Abstract
Introduction
Non-ischaemic heart disease (NIHD) is the underlying pathology in∼20% of all sudden cardiac deaths (SCDs). Heavy drinking is known to be associated with SCD due to ischaemic heart disease, but studies on association of recent alcohol consumption and SCD in patients with NIHD are scarce. We evaluated the blood alcohol levels of autopsy verified non-ischaemic SCD victims.
Methods
Study population was derived from the Finnish Genetic Study of Arrhythmic Events (Fingesture) (n = 5869, mean age 65 ± 12, 79% males). All deaths occurred in Northern Finland during 1998–2017. All victims underwent a medico-legal autopsy. Subjects of SCD due to ischaemic heart disease were excluded.
Results
A total of 1301 (mean age 57 ± 12, 78% males) victims of SCD due to NIHD were included in the study. The blood ethanol level was elevated in 543 (42%) subjects, out of which the blood alcohol level was ≥0.10%in 339 (62%) subjects and ≥0.15%in 252 (46%) subjects. Male SCD victims had alcohol in blood more frequently compared to females (45% versus 31%, p < .001).
Conclusion
Elevated blood alcohol level is common in SCD victims due to NIHD, especially in males. Recent alcohol consumption might contribute to the subsequent SCD in many non-ischaemic SCD victims.
KEY MESSAGES
Elevated blood alcohol level is common in victims of sudden cardiac death due to non-ischaemic heart disease, especially in males.
Recent alcohol consumption may contribute to the subsequent death in many nonischemic sudden cardiac death victims.
Keywords: Alcohol, non-ischaemic heart disease, sudden cardiac death, medico-legal autopsy
Introduction
Non-ischaemic heart disease (NIHD) consists of a diverse group of diseases, such as cardiomyopathies and inherited ion channel disorders, and accounts for about 20% of all sudden cardiac deaths (SCDs) [1]. The incidence of SCD in general and SCD from ischaemic heart disease seems to be declining, whereas the incidence of SCD from NIHD may have remained in the same level or even increased [2,3]. The three-year mortality rate of patients with severe NIHD with decreased left ventricular systolic function is approximately 12–20% [4,5]. Chronic heavy drinking can lead to alcoholic cardiomyopathy (CM), which is a common subtype of NIHD [1,6].
The role of alcohol in the development of SCD is a controversial subject. High alcohol consumption has long been known as a risk factor for SCD [7]. Light-to-moderate alcohol use has been reported to increase cardiovascular health and reduce the risk for SCD, [8,9]. but these findings have also been criticised [10]. Heavy drinking and especially binge drinking has been associated with SCD in patients with coronary artery disease in multiple studies [7,11]. Perkiömäki et al reported elevated blood alcohol levels in 38% of 1691 autopsied victims of SCD due to ischaemic heart disease [12]. While the risk for SCD due to heavy drinking is well established in patients with coronary artery disease, the association of recent alcohol consumption with SCD in patients with NIHD has not been largely studied. Our aim was to determine the blood alcohol levels of autopsy verified NIHD SCD victims.
