Abstract
Background:
Inpatient treatment for substance use disorders is a collection of strategies ranging from short term detoxification to longer term residential treatment. How those with opioid use disorder (OUD) navigate this inpatient treatment system after an encounter for detoxification and subsequent risk of opioid-related overdose is not well understood.
Methods:
We used a comprehensive Massachusetts database to characterize the movement of people with OUD through inpatient care from 2013–2015, identifying admissions to inpatient detoxification, subsequent inpatient care, and opioid overdose while navigating treatment. We measured the person-years accumulated during each transition period to calculate rates of opioid-related overdose, and investigated how overdose differed in select populations.
Results:
Sixty-one percent of inpatient detoxification admissions resulted in a subsequent inpatient detoxification admission without progressing to further inpatient care. Overall, there were 287 fatal and 7,337 non-fatal overdoses. Persons exiting treatment after detoxification had the greatest risk of overdose (17.3 per 100 person-years) compared to those who exited after subsequent inpatient care (ranging from 5.9 to 6.6 overdoses per 100 person-years). Non-Hispanic whites were most at risk for opioid related overdose with 16 overdoses per 100 person-years and non-Hispanic blacks had the lowest risk with 5 overdoses per 100 person-years.
Conclusions:
The majority of inpatient detoxification admissions do not progress to further inpatient care. Recurrent inpatient detoxification admission is common, likely signifying relapse. Rather than functioning as the first step to inpatient care, inpatient detoxification might be more effective as a venue for implementing strategies to expand addiction services or treatment such as medications for opioid use disorder.
Keywords: substance use, opioid use, overdose
1. Introduction
As the opioid epidemic has strained treatment systems, there is an urgent need for more opioid use disorder (OUD) treatment capacity. One treatment model is inpatient addiction treatment, which lacks compelling evidence supporting its efficacy in addressing OUD, but represents a large proportion of treatment overall (Saloner & Karthikeyan, 2015). This problem of evidence was highlighted in a recent systematic review that pointed to the gaps in knowledge of the components of inpatient care, particularly of retention and movement through different types of inpatient treatment, that make it difficult to establish a viable measure of treatment efficacy (de Andrade, Elphinston, Quinn, Allan, & Hides, 2019). In many communities, the inpatient addiction treatment system was initially designed for persons with alcohol use disorder. In the response to the opioid crisis, this treatment programs have been utilized to meet the treatment needs of people with OUD. As the addiction epidemiology changes, we need a better understanding of how the system adapts to patient needs and how patients transition through inpatient treatment. Furthermore, following detoxification that results in opioid abstinence, patients leave treatment with lower opioid tolerance and, thus, higher risk for overdose upon opioid relapse. However this effect of this risk has not been studied, particularly within the system of inpatient treatment which is subject to resource constraints and wait times. Thus, it is critically important to investigate overdoses in the context of navigating the distinct levels of inpatient care.
The American Society for Addiction Medicine’s (ASAM) describes the levels of addiction treatment which while not specific to OUD, are useful in understanding the Massachusetts inpatient system. ASAM levels of inpatient care includes: 1) detoxification, or inpatient medically managed withdrawal treatment (ASAM Levels III.7 and IV); 2) post-detoxification treatment for stabilization and transition to (ASAM Levels III.3 and III.5); 3) residential treatment (ASAM Levels III.1) (Massachusetts Department of Public Health, 2014; Mee-Lee & American Society of Addiction Medicine, 2013). These inpatient levels offer a path towards recovery from inpatient detoxification through long-term residential treatment. Massachusetts inpatient treatment providers are licensed in categories that adhere to these levels by the Massachusetts Department of Public Health (MDPH), some of which receive funding from the state to pay for services not covered by other payers as well as services provided to the uninsured (Massachusetts Department of Public Health, 2014). Previous research in Massachusetts and other states has demonstrated that patients often do not complete this pathway in a linear fashion and are frequently readmitted to detoxification (Acevedo, Garnick, Ritter, Lundgren, & Horgan, 2016; Acevedo et al., 2018; Lee et al., 2014; Quinn et al., 2017). While navigating inpatient treatment, particularly during transition periods between levels, patients are at higher risk for relapse and overdose (Davoli et al., 2007; Ravndal & Amundsen, 2010; Walley et al., 2017; Wines, Saitz, Horton, Lloyd-Travaglini, & Samet, 2007). To better understand inpatient OUD treatment, we examined inpatient care in Massachusetts from detoxification through inpatient continuity of care including post-detoxification services and residential treatment. We described opioid-related overdose through inpatient treatment, and examined overdose rates at different points and among different patient populations.
2. Material and methods
2.1. Overview
Chapter 55 of the Acts of 2015 (Chapter 55) mandated that the MDPH analyze data from several Massachusetts government agencies to identify and report on trends among persons who suffered a fatal opioid overdose. This was later expanded to include non-fatal overdose. Linkage across datasets at the individual level allowed analysts to gain a deeper understanding of the circumstances that influence fatal and non-fatal opioid overdoses (Massachusetts Department of Public Health, 2017). We used the Massachusetts Public Health Data Warehouse (PHD) dataset to perform a retrospective study of admissions to inpatient detoxification from January 2013 through September 2015. This is the period in which we had full data for individuals seeking inpatient care and overdose reporting. We identified admissions to inpatient medically managed withdrawal treatment (inpatient detoxification) and followed each admission longitudinally to describe the events following exit from inpatient detoxification including readmissions to inpatient detoxification, admissions to post-detoxification and residential care, exit inpatient care, and overdose.
