Abstract
BACKGROUND:
Early identification of myocardial infarction (MI) is a determinant in the provision of appropriate treatment modalities. The focus of the present study is on the identification of gender-based differences in risk factors, clinical manifestations, and coronary angiography findings in patients presenting with MI.
MATERIALS AND METHODS:
A cross-sectional study was conducted among patients admitted with MI at a tertiary care center in South India during March 2016 to June 2017. Selected 120 male and 120 female consecutive patients admitted with acute MI, who had survived and been stabilized. Data was collected using a pre-tested structure data sheet. Appropriate parametric and nonparametric tests were used to analyze the data.
RESULTS:
Participants were homogenous as regards age (P < 0.107); majority of men and women were from the rural areas. About 32.5% of the men interpreted the pain as due to a cardiac problem or indigestion, whereas 60.8% of the women thought it was fatigue/muscle pain. The self-interpretation or perception of pain in both genders was statistically significant (P < 0.001). Compared to the men, the females increasingly presented with atypical symptoms (P = 0.005). Regarding ST-elevated MI, male preponderance was noted (P = 0.004)). Considering the anatomical location of MI, the presentation of Inferior Wall Myocardial Infarction (IWMI) was predominant in females compared to men (P = 0.003). The majority of men had increased presentation of single-vessel disease compared to women (P = 0.02), whereas normal coronaries and double-vessel disease were found statistically significantly higher in females (P = 0.03 and P = 0.008, respectively).
CONCLUSION:
Public education is needed on the atypical presentations which are common with women than in men. The public should, therefore, be informed of those symptoms and how to recognize them so that they may seek medical care promptly.
Keywords: Atypical symptoms, chest pain, gender difference in myocardial infarction, myocardial infarction
Introduction
Cardiovascular diseases (CVDs) have become an important cause of mortality. This epidemiological alteration is mainly due to the increase in the prevalence of CVDs and CVD risk factors.[1] Coronary artery disease (CAD) is of significant human cost and financial burden worldwide. Individuals lifestyle, hereditary history, and environmental factors are the risk factors in the development of the CVD.[2,3] CAD develops as a result of plague deposition within coronary arteries that are responsible for blood supply to heart muscles leading to a condition known as atherosclerosis.[4] Atherosclerotic changes result in the narrowing of the coronary arteries and reduced blood flow to the heart. Myocardial infarction (MI) occurs as a result of prolonged myocardial cell ischemia with the involvement of myocardial necrosis that may lead to traumatic events that are life-threatening and uneventful.[1] Acute MI (AMI) is one of the most significant CVDs with significant morbidity and mortality. Although atherosclerotic plaque rupture with acute thrombosis development is shared pathology by both men and women, women reportedly have a lower incidence of MI, though with higher mortality.[5]
Gender differences in clinical presentation contribute to the outcome as patients with typical symptoms of CAD tend to seek early treatment than the patients with atypical symptoms. Since health-care workers often assess chest pain and its associated symptoms as primary symptoms, patients with atypical symptoms go unnoticed resulting in early discharge from emergency departments.[6,7] Although coronary plaque rupture with acute thrombosis formation is a common pathophysiology for men and women, women are usually older than men, with a low incidence of AMI, but with an increased atypical manifestations and greater mortality.[8]
There is a need to find current evidence of clinical presentations of symptoms following AMI in both men and women, but with greater focus on women with cardiovascular risk to make their management more evidence based.[6] Medical care and technologies have greatly improved and facilitated access to health care . However, primary prevention strategies of CVDs have not reached the common people.[9,10] This study was mainly to identify the gender-based difference in risk factors, clinical manifestations, and coronary angiography findings in patients presenting with MI.
Materials and Methods
This cross-sectional study was conducted among patients admitted with MI at a tertiary care center in South India during March 2016 to June 2017. Selected 120 male and 120 female consecutive patients admitted with acute MI, who had survived and been stabilized. Considering proportion of males and females with atypical clinical features as 29% and 42%, respectively, the finite population of MI patients admitted in Emergency. Department during the study period as 250, and relative precision of 20%, alpha = 5%, and power = 80%, the calculated sample size in each group was 114. Considering 5% attrition rate, the final sample size of each arm was 120.
