Genetic predisposition to hematologic malignancies represents a heterogeneous group of rare disorders that have been included as distinct entities in the revised World Health Organization 2016 classification of myeloid neoplasms and acute leukemia.1 The diagnosis of patients with these disorders is of clinical relevance, as they can benefit from specific clinical care, adapted surveillance and genetic counseling.2-4 Clinical features as well as personal or family history may help to ascertain genetic predisposition to hematologic malignancies. However, up to 40% of patients diagnosed with a cancer predisposition syndrome or inherited bone marrow failure do not have any of these features.5 The very broad variations in the type of hematologic malignancies, age at onset and penetrance also contribute to a lack of clinical recognition. Consequently, many patients present with a diagnosis of an apparently sporadic hematologic malignancy and it is assumed that cases with a genetic predisposition are currently underestimated.
The wide use of high-throughput sequencing technologies has revolutionized the genetic characterization of malignant diseases. Leukemogenesis is now usually considered as a multistep process involving many gene classes and pathways. Notably, some relevant genes, including transcription factors (CEBPA, ETV6, GATA2, RUNX1 and TP53), are targets of both somatic and germline pathogenic variants or more rarely deletions.6,7 Sequencing gene panels used clinically for the genetic characterization of hematologic malignancies usually include transcription factor genes, and may represent a gateway to the identification of germline variants.7,8 High-throughput sequencing offers the possibility to estimate variant allele frequencies (VAF) and a broad view of tumor architecture. Specifically, pathogenic variants with low VAF are assumed to be somatically acquired while pathogenic variants with a VAF of ≥50% may indicate either somatic or germline origin requiring the study of non-tumor samples. Additionally, several studies have pointed out somatic mechanisms, including variant amplification (chromosome doubling, uniparental disomies) or double mutations that are associated with transformation in patients with a germline disorder. 3,9
Here we aimed at retrospectively identifying syndromes with a genetic predisposition due to germline pathogenic variants or deletions in transcription factors (CEBPA, ETV6, GATA2, RUNX1 and TP53) using a practical, molecular-based algorithm in pediatric patients with acute myeloid leukemia (AML) from the French ELAM02 cohort.
The randomized, prospective, multicenter, phase III ELAM02 trial (clinicaltrials.gov identifier: NCT00149162) was conducted from March, 2005 to December, 2011 in pediatric patients (aged 0-18 years old) with AML.10 Children with secondary AML and AML with an underlying known predisposition disorder (Down syndrome, chromosomal breakage diseases, Kostman and Schwachman-Diamond diseases) were excluded. Of note, two patients have been previously reported: one with a germline GATA2 pathogenic variant and the other one with a germline RUNX1 deletion.9,11 Patients with available amplicon-based high-throughput sequencing data and information from single nucleotide polymorphism (SNP)-array analyses at the time of diagnosis of AML were selected for the present study (385 patients out of the 438 patients included in the ELAM02 trial). The molecular profiling using a 36-gene panel with a high depth of coverage (>1500×) at AML diagnosis was reported previously10 (Online Supplementary Table S1). CEBPA mutations were systematically sought by Sanger sequencing because of insufficient coverage by the highthroughput sequencing. Single nucleotide variants were selected based on the absence of a description in public databases of human polymorphisms, and their functional effect was assessed by in silico predictions as previously described.10 Cytoscan HD array (ThermoFisher) was used, according to the manufacturer’s instructions, to screen for gene deletions. The data were analyzed using Chromosome Analysis Suite (ChAS) 3.1 software (ThermoFisher). Since germline specimen collection was not planned by the ELAM02 protocol, blood samples taken at the time of complete remission were used to assess the germline status of variants and deletions by direct Sanger sequencing and SNP-array, respectively. Complete remission was defined as cytological remission associated with a level of WT1 expression below 2% in the bone marrow and below 0.1% in peripheral blood or a core-binding factor transcript expression level below 0.01% in core-binding factor AML. The pathogenic status of the suspected germline alterations was established as per American College of Medical Genetics and Genomics and Association for Molecular Pathology (ACMG-AMP) guidelines.12,13 The study was approved by the Ethics Committee of Saint-Antoine Paris University Hospital (Paris, France) and was conducted in accordance with the Declaration of Helsinki.