Materials and methods
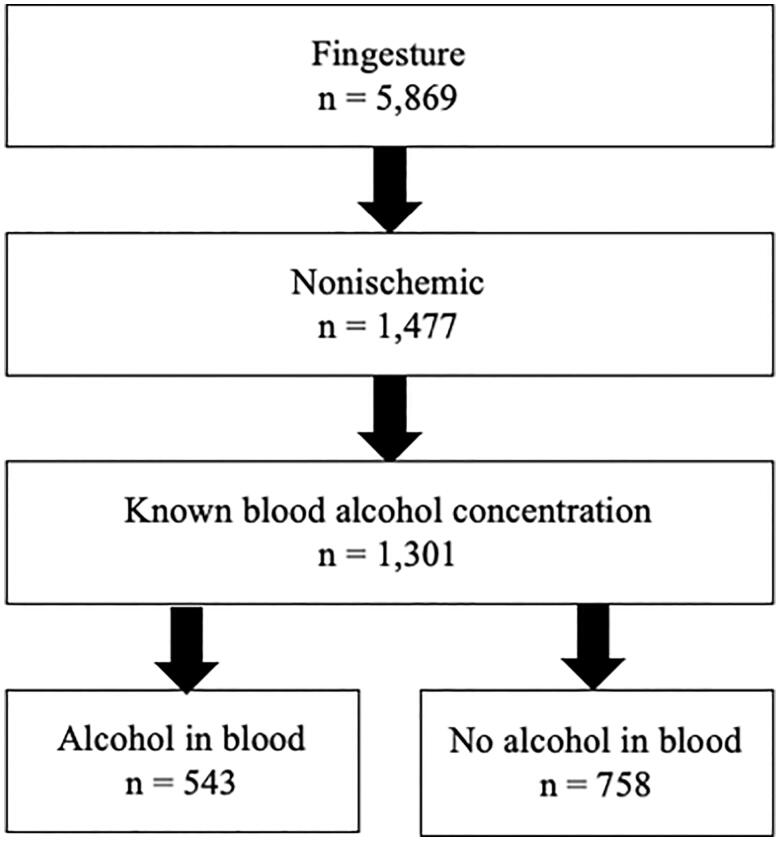
Study population was derived retrospectively from the Finnish Genetic Study of Arrhythmic Events (Fingesture) which consists of 5869 (mean age 65 ± 12, 79% males) victims of SCD due to cardiac causes. This cohort study was designed to systematically collect information of all SCDs occurring in Province of Oulu, Northern Finland. All victims died between years 1998 and 2017 and were autopsied by experienced forensic pathologists. The medico-legal autopsies were performed at the Department of Forensic Medicine of the University of Oulu and Finnish Institute for Health and Welfare, Oulu, Finland. According to Finnish law, medico-legal autopsy is to be performed to all victims of sudden death if the patient has not been treated by physicians during their last illness, if the death is not due to a pre-existing known disease or it is otherwise unexpected. A death was considered sudden if it was witnessed within 6 h of the onset of symptoms or the person was last seen alive less than 24 h ago. The criteria for sudden death used in the Fingesture have been discussed in our previous study by Haukilahti et al. [13]. All autopsies included histologic examination. Toxicologic investigation was performed in cases with suspicion of toxic exposure, and all cases of intoxication and alcohol poisoning were excluded. The blood ethanol level of the subjects was determined by post-mortem gas chromatography in the Forensic Toxicology Unit, Finnish Institute for Health and Welfare, Helsinki, Finland. Blood alcohol concentrations ≥0.02% were considered positive/elevated. The post-mortem time intervals in Finland are on average about 5 days from death to autopsy and 2-3 weeks from death to toxicology investigation [14]. The probability of ethanol synthesis or other post-mortem factors influencing the toxicology results is considered small. In this study, SCD is defined as a sudden death of cardiac cause, as the study population did not include any cases of sudden death due to non-cardiac causes. Cases of SCD due to ischaemic heart disease (n = 4392) and cases with no information on blood alcohol level (n = 176) were excluded. The selection of the study population is illustrated in Figure 1.
Figure 1.
Flow chart of the study population.
Data on the subjects was gathered from autopsy reports, which included a death certificate and previous medical records, and questionnaires to closest family members. The expression “known heavy drinker” was used of a subject if they consumed large amounts of alcohol regularly. This information was documented in previous medical records over time by multiple physicians during a clinical assessment of the patient. In Finland, the definition of high-risk alcohol consumption is more than 16 drinks per week for females and 24 for males. While no information about specific consumption or duration of alcohol use of the subjects was available retrospectively, these definitions were probably used as a reference for heavy drinking.