Structured participant datasheet had sociodemographic data, clinical presentation survey, clinical variables including electrocardiogram findings, an anatomical area involved, left ventricular ejection fraction details, location of MI, and prehospitalization delay and coronary angiogram findings. It was developed through extensive literature review followed by the validation of contents of participants' datasheet by experts in cardiology. The developed participant datasheet was translated into the local language and retranslated into English. Pretesting of the participant datasheet was done on 10 patients who were admitted into the cardiology department. The patients found clinical presentation survey and sociodemographic components comprehensible. Reliability of the participant datasheet was assessed by the test–retest method. The value of 'r' was established at 0.9.
Ethical approval was obtained from the Institutional Ethics Committee vide Letter No. JIP/IEC/2016/1110 dated 30/01/2016. Informed written consent was taken from all participants.
Sociodemographic variables, including age, sex, income, education, domicile, and occupation, were analyzed using the descriptive statistics including frequency with percentage, mean, and standard deviation. The Chi-square test was used as a test of significance to analyze the difference in risk factor profiles in men and women. The Chi-square test and Fisher's exact test was used as a test of significance to analyze the difference in clinical profile and coronary angiogram profile in men and women.
Results
In this study, the participants were homogeneous with regard to age (P = 0.107). However, the educational qualification of males was higher than females (P = 0.003). The majority of men and women were from the rural areas and more women than men were unemployed (P < 0.001) [Table 1].
Table 1.
Sociodemographic variables of men and women with myocardial infarction (n=240)
| Variables | Male (n=120) N (%) | Female (n=120) N (%) | P-value# |
|---|---|---|---|
| Age, mean±SD | 54.8±10.04 | 56.8±9.84 | 0.107 |
| Education | |||
| Illiterate | 34 (28.3) | 61 (50.8) | 0.003 |
| Primary education | 70 (58.3) | 52 (43.3) | |
| Higher education | 8 (6.7) | 4 (3.3) | |
| Graduate/postgraduate | 8 (6.7) | 3 (2.5) | |
| Domicile | |||
| Urban | 14 (11.7) | 26 (21.7) | 0.038 |
| Rural | 106 (88.3) | 94 (78.3) | |
| Occupation | |||
| Unemployed | 26 (21.7) | 93 (77.5) | <0.001 |
| Skilled workers | 93 (77.5) | 25 (20.8) | |
| Professional workers | 1 (0.8) | 2 (1.7) |
#Chi-square test. SD=Standard deviation
The difference in self-perception or interpretation by the two genders of myocardial chest pain reported as due to other illness has been shown in Table 2. This study revealed that 32.5% of men interpreted chest pain as due to indigestion/stomach problem, whereas majority of the women interpreted it as due to fatigue/muscle pain (60.8%) and indigestion (15.5%). Overall, the self-perception or interpretation of myocardial pain as of noncardiac origin by both genders was statistically significant (P < 0.000). When compared to men, females increasingly presented with atypical symptoms such as dizziness, sweating, shortness of breath, vomiting, palpitation, fainting, back pain, and fatigue (P = 0.005).
Table 2.
Comparison of self-interpretation of chest pain and presence of atypical manifestations of men and women with myocardial infarction (n=240)
| Variables | Male (n=120) N (%) | Female (n=120) N (%) | P-value |
|---|---|---|---|
| Self-interpreted of chest pain as | |||
| Related to heart | 39 (32.5) | 13 (10.8) | <0.001* |
| Indigestion or stomach problem | 39 (32.5) | 19 (15.8) | |
| Fatigue/muscle pain | 29 (24.2) | 73 (60.8) | |
| Related to stress | 2 (1.7) | 12 (10.0) | |
| Related to diabetes/hypertension | 7 (5.8) | 10 (8.4) | |
| Breathing problem | 0 | 1 (1.8) | |
| Thyroid problem | 1 (0.8) | 4 (3.3) | |
| Due to smoking | 5 (4.1) | 0 | |
| Presence of atypical clinical presentations | 84 (70.0) | 102 (85.0) | 0.005 |
#Pearson Chi-square test
Risk factors such as, diabetes, hypertension, known history of IHD and obesity were still observed more often in women, whereas smoking as a risk factor was noted only in men. Regarding ST-elevated MI (STEMI), male preponderance was noted whereas, women increasingly presented with non-STEMI (NSTEMI) which was significant (P = 0.004). Considering anatomical location of MI, presentation of IWMI was more predominant in females than men (P = 0.003), and the groups were homogenous in the presentation of other types of MI. Prehospitalization delay between groups was found to be nonsignificant (P = 0.160). Compared to men, a smaller proportion of the women had thrombolysis (P = 0.041) [Table 3].