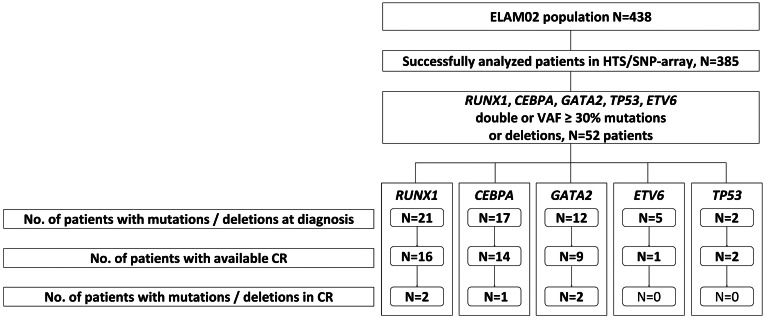
Figure 1.
Study workflow. HTS: high-throughput sequencing; SNP: single nucleotide polymorphism; VAF: variant allele frequency; CR: complete remission.
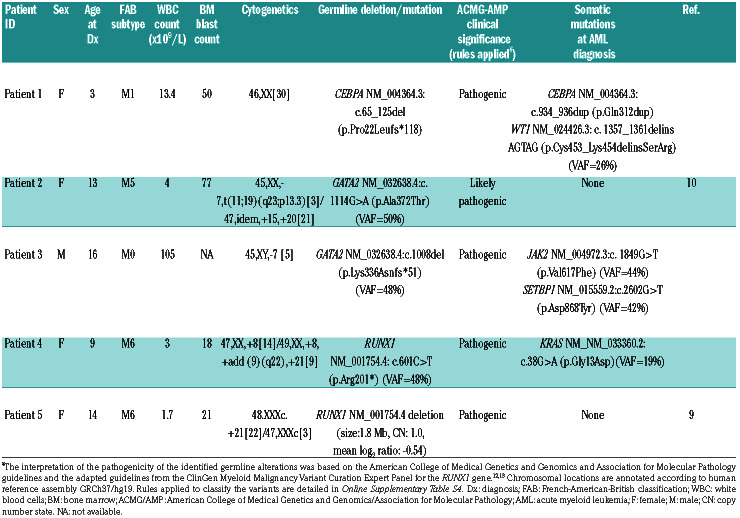
Table 1.
Characteristics of patients with identified germline mutations or deletions.
Investigations were restricted to patients with deletions, double pathogenic variants or unique pathogenic variants with a high VAF (a threshold of ≥30% was chosen to avoid being too restrictive) in one of the following genes: CEBPA, ETV6, GATA2, RUNX1 and TP53 at AML diagnosis. Of note, as the cis-trans allelic configuration for identified variants was not assessed for this study, the term double mutation was preferred, when appropriate.
Fifty-two patients (13%) out of the 385 analyzed met at least one of these criteria (45 with pathogenic variants and 7 with targeted deletions) (Online Supplementary Table S2). Among these patients, 17 had CEBPA double pathogenic variants, including one patient with a homozygous pathogenic variant. RUNX1 pathogenic variants were found in 16 patients (4 with double mutations and 12 with a VAF ≥30%). GATA2, ETV6 and TP53 pathogenic variants with a VAF ≥30% were identified in 12, three, and two patients respectively. Targeted deletions encompassing RUNX1 or ETV6 were found in five and two patients, respectively (size range: 50 kb to 1.8 Mb) (Figure 1). Three of the 52 patients did not reach complete remission, including one patient who died during induction.
Thirty-eight patients had available DNA samples at the time of complete remission. Direct Sanger sequencing and SNP-array analysis of these samples identified five patients with still detectable alterations comprising four with pathogenic/likely pathogenic variants (CEBPA, n=1; GATA2, n=2; RUNX1, n=1) and one with a pathogenic deletion (RUNX1; size: 1.8 Mb) (Table 1, Online Supplementary Table S3, Online Supplementary Figure S1).
