Abstract
One Health is a well-recognized concept; however, it has been at the fringe of most operational health policies rather than being the central theme. Although, global experts and policy makers have agreed on this theory, the transition from a vision to practical application is inconspicuous. COVID-19 pandemic has caused massive damage to the world economy and continues to peril human lives everywhere. Ignorance of the principles of One Health approach in the current health care system has proved to be the Achilles heel of our health policy. Social distancing, lockdown, and hand hygiene are short-term preventive measures imposed by nations worldwide but are difficult to sustain in the long run. Thus, it is long overdue that we change our unidimensional approach regarding the control and prevention of diseases. A rational practice of the One Health strategy should be our utmost priority to control the ongoing grave situation. The purpose of this article is to bring the attention of healthcare professionals and researchers toward the One Health paradigm for the betterment of public health while combating COVID-19 and to prepare for future emergence of infectious diseases. Our assessment for this review is based on the philosophy and views shared by recent publications on the One Health approach which emphasizes an integrated, multisectoral, and holistic concept (animal health-human health-environmental factors) and promotes a transdisciplinary-integrated tactic for disease prevention and control.
Keywords: COVID-19, One Health, pandemic, SARS-CoV-2, zoonotic diseases
Introduction
The world is experiencing a major health crisis due to the irrepressible spread of a respiratory illness labelled as COVID-19, caused by a novel coronavirus, i.e., the SARS-CoV-2. From its first appearance in China in late December 2019 to presently affecting more than 200 countries and territories within few months, COVID-19 is rapidly transmitting across the globe with an escalating number of positive cases and deaths. As on March 11, 2020, the World Health Organization (WHO) declared COVID-19 as a pandemic and a public health emergency of severe consequences. After genomic characterization and identification of phylogenetic analysis of coronavirus, multiple nations are competing to develop an effective vaccine and most are progressing toward human clinical trials.
As per the situation report-209 released by WHO on August 16, 2020, the number of confirmed cases has reached 21,294,845 with 7,61,779 deaths worldwide. Besides the appalling data and human misery, coronavirus-driven socioeconomic loss of several countries demands us to revisit the “One Health” concept that was designed many years ago as an all-inclusive approach incorporating the direct impact of environmental epidemiology on human and animal health.[1] According to WHO, health is a “state of complete physical, mental and social well-being and not merely the absence of disease and infirmity”. To attain a healthy state, humans cannot overlook the essential contribution of coexisting species—animals and plants—since we share the same environment and ecosystem. Human health, animal health, and environmental factors are inextricably dependent on each other. Therefore, “Health” as a concept should not be confined to the well-being of human beings only. The commonalities between animal and human health have long been recognized by the concept of “One Medicine” which is an intersection of the veterinarians and human health. After the outbreak of Severe Acute Respiratory Syndrome (SARS) in 2003, the “One Medicine” concept evolved into an improved all-inclusive approach of “One Health” which incorporated the direct impact of environmental epidemiology on human and animal health. As stated by the One Health Initiative Task Force, “One Health is the collaborative efforts of multiple disciplines working locally, nationally, and globally, to achieve optimal health for people, animals, and our environment.” This approach is governed by public health experts, leaders from governments and nongovernmental health organizations, economic sectors and ecologists, etc., These global experts need to review and scrutinize policies necessary for the prevention of potential outbreaks. Globally and regionally, we must develop a feasible, sustainable, and cutting-edge model for addressing disease outbreaks that work on the concept of One Health by considering it as the fundamental theme on which future environmental, economical, and medical advancements are based on.
In current times, when the whole world is fighting a pandemic and undergoing an unprecedented collapse of economies, the transition from just “health” to the broader concept of “One Health” is pivotal for achieving improved public health outcomes. We must robustly work and invest in developing altruistic environmental and health policies for the betterment of all species by understanding the complex interface between environment and health.
