in circumstances where this equipment will be worn for a prolonged period of time. Health care systems, government agencies, and experts in human performance should therefore work together to set universal standards for equipment quality, requirements, fit, and training. Although this article has described physiologic and psychologic stressors in the context of the current pandemic, the principles described are similar whenever clinicians work in an environment to which they are not accustomed. Healthcare professionals can improve patient safety and protect themselves by understanding how they are affected by physiologic and psychologic stressors and then implementing the appropriate countermeasures.
Acknowledgments
The authors thank John Loadsman, M.B.B.S., Ph.D., F.A.N.Z.C.A., Conjoint Associate Professor, University of Sydney, Sydney, Australia, for his thoughtful review of the manuscript and his insightful comments.
Research Support
Support for this study was provided solely from institutional and/or departmental sources.
Competing Interests
Dr. K. J. Ruskin is partially supported by Federal Aviation Administration Cooperative Research Agreement 692M151940006: Air Traffic Organization Alarm Management. This funding did not support any of the work involved in the preparation of this manuscript. Dr. K. J. Ruskin also receives royalties from UpToDate (published by Wolters Kluwer, Philadelphia, Pennsylvania). Dr. A. C. Ruskin receives royalties from UpToDate (published by Wolters Kluwer) and SpringerNature AG (New York, New York). She has also received an internal research grant from the University of Chicago (Chicago, Illinois). Dr. O’Connor is on the Advisory Board and has an equity interest in CLEW (Wilmington, Delaware), a startup company that does predictive analytics in healthcare. The remaining authors declare no competing interests.
Footnotes
Published online first on January 6, 2021.
Contributor Information
Anna Clebone Ruskin, Email: aclebone@gmail.com.
Brian T. Musselman, Email: moose@me.com.
Jaime Rivas Harvey, Email: jaime_leigh@mac.com.
Thomas E. Nesthus, Email: tom.nesthus@faa.gov.
Michael O’Connor, Email: moc5@dacc.uchicago.edu.
References
- 1.Lee HP, Wang DY: Objective assessment of increase in breathing resistance of N95 respirators on human subjects. Ann Occup Hyg. 2011; 55:917–21 [DOI] [PubMed] [Google Scholar]
- 2.Visentin LM, Bondy SJ, Schwartz B, Morrison LJ: Use of personal protective equipment during infectious disease outbreak and nonoutbreak conditions: A survey of emergency medical technicians. CJEM. 2015; 11:44–56 [DOI] [PubMed] [Google Scholar]
- 3.Castle N, Owen R, Hann M, Clark S, Reeves D, Gurney I: Impact of chemical, biological, radiation, and nuclear personal protective equipment on the performance of low- and high-dexterity airway and vascular access skills. Resuscitation. 2009; 80:1290–5 [DOI] [PubMed] [Google Scholar]
- 4.Loibner M, Hagauer S, Schwantzer G, Berghold A, Zatloukal K: Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomised study. PLoS One. 2019; 14:e0210775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yánez Benítez C, Güemes A, Aranda J, Ribeiro M, Ottolino P, Di Saverio S, Alexandrino H, Ponchietti L, Blas JL, Ramos JP, Rangelova E, Muñoz M, Yánez C, Sr; International Cooperation Group on PPE and Emergency Surgery: Impact of personal protective equipment on surgical performance during the COVID-19 pandemic. World J Surg. 2020; 44:2842–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang J, Kim EJ, Choi JH, Hong HK, Han SH, Choi IS, Ryu JG, Kim J, Kim JY, Park ES: Difficulties in using personal protective equipment: Training experiences with the 2015 outbreak of Middle East respiratory syndrome in Korea. Am J Infect Control. 2018; 46:235–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mueller S, Simpkins B, Anno G, Fallon C, Price O, McCellelan G: Adapting the task-taxon-task methodology to model the impact of chemical protective gear. Comput Math Organ Theory. 2011;17:251–71 [Google Scholar]
- 8.Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ: Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010; 55:569–77 [PubMed] [Google Scholar]
- 9.Sinkule EJ, Powell JB, Goss FL: Evaluation of N95 respirator use with a surgical mask cover: Effects on breathing resistance and inhaled carbon dioxide. Ann Occup Hyg. 2013; 57:384–98 [DOI] [PubMed] [Google Scholar]
- 10.Bansal S, Harber P, Yun D, Liu D, Liu Y, Wu S, Ng D, Santiago S: Respirator physiological effects under simulated work conditions. J Occup Environ Hyg. 2009; 6:221–7 [DOI] [PubMed] [Google Scholar]
- 11.Ernsting J: Physiological requirements for advanced oxygen systems, Advanced Oxygen Systems for Aircraft. Edited by Ernsting J, Miller RL. Neuilly-sur-Seine, France, NATO, 1996, NATO Aerospace Medical Panel Agardograph 286, AGARD-AG-286 [Google Scholar]
- 12.F-22 Pilot Physiological Issues: Hearing before the Committee on Armed Services, House of Representatives, 112th Congress, 2012. Available at: https://www.govinfo.gov/content/pkg/CHRG-112hhrg76215/pdf/CHRG-112hhrg76215.pdf. Accessed April 2020.