Table 3.
Clinical presentation survey of men and women with myocardial infarction (n=240)
| Variables | Male (n=120) N (%) | Female (n=120) N (%) | P-value |
|---|---|---|---|
| Risk factors survey | |||
| Smoking | 72 (60.0) | 0 | <0.001 |
| Hypertension | 51 (42.5) | 75 (62.5) | 0.002 |
| Diabetes | 53 (44.2) | 65 (54.2) | 0.121 |
| Dyslipidemia | 21 (17.5) | 24 (20.0) | 0.620 |
| Prior PCI | 8 (6.7) | 2 (1.7) | 0.053 |
| Co-morbid illness | |||
| Known IHD | 17 (14.2) | 39 (32.5) | 0.001 |
| Co-morbidities | 103 (85.8) | 81 (67.5) | |
| ECG findings | |||
| STEMI | 83 (69.2) | 61 (50.8) | 0.004 |
| NSTEM | 37 (30.8) | 59 (49.2) | |
| Treated with thrombolysis | 39 (32.5) | 25 (20.8) | 0.041 |
| LVEF findings (%) | |||
| >50 | 52 (43.3) | 60 (50.0) | 0.483 |
| 40-50 | 52 (43.3) | 43 (35.8) | |
| <40 | 16 (13.3) | 17 (14.2) | |
| Location of MI | |||
| Anterior | 47 (56.6) | 30 (49.2) | 0.148 |
| Antero septal | 5 (6.0) | 2 (3.3) | 0.285 |
| Inferior | 23 (27.7) | 28 (45.9) | 0.003 |
| Inferior posterior | 2 (2.4) | 0 | 0.330 |
| Anterolateral | 4 (4.8) | 1 (1.6) | 0.147 |
| Lateral | 2 (2.4) | 0 | 0.330 |
| Prehospitalization delay (h) | |||
| <3 | 60 (50.0) | 69 (57.5) | <0.160 |
| 3-6 | 10 (8.3) | 11 (9.2) | |
| 6-12 | 11 (9.2) | 16 (13.3) | |
| >12 | 39 (32.5) | 24 (20.0) |
MI: Myocardial infarction, STEMI: ST-elevated myocardial infarction, NSTEMI: Non-STEMI, PCI: Percutaneous coronary intervention, ECG: Electrocardiogram, LVEF: Left ventricular ejection fraction , IHD: Ischemic heart disease
Increased presentation of single-vessel disease (SVD) and triple-vessel disease (TVD) was observed in more males than women (P = 0.02). Normal coronaries and nonobstructive CAD preponderance in coronary angiograms were found to be statistically significantly higher in females (P = 0.018, P = 0.028) [Table 4].
Table 4.
Description of coronary angiography findings among men and women with ST elevated myocardial infarction and non-ST elevated myocardial infarction (n=240)
| Coronary angiogram findings | Male N (%) | Female N (%) | P-value |
|---|---|---|---|
| Patients with STEMI | n=83 | n=61 | |
| Normal coronaries | 0 | 4(6.5) | 0.030# |
| Non-obstructive CAD | 2(2.4) | 3(5.0) | 0.357# |
| Re-canalized coronaries | 1(1.2) | 1(1.5) | 0.669* |
| SVD | 39(47.0) | 19(31.0) | 0.027* |
| DVD | 11(13.3) | 18(30.0) | 0.008* |
| TVD | 30(36.1) | 16(26.2) | 0.103* |
| Patients with NSTEMI | n=37 | n=59 | |
| Normal coronaries | 1(2.7) | 11(18.7) | 0.018# |
| Non-obstructive CAD | 0 | 7(11.8) | 0.028# |
| SVD | 19(51.4) | 22(37.3) | 0.087* |
| DVD | 7(18.9) | 6(10.2) | 0.111* |
| TVD | 10(27.0) | 13(22.0) | 0.288* |
# Fisher’s exact test, *Chi square test. STEMI: ST elevated myocardial infarction, NSTEMI: Non STEMI, SVD: Single vessel disease, DVD: Double vessel disease, TVD: Triple vessel disease, CAD: Coronary artery disease
The occurrence of MI was the highest in the morning hours in males and females [Figure 1]. Compared to females, men also had more MI between 12 am and 6 am (P<0.001) and between 6 am and 12 pm (P=0.004).