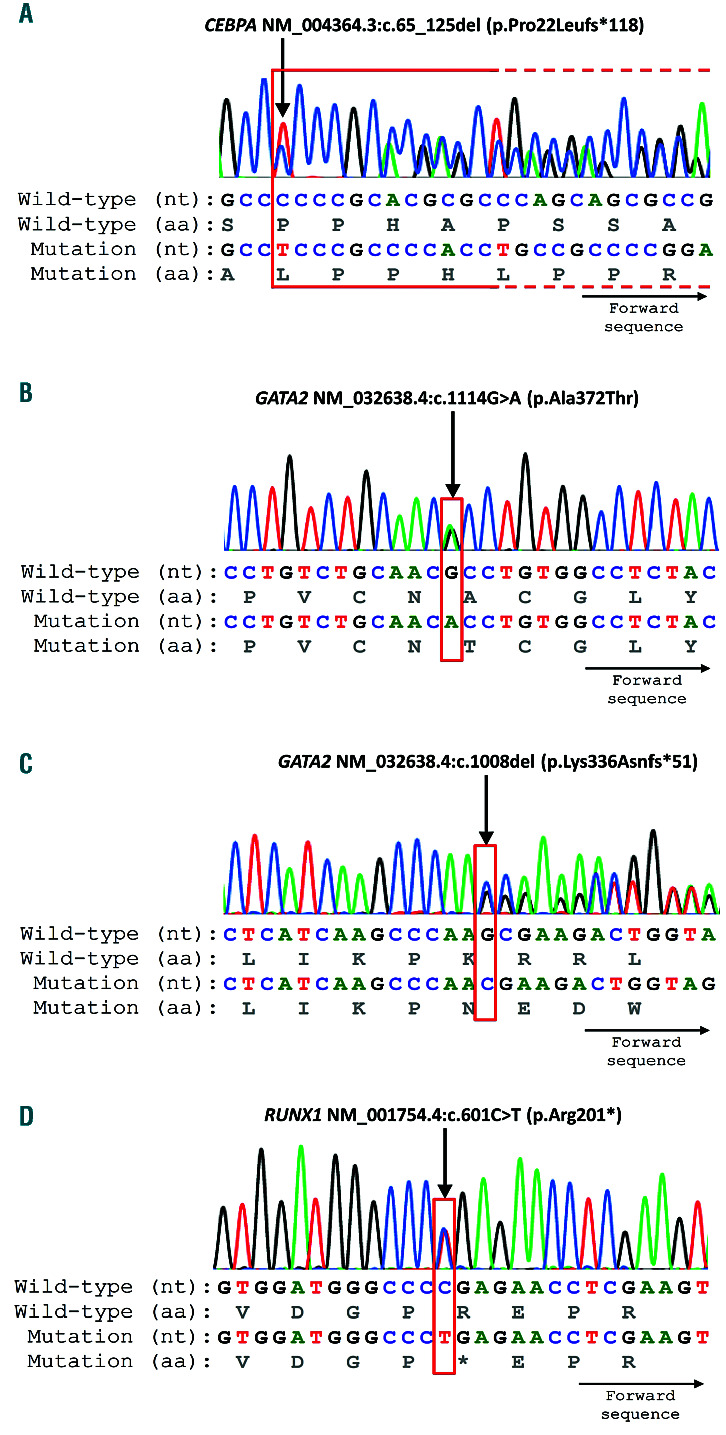
Patient n. 1 was a 3-year old girl who carried a frameshift CEBPA pathogenic variant (NM_004364:c.65_125del (p.Pro22Leufs*118)) (Figure family history revealed leukemia in her paternal grandmother at the age of 30 years and childhood leukemia in her paternal aunt (Online Supplementary Figure S2). Most of the described germline CEBPA mutations include Nterminal frameshift upstream of the p30 start codon and are supposed to be highly penetrant.3 Interestingly, the CEBPA variant in our patient was subsequently found to be inherited from the proband’s father who had no history of leukemia. Along with the family history, the detection of the CEBPA variant in the proband’s complete remission sample and in her father is consistent with a germline mutation.
Figure 2.
Variants confirmed by Sanger sequencing in samples taken at complete remission. nt: nucleotide; aa: amino acid.
Patient n. 2 was a 13-year old girl with a GATA2 variant, likely pathogenic, involving a highly conserved zinc finger domain of the protein (NM_032638:c.1114G>A (p.Ala372Thr)) (Figure 2B). This patient had no family history of malignancies (Online Supplementary Figure S2). When achieving complete remission, the patient developed a progressive decrease of neutrophils, monocytes, B cells, and natural killer cells associated with numerous infections. The GATA2 variant found in this patient was previously reported in another patient with recurrent episodes of pancytopenia, fever and infections.14 The clinical features and persistence of the GATA2 variant in complete remission finally led to the diagnosis of a germline GATA2-mutated disorder (reported by Pasquet et al.11).