2.2. Data Source
The PHD links records at the person-level across 22 unique datasets and has been described in depth elsewhere (Massachusetts Department of Public Health, 2017).
We used the Bureau of Substance Addiction Services (BSAS) treatment data to identify admissions to ASAM Levels III.7 inpatient detoxification and subsequent admissions to post-detoxification stabilization, and long-term residential care. The BSAS administrative dataset contains admission-level data, including dates of admissions and discharge, from admissions to BSAS licensed inpatient treatment facility in Massachusetts. We identified fatal and non-fatal overdoses with the following PHD sources (Massachusetts Department of Public Health, 2017):
Case-Mix acute care hospital database (Case Mix). Case Mix data include records of all inpatient, emergency department, and outpatient observation discharges, including International Classification of Disease (ICD-9) diagnosis codes that were associated with the event. We identified overdoses as any admission associated with ICD-9 codes 965.0x, E850.0, E850.1, and E850.2.
Registry of Vital Records and Statistics (RVRS). Death certificates are filed with the RVRS and contain the official cause of death and manner of death assigned by physicians and medical examiners. Deaths were categorized by using the International Classification of Disease (ICD-10) codes for mortality or using a literal search of written cause of death from the medical examiner’s office for records that did not yet have a valid ICD-10 code. The following codes were selected from the underlying cause of death field to identify poisonings/overdoses: X40-X49, X60-X69, X85-X90, Y10-Y19, and Y35.2. All multiple cause of death fields were then used to identify an opioid-related death: T40.0, T40.1, T40.2, T40.3, T40.4, and T40.6.
Massachusetts Ambulance Trip Record Information System (MATRIS). Emergency Medical Services in Massachusetts are required to maintain records of all ambulance calls and submit them to Office of Emergency Medical Services which maintains the MATRIS database. Opioid-related overdoses were determined by an algorithm developed by MDPH in collaboration with Centers for Disease Control and Prevention.
All databases were linked through the Massachusetts All-Payer Claims Database (APCD), which includes all medical, pharmacy, and dental claims submitted to a participating payer, commercial or public, in the state. A unique random identifier was assigned to each person in the database, such that it was possible to link records over time at the person-level.
2.3. Defining the inpatient system of care
We included three inpatient treatment stages in our analysis: 1) inpatient detoxification – delivers intensive management of acute withdrawal symptoms. This treatment stage is typically short-term, between three to seven days. The definition of detoxification in BSAS matches the ASAM criteria of withdrawal management. 2) Post-detoxification – short-term inpatient management including clinical stabilization and transitional support services, e.g. case management and identifying longer-term treatment needs, and typically lasts between 10 and 30 days. 3) Long-term residential treatment – lasts between six months and two years and provides structured individual and group counseling, activities supporting recovery, and transition back to work (Center for Health Information and Analysis, 2015). We also included an “exit” stage. Exit from inpatient care may be appropriate or not, and may be patient-driven or not. Exit could indicate that a patient relapsed and is not seeking treatment, is in recovery, sought treatment in a non-BSAS funded residential facility, was referred to an outpatient provider, moved out of Massachusetts, was lost to follow-up, died, or otherwise ceased inpatient treatment.
2.4. Inclusion criteria
We included all inpatient detoxification admissions where opioids were indicated as the first, second, or third predominate drug identified in the BSAS treatment data between January 1st 2013 and September 30th 2015. We followed future events after each detoxification admission, tracking admissions to other inpatient treatment facilities (post- detoxification and residential), as well as fatal and non-fatal opioid overdoses, until one of the following events occurred: 1) readmission to inpatient detoxification—at which point a new care episode begins, or; 2) end of the database in 2015.
2.5. Analysis
Among inpatient detoxification admissions, we characterized the progression through care by calculating the number of admissions to and person-time accrued in each treatment stage (inpatient detoxification, post-detoxification, and residential). Among those who exited care we defined the number readmitted to inpatient detoxification and those who had no other known inpatient care episodes.
Next, we calculated the total number of fatal and non-fatal opioid overdoses that occurred during each transition period while in care and after exit from any of the three stages. Because there is no follow-up after death, we characterized fatal opioid overdose based on the last treatment episode in the database. Using the total number of opioid overdoses and the person-time accrued in each transition period we calculated the opioid overdose rate per 100 person-years. To better characterize overdose after exiting care, we compared the timing of opioid overdoses following exit after detoxification, post-detoxification, and residential care. We also characterized when overdoses took place relative to the last stage of care in order to assess how often overdoses were “clustered” near discharge from inpatient care, as this may reflect a relapse after a loss of tolerance from inpatient-induced abstinence.
In order to evaluate populations who may be at elevated risk of opioid-related overdose, we examined whether navigating the inpatient care system and risk of overdose was different in these individuals. We calculated overall and transition-specific opioid-related overdose rates stratified by sex (male, female), race and ethnicity (non-Hispanic whites, non-Hispanic blacks, and Hispanic), age (emerging adults aged 18–29 years old versus other adults), homelessness at any point in the study period, and presence of mental health treatment at any point during the study period.