Human and Animal Interface
A large number of infectious diseases are zoonotic, which means they originate in animals and are transmitted to humans. Various factors like climate change, population explosion, international travel, global trade, biodiversity loss, erratic human lifestyle along with mutations and variations in pathogens have contributed to the threat of emergence and spread of newer infectious diseases like SARS, Middle East Respiratory Syndrome (MERS), and COVID-19. Since 2003, humans have encountered three coronavirus-related health emergencies. The skipping over of diseases from one species to another is majorly dependent upon ecosystem conditions. With the world becoming a smaller place due to previously mentioned factors, the transcontinental spread of infectious diseases like H1N1, influenza, and COVID-19 has become much easier.[2] Humans are unvaryingly dependent on animals for their livelihood and food requirements (livestock).
It has been postulated that COVID-19 originated in a city of China, Wuhan. The outbreak was traced back to the first reported cluster of pneumonia cases of unknown etiology identified from the seafood market of Wuhan; the market not only trades freshly killed wild animals but also supplies living animals for human consumption. It has been hypothesized that the initial entry in human population was either through direct contact with the infected animal or via eating the undercooked meat of an infected animal. Another possibility can be the arrival of the virus by illegal transport of animal meat from a distinct region. The emergence of highly pathogenic Asian avian influenza A also happened in a similar way and it also originated from a poultry outbreak.
To understand the complex interdependency of animal–human health and environment with clarity, a classic example would be the infection caused by the “West Nile Virus,” which is transmitted to humans from mosquitoes. Herein, the ideal approach would require monitoring of mosquito population (breeding season & duration, favorable conditions), the migration pattern of birds carrying the virus (carrier animal dynamics), and the climate conditions (environmental factor) that generate suitable conditions for mosquitoes to breed. One of the major issues regarding flu viruses is the constantly changing genome of these viruses as they undergo mutations while evolving, and hence, can affect other species including humans by conveniently entering the food chain. The reciprocal transmission can also occur through humans to animals as shown by the recent reports of SARs-CoV-2 being isolated from animals; two cats in New York, a tiger from Bronx zoo, and later on three more lions and tigers were found to have been harboring the virus. The zoo officials believe that the spread of coronavirus might have been through infected zookeepers. Many human cases are asymptomatic as well; therefore, safe hygiene practices and regular health checkups of zoo animals and their handlers is the only way to prevent the spread from animal to human and vice versa. Overall, the protection of animal health is required to protect human health.
The principles of One Health will be useful in dealing with COVID-19 which is thought to originate from animals and then got transmitted to human population suggesting that such viruses thrive on the human–animal interface and are driven by environmental parameters. Apart from the spread of zoonotic diseases, other concerns include antimicrobial resistance, environmental contamination, and food safety measures, etc., The animal source of COVID-19 is still unidentified, some virologists have suggested bats at the contenders as they are the only flying mammals which can carry multiple pathogens while others suggest that it is from pangolins. However, we must not forget that this pandemic is a result of the continuous negligence of environmental degradation by human activities. Therefore, human beings are the only species accountable to overcome this crisis.
Human and Environment Interface
One of the reasons for the Ebola outbreak in West Africa was deforestation bridging the gap between wildlife and human habitat. Nipah virus spread was related to the upsurge in the migration of fruit bats and avian influenza was linked to unchecked poultry farming. Human manipulations like biodiversity change, intensified production of livestock, illegal trade of wildlife, and climate change have directly or indirectly contributed to the emergence of novel infectious diseases. Our persistent destruction of wildlife due to explosive population growth has brought us near to the wild animals and plants that foster pathogens that can move from animals to humans. Also, global warming, toxic pollution from vehicles and factories, and urban expansion have threatened nature to the core. These infectious zoonotic diseases can be both a cause or a consequence of biodiversity loss.
The pandemic has just reiterated the simple fact that humans like most animals are equally vulnerable to environmental conditions. A similar view is shown in Figure 1.[3] Now, to address the present and future pandemics effectively, a collective One Health method will be vital which involves protecting human and animal health by managing chemical wastes, monitoring biodiversity, ecosystem change, and by reducing carbon footprint. Human exposure to novel pathogens is also done by industries like oil exploration and mining. Moreover, climate change is a major player in the progression of infectious diseases as virus distribution and population size are affected by local climate fluctuations.
Figure 1.
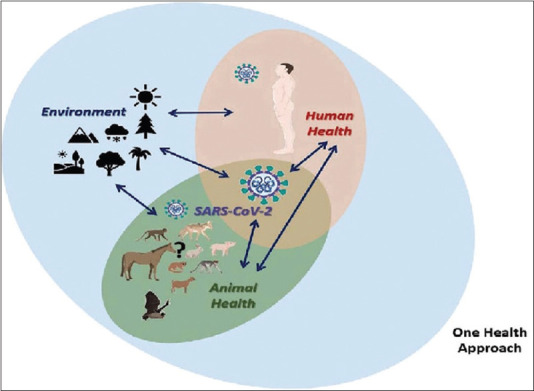
Schema displaying the interconnection and potential spread of coronavirus between human health, animal health, and environment. Adapted from Bonilla-Aldana et al
According to the researchers, generally various pathogens keep circulating in milder forms in animals living in undistributed habitats but if the balance is disturbed; they move out of their natural distribution and come in contact with human population, they usually jump the interspecies barrier by undergoing mutations and then infect humans and other species. Similarly, coronavirus transmission is likely an overall effect of globalization and natural habitat destruction. Here, the direct nexus between disease outbreaks and deforestation is evident. One of the aims of the One Health approach should be reducing deforestation and forest fragmentation which will subsequently decrease the interaction between the virus-carrying wildlife species and humans. Therefore, for achieving a future with improved human and animal health, we need to also consider environmental health to maintain the natural equilibrium.
Importance of One Health approach for COVID-19
As mentioned by CDC (Centers for Disease Control and Prevention), the foundation of the One Health approach comprises communication, coordination, and collaboration. This combined holistic method will surely reduce the occurrence and spread of such infections if done under the supervision of experts from different sectors like animal health (veterinarians), environmental health (ecologists, agricultural workers, and wildlife experts), and human health (doctors, epidemiologists, and public health experts). It would require an intense amalgamation of various bodies like WHO, various health organizations and national governments leading to the formulation and implementation of stringent policies including laws and penalization for successful application of One Health idea at a global level. In the interim, people have been following the nonpharmaceutical interventions: washing hands regularly, social distancing by staying at home, self-quarantine if found sick, masking, and following the instructions applied by authorities to contain the spread of infection. Interestingly, India has used a unique pharmaceutical intervention by allowing the use of hydroxychloroquine (HCQ) as prophylaxis among health care workers, the results of which will certainly be interesting to look at in the coming days. However, even with all these measures, we will only be able to delay the rapid spread of virus to a certain level and the final numbers of deaths and affected people may remain the same. Moreover, the data of the conversion of active cases to recovered individuals are not promising enough. We all are familiar with the good old saying “Prevention is better than cure%” but foremost it is important to recognize the stage at which prevention should be executed and fully beneficial. The current preventive measures are important but merely useful to slow the spread of virus which at present is already residing in human and animal populations.
On the other hand, by taking preemptive precautions at early stages of transmission before it reaches animal–human interface or by regular monitoring of the animal health and environment conditions, we can reduce the damage to a much larger extent. Therefore, the aim is to catch such infectious diseases before they even become epidemic and constitute remedial measures. On the optimistic note, as the pandemic has evolved and along with it the measures like social distancing, nationwide lockdowns with minimum human movement have shown positive impacts on the environment, whether it is clearer water bodies or better air quality index (AQI) due to reduction in pollutants and carbon emission. Therefore, we can regain a state of a healthy atmosphere to live by allowing the Earth to recover and by strictly monitoring human actions to avoid future pandemic. As suggested by experts,[4] a transformative change comprising the reorganization of responsibilities in different economic, scientific, and social sectors along with proper funding for research and health and increase in science budget by governments is needed to construct better health facilities. For instance, supply of personal protective equipment for health professionals who are working in frontline, is falling short at this crucial stage. The possibility and effectiveness of the One Health concept have been verified and argued previously.[5] Moreover, it has been proved as a superior approach for disease prevention over other conventional methods. Although, it is not a simple and straightforward method and requires a lot of multidisciplinary actions by many experts and professionals of several fields; however, it is still a better cost-effective investment as compared to the situation we are currently in. Presently, the uncertainty and anxiety related to COVID-19 is increasing rapidly with the number of affected cases; hence, we also need psychologists to manage people's mental health issues.[6] Authorities of One Health commission and medical professionals should demand the enforcement of improved guidelines for environmental and industrial regulation.
Key points
Human health, animal health, and environment are dependent on each other.
Over the years climate change, population explosion, biodiversity destruction, globalization etc., have led to outbreak of infectious diseases
Current pandemic demands for collaborative One Health approach globally.
Implementation of One Health strategies by all stakeholders will help to prevent further spread.
Conclusion
We must adopt “One World, One Health” philosophy from global to the most local levels to avoid any impending pandemics which are likely to occur more often considering the exponentially increasing global population and urbanization. In India, One Health approach is receiving a positive response from multiple sectors, however, we still stand in a preliminary stage and need to adapt useful strategies of international standards to provide the finest healthcare facilities.[7,8] Surveillance of emerging and re-emerging zoonotic diseases of public health importance is the only way forward.[9,10] Future decisions regarding human development must embrace both people and nature at its core with sustainability at the forefront.[11,12] We must robustly work and invest in developing altruistic environmental and health policies for the betterment of all species by understanding the complex interface between environment and health.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
None
References
- 1.Van Helden PD, Van Helden LS, Hoal EG. One world, one health. Humans, animals and the environment are inextricably linked-a fact that needs to be remembered and exploited in our modern approach to health. EMBO Rep. 2013;14:497–501. doi: 10.1038/embor.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El Zowalaty ME, Jarhult JD. From SARS to COVID-19: A previously unknown SARS- related coronavirus (SARS-CoV-2) of pandemic potential infecting humans-Call for a One Health approach. One Health. 2020;9:100124. doi: 10.1016/j.onehlt.2020.100124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonilla-Aldana DK, Dhama K, Rodriguez-Morales AJ. Revisiting the one health approach in the context of COVID-19: A look into the ecology of this emerging disease. Adv Anim Vet Sci. 2020;8:234–6. [Google Scholar]
- 4.Settele Joef, Dias Sandra, Brondizio Eduardo, Dszak Peter IPBES Expert Guest Article. COVID-19 stimulus measures must save lives, protect livelihoods, and safeguard nature to reduce the risk of future pandemics. 2020 Apr 27; [Google Scholar]
- 5.Rabinowitz PM, Kock R, Kachani M, Kunkel R, Thomas J, Gilbert J, et al. Toward proof of concept of a one health approach to disease prediction and control. Emerg Infect Dis. 2013;19:e130265. doi: 10.3201/eid1912.130265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neil G, Mary D, Sam G, Simon W. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 7.Aggarwal D, Ramachandran A. One health approach to address zoonotic diseases. Indian J Community Med. 2020;45(Suppl 1):S6–8. doi: 10.4103/ijcm.IJCM_398_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryu S, Kim BI, Lim J-S, Tang CS, Chun BC. One health perspectives on emerging public health threats. J Prev Med Public Health. 2017;50:411–4. doi: 10.3961/jpmph.17.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zoonotic Diseases of Public Health Importance. [Last accessed on 2019 Sep 06]. Available from: https://ncdc.gov.in/WriteReadData/l892s/File618.pdf .
- 10.USAID-Emerging Pandemic Threats. [Last accessed on 2020 Jun 20]. Available from: https://www.cbd.int/health/onehealth-casestudies2016-final-en.pdf .
- 11.Mushi V. The holistic way of tackling the COVID-19 pandemic: The one health approach. Trop Med Health. 2020;48:69. doi: 10.1186/s41182-020-00257-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foddai A, Lindberg A, Lubroth J, Ellis-Iversen J. Surveillance to improve evidence for community control decisions during the COVID-19 pandemic – Opening the animal epidemic toolbox for public health. One Health. 2020;9:100130. doi: 10.1016/j.onehlt.2020.100130. [DOI] [PMC free article] [PubMed] [Google Scholar]