Figure 1.
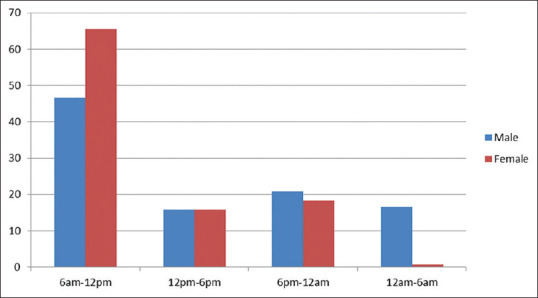
Comparison of time of onset of pain among men and women with myocardial infarction
Discussion
Understanding women's clinical symptoms during AMI and its clinical significance is paramount in the provision of treatment. The present explanation of “typical” cardiac symptoms is based primarily on the experience of white, middle-aged men, with deviations called “atypical.” However, studies[6,11,12,13,14,15] have shown that this tag contributes to misunderstanding by clinicians and lay individuals, leading to inaccurate diagnoses, causing women to delay in seeking treatment.
Accurate information about women's symptoms and their pattern during AMI would provide a normative explanation of women's cardiac symptom experience. In this study, although the predominant symptom exhibited by men and women was chest pain, compared to men, females increasingly presented with atypical presentations such as dyspnea, nausea, vomiting, dizziness, sweating, and back pain. Similar studies with reported high presentation of atypical symptoms such as breathlessness and fatigue, nausea, and vomiting were higher in women.[16,17,18] It has been reported that the presentation of AMI symptoms are similar for young women and men, with chest pain as the predominant symptom for both sexes. Women presented with a greater number of additional nonchest pain symptoms regardless of the presence of chest pain, and both women and their health-care providers rather than men were less likely to attribute their prodromal symptoms to heart disease.[19,20]
The factors related to health-care-seeking behaviors of patients with AMI have been studied widely. Patient's perception or self-interpretation of chest pain contributes significantly to the delay of treatment.[21] The lack of correspondence between expectation and actual symptoms is always associated with longer prehospital delay and decreased use of emergency medical services. In this study, only a small proportion of patients interpreted their discomfort as being of cardiac origin. The majority of the men perceived it as indigestion while women perceived it as of muscular origin or fatigue because their symptoms were atypical 0.[22,23,24,25] Owing to their misperception of the symptoms, one fourth of the males delayed their visit to the emergency department for more than 12 h. Although the current study focused on self-perception of symptoms in both genders, the correlation of self-perception of symptoms and prehospitalization delay was not studied. Several studies have reported longer prehospital delays of participants because of wrong perception of symptoms.[13,20]
The present study shows that the majority of men had presented with STEMI. Several studies have reported findings similar to those of the current study, showing higher prevalence of STEMI in men than women.[9,10,11] This study also noted that prehospitalization delay in both men and women was not significant, although one-fourth of the males delayed their visit to the emergency department by more than 12 h, but this was not statistically significant. Another study confirmed that gender was not a determinant factor for prehospitalization delay.[12,13]
In contrast to these findings, several studies have established an association of female gender as a cause for prehospitalization delay.[15,26,27,28]
Age, dyslipidemia, hypertension, smoking, diabetes, obesity, and physical inactivity are considered the common risk factors for both men and women. Further, women have added risk factors, such as the use of contraceptives and the reduction of ovarian function with age. Besides, coronary heart disease (CHD) was always considered a male problem, partly because of delay of its clinical appearance in women owing to the effect of estrogen, which is thought to be beneficial because of effects on atherosclerotic plaque progression, vasodilatation, blood pressure, and its anti-oxidative and anti-inflammatory properties. Recent studies have emphasized this increase and the fact that CHD is the leading cause of death in women. In our study also, with the exception of smoking its preponderance as a risk factor in females was noted.[29]
Coronary angiography findings of patients with STEMI revealed that a majority of men had presented with increased SVD when compared to women, whereas normal coronaries and double vessel disease (DVD) were significantly higher in females than men. Coronary angiography findings of the patients with NSTEMI revealed that normal coronaries and nonobstructing CAD were statistically significantly higher in females than men (P < 0.01 and P < 0.02, respectively). Similar results reported from previous studies showed that normal coronaries were significantly higher in females than men.[21,22,23] In contrast to the current study, several studies have reported that there was no gender difference in the presentation of SVD[4,21] Conti et al. reported equal prevalence of SVD, DVD, and TVD presentation in both genders.[26] The findings of Bajaj et al. were in conflict with ours, showing a higher prevalence of DVD in men.[6] xHigher presentation of DVD in men with NSTEMI was reported by Sadowski et al.[29]
Limitations
As the data were collected from participants using self-structured questionnaire and interview method, recall bias may have contributed to the loss of some relevant information. Further, the sample size of the study is limited.