- 13.West JB: A strategy for in-flight measurements of physiology of pilots of high-performance fighter aircraft. J Appl Physiol (1985). 2013;115:145–9 [DOI] [PubMed] [Google Scholar]
- 14.Morgan WP: Psychological problems associated with the wearing of industrial respirators: A review. Am Ind Hyg Assoc J. 1983; 44:671–6 [DOI] [PubMed] [Google Scholar]
- 15.Rietveld S, Creer TL: Psychiatric factors in asthma: implications for diagnosis and therapy. Am J Respir Med. 2003; 2:1–10 [DOI] [PubMed] [Google Scholar]
- 16.Masaoka Y, Homma I: Expiratory time determined by individual anxiety levels in humans. J Appl Physiol (1985). 1999; 86:1329–36 [DOI] [PubMed] [Google Scholar]
- 17.Wu S, Harber P, Yun D, Bansal S, Li Y, Santiago S: Anxiety during respirator use: comparison of two respirator types. J Occup Environ Hyg. 2011; 8:123–8 [DOI] [PubMed] [Google Scholar]
- 18.Roberge RJ: Are exhalation valves on N95 filtering facepiece respirators beneficial at low-moderate work rates: an overview. J Occup Environ Hyg. 2012; 9:617–23 [DOI] [PubMed] [Google Scholar]
- 19.Thomas M, McKinley RK, Freeman E, Foy C, Prodger P, Price D: Breathing retraining for dysfunctional breathing in asthma: A randomised controlled trial. Thorax. 2003; 58:110–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peko Cohen L, Ovadia-Blechman Z, Hoffer O, Gefen A: Dressings cut to shape alleviate facial tissue loads while using an oxygen mask. Int Wound J. 2019; 16:813–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jang W, Shin JH, Kim M, Kim KK: Human field of regard, field of view, and attention bias. Comput Methods Programs Biomed. 2016; 135:115–23 [DOI] [PubMed] [Google Scholar]
- 22.Gunther PJ, Riddle MS: Effect of combat eye protection on field of view among active-duty U.S. military personnel. Optometry. 2008; 79:663–9 [DOI] [PubMed] [Google Scholar]
- 23.Lombardi DA, Verma SK, Brennan MJ, Perry MJ: Factors influencing worker use of personal protective eyewear. Accid Anal Prev. 2009; 41:755–62 [DOI] [PubMed] [Google Scholar]
- 24.Greenland KB, Tsui D, Goodyear P, Irwin MG: Personal protection equipment for biological hazards: Does it affect tracheal intubation performance? Resuscitation. 2007; 74:119–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mardimae A, Slessarev M, Han J, Sasano H, Sasano N, Azami T, Fedorko L, Savage T, Fowler R, Fisher JA: Modified N95 mask delivers high inspired oxygen concentrations while effectively filtering aerosolized microparticles. Ann Emerg Med. 2006; 48:391–9, 399.e1–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johansen T, Jack S, Dahl R: Normalizing CO2 in chronic hyperventilation by means of a novel breathing mask: A pilot study. Clin Respir J. 2013; 7:359–66 [DOI] [PubMed] [Google Scholar]
- 27.Radonovich LJ, Jr, Yanke R, Cheng J, Bender B: Diminished speech intelligibility associated with certain types of respirators worn by healthcare workers. J Occup Environ Hyg. 2010; 7:63–70 [DOI] [PubMed] [Google Scholar]
- 28.Palmiero AJ, Symons D, Morgan JW, 3rd, Shaffer RE: Speech intelligibility assessment of protective facemasks and air-purifying respirators. J Occup Environ Hyg. 2016; 13:960–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tan NC, Goh LG, Lee SS: Family physicians’ experiences, behaviour, and use of personal protection equipment during the SARS outbreak in Singapore: Do they fit the Becker Health Belief Model? Asia Pac J Public Health. 2006; 18:49–56 [DOI] [PubMed] [Google Scholar]