3. Results
3.1. Progression through inpatient care
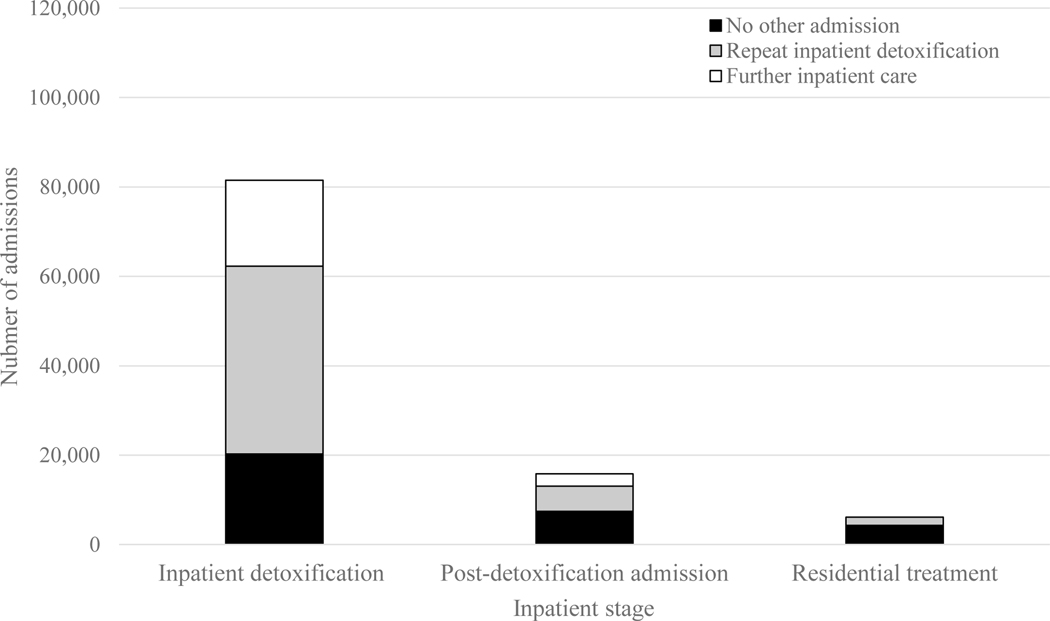
Between January 2013 and September 2015, there were 81,519 admissions to inpatient detoxification (Figure 1). Among those admissions, 24% (19,246) engaged in further, non-detoxification inpatient care; 20,276 (25%) exited care and were not admitted again to any known inpatient treatment, and; 41,997 (52%) were next readmitted to inpatient detoxification. In total, only 8% (6,163) of all inpatient detoxification admissions resulted in complete navigation of the inpatient treatment system with admission to long-term residential care. Sixty-one percent (49,507) of all inpatient detoxification admissions resulted in readmission to inpatient detoxification at some point in the future. Among the 19,246 admissions that progressed from inpatient detoxification, 15,816 (82%) were next admitted to a post-detoxification facility and 3,430 (18%) moved directly from inpatient detoxification to residential treatment. Of 15,816 post-detoxification admissions, 2,733 (17%) went next to residential treatment while 13,083 (83%) exited care, of which 43% were readmitted to inpatient detoxification and 57% had no other known inpatient admissions. After residential treatment, 30% of the 6,163 residential admissions were ultimately readmitted to inpatient detoxification, while 70% had no other interaction with the inpatient system.
Figure 1: Subsequent admissions stratified by current inpatient stage.
Figure legend: The bar graph displays the subsequent admission stratified by the current inpatient stage. The first bar is the total number of inpatient detoxification admissions (81,519), colored depending on the number of these admissions which were next followed by no other admission (black, 20,276 admissions), a repeat inpatient detoxification admission (grey, 41,997 admissions), or further inpatient care, which could include post-detoxification or residential treatment (white, 19,246 admissions). The middle bar reflects the 15,816 admissions to post-detoxification, of which 7,432 were followed by no other admission (black), 5,651 were followed by an inpatient detoxification admission (grey), and 2,733 were followed by further treatment (white). The final 6,163 admissions to residential treatment are followed either by no other known admissions (4,304, black) or a subsequent inpatient detoxification admission (1,859, grey).