The causes of death were reported according to ICD-10 code classes, and the more detailed classification of NIHD was based on the post-mortem findings being in conjunction with medical records and questionnaires. The underlying heart disease was known before death in only 33% of the cases. The subtypes of NIHD were classified as hypertensive CM, CM related to obesity, alcoholic CM, fibrotic CM, dilated CM, hypertrophic CM, myocarditis, valvular heart disease, arrhythmogenic right ventricular CM, anomalous coronary arteries, unspecified CM and structurally normal heart. Victims with a structurally normal heart were tested for long QT syndrome mutations. The definitions of these subtypes of NIHD are shown in Table 1 and have also been described in earlier Fingesture studies [1]. Stages of fatty liver and hepatic cirrhosis were determined during autopsy in a macroscopic and/or microscopic examination of the liver.
Table 1.
Autopsy-based definitions of the subtypes of nonischemic heart disease (NIHD).
| Causes of nonischemic SCD | Definition of the subtype of NIHD based on autopsy |
|---|---|
| Hypertensive CM | LVH, increased heart weight, unspecific fibrosis, other organ changes related to hypertension (e.g. arterial medial hypertrophy, intimal fibrosis in renal arterioles). |
| CM related to obesity | LVH or both left and right ventricular wall hypertrophy, increased heart weight, dilation of ventricles and atria, excessive epicardial and myocardial fat, obesity. |
| Alcoholic CM or unspecified CM | Focal replacement fibrosis of the myocardium, increased heart weight and LVH. In later stages, signs of dilated cardiomyopathy, other organ changes related to excessive long-term alcohol consumption (e.g. liver cirrhosis and/or severe steatosis, pancreatic fibrosis). |
| Fibrotic CM | Diffuse, interstitial or patchy myocardial fibrosis without myocardial scarring, LVH, or other apparent cause for fibrosis. |
| DCM | Left ventricular dilation with inadequate degree of LVH, unspecific fibrosis and focal atrophy or hypertrophy of myocytes. In later stages, pale and flabby myocardium and dilation of ventricles and atria. |
| HCM | Concentric LVH with myocyte disarray and various degrees of interstitial fibrosis, often asymmetrical septal hypertrophy. |
| Myocarditis | Inflammatory infiltration of the myocardium with necrosis and/or degeneration of the adjacent myocytes. |
| Valvular heart disease | Aortic or mitral valve calcification |
| ARVC | Right ventricular dilation, right ventricular myocardial atrophy with fibro fatty replacement of myocytes. |
| Anomalous coronary arteries | Anomalies of origination, course or coronary termination. Anomalous collateral vessels, anomalies of intrinsic coronary arterial anatomy. |
| Structurally normal heart | Macroscopically and microscopically normal heart with or without long QT syndrome mutations |
ARVC: Arrhythmogenic right ventricular cardiomyopathy; CM: cardiomyopathy; DCM: dilated cardiomyopathy; HCM: hypertrophic cardiomyopathy, LVH: left ventricular hypertrophy.
The study complies with the Declaration of Helsinki and was approved by the ethics committee of Northern Ostrobothnia Hospital district (Oulu University Hospital). Permissions to review the medico-legal autopsy data were gained from the Finnish National Institute for Health and Welfare and the Regional State Administrative Agency of Northern Finland.
Statistical analysis
Chi-square test was used to detect significant differences in the distribution of dichotomised variables and Fisher’s exact test was used when a cell count was less than five, and thus, the assumptions for validity of the Chi-square test were violated. Gaussian distribution of variables was evaluated by skewness test. When comparing continuous variables of two groups, independent samples t-test was used for variables with normal distribution and Mann–Whitney test for variables with non-normal distribution. The IBM Statistical Package for Social Studies 25 (SPSS Inc., Chicago, IL) was used to perform the analyses, and two-sided p-values <.05 were considered statistically significant.