- 30.Etherington N, Wu M, Cheng-Boivin O, Larrigan S, Boet S: Interprofessional communication in the operating room: A narrative review to advance research and practice. Can J Anaesth. 2019; 66:1251–60 [DOI] [PubMed] [Google Scholar]
- 31.Wong B: Medical Workers Wear Pics of Themselves Smiling to Comfort COVID-19 Patients. Huffpost. April 10, 2020. Available at: https://www.huffpost.com/entry/medical-workers-pics-smiling-covid-19-patients_l_5e8f725bc5b6b371812da523. Accessed April 2020.
- 32.Batra S, Bronkema L, Wang M, Bishu R: Glove attributes: Can they predict performance? Int J Indust Ergo. 1994;14:201–9 [Google Scholar]
- 33.Suyama J, Knutsen CC, Northington WE, Hahn M, Hostler D: IO versus IV access while wearing personal protective equipment in a HazMat scenario. Prehosp Emerg Care. 2007; 11:467–72 [DOI] [PubMed] [Google Scholar]
- 34.Headley DB, Hudgens GA, Cunningham D: The impact of chemical protective clothing on military operational performance. Military Psychology. 2009;9:359–74 [Google Scholar]
- 35.Chen J, Lu KZ, Yi B, Chen Y: Chest compression with personal protective equipment during cardiopulmonary resuscitation: A randomized crossover simulation study. Medicine (Baltimore). 2016; 95:e3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deshayes TA, Jeker D, Goulet EDB: Impact of pre-exercise hypohydration on aerobic exercise performance, peak oxygen consumption and oxygen consumption at lactate threshold: A systematic review with meta-analysis. Sports Med. 2020; 50:581–96 [DOI] [PubMed] [Google Scholar]
- 37.AlGhamri AA, Murray SL, Samaranayake VA: The effects of wearing respirators on human fine motor, visual, and cognitive performance. Ergonomics. 2013; 56:791–802 [DOI] [PubMed] [Google Scholar]
- 38.Darke S: Anxiety and working memory capacity. Cogn Emot. 1988;2:145–54 [Google Scholar]
- 39.Rubenstein CD, DenHartog EA, Deaton AS, Bogerd CP, DeKant S: Fluid replacement advice during work in fully encapsulated impermeable chemical protective suits. J Occup Environ Hyg. 2017; 14:448–55 [DOI] [PubMed] [Google Scholar]
- 40.Clebone A, Burian BK, Tung A: Matching design to use: A task analysis comparison of three cognitive aid designs used during simulated crisis management. Can J Anaesth. 2019; 66:658–71 [DOI] [PubMed] [Google Scholar]
- 41.Sprecher AG, Caluwaerts A, Draper M, Feldmann H, Frey CP, Funk RH, Kobinger G, Le Duc JW, Spiropoulou C, Williams WJ: Personal protective equipment for filovirus epidemics: A call for better evidence. J Infect Dis. 2015; 212 Suppl 2:S98–S100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ortega R, Bhadelia N, Obanor O, Cyr K, Yu P, McMahon M, Gotzmann D: Videos in clinical medicine: Putting on and removing personal protective equipment. N Engl J Med. 2015; 372:e16. [DOI] [PubMed] [Google Scholar]