3.2. Overdose while navigating inpatient care
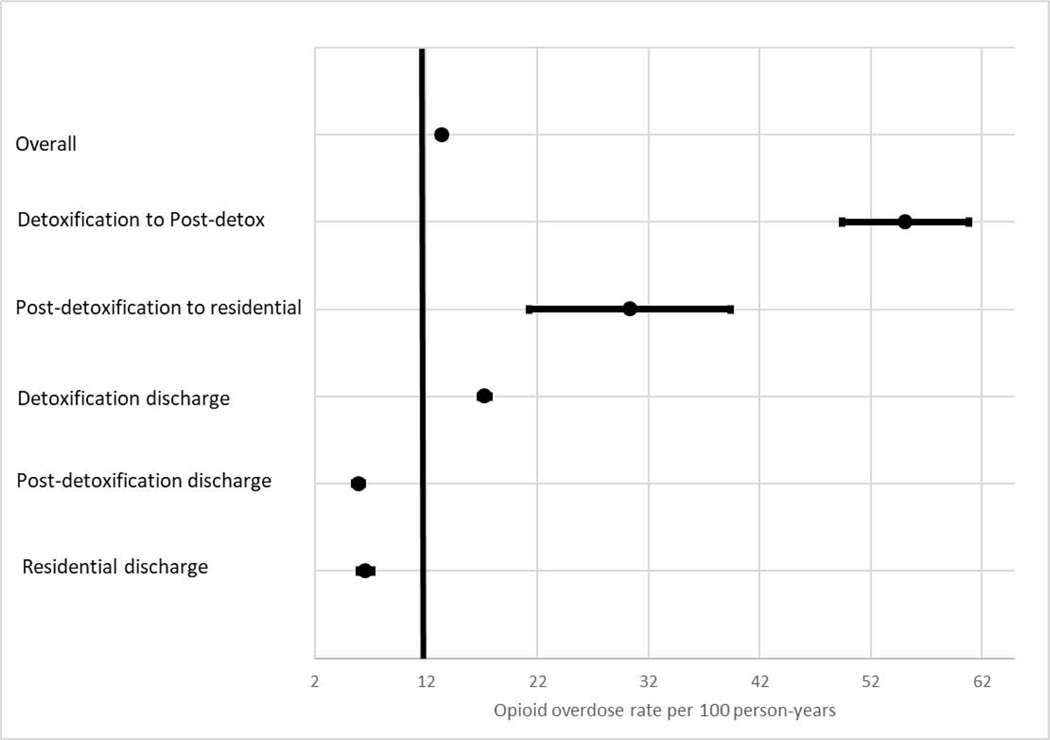
There were 7,624 opioid overdoses that occurred following the 81,519 total inpatient detoxification discharges, meaning that nearly 10% of all discharges from inpatient detoxification were followed by an opioid overdose at some point. Of these opioid overdoses, 4% (287) were fatal (Table 1). A total of 56,761 person-years accrued during while navigating care, yielding an overall opioid-related overdose rate of 13.4 per 100 person-years. However, we found that the opioid overdose rate differed widely throughout care (Figure 2). The greatest risk of opioid overdose occurred close to detoxification; in the transition between detoxification and post-detoxification (55.1 per 100 person-years compared to 30.4 overdoses per 100 person-years between post-detoxification and residential) and among those who exited care, exiting following detoxification carried the greatest risk of opioid overdose (17.3 per 100 person-years compared to 5.9 and 6.6 per 100 person-years for exit after post-detoxification and residential treatment, respectively).
Table 1:
Tracking fatal opioid overdose stratified by last known inpatient care admission
| LAST ADMISSION | NUMBER FATAL OPIOID OD | % OF ALL FATAL OPIOID OD |
|---|---|---|
| INPATIENT DETOXIFICATION | 221 | 77% |
| POST-DETOXIFICATION | 37 | 13% |
| RESIDENTIAL | 29 | 10% |
Figure 2: Opioid-related overdose during transitions between inpatient care stages.
Figure legend: Each point represents the rate of opioid-related overdose in the stage per 100 person-years, and the error bars represent the 95% confidence interval for each estimate. The vertical line through the overall rate provides a visual representation of how overdose rates in transition periods compare to the overall overdose rate.
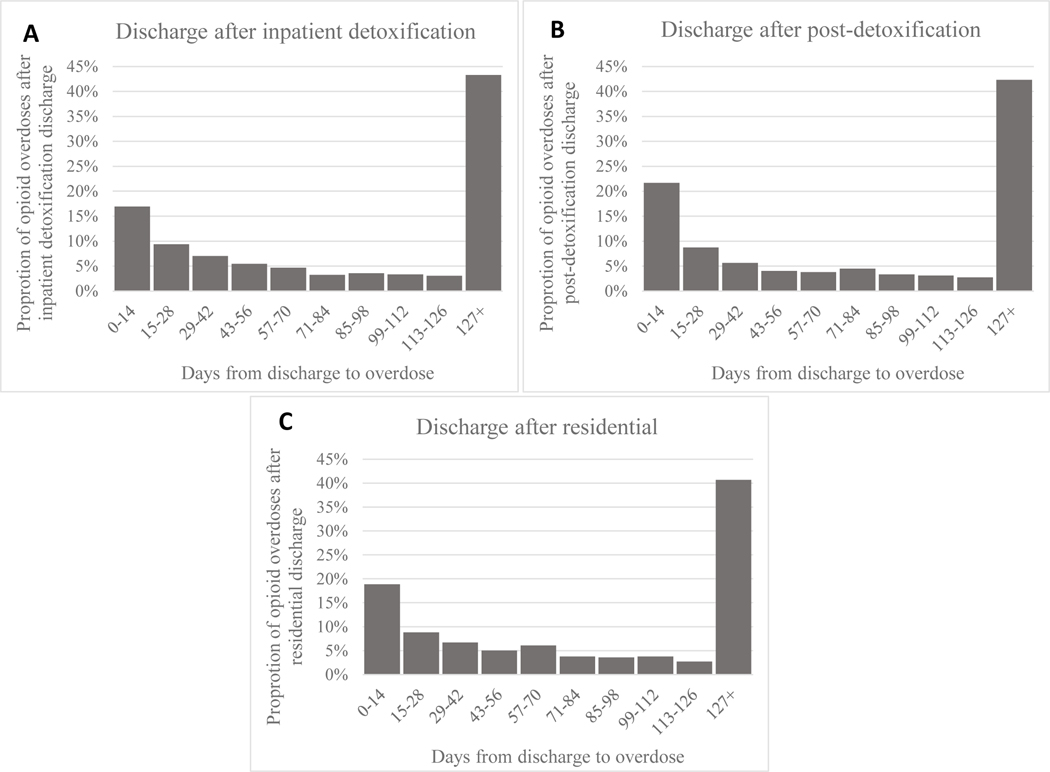
More than 90% (6,976) of opioid overdoses occurred after individuals exited care. Figure 3 describes when those opioid overdoses occurred relative to the date of discharge from the given stage. We found similar rates of opioid overdose clustering after discharge among each exit point, with 17%, 22%, and 19% of opioid overdoses after exiting care occurring within 14 days of discharge from inpatient detoxification, post-detoxification, and residential care, respectively. In each case, more than twice as many individuals experienced opioid overdose in the first two weeks after discharge than did in the second two weeks. Over 40% of all opioid overdoses after exiting care occurred more than 4 months after exiting care.
Figure 3: Timing of opioid overdose after discharge from inpatient treatment.
Figure legend: Among individuals who are discharged from inpatient treatment and experience an opioid overdose, each graph represents the proportion of those individuals experiencing an opioid overdose in each two week period stratified by discharges from inpatient detoxification (A), post-detoxification (B), and residential treatment (C).
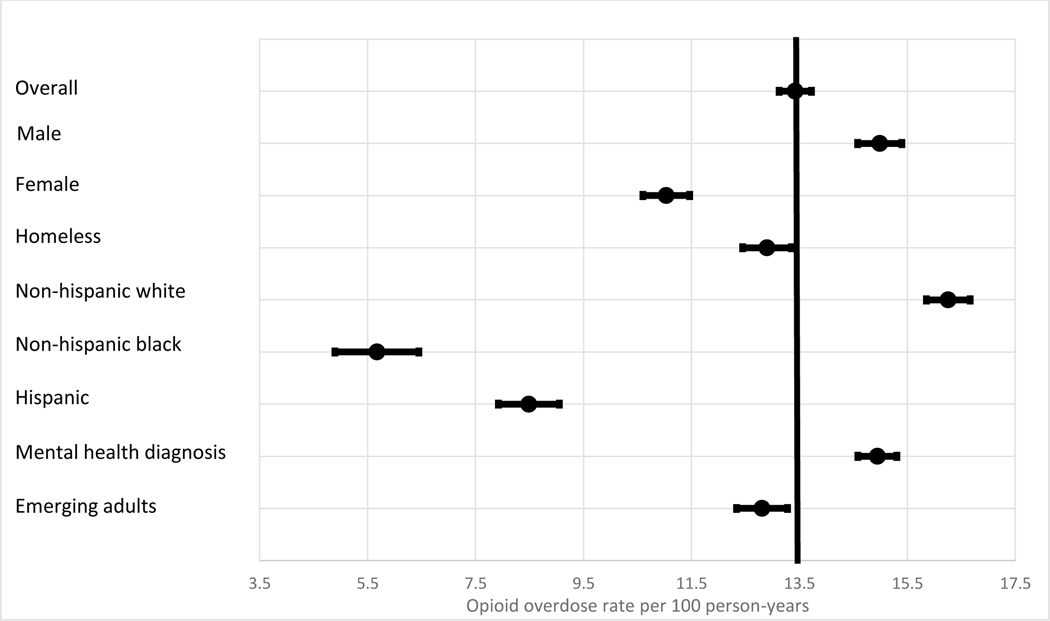
We found that opioid overdose rates differed among several subpopulations (Figure 4). Populations at higher risk included males (15 overdoses per 100 person-years), those receiving mental health treatment during the study period (15 overdoses per 100 person-years), and non-Hispanic whites (16 overdoses per 100 person-years). Those at lower risk for opioid overdose on average were females (11 overdoses per 100 person-years), non-Hispanic blacks (5 overdoses per 100 person-years) and Hispanics (8 overdoses per 100 person-years). We did not detect a difference in persons experiencing homelessness or in emerging adults.
Figure 4: Overall opioid-related overdose by subpopulation.
Figure legend: Each point represents the overall rate of opioid-related overdose in select subpopulations per 100 person-years, and the error bars represent the 95% confidence interval for each estimate, calculated assuming a Poisson distribution. The vertical line through the overall rate provides a visual representation of how opioid overdose rates in subpopulations compares to the overall overdose rate. NOKA = no other known admission.
4. Discussion
We used a comprehensive, linked state-wide database to investigate inpatient OUD care, tracking progression through care and opioid-related overdose. First, we found that progression through the all stages of inpatient care was uncommon. The majority of admissions to inpatient detoxification were followed by exit from inpatient care, and less than one quarter were followed by another step of inpatient care. More striking is that only 8% of admissions to inpatient detoxification led to long-term residential treatment. While further research is needed to understand why individuals do not continue to long-term residential treatment, it is unlikely that adding capacity alone is sufficient. For example, only patients completing detoxification can transition to post-detoxification care, and approximately half do not complete treatment. While we cannot measure relapse to substance use directly, our finding that 61% of all inpatient detoxifications admissions were readmissions aligns with previous studies that documented high rates of relapse after inpatient detoxification (Amato et al., 2013; McLellan, Lewis, O’Brien, & Kleber, 2000; Stein, Anderson, & Bailey, 2015). While opioid use disorder is a chronic relapsing and remitting disease, the rate and severity of relapse differs by treatment strategy and is lower for medication for opioid use disorder (Mattick, Breen, Kimber, & Davoli, 2009, 2014). This supports rethinking the approach to inpatient detoxification.
These findings complement previous studies of detoxification populations in Massachusetts and other states regarding process measures (Lee et al., 2014), payment strategies (Quinn et al., 2017), the effect of patient engagement in detoxification readmission (Acevedo et al., 2016) and the high prevalence of recurrent detoxification encounters (Lundgren, Sullivan, & Amodeo, 2006). Lee et al. (2014) considered the effect of a 14-day continuity of care process measure, examining transitions between inpatient detoxification and continuity of care, and found that just 10.5% of their cohort proceeded to inpatient continuity of care (Lee et al., 2014). Continuity of care was challenging in a study of a large scale intervention in Washington State that tested the use of financial incentives and electronic reminders to increase continuity rates, where neither had an effect (Acevedo et al., 2018). This is concerning given the importance of continuity of care following detoxification to decreasing the risk of subsequent admissions to detoxification (Acevedo et al., 2018). Multiple admissions to a detoxification program suggests ongoing and potentially hazardous substance use. Furthermore, previous admission for detoxification has been found to contribute to increased stigma among patients (Bozinoff, Anderson, Bailey, & Stein, 2017) – recurrently accessing detoxification can result in worse health outcomes and increase barriers to care.
Next, we found that opioid-related overdose was common, with 7,624 total opioid overdoses. Patients were particularly vulnerable to opioid overdose the closer they were in their navigation of treatment to inpatient detoxification – either shortly after release and in transition to post-detoxification or following discharge from inpatient detoxification. While relatively higher rates of opioid overdose after discharge, potentially due to relapse, are expected, we did not anticipate the high rate of opioid overdose during the transition periods between inpatient detoxification and post-detoxification, which was the highest we observed at over 55 overdoses per 100 person-years. Despite having the highest opioid overdose rates, this transition period is the shortest in the treatment progression at an average of 15 days between inpatient detoxification and post-detoxification care. Our results suggest that patients that do not transition immediately are at elevated risk of opioid overdose and that shortening the transition time might be beneficial, particularly given that those who do engage in post-detoxification treatment have a longer time to readmission compared to those that do not (Mark, Vandivort-Warren, & Montejano, 2006). Our finding that males, non-Hispanic whites, and those with a mental health diagnosis are at greater risk of an opioid-related overdose suggests that providers may need to pay special attention to these populations. It may be necessary to re-examine the treatment system in general to understand how we can better treat those with co-occurring mental health illness. Our work reinforces previous findings that the risk of opioid overdose after inpatient detoxification is high (Davoli et al., 2007; Ravndal & Amundsen, 2010; Walley et al., 2017; Wines et al., 2007) and adds value by demonstrating that opioid overdose risk is high even among those actively engaged in inpatient treatment, in particular those who do not transition immediately between inpatient-detoxification and post-detoxification care. This could indicate a lack of coordination between treatment stages, a lack of capacity, or some other barrier. Interventions aimed at streamlining this transition may be an effective way to decrease overdoses in patients who are navigating stages of inpatient care.
Integrating all of these findings, including frequent readmissions and overdose, inpatient detoxification appears to be a place accessed in time of crisis without serving as an efficient entry point into longer term treatment of OUD. The overwhelming majority of detoxification admissions result only in another detoxification admission and very few advance to subsequent levels of care. Further, the large majority of overdoes observed were in the high risk period between detoxification admissions. For detoxification settings to become venues for effective OUD treatment, they should be converted to MOUD induction centers to initiate MOUD and link to settings that offer ongoing MOUD. While inpatient detoxification is an important resource for those experiencing active withdrawal, jurisdictions could benefit from leveraging this crisis-oriented service into a true first step towards effective evidence-based care. One way of achieving this may be to incorporate medications for opioid use disorder (MOUD), which are associated with reduced overdose risk (J. Morgan, Schackman, Weinstein, Walley, & Linas, 2019; Pierce et al., 2016; Sordo et al., 2017) and improved retention in care, into inpatient detoxification. Currently, MOUDs are not routinely incorporated into inpatient detoxification or the care immediately after (Batts et al., 2012), and remain underutilized overall (J. R. Morgan, Schackman, Leff, Linas, & Walley, 2017). Some medications such as injectable naltrexone require detoxification before initiation, so follow naturally from the detoxification process. Agonist medications, such as buprenorphine and methadone, do not require detoxification, but initiation for some patients may be more successful as part of a stabilizing inpatient treatment episode that offers additional short-term medication to manage other substance withdrawal symptoms, counseling, safe short-term shelter and facilitated referral to further structured inpatient and outpatient care. Future research exploring the current and future integration of other services into inpatient treatment, such as referrals for MOUD or actively linking patients to subsequent care is needed. We found that exiting care following any stage featured a substantial risk of opioid overdose; there were twice as many opioid overdoses in the first two weeks after exiting care than the second two weeks. After this, opioid overdoses seem to level off and most opioid overdoses occur far after exiting care. The two week period immediately after exiting care may be another opportunity for linking patients to MOUD. While the reasons for disengagement may be different for those exiting after a stay in inpatient detoxification and for those leaving a residential setting, the proportion of opioid overdoses occurring in the two week period following discharge is similar, implying both could benefit from intervention at that point.
We envision these results being used in several ways. First, one response to the growing opioid crisis has been to increase capacity for treating OUD by increasing capacity at inpatient detoxification facilities, or “adding beds.” Our data indicate that adding inpatient detoxification capacity alone is not enough and needs to be coupled with better use of existing capacity, focusing on reducing transition times during high risk periods. For example, focusing on reducing transition times during high risk periods may be an opportunity to reduce the time at risk as patients navigate inpatient care. Second, these data provide insight into prioritization of interventions. For example, we found that the highest number of overdoses occurred directly after discharge from inpatient detoxification. This suggests that interventions targeted at individuals with a history of inpatient detoxification but no other engagement with the inpatient care system (those frequently readmitted into inpatient detoxification) may be good candidates for preventing the highest number of overdoses. Finally, our results provide additional evidence to support the evaluation of integrating proven OUD treatments, such as MOUDs, into the inpatient care.
4.1. Limitations
Our work has several limitations. First, we included admissions where an opioid was reported as the primary, secondary, or tertiary drug of choice at time of admission. This implies that some individuals in the study had a primary drug of alcohol with opioids as secondary or tertiary. However, individuals with OUD often struggle with multiple use disorders (J. R. Morgan et al., 2017), and we believe this is important to capture in this analysis to represent the OUD population as a whole. Second, our goal was to describe how individuals engage with a complex inpatient system of care and we do not include outpatient services, other recovery support services, or MOUD, and it is likely that utilization of those services decreases overdose risk. By excluding outpatient visits from our purview, our estimate of those discontinuing inpatient care includes both those disengaging with all treatment and those referred to outpatient treatment. It is likely that the risks are different in each of those groups, and for some patients referral to outpatient therapy may have been more appropriate than further inpatient treatment. Our primary finding, that most admissions were actually readmissions to care, still holds, however. We demonstrate that readmission to inpatient detoxification is high at every level of inpatient care and that opioid overdose risk is also high during periods between inpatient care episodes, and reducing this transition time – whether via referral to outpatient care or more direct transition between inpatient stages – would likely reduce overdose risk. Third, we conducted this study with data from Massachusetts; therefore, our findings may not be generalizable to other locales. However, while there is state-to-state variability with regard to inpatient treatment capacity and structure, other states may be able to use our experience to better understand and improve their own treatment systems. Fourth, our inpatient treatment measures are all from BSAS-licensed and funded treatment programs. While this includes a significant portion of the inpatient treatment in the state, it excludes programs not funded or licensed by BSAS. Fifth, we are unable to determine why individuals did not progress through given stages of inpatient care. Some may have terminated detoxification early and against medical advice so were not eligible to progress, some may have relapsed, some may have been referred to outpatient care, and some may have faced other barriers to subsequent inpatient treatment such as capacity constraints of the inpatient system. Regardless of the reason, progression was rare and readmission was frequent.
5. Conclusions
The opioid epidemic is a major challenge to public health, hampered further by a limited understanding of how individuals navigate inpatient OUD care. Our description of the inpatient OUD system of care in MA reveals how rarely an inpatient detoxification admission results in long-term residential care and also documents the concerning number of opioid overdoses occurring while navigating treatment, particularly between detoxification and post-detoxification care. Decreasing this transition time would greatly reduce the risk of individuals navigating inpatient care. Increasing inpatient detoxification capacity is an intuitively appealing means of expanding OUD treatment capacity and fighting the opioid epidemic. Our work demonstrates, however, that increasing detoxification capacity without fundamentally altering the service that detoxification provides – or subsequent linkage to MOUD or additional inpatient care – likely will have little benefit. The majority of inpatient detoxification admissions do not result in progress through inpatient care. Future work and resources should be directed to understanding how best to integrate inpatient and outpatient OUD care modalities to retain high-risk individuals in care and reduce relapse and opioid overdose risk.
Highlights for Opioid overdose and inpatient care for substance use disorder care in Massachusetts.
Inpatient detoxification rarely leads to long-term residential treatment
The risk of overdose is high after detox and before subsequent care
Decreasing transition while navigating inpatient care would reduce overdose risk
Better linkage to subsequent care, including medication, is needed
Acknowledgements:
We want to acknowledge the Massachusetts Department of Public Health for creating this unique, cross-section database and for providing technical support for the analysis. This work was supported by the National Institute on Drug Abuse (grant number P30DA040500 and R01DA046527).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acevedo A, Garnick D, Ritter G, Lundgren L, & Horgan C.(2016). Admissions to detoxification after treatment: Does engagement make a difference? Subst Abus, 37(2), 364–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo A, Lee MT, Garnick DW, Horgan CM, Ritter GA, Panas L, … Bean-Mortinson J.(2018). Agency-level financial incentives and electronic reminders to improve continuity of care after discharge from residential treatment and detoxification. Drug Alcohol Depend, 183, 192–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato L, Davoli M, Minozzi S, Ferroni E, Ali R, & Ferri M.(2013). Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database Syst Rev(2), CD003409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batts K, Pemberton M, Bose J, Weimer B, Henderson L, Penne M, … Strashny A.(2012). Comparing and Evaluating Substance Use Treatment Utilization Estimates from the National Survey on Drug Use and Health and Other Data Sources. In CBHSQ Data Review. Rockville (MD) [PubMed] [Google Scholar]
- Bozinoff N, Anderson BJ, Bailey GL, & Stein MD (2017). Correlates of Stigma Severity Among Persons Seeking Opioid Detoxification. J Addict Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Health Information and Analysis. (2015). Access to substance use disorder treatment in Massachusetts. Retrieved from: http://www.mass.gov/courts/docs/csat-access-to-substance-use-disorder-treatment-in-mass.pdf. (Accessed September 12 2017).
- Davoli M, Bargagli AM, Perucci CA, Schifano P, Belleudi V, Hickman M, … Group VES (2007). Risk of fatal overdose during and after specialist drug treatment: the VEdeTTE study, a national multi-site prospective cohort study. Addiction, 102(12), 1954–1959. [DOI] [PubMed] [Google Scholar]
- de Andrade D, Elphinston RA, Quinn C, Allan J, & Hides L.(2019). The effectiveness of residential treatment services for individuals with substance use disorders: A systematic review. Drug Alcohol Depend, 201, 227–235. [DOI] [PubMed] [Google Scholar]
- Lee MT, Horgan CM, Garnick DW, Acevedo A, Panas L, Ritter GA, … Reynolds M.(2014). A performance measure for continuity of care after detoxification: relationship with outcomes. J Subst Abuse Treat, 47(2), 130–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundgren LM, Sullivan L, & Amodeo M.(2006). How do treatment repeaters use the drug treatment system? An analysis of injection drug users in Massachusetts. J Subst Abuse Treat, 30(2), 121–128. [DOI] [PubMed] [Google Scholar]
- Mark TL, Vandivort-Warren R, & Montejano LB (2006). Factors affecting detoxification readmission: analysis of public sector data from three states. J Subst Abuse Treat, 31(4), 439–445. [DOI] [PubMed] [Google Scholar]
- Massachusetts Department of Public Health. (2014). Mapping of Services Retrieved from: http://www.mass.gov/courts/docs/mapping-of-services.pdf. (Accessed December 5 2017).
- Massachusetts Department of Public Health. (2017). An assessment of fatal and nonfatal opioid overdoses in Massachusetts (2011 – 2015). Retrieved from: https://www.mass.gov/files/documents/2017/08/31/legislative-report-chapter-55-aug-2017.pdf. (Accessed September 10 2017).
- Mattick RP, Breen C, Kimber J, & Davoli M.(2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev(3), CD002209. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, & Davoli M.(2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev(2), CD002207. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, & Kleber HD (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA, 284(13), 1689–1695. [DOI] [PubMed] [Google Scholar]
- Mee-Lee D, & American Society of Addiction Medicine. (2013). The ASAM criteria : treatment for addictive, substance-related, and co-occurring conditions. (Third edition. ed.). Chevy Chase, Maryland: American Society of Addiction Medicine. [Google Scholar]
- Morgan J, Schackman B, Weinstein Z, Walley A, & Linas B.(2019). Overdose following initiation of naltrexone and buprenorphine medication treatment for opioid use disorder in a United States commercially insured cohort. Drug Alcohol Depend. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan JR, Schackman BR, Leff JA, Linas BP, & Walley AY (2017). Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. J Subst Abuse Treat. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M, Bird SM, Hickman M, Marsden J, Dunn G, Jones A, & Millar T.(2016). Impact of treatment for opioid dependence on fatal drug-related poisoning: a national cohort study in England. Addiction, 111(2), 298–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn AE, Hodgkin D, Perloff JN, Stewart MT, Brolin M, Lane N, & Horgan CM (2017). Design and impact of bundled payment for detox and follow-up care. J Subst Abuse Treat, 82, 113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravndal E, & Amundsen EJ (2010). Mortality among drug users after discharge from inpatient treatment: an 8-year prospective study. Drug Alcohol Depend, 108(1–2), 65–69. [DOI] [PubMed] [Google Scholar]
- Saloner B, & Karthikeyan S.(2015). Changes in Substance Abuse Treatment Use Among Individuals With Opioid Use Disorders in the United States, 2004–2013. JAMA, 314(14), 1515–1517. [DOI] [PubMed] [Google Scholar]
- Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, … Pastor-Barriuso R.(2017). Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ, 357, j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Anderson BJ, & Bailey GL (2015). Preferences for Aftercare Among Persons Seeking Short-Term Opioid Detoxification. J Subst Abuse Treat, 59, 99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walley AY, Cheng DM, Quinn EK, Blokhina E, Gnatienko N, Chaisson CE, … Samet JH (2017). Fatal and non-fatal overdose after narcology hospital discharge among Russians living with HIV/AIDS who inject drugs. Int J Drug Policy, 39, 114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wines JD Jr., Saitz R, Horton NJ, Lloyd-Travaglini C, & Samet JH (2007). Overdose after detoxification: a prospective study. Drug Alcohol Depend, 89(2–3), 161–169. [DOI] [PubMed] [Google Scholar]