Results
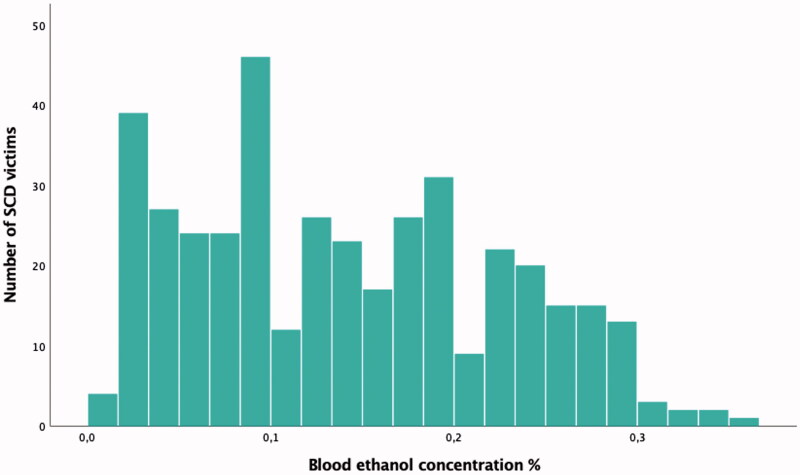
A total of 1301 (mean age 57 ± 12, 78% males) victims of SCD due to NIHD were included in the study. .The characteristics of the study population are shown in Table 2. The blood ethanol level was elevated in 543 (42%) subjects, out of which the concentration of alcohol was ≥0.10% in 339 (62%) subjects and ≥0.15% in 252 (46%) subjects. The alcohol concentration of subjects with elevated blood ethanol level is shown in Figure 2. The group with alcohol in blood had more males than the group with no alcohol in blood, and male SCD victims had more frequently alcohol in blood compared to females (45% versus 31%, p < .001). Among males with alcohol in blood, the concentration of alcohol was ≥0.10%in 282 (62%) subjects and ≥0.15% in 213 (47%) subjects. Among females with alcohol in blood, the concentration of alcohol was ≥0.10% in 57 (63%) subjects and ≥0.15% in 39 (43%) subjects. The medians of concentrations of alcohol between males with alcohol in blood and females with alcohol in blood were similar (0.14% versus 0.13%, p = .476). Out of all victims of NIHD SCD, 664 (51%) were known to be heavy drinkers. Subjects with alcohol in blood were more often known heavy drinkers than subjects with no alcohol in blood (61% versus 44%, p < .001). Within known heavy drinkers (n = 664), alcohol blood test was positive in 329 (50%).
Table 2.
Characteristics of the study population and subgroups.
| Total n = 1,301 |
Victims with alcohol in blood n = 543 (42 %) |
Victims with no alcohol in blood n = 758 (58 %) |
p Value | |
|---|---|---|---|---|
| Age, years (mean ± standard deviation) | 57 ± 12 | 58 ± 11 | 56 ± 13 | .067 |
| Gender, male | 78 % | 83 % | 74 % | <.001 |
| BMI, kg/m2 (mean ± standard deviation) | 30 ± 8.1 | 30 ± 7.8 | 30 ± 8.3 | .747 |
| Diabetes, % | 19 % | 20 % | 19 % | .925 |
| Hypertensiona, % | 42 % | 47 % | 39 % | .007 |
| Moderate or severe fatty liver in autopsyb | 57 % | 63 % | 53 % | <.001 |
| Any stage of hepatic cirrhosis in autopsyb | 34 % | 37 % | 32 % | .067 |
| Time of death (24-06/06-12/12-18/18-24/unknown) % | 9/8/7/7/69 | 9/7/5/7/72 | 9/9/8/7/68 | .293 |
| Hypertensive CM n = 351 | 8/6/7/8/71 | 9/5/5/9/72 | 7/7/8/7/70 | .489 |
| CM related to obesity n = 307 | 13/9/12/9/57 | 10/10/10/12/58 | 16/8/13/7/56 | .161 |
| Alcoholic CM n = 289 | 5/6/4/2/83 | 4/5/4/2/84 | 6/6/4/3/82 | .994 |
| Fibrotic CM n = 170 | 11/6/6/5/73 | 14/3/2/0/81 | 9/7/8/7/69 | .050 |
BMI: body mass index; CM: cardiomyopathy.
aMissing data from 39 subjects.
bMissing data from 1 subject.
Figure 2.
Blood ethanol concentration in 543 victims of sudden cardiac death(SCD) with elevated blood alcohol level.