- 43.Powell JB, Kim JH, Roberge RJ: Powered air-purifying respirator use in healthcare: Effects on thermal sensations and comfort. J Occup Environ Hyg. 2017; 14:947–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fogel I, David O, Balik CH, Eisenkraft A, Poles L, Shental O, Kassirer M, Brosh-Nissimov T: The association between self-perceived proficiency of personal protective equipment and objective performance: An observational study during a bioterrorism simulation drill. Am J Infect Control. 2017; 45:1238–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon JH, Burnham CD, Reske KA, Liang SY, Hink T, Wallace MA, Shupe A, Seiler S, Cass C, Fraser VJ, Dubberke ER: Assessment of healthcare worker protocol deviations and self-contamination during personal protective equipment donning and doffing. Infect Control Hosp Epidemiol. 2017; 38:1077–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mumma JM, Durso FT, Ferguson AN, Gipson CL, Casanova L, Erukunuakpor K, Kraft CS, Walsh VL, Zimring C, DuBose J, Jacob JT; Centers for Disease Control and Prevention Epicenters Program, Division of Healthcare Quality Promotion: Human factors risk analyses of a doffing protocol for ebola-level personal protective equipment: Mapping errors to contamination. Clin Infect Dis. 2018; 66:950–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.John A, Tomas ME, Hari A, Wilson BM, Donskey CJ: Do medical students receive training in correct use of personal protective equipment? Med Educ Online. 2017; 22:1264125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Angeli E, Norwood C: Responding to public health crises: Bridging collective mindfulness and user experience to create communication interventions. Commun Des Q. 2017;5:29–39 [Google Scholar]
- 49.Herlihey TA, Gelmi S, Cafazzo JA, Hall TNT: The impact of environmental design on doffing personal protective equipment in a healthcare environment: A formative human factors trial. Infect Control Hosp Epidemiol. 2017; 38:712–7 [DOI] [PubMed] [Google Scholar]
- 50.Godden DR, Baddeley AD: Context-dependent memory in two natural environments: On land and underwater. British Journal of Psychology. 1975;66:325–31 [Google Scholar]
- 51.Hanczakowski M, Zawadzka K, Collie H, Macken B: Metamemory in a familiar place: The effects of environmental context on feeling of knowing. J Exp Psychol Learn Mem Cogn. 2017; 43:59–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang Y, Jackson T, Cai L: Causal effects of threat and challenge appraisals on coping and pain perception. Eur J Pain. 2016; 20:1111–20 [DOI] [PubMed] [Google Scholar]
- 53.Chen S, Jackson T: Causal effects of challenge and threat appraisals on pain self-efficacy, pain coping, and tolerance for laboratory pain: An experimental path analysis study. PLoS One. 2019; 14:e0215087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moran TP: Anxiety and working memory capacity: A meta-analysis and narrative review. Psychol Bull. 2016; 142:831–64 [DOI] [PubMed] [Google Scholar]
- 55.Johnson DC, Thom NJ, Stanley EA, Haase L, Simmons AN, Shih PA, Thompson WK, Potterat EG, Minor TR, Paulus MP: Modifying resilience mechanisms in at-risk individuals: A controlled study of mindfulness training in Marines preparing for deployment. Am J Psychiatry. 2014; 171:844–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chughtai AA, Chen X, Macintyre CR: Risk of self-contamination during doffing of personal protective equipment. Am J Infect Control. 2018; 46:1329–34 [DOI] [PubMed] [Google Scholar]
- 57.Lebares CC, Guvva EV, Olaru M, Sugrue LP, Staffaroni AM, Delucchi KL, Kramer JH, Ascher NL, Harris HW: Efficacy of mindfulness-based cognitive training in surgery: Additional analysis of the mindful surgeon pilot randomized clinical trial. JAMA Netw Open. 2019; 2:e194108. [DOI] [PMC free article] [PubMed] [Google Scholar]