Patient n. 3 was a 16-year old boy who carried a frameshift GATA2 pathogenic variant (NM_032638:c.1008del (p.Lys336Asnfs*51)) (Figure 2C) which was located between the two zinc finger domains of the GATA2 protein. This patient had no particular personal or family history (Online Supplementary Figure S2). Of note, absence of family history is common in germline GATA2-mutated children/adolescents with hematologic malignancies,15 suggesting a de novo mutation in this patient.
Patient n. 4 was a 9-year old girl with a pathogenic variant in the highly conserved homology domain (RHD) of the RUNX1 protein (NM_001754.4:c.601C>T (p.Arg201*)) (Figure 2D). Pathogenic variants involving this codon have been reported several times as somatic or germline.16 The family history of this patient identified solid tumors (testicular cancer in her father, 2 breast cancers and colorectal cancer in her paternal grandmother) but neither thrombocytopenia nor hematologic malignancies (Online Supplementary Figure S2).
Patient n. 5 was followed up for a thrombocytopenia since the age of 2 years. At 14 years old, she developed AML shortly after a phase of refractory anemia with excess blasts (Online Supplementary Figure S2). Cytogenetics revealed a constitutional triple X syndrome and an acquired trisomy 21. SNP-array analysis revealed a complete deletion of the RUNX1 locus (Online Supplementary Figure S1). This case was previously reported by Preudhomme et al.9
This study emphasizes the complexity of identifying inherited syndromes without any extra-hematologic features. In such cases, high-throughput sequencing appears to be an informative tool for identifying syndromes predisposing to hematologic malignancies.5,7,8 When using amplicon-based high-throughput sequencing, copy number analysis (i.e. comparative genome hybridization/SNP-array) should also be used since large deletions could be missed with the sequencing approach. Current capture-based high-throughput sequencing techniques are good alternatives to detect both mutations and copy-number alterations with specific pipelines. Assessment of both the inherited nature of variants and their pathological significance remains a challenge in practice. Cultured skin fibroblasts are recommended to ascertain the germline status of a specific variant. Particular attention should be paid to epidemiological data, functional studies and expert recommendations. Recent guidelines on the interpretation of variants written by the ACMG-AMP working group may help to refine the clinical significance of variants.12,13,17,18
We restricted our study to transcription factor alterations reported to be involved in predisposition syndromes. Other well-known targets, such as ANKRD26, DDX41 (which is mostly present in adult patients) and SAMD9/SAMD9L were not studied here. Consequently, we were not able to evaluate the incidence of germline disorders in pediatric AML with known predisposing gene mutations.19
The identification of germline pathogenic variants has a strong impact on patients’ management. The downstream genetic counseling requires cautious consideration of potential, related donors, excluding mutation carriers and searching for a matched, unrelated donor if necessary.
Genetic counseling should be adapted taking into account the characteristics of the predisposition syndrome and its penetrance. A few guidelines are being produced to help with genetic counseling in daily practice. 2,17,20,21 Further efforts are needed to provide a more formal passage from suspicion to genetic counseling relying on a multidisciplinary approach integrating the expertise of clinicians, hematologists and geneticists.
In conclusion, this study highlights the complexity of identifying predisposition syndromes to myeloid malignancies in the absence of extra-hematologic symptoms. Although focusing on transcription factor genes, predisposition syndromes to pediatric AML were not rare in this cohort (5/38 patients, 13%) and should be sought. In this setting, we show here the performance of highthroughput sequencing and a SNP-array. Non-mosaic deletions smaller than 5 Mb should foster further investigations to identify germline pathogenic variants. Interestingly, in our series of patients, none of the selected pathogenic or likely pathogenic variants with allele frequencies comprised between 30% and 40% remained in complete remission, corroborating the previously suggested7 threshold of 40% as that for seeking an underlying predisposition syndrome in daily practice.
Supplementary Material
Acknowledgments
The authors would like to thank all the patients, their families and the staff of all the centers of the Société Française de lutte contre les Cancers et les leucémies de l’Enfant et de l’adolescent (SFCE) for their involvement in the ELAM02 trial. The authors are grateful to the ELAM02 national bank and the Tumor Bank at Lille University Hospital (certification NF 96900-2014/65453-1) for handling, conditioning and storing patients’ samples.
Funding Statement
Funding: the ELAM02 trial was supported by a grant from the French Ministry of Health (PRTK 2012-43-CARAMELE). CONECT-AML (COllaborative Network for Children and Teenagers with Acute Myeloid Leukemia) is supported by a grant from InCA, Fondation ARC, Ligue nationale contre le cancer, and Laurette Fugain (InCa-ARC-LIGUE_11905).