Conclusion
Gender-based differences in clinical presentation in men and women with MI had been a focus in research that emphasized the gender-specific approach. The current study also supports the need of a gender-specific approach as women increasingly presented with atypical manifestations and different presentation of coronary angiogram profile. The public has to be made aware of this to avoid the disparities in the treatment and delays in management despite the availability of a multifaceted health-care sector.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bauersachs R, Zeymer U, Brière JB, Marre C, Bowrin K, Huelsebeck M. Burden of coronary artery disease and peripheral artery disease: A Literature review. Cardiovasc Ther. 2019;2019:1–9. doi: 10.1155/2019/8295054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S. A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol. 2019;234:16812–23. doi: 10.1002/jcp.28350. [DOI] [PubMed] [Google Scholar]
- 3.Abdul-Aziz AA, Desikan P, Prabhakaran D, Schroeder LF. Tackling the burden of cardiovascular diseases in India. Circ Cardiovasc Qual Outcomes. 2019;12:e005195. doi: 10.1161/CIRCOUTCOMES.118.005195. [DOI] [PubMed] [Google Scholar]
- 4.Ranjith N, Verho NK, Verho M, Winkelmann BR. Acute myocardial infarction in a young South African Indian-based population: Patient characteristics on admission and gender-specific risk factor prevalence. Curr Med Res Opin. 2002;18:242–8. doi: 10.1185/030079902125000624. [DOI] [PubMed] [Google Scholar]
- 5.Rani SB, Lakshmi R, Pillai AA, Nisha SA. The riskfactors associated with complications of coronary angiogram: A cross sectional Observational Study. Int J Adv Res. 2016;3:11–5. [Google Scholar]
- 6.Bajaj S, Mahajan V, Grover S, Mahajan A, Mahajan N. Gender based differences in risk factor profile and coronary angiography of patients presenting with acute myocardial infarction in north Indian population. J Clin Diagn Res. 2016;10:OC05–7. doi: 10.7860/JCDR/2016/16512.7725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, et al. Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation. 2016;133:916–47. doi: 10.1161/CIR.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 8.Park JS, Kim YJ, Shin DG, Jeong MH, Ahn YK, Chung WS, et al. Gender differences in clinical features and in-hospital outcomes in ST-segment elevation acute myocardial infarction: From the Korean Acute Myocardial Infarction Registry (KAMIR) study. Clin Cardiol. 2010;33:E1–6. doi: 10.1002/clc.20557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kodliwadmath A, Nimbal NV. Sex differences in clinical presentation in acute MI. Int J Adv Med. 2017;4:940–3. [Google Scholar]
- 10.Lichtman JH, Leifheit EC, Safdar B, Bao H, Krumholz HM, Lorenze NP, et al. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: Evidence from the VIRGO study (variation in recovery: Role of gender on outcomes of young AMI patients) Circulation. 2018;137:781–90. doi: 10.1161/CIRCULATIONAHA.117.031650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hao Y, Liu J, Liu J, Yang N, Smith SC, Jr, Huo Y, et al. Sex Differences in in-hospital management and outcomes of patients with acute coronary syndrome. Circulation. 2019;139:1776–85. doi: 10.1161/CIRCULATIONAHA.118.037655. [DOI] [PubMed] [Google Scholar]
- 12.Sadowski M, Gasior M, Gierlotka M, Janion M, Poloński L. Clinical characteristics of Polish women with ST-segment elevation myocardial infarction. Kardiol Pol. 2010;68:627–34. [PubMed] [Google Scholar]