The causes of SCD due to NIHD are presented in Table 3. The most prevalent causes of death were hypertensive CM (27%), CM related to obesity (24%), alcoholic CM (22%) and fibrotic CM (13%). Out of 13 subjects with structurally normal heart, long QT syndrome mutation was found in 4 (31%) subjects. When compared to other types of NIHD, hypertensive CM, fibrotic CM, myocarditis and valvular heart disease were associated with elevated blood alcohol level (Table 3).
Table 3.
Types of underlying nonischemic heart disease (NIHD) in subjects with alcohol in blood and subjects with no alcohol in blood.
| Causes of nonischemic SCD | All victims of nonischemic SCD n = 1,301 (%) |
Victims with alcohol in blood n = 543 (42 %) |
Victims with no alcohol in blood n = 758 |
p Value |
|---|---|---|---|---|
| Hypertensive CM | 351 (27a) | 162 (46b) | 189 (54c) | .050 |
| CM related to obesity | 307 (24) | 135 (44) | 172 (56) | .363 |
| Alcoholic CM | 289 (22) | 135 (47) | 154 (53) | .052 |
| Fibrotic CM | 170 (13) | 58 (34) | 112 (66) | .031 |
| DCM | 39 (3) | 13 (33) | 26 (67) | .280 |
| HCM | 30 (2) | 14 (47) | 16 (53) | .580 |
| Myocarditis | 46 (4) | 9 (20) | 37 (80) | .002 |
| Valvular heart disease | 44 (3) | 10 (23) | 34 (77) | .009 |
| ARVC | 5 (0) | 3 (60) | 2 (40) | .655 |
| Anomalous coronary arteries | 4 (0) | 0 (0) | 4 (100) | .145 |
| Unspecified CM | 3 (0) | 0 (0) | 3 (100) | .270 |
| Structurally normal heart | 13 (1) | 4 (31) | 9 (69) | .575 |
ARVC: Arrhythmogenic right ventricular cardiomyopathy; CM: cardiomyopathy; DCM: dilated cardiomyopathy; HCM: hypertrophic cardiomyopathy.
aPercentage of cause of death within all victims.
bPercentage of cases with alcohol in blood.
cPercentage of cases with no alcohol in blood.
Discussion
Elevated blood alcohol level was observed in more than 4 out of 10 victims of non-ischaemic SCD and was more common in males compared to females. Hypertensive CM, fibrotic CM, myocarditis and valvular heart disease were associated with a positive blood alcohol test.
Extensive research has been done on the effects of alcohol on the cardiovascular system. Acute alcohol intake increases blood pressure, promotes neurohormonal stimulation and causes left ventricular dysfunction, which may last for a few days even after withdrawing from alcohol [15,16]. As a part of the Fingesture study, Perkiömäki et al. [12] reported elevated blood alcohol levels in 38% of 1,691 autopsied victims of SCD due to ischaemic heart disease, suggesting an association between acute alcohol intake and increased risk of SCD in patients with coronary artery disease. Sjögren et al.17 demonstrated elevated blood alcohol levels in 39% of 15,630 autopsied victims of all types of unnatural deaths. Chronic drinking seems to have both favourable and harmful effects on the heart. Light-to-moderate alcohol consumption (two to six standard drinks per week) has been reported to lower blood pressure and have beneficial effects on haemostatic factors, lipoproteins and inflammatory markers, lowering the risk of coronary artery disease, myocardial infarction, and death from cardiovascular disease [16,18]. However, some studies have been criticized for classifying ex-drinkers in the same category as non-drinkers, which might result in a bias towards light-to-moderate drinkers [10]. Chronic heavy drinking (more than six standard drinks per day) is associated with hypertension, myocyte hypertrophy and increased cortisol and cholesterol levels, increasing the risk of myocardial infarction, dilated CM, heart failure and cardiac arrhythmias [7,16,19]. Binge drinking, or heavy episodic drinking, is associated with myocardial inflammation and arrhythmias, such as atrial fibrillation, ventricular tachycardia and ventricular fibrillation [6].