References
- 1.Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391-2405. [DOI] [PubMed] [Google Scholar]
- 2.Godley LA, Shimamura A. Genetic predisposition to hematologic malignancies: management and surveillance. Blood. 2017;130(4): 424-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tawana K, Wang J, Renneville A, et al. Disease evolution and outcomes in familial AML with germline CEBPA mutations. Blood. 2015;126(10):1214-1223. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton KV, Maese L, Marron JM, Pulsipher MA, Porter CC, Nichols KE. Stopping leukemia in its tracks: should preemptive hematopoietic stem-cell transplantation be offered to patients at increased genetic risk for acute myeloid leukemia? J Clin Oncol. 2019;37(24):2098-2104. [DOI] [PubMed] [Google Scholar]
- 5.Tawana K, Drazer MW, Churpek JE. Universal genetic testing for inherited susceptibility in children and adults with myelodysplastic syndrome and acute myeloid leukemia: are we there yet? Leukemia. 2018;32(7):1482-1492. [DOI] [PubMed] [Google Scholar]
- 6.Duployez N, Martin J-E, Khalife-Hachem S, et al. Germline RUNX1 intragenic deletion: implications for accurate diagnosis of FPD/AML. HemaSphere. 2019;3(3):e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drazer MW, Kadri S, Sukhanova M, et al. Prognostic tumor sequencing panels frequently identify germ line variants associated with hereditary hematopoietic malignancies. Blood Adv. 2018;2(2):146-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yannakou CK, Jones K, Ryland GL, et al. Incidental detection of germline variants of potential clinical significance by massively parallel sequencing in haematological malignancies. J Clin Pathol. 2018;71(1):84-87. [DOI] [PubMed] [Google Scholar]
- 9.Preudhomme C, Renneville A, Bourdon V, et al. High frequency of RUNX1 biallelic alteration in acute myeloid leukemia secondary to familial platelet disorder. Blood. 2009;113(22):5583-5587. [DOI] [PubMed] [Google Scholar]
- 10.Marceau-Renaut A, Duployez N, Ducourneau B, et al. Molecular profiling defines distinct prognostic subgroups in childhood AML: a report from the French ELAM02 study group. HemaSphere. 2018;2(1):e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pasquet M, Bellanné-Chantelot C, Tavitian S, et al. High frequency of GATA2 mutations in patients with mild chronic neutropenia evolving to MonoMac syndrome, myelodysplasia, and acute myeloid leukemia. Blood. 2013;121(5):822-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luo X, Feurstein S, Mohan S, et al. ClinGen Myeloid Malignancy Variant Curation Expert Panel recommendations for germline RUNX1 variants. Blood Adv. 2019;3(20):2962-2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ganapathi KA, Townsley DM, Hsu AP, et al. GATA2 deficiencyassociated bone marrow disorder differs from idiopathic aplastic anemia. Blood. 2015;125(1):56-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wlodarski MW, Collin M, Horwitz MS. GATA2 deficiency and related myeloid neoplasms. Semin Hematol. 2017;54(2):81-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sood R, Kamikubo Y, Liu P. Role of RUNX1 in hematological malignancies. Blood. 2017;129(15):2070-2082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kohlmann W, Schiffman JD. Discussing and managing hematologic germ line variants. Blood. 2016;128(21):2497-2503. [DOI] [PubMed] [Google Scholar]
- 18.Li MM, Datto M, Duncavage EJ, et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer: a joint consensus recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J Mol Diagn. 2017;19(1):4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidsson J, Puschmann A, Tedgård U, Bryder D, Nilsson L, Cammenga J. SAMD9 and SAMD9L in inherited predisposition to ataxia, pancytopenia, and myeloid malignancies. Leukemia. 2018;32(5):1106-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jongmans MCJ, Loeffen JLCM, Waanders E, et al. Recognition of genetic predisposition in pediatric cancer patients: an easy-to-use selection tool. Eur J Med Genet. 2016;59(3):116-125. [DOI] [PubMed] [Google Scholar]
- 21.DiNardo CD, Bannon SA, Routbort M, et al. Evaluation of patients and families with concern for predispositions to hematologic malignancies within the Hereditary Hematologic Malignancy Clinic (HHMC). Clin Lymphoma Myeloma Leuk. 2016;16(7):417-428.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.