Abstract
Background:
Keratoconus (KC) is a non-inflammatory disease occur to the cornea and cause it to be thin and progressively bulge it into a cone shape which result to blurred vision secondary to irregular astigmatism, frequently eyeglass changing and increase the sensitivity to the bright light, occur usually at second decade of life and stops progressive after fourth decade of life. keratoconus is unknown in aetiology but is a multifactorial disease in causes which divided into genetic and environmental factors, the genetic factors as if patient under ethnic with high prevalence and family history with keratoconus or Atopy.
Aim:
to assess the general population awareness regarding keratoconus in Aseer region, southern of Saudi Arabia.
Methodology:
A descriptive cross-sectional approach was used targeting all population in Aseer region. The study was conducted during the period from January 2019 to May 2020. Data were collected using structured questionnaire included person's socio-demographic data, Participants’ Participants’ awareness regarding KC. The questionnaire was uploaded online using social media platforms.
Results:
The study included 638 participants who completed the study questionnaire with mean age of 36.8 ± 11.1 years. Exact of 331 (51.9%) of the participants were males. University level of education was reported by 424 participants (66.5%). Fifty-nine participants (9.2%) reported that they had keratoconus.
Conclusions & Recommendations:
In conclusion, the study revealed that public awareness in Aseer region regarding keratoconus was moderately poor with defect regarding treatment modalities and its consequences.
Keywords: Awareness, corneal protrusion, keratoconus, knowledge, population, risk factors
Introduction
Keratoconus (KC) is an eye disorder featured by progressive thinning of the cornea.[1] KC may be associated with blurred or double vision, near-sightedness, astigmatism, with photo sensitivity.[2] KC is usually bilateral. Further in most of the critical cases a disfigure or a round circle may be seen inside the cornea.[3] At times the genuine explanation of KC is unexplored however some way or other scientists accepted on the supposition it is created because of a blend of numerous hereditary, natural, and hormonal impacts.[4,5,6] Positive family ancestry for KC was recorded among almost seven percent of those influenced.[7] Presume substantial influences including soreness in eyes and allergic reactions.[8] The fundamental mechanism includes variations in the shape of the cornea to lookalikes as a cone. We have discovered the varieties in the pervasiveness of KC in various examinations Theses commonness of keratoconus varies all around as indicated by the effect of geographic area and furthermore relies upon the diagnostic features. The commonness in studies can go from 0.3 per 100,000 in Russia[9] to 2300 for each 100,000 in Central India.[10] The principal populace based investigation was finished by Hofstetter utilizing a Placido plate with a rate of 600 for every 100,000.[11] The most detailed pervasiveness is 0.054% in Minnesota, USA by Kennedy who utilized scissors development on retinoscopy and keratometry for conclusion[12] In Saudi Arabia, the main investigation was led in Aseer region with occurrence 20 cases for each 100000 populace. Additionally, the ailment seriousness was high and for the most part among youthful matured populace (mean age is 17.7 ± 3.6 years).[13]
Evaluation of overall public mindfulness with respect to KC help in early recognition and ideal intercession which assume a noteworthy job in the control or anticipation of cut off visual disability as a result of KC Also, public awareness potentially promotes a better community absorption of the educational programs and eventually a proper utilization of the available health-care facilities. Early detection of KC is good to avoid further complications and to avoid the worries of family and reduce the burden on family physicians/ophthalmologists. the study revealed that public awareness in Aseer region regarding keratoconus was moderately poor with defect regarding treatment modalities and its consequences.
The current study aimed to assess population awareness regarding keratoconus and its consequences in Aseer region, Southern of Saudi Arabia.
Methodology
A descriptive cross-sectional survey was used targeting all population in Aseer region. The study was conducted during the period from January 2019 to May 2020. Data were collected using structured questionnaire which developed by the researchers after intensive literature review and expert's consultation. The questionnaire data included person's socio-demographic data such as age, gender, and education. Participants’ awareness regarding keratoconus was assessed covering definition, features, risk factors, intervention needed, and follow-up. Also, participants were asked if they had KC or visual impairment. A panel of 3 experts reviewed the questionnaire independently for content validity and all suggested modifications were applied till the final tool achieved. The questionnaire was uploaded online using social media platforms by the researchers and their relatives and friends to be filled with all population in Aseer region. A pilot study was conducted to assess tool applicability and reliability. The tool reliability coefficient (Alpha Cronbach's) was assessed and equalled 0.73. After data were extracted, it was revised, coded and fed to statistical software IBM SPSS version 22(SPSS, Inc. Chicago, IL). All statistical analysis was done using two tailed tests. P value less than 0.05 was considered to be statistically significant. For awareness items, each correct answer was scored one point and total summation of the discrete scores of the different items was calculated. A patient with score less than 60% (11 points) of the maximum score was considered to have poor awareness while good awareness was considered if he had score of 60% (12 points or more) of the maximum or more. Descriptive analysis based on frequency and percent distribution was done for all variables including demographic data, awareness items and source of information. Crosstabluation was used to assess distribution of awareness according to participants’ personal data and source of information. Relations were tested using Pearson exact probability tests. Ethical approval was obtained from the REC of the King Khalid University. Date of ethical approval was 26-02-2020 from research ethical committee of the king Khalid university.
Results
A total of 638 participants completed the study questionnaire whose ages ranged from 18 to 75 years old with mean age of 36.8 ± 11.1 years. Exact of 331 (51.9%) of the participants were males. University level of education was reported by 424 participants (66.5%). Fifty-nine participants (9.2%) reported that they had keratoconus and 171 (26.8%) reported having progressive declining in vision. Squeezing eyes aggressively was reported by 73% of the respondents [Table 1].
Table 1.
Personal data of survey participants in Aseer region, Saudi Arabia
| Personal data | No | % | |
|---|---|---|---|
| Age in years | <20 years | 26 | 4.1% |
| 20-29 | 181 | 28.4% | |
| 30-39 | 123 | 19.3% | |
| 40-49 | 220 | 34.5% | |
| 50+ | 88 | 13.8% | |
| Gender | Male | 331 | 51.9% |
| Female | 307 | 48.1% | |
| Education | Basic | 171 | 26.8% |
| High | 43 | 6.7% | |
| University/more | 424 | 66.5% | |
| Do you have keratoconus | Yes | 59 | 9.2% |
| May be | 59 | 9.2% | |
| No | 520 | 81.5% | |
| Complain of continuous declined vision | Yes | 171 | 26.8% |
| May be | 78 | 12.2% | |
| No | 389 | 61.0% | |
| Did you squeeze your eyes | Rarely | 172 | 27.0% |
| Sometimes | 390 | 61.1% | |
| Usually | 76 | 11.9% |
Table 2 demonstrates general population awareness regarding keratoconus. Exact of 269 (42.2%) of the participants heard about KC and 219 (34.3%) correctly defined the disorder. Blindness as a complication of KC was reported by 262 participants (41.1%). Regarding risk factors of KC, 52.4% of the participants told about family history, 38.9% told about intensive use of electronic devices, and 30.9% reported for intensive eye friction. Surgical intervention as management for KC was reported by 394 (61.8%) participants and 46.6% reported that wearing glass limit KC progression. Regarding management methods, 49.2% reported eye glass or lenses with surgery and 42% told that they don't know about management methods. In total, good awareness was detected among 119 (18.7%) participants [Figure 1].
Table 2.
Awareness of general population regarding keratoconus, Aseer region, Saudi Arabia
| Keratoconus awareness items | No | % | |
|---|---|---|---|
| Know about keratoconus | No | 369 | 57.8% |
| Yes | 269 | 42.2% | |
| Keratoconus definition | Thin protruded cornea | 219 | 34.3% |
| Thick cornea | 54 | 8.5% | |
| Corneal inflammation | 29 | 4.5% | |
| Don’t know | 336 | 52.7% | |
| Keratoconus causes blindness | Yes | 262 | 41.1% |
| No | 65 | 10.2% | |
| Don’t know | 311 | 48.7% | |
| Keratoconus risk factors | Intensive use of electronic devices | 248 | 38.9% |
| Non wearing glass for those with visual defect | 182 | 28.5% | |
| Family history | 334 | 52.4% | |
| Hard eye friction | 197 | 30.9% | |
| Keratoconus need surgical intervention | Yes | 394 | 61.8% |
| No | 34 | 5.3% | |
| Don’t know | 210 | 32.9% | |
| Wearing glass limit KC progression | Yes | 297 | 46.6% |
| No | 68 | 10.7% | |
| Don’t know | 273 | 42.8% | |
| Management methods for KC | Eye drops | 14 | 2.2% |
| Eye glass or lenses with surgery | 314 | 49.2% | |
| Only glass | 28 | 4.4% | |
| Nothing | 14 | 2.2% | |
| Don’t know | 268 | 42.0% | |
| KC needs continues assessment and evaluation | Yes | 460 | 72.1% |
| No | 15 | 2.4% | |
| Don’t know | 163 | 25.5% |
Figure 1.
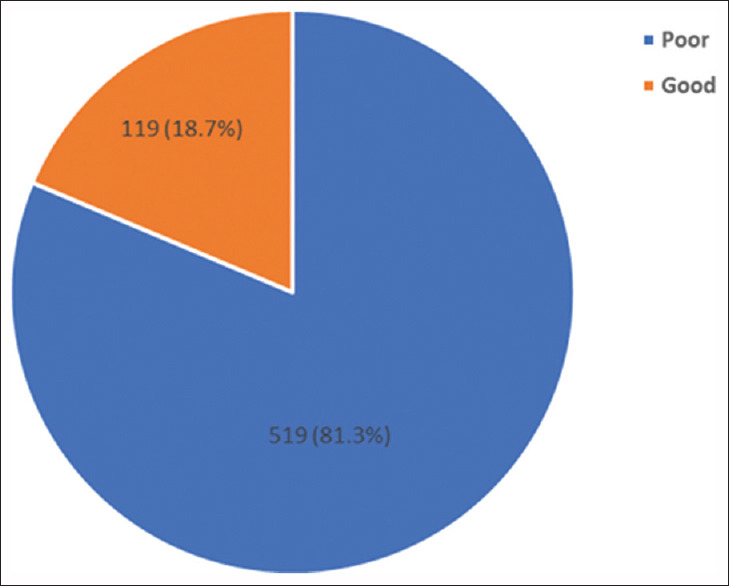
Overall awareness level regarding keratoconus
Figure 2 illustrates public source of information regarding KC. Family and friends was the most reported source (29.2%) followed by internet (18%), health care staff (11%), and affected family member (2.5%). About 38% of the participants had no specific source of information.
Figure 2.
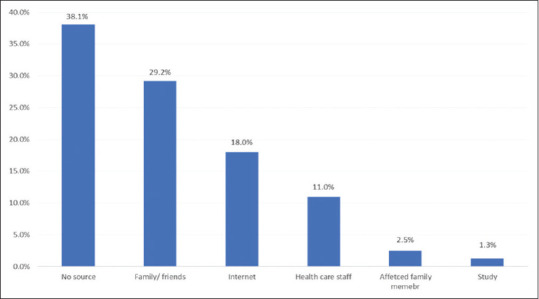
Source of information regrading keratoconus among general population in Aseer region
Distribution of awareness level by participants personal data was demonstrated in Table 3. It was found that 23.6% of participants aged 30–39 years old had good awareness level compared to 9.1% of old participants with recorded statistical significance (P = 0.049). Also, good awareness regarding KC was detected among 37.3% of those who had the disorder compared to 16.7% of those who were did not (P = 0.001). Exact of 21.1% of the participants who had progressive declined vision had good awareness regarding KC compared to 19.8% of those who said no (P = 0.028). Besides, good awareness regarding KC was detected among 75% of those who had their information during study compared to 3.7% of those who had no source (P = 0.001).
Table 3.
Distribution of awareness level by participants personal data, Aseer region, Saudi Arabia
| Personal data | Awareness level | P | ||||
|---|---|---|---|---|---|---|
| Poor | Good | |||||
| No | % | No | % | |||
| Age in years | < 20 years | 21 | 80.8% | 5 | 19.2% | 0.049* |
| 20-29 | 141 | 77.9% | 40 | 22.1% | ||
| 30-39 | 94 | 76.4% | 29 | 23.6% | ||
| 40-49 | 183 | 83.2% | 37 | 16.8% | ||
| 50+ | 80 | 90.9% | 8 | 9.1% | ||
| Gender | Male | 272 | 82.2% | 59 | 17.8% | 0.578 |
| Female | 247 | 80.5% | 60 | 19.5% | ||
| Education | Basic | 149 | 87.1% | 22 | 12.9% | 0.069 |
| High | 33 | 76.7% | 10 | 23.3% | ||
| University/more | 337 | 79.5% | 87 | 20.5% | ||
| Do you have keratoconus | Yes | 37 | 62.7% | 22 | 37.3% | 0.001* |
| May be | 49 | 83.1% | 10 | 16.9% | ||
| No | 433 | 83.3% | 87 | 16.7% | ||
| Complain of continuous declined vision | Yes | 135 | 78.9% | 36 | 21.1% | 0.028* |
| May be | 72 | 92.3% | 6 | 7.7% | ||
| No | 312 | 80.2% | 77 | 19.8% | ||
| Did you squeeze your eyes | Rarely | 136 | 79.1% | 36 | 20.9% | 0.077 |
| Sometimes | 327 | 83.8% | 63 | 16.2% | ||
| Usually | 56 | 73.7% | 20 | 26.3% | ||
| Source of information regarding KC | Internet | 91 | 79.1% | 24 | 20.9% | 0.001* |
| Study | 2 | 25.0% | 6 | 75.0% | ||
| Health care staff | 40 | 57.1% | 30 | 42.9% | ||
| Family/friends | 139 | 74.7% | 47 | 25.3% | ||
| Affected family member | 13 | 81.3% | 3 | 18.8% | ||
| No source | 234 | 96.3% | 9 | 3.7% | ||
P: Pearson X2 test. *P<0.05 (significant)
Discussion
The current study aimed to assess population awareness regarding keratoconus in Aseer region. This is essential to delineate attention to recognize deformity zones in open information and attempt to cover. This is crucial for appropriate identification of keratoconus cases which thus limit its difficulties which may end with complete visual deficiency. The investigation uncovered that about 10% of the members revealed having keratoconus and one quarter grumbled of dynamic visual disability. Altogether, great mindfulness with respect to keratoconus was recognized among about 1 out of every five participants. Nearly half of the participants heard about keratoconus and one third correctly defined disease in correct terms. Also, nearly half of the participants correctly named the disease complications and consequences besides its risk factors. Not all participants identified the management methods of keratoconus, but the majority said that it needs continuous assessment. The most detailed wellspring of data was loved ones, family members either straightforwardly or through their affection with the diseases. Health care staff as a source was in the third order and this mean that they should pay more effort in raising public awareness. Regarding determinants of public awareness, young age, high education, having the disorder of at least visual problems, being physician as the main source of information were the most important predictors.
These findings were mostly consistent with a study conducted in Saudi Arabia to assess awareness among non-medical students toward keratoconus.[14] The examination uncovered that the greater part of the investigation members never heard about KC; moreover, just 32 (8.1%) became acquainted with about KC through their physician. A total of 238 (60.6%) students did not know what KC. is Nearly 40% reported that KC is thinning of cornea and only 33.6% told that KC leads to myopia and astigmatism. More than 90% of the students disagreed on presence of association between keratoconus and allergic eye disease. Just a single fifth accept that KC has a genetic foundation. 347 (88.3%) of the investigation member didn't have the foggiest idea how to treat the KC There were no measurably noteworthy contrasts (no statistical difference) among males and females. All around, the degree of awareness about the disorders and the accessible strategies for treatment would improve the visualization and limit the social, mental, and monetary weight and handicap of influenced people. Scientists revealed a pattern of inappropriate of the health-care system in the developed countries as well as Saudi Arabia.[15,16] Keratoconus (KC) is a chronic progressive thinning of the cornea that results in myopia and irregular astigmatism[17,18,19]
Conclusions
In conclusion, the study revealed that public awareness in Aseer region regarding keratoconus was moderately poor with defect regarding treatment modalities and its consequences.
Key Points
Medicinal services staff was faulty and questionable which implies more consideration ought to be paid to improve health care providers health education skills. More large scale studied are recommended to first detect the magnitude of keratoconus disorder among general population and to construct and validate effective health education programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Muhammad Abid Khan for statistical support and valued contribution.
References
- 1.Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: A review. Contact Lens Anterior Eye. 2010;33:157–66. doi: 10.1016/j.clae.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Wachler BS, Chandra NS, Chou B, Korn TS, Nepomuceno R, Christie JP. Intacs for keratoconus. Ophthalmology. 2003;110:1031–40. doi: 10.1016/s0161-6420(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 3.Li SW, Li ZX, Shi WY, Zeng QY, Jin XM. Clinical features of 233 cases of keratoconus. [Zhonghua yan ke za zhi] Chinese J Ophthalmol. 2005;41:610–3. [PubMed] [Google Scholar]
- 4.Owens H, Gamble G. A profile of keratoconus in New Zealand. Cornea. 2003;22:122–5. doi: 10.1097/00003226-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Millodot M, Shneor E, Albou S, Atlani E, Gordon-Shaag A. Prevalence and associated factors of keratoconus in Jerusalem: A cross-sectional study. Ophthalmic Epidemiol. 2011;18:91–7. doi: 10.3109/09286586.2011.560747. [DOI] [PubMed] [Google Scholar]
- 6.Gordon-Shaag A, Millodot M, Kaiserman I, Sela T, Barnett Itzhaki G, Zerbib Y, et al. Risk factors for keratoconus in Israel: A case–control study. Ophthalmic Physiol Opt. 2015;35:673–81. doi: 10.1111/opo.12237. [DOI] [PubMed] [Google Scholar]
- 7.Naderan M, Rajabi MT, Zarrinbakhsh P, Naderan M, Bakhshi A. Association between family history and keratoconus severity. Curr Eye Res. 2016;41:1414–8. doi: 10.3109/02713683.2015.1128553. [DOI] [PubMed] [Google Scholar]
- 8.Galvis V, Tello A, Carreño NI, Berrospi RD, Niño CA. Risk factors for keratoconus: Atopy and eye rubbing. Cornea. 2017;36:e1. doi: 10.1097/ICO.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 9.Gorskova EN, Sevost’ianov EN. Epidemiology of keratoconus in the Urals. Vestnik Oftalmologii. 1998;114:38–40. [PubMed] [Google Scholar]
- 10.Jonas JB, Nangia V, Matin A, Kulkarni M, Bhojwani K. Prevalence and associations of keratoconus in rural maharashtra in central India: The central India eye and medical study. Am J Ophthalmol. 2009;148:760–5. doi: 10.1016/j.ajo.2009.06.024. [DOI] [PubMed] [Google Scholar]
- 11.Hofstetter HW. A keratoscopic survey of 13,395 eyes. Optometry Vision Sci. 1959;36:3–11. doi: 10.1097/00006324-195901000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101:267–73. doi: 10.1016/0002-9394(86)90817-2. [DOI] [PubMed] [Google Scholar]
- 13.Al-Amri AM. Prevalence of keratoconus in a refractive surgery population. J Ophthalmol. 2018;2018:5983530. doi: 10.1155/2018/5983530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Amri AM, Al-Ghamdi AS, Al-Khabbaz FI, Al-Qallaf AA, Siddiqui JJ, Al-Sadiq FA, et al. Level of awareness among non-medical students toward keratoconus, Abha, Saudi Arabia. Saudi J Health Sci. 2020;9:7. [Google Scholar]
- 15.Kymes SM, Walline JJ, Zadnik K, Sterling J, Gordon MO Collaborative Longitudinal Evaluation of Keratoconus Study Group. Changes in the quality-of-life of people with keratoconus. Am J Ophthalmol. 2008;145:611–7. doi: 10.1016/j.ajo.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma R, Titiyal JS, Prakash G, Sharma N, Tandon R, Vajpayee RB. Clinical profile and risk factors for keratoplasty and development of hydrops in north Indian patients with keratoconus. Cornea. 2009;28:367–70. doi: 10.1097/ICO.0b013e31818cd077. [DOI] [PubMed] [Google Scholar]
- 17.Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. BioMed Res Int. 2015. p. 795738. https://doi.org/10.1155/2015/795738 . [DOI] [PMC free article] [PubMed]
- 18.Shehata AEM, Foster JW, Jun AS, Soiberman US. The correlation between corneal findings and disease severity in keratoconus per scheimpflug corneal tomography. J Ophthalmol. 2020;2020:6. doi: 10.1155/2020/4130643. Article ID 4130643. https://doi.org/10.1155/2020/4130643 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belin MW, Rapuano CJ, Tan DTH. Keratoconus: New Consensus, New Goals. EyeNet Magazine. 2020 [Google Scholar]