NIHD consists of various different conditions, such as CMs, myocarditis and valvular heart disease. CMs compose the majority of NIHD [1]. Inherited ion channel disorders, such as long QT syndrome, are a type of NIHD and one possible explanation for SCD in victims with a structurally normal heart in autopsy [1]. The three-year mortality rate of severe NIHD with reduced left ventricular ejection fraction (<35%) is approximately 12–20%, with death resulting typically from ventricular arrhythmias or heart failure [4,5]. NIHD is responsible for about 30–40% cases of heart failure [20]. Patients with CMs develop progressive heart failure and structural changes, such as hypertrophy, fatty or fibrotic infiltration, chamber dilation and reduced ejection fraction, as well as tachyarrhythmias, which may lead to SCD [21]. In this study, the most prevalent causes of non-ischaemic SCD were hypertensive CM, CM related to obesity, alcoholic CM and fibrotic CM.
An estimated 30–50% of all non-ischaemic CMs is associated with alcohol abuse [16]. After genetic factors, alcohol abuse is a leading cause of non-ischaemic dilated CM [6,16]. Chronic alcohol abuse reduces cardiac contractility, activates compensatory mechanisms and can thus lead to alcoholic CM, which is characterised by ventricle dilation, left ventricular hypertrophy and reduced ejection fraction [6,16,19]. It is estimated that a consumption of about 7–8 standard drinks per day for >5 years is a significant risk for developing alcoholic CM in both males and females [19]. Nevertheless, less than half of all chronic heavy drinkers develop alcoholic CM [1,16,19]. The prevalence of alcoholic CM is higher in men compared to women, as is death from alcoholic CM [16,19]. Men drink more alcohol than women, however, women might be more vulnerable to the effects of alcohol abuse and to developing alcoholic CM [6,19]. In our study, elevated blood ethanol level at the time of SCD was more often seen in men than women.
The majority of studies concerning alcohol ingestion and SCD have been done on ischaemic heart disease. The effect of alcohol on the development of alcoholic CM is well established, but information on the association of alcohol abuse with non-ischaemic SCD is limited. In a large, population-based study by Klatsky et al. [9], heavy alcohol abuse was reported to increase the risk of heart failure in patients with no coronary artery disease. Cooper et al. [8] found no association between light-to-moderate drinking and death from NIHD in patients with left ventricular systolic dysfunction, although a modest trend towards risk of hospitalisation from non-ischaemic heart failure was seen. In an earlier study of 7,735 middle-aged British men, Wannamethee et al. [7] demonstrated a marginally increased risk of sudden death in heavy drinking men with no evidence of pre-existing coronary artery disease. In their study, cause of death was defined only by existing information on medical history, as the victims were not autopsied; also, the study included all types of sudden death. Cittadini et al. [22] released a case report about an autopsy-verified victim of SCD due to arrhythmogenic right ventricular CM and ethanol and cocaine abuse. Alcohol abuse can prolong the QT interval and has been reported to increase the risk of drowning in patients with long QT syndrome [23].
Our study suggests a possible association between acute alcohol intake and autopsy-verified non-ischaemic SCD. As previous research data concerning non-ischaemic SCD and alcohol is limited, it is not quite obvious why hypertensive CM, fibrotic CM, myocarditis and valvular heart disease specifically were associated with elevated blood alcohol level compared to other types of NIHD. We found no studies about alcohol use in patients with myocarditis or valvular heart disease as a cause of death. Hypertensive and fibrotic CM, on the other hand, often cause changes in the myocardium. Therefore, a possible mechanism behind the associations mentioned before could be a synergic effect of the arrhythmia-inducing structural abnormalities and reduced cardiac contractility often seen in NIHD, with the susceptibility to arrhythmias and left ventricular dysfunction caused by acute alcohol intake. Further studies are needed to assess whether this association could be described as a causal effect, as well as to determine the relationship between chronic drinking and the risk of non-ischaemic SCD.