- 13.Zucker DR, Griffith JL, Beshansky JR, Selker HP. Presentations of acute myocardial infarction in men and women. J Gen Intern Med. 1997;12:79–87. doi: 10.1046/j.1525-1497.1997.00011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berg J, Björck L, Dudas K, Lappas G, Rosengren A. Symptoms of a first acute myocardial infarction in women and men. Gend Med. 2009;6:454–62. doi: 10.1016/j.genm.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Duraes AR, Bitar YS, Freitas ACT, Filho IM, Freitas BC, Fernandez AM. Gender differences in ST-elevation myocardial infarction (STEMI) time delays: Experience of a public health service in Salvador-Brazil. Am J Cardiovasc Dis. 2017;7:102–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Butala NM, Desai MM, Linnander EL, Wong YR, Mikhail DG, Ott LS, et al. Gender differences in presentation, management, and in-hospital outcomes for patients with AMI in a lower-middle income country: Evidence from Egypt. PLoS One. 2011;6:e25904. doi: 10.1371/journal.pone.0025904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu CH, Huang YC. Comparison of STEMI and NSTEMI patients in the emergency department. JACME. 2011;1:1–4. [Google Scholar]
- 18.George L, Ramamoorthy L, Satheesh S, Saya RP, Subrahmanyam DK. Prehospital delay and time to reperfusion therapy in ST elevation myocardial infarction. J Emerg Trauma Shock. 2017;10:64–9. doi: 10.4103/0974-2700.201580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farshidi H, Rahimi S, Abdi A, Salehi S, Madani A. Factors associated with pre-hospital delay in patients with acute myocardial infarction. Iran Red Crescent Med J. 2013;15:312–6. doi: 10.5812/ircmj.2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: Experience in 4 US communities from 1987-2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 21.Kendall H, Marley A, Patel JV, Khan JM, Blann AD, Lip GY, et al. Hospital delay in South Asian patients with acute ST-elevation myocardial infarction in the UK. Eur J Prev Cardiol. 2013;20:737–42. doi: 10.1177/2047487312447844. [DOI] [PubMed] [Google Scholar]
- 22.Ottesen MM, Dixen U, Torp-Pedersen C, Køber L. Prehospital delay in acute coronary syndrome--an analysis of the components of delay. Int J Cardiol. 2004;96:97–103. doi: 10.1016/j.ijcard.2003.04.059. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: A systematic review. Circ Cardiovasc Qual Outcomes. 2010;3:82–92. doi: 10.1161/CIRCOUTCOMES.109.884361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobs AK. Coronary intervention in 2009: Are women no different than men? Circ Cardiovasc Interv. 2009;2:69–78. doi: 10.1161/CIRCINTERVENTIONS.108.847954. [DOI] [PubMed] [Google Scholar]
- 25.Ghazaway ER, Seedhom AE, Mahfouz EM. Predictors of delay in seeking health care among myocardial infacrtion patients, Minia district, Egypt. Adv Prev Med. 2015;2015:342–61. doi: 10.1155/2015/342361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conti RA, Solimene MC, da Luz PL, Benjo AM, Lemos Neto PA, Ramires JA. Comparison between young males and females with acute myocardial infarction. Arq Bras Cardiol. 2002;79:510–25. doi: 10.1590/s0066-782x2002001400009. [DOI] [PubMed] [Google Scholar]
- 27.Leaf DA, Sanmarco ME, Bahl RA. Gender differences in coronary angiographic findings from 1972 through 1981 in Los Angeles, California. Angiology. 1990;41:609–15. doi: 10.1177/000331979004100804. [DOI] [PubMed] [Google Scholar]
- 28.Mega JL, Hochman JS, Scirica BM, Murphy SA, Sloan S, McCabe CH, et al. Clinical features and outcomes of women with unstable ischemic heart disease: Observations from metabolic efficiency with ranolazine for less ischemia in non-ST-elevation acute coronary syndromes-thrombolysis in myocardial infarction 36 (MERLIN-TIMI 36) Circulation. 2010;121:1809–17. doi: 10.1161/CIRCULATIONAHA.109.897231. [DOI] [PubMed] [Google Scholar]
- 29.Sadowski M, Gutkowski W, Raczyński G, Janion-Sadowska A, Gierlotka M, Poloński L. Acute myocardial infarction due to left main coronary artery disease in men and women: Does ST-segment elevation matter? Arch Med Sci. 2015;11:1197–204. doi: 10.5114/aoms.2015.56345. [DOI] [PMC free article] [PubMed] [Google Scholar]


