Abstract
Various factors interplay when it comes to successful containment of pandemic. In last one year, we have witnessed various countries formulating and practicing their own unique ways to tackle coronavirus. We have seen the most developed countries failing terribly and unable to slow the COVID-19 spread, but at the same time also endorsed the comparatively less resourceful countries outperforming in terms of reduced disease morbidity and mortality. Current review is about two regions from India (Dharavi and Kerala) who were different in their approach as compared to rest of the country and were able to keep the COVID-19 cases to the minimum.
Keywords: Coronavirus, Pandemic: Global health
Introduction
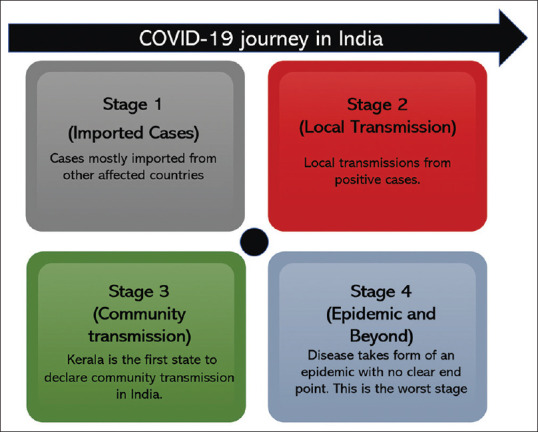
World health Organisation (WHO) declared Coronavirus disease 2019 (COVID-19) as a 'Public Health Emergency of International Concern’ on 30 January 2020.[1] As of 5 November 2020, the COVID-19 disease has affected more than 48 million, and has led to the death of 1.23 million people.[2] India prepared for the pandemic with the development of a national emergency plan and the early establishment of screening at entry points and molecular diagnostic facilities across the country with a network of public health laboratories. Kerala was