Limited data are available about alcohol consumption as a contributor to death in Finland. According to Statistics Finland (2018), alcohol-related disease and alcohol poisoning account for about 3% of all deaths in Finland, although alcohol-related deaths may be slightly under-recorded [24]. A medico-legal autopsy is performed in 15–20% of deaths that occur in Finland (Statistics Finland 2015), and toxicologic investigation is performed in most cases. Ketola et al. reported elevated blood alcohol levels in 36% of 122 234 Finnish autopsy cases over 18 years [25]. The majority (78%) of the subjects were men, and male victims had significantly more often alcohol in blood compared to females (81% vs 19%). These findings do not represent the whole population and are biased towards users of alcohol, as toxicologic investigation is performed primarily in cases with suspicion of toxic exposure. Also, in our study, all cases of intoxication and alcohol poisoning were excluded.
In previous studies, the cause of a sudden death has often been determined by prior medical history. In this study, all deaths were confirmed to be due to a cardiac cause by autopsy. We consider autopsy to be a more reliable way to determine the cause of a sudden death, for many sudden conditions, such as aortic dissection, pulmonary embolism and stroke, can lead to sudden death and might be interpreted as SCD, if not autopsied [26].
Limitations
As a limitation, this study only addresses acute alcohol intake at the time of SCD, as previous use of alcohol was not taken into account. Almost half of the subjects with no alcohol in blood were known to be heavy drinkers, although the subjects with alcohol in blood were more often known heavy drinkers. In addition, toxicologic investigation was not performed to all victims of SCD, presenting a possible bias towards cases in which alcohol consumption might have been suspected. Also, medico-legal autopsy is performed with a higher probability if the victim is a known heavy drinker, which might bias the results towards the group with alcohol in blood. No control population could be included in the study, and it is debateable whether these findings can be generalised to other populations. Nevertheless, we consider the autopsy verification of all cases of SCD a major strength in the study, offering an accurate way to determine the causes of non-ischaemic SCD.
Conclusions
Elevated blood alcohol level is common in victims of SCD due to NIHD, especially in males. Recent alcohol consumption may contribute to the subsequent SCD in many non-ischaemic SCD victims.
Funding Statement
This work was supported by The Finnish Medical Foundation, Sigrid Juselius Foundation, Yrjö Jahnsson Foundation and Finnish Foundation for Cardiovascular Research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data is available for reproduction of results on request from the corresponding author.
References
- 1.Hookana E, Junttila MJ, Puurunen VP, et al. Causes of nonischemic sudden cardiac death in the current era. Hear Rhythm. 2011;8(10):1570–1575. [DOI] [PubMed] [Google Scholar]
- 2.Bunch TJ, White RD.. Trends in treated ventricular fibrillation in out-of-hospital cardiac arrest: Ischemic compared to non-ischemic heart disease. Resuscitation. 2005;67(1):51–54. [DOI] [PubMed] [Google Scholar]
- 3.Väyrynen T, Boyd J, Sorsa M, et al. Long-term changes in the incidence of out-of-hospital ventricular fibrillation. Resuscitation. 2011;82(7):825–829. [DOI] [PubMed] [Google Scholar]
- 4.BäNsch D, Antz M, Boczor S, et al. Primary prevention of sudden cardiac death in idiopathic dilated cardiomyopathy: The Cardiomyopathy Trial (CAT). Circulation. 2002;105(12):1453–1458. [DOI] [PubMed] [Google Scholar]
- 5.Kadish A, Dyer A, Daubert JP, et al. ; Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators . Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004;350(21):2151–2158. [DOI] [PubMed] [Google Scholar]
- 6.Mirijello A, Tarli C, Vassallo GA, et al. Alcoholic cardiomyopathy: What is known and what is not known. Eur J Intern Med. 2017;43:1–5. [DOI] [PubMed] [Google Scholar]
- 7.Wannamethee G, Shaper AG.. Alcohol and sudden cardiac death. Br Heart J. 1992;68(5):443–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper HA, Exner DV, Domanski MJ.. Light-to-moderate alcohol consumption and prognosis in patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2000;35(7):1753–1759. [DOI] [PubMed] [Google Scholar]
- 9.Klatsky AL, Chartier D, Udaltsova N, et al. Alcohol drinking and risk of hospitalization for heart failure with and without associated coronary artery disease. Am J Cardiol. 2005;96(3):346–351. [DOI] [PubMed] [Google Scholar]
- 10.Naimi TS, Stockwell T, Zhao J, et al. Selection biases in observational studies affect associations between 'moderate' alcohol consumption and mortality. Addiction. 2017;112(2):207–214. [DOI] [PubMed] [Google Scholar]
- 11.Mukamal KJ, Maclure M, Muller JE, et al. Binge drinking and mortality after acute myocardial infarction. Circulation. 2005;112(25):3839–3845. [DOI] [PubMed] [Google Scholar]
- 12.Perkiömäki J, Hookana E, Kaikkonen K, et al. Blood alcohol in victims of sudden cardiac death in northern Finland. Europace. 2016;18(7):1006–1009. [DOI] [PubMed] [Google Scholar]
- 13.Haukilahti MAE, Holmström L, Vähätalo J, et al. Sudden cardiac death in women. Circulation. 2019;139(8):1012–1021. [DOI] [PubMed] [Google Scholar]
- 14.Launiainen T, Ojanperä I.. Drug concentrations in post-mortem femoral blood compared with therapeutic concentrations in plasma. Drug Test Analysis. 2014;6(4):308–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedman HS. Cardiovascular effects of alcohol with particular reference to the heart. Alcohol. 1984;1(4):333–339. [DOI] [PubMed] [Google Scholar]
- 16.Gardner JD, Mouton AJ.. Alcohol effects on cardiac function. Compr Physiol. 2015;5(2):791–802. [DOI] [PubMed] [Google Scholar]
- 17.Sjögren H, Eriksson A, Ahlm K.. Alcohol and unnatural deaths in Sweden: a medico-legal autopsy study. J Stud Alcohol. 2000;61(4):507–514. [DOI] [PubMed] [Google Scholar]
- 18.Ronksley PE, Brien SE, Turner BJ, et al. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342(feb22 1):d671–d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piano MR. Alcoholic cardiomyopathy: Incidence, clinical characteristics, and pathophysiology. Chest. 2002;121(5):1638–1650. [DOI] [PubMed] [Google Scholar]
- 20.Pimentel M, Zimerman LI, Rohde LE.. Stratification of the Risk of Sudden Death in Nonischemic Heart Failure. Arq Bras Cardiol. 2014;:348–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braunwald E. Cardiomyopathies: An overview. Circ Res. 2017;121(7):711–721. [DOI] [PubMed] [Google Scholar]
- 22.Cittadini F, De Giovanni N, Alcalde M, et al. Genetic and toxicologic investigation of Sudden Cardiac Death in a patient with Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) under cocaine and alcohol effects. Int J Legal Med. 2015;129(1):89–96. [DOI] [PubMed] [Google Scholar]
- 23.Vincenzi FF. Drug-induced long QT syndrome increases the risk of drowning. Med Hypotheses. 2016;87:11–13. [DOI] [PubMed] [Google Scholar]
- 24.Lahti RA, Sajantila A, Korpi H, et al. Under-recording of ethanol intoxication and poisoning in cause-of-death data: Causes and consequences. Forensic Sci Int. 2011;212(1-3):121–125. [DOI] [PubMed] [Google Scholar]
- 25.Ketola RA, Ojanperä I.. Summary statistics for drug concentrations in post-mortem femoral blood representing all causes of death. Drug Test Anal. 2019;11(9):1326–1337. [DOI] [PubMed] [Google Scholar]
- 26.Marshall HS, Milikowski C.. Comparison of clinical diagnoses and autopsy findings: Six-year retrospective study. Arch Pathol Lab Med. 2017;141(9):1262–1266. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data is available for reproduction of results on request from the corresponding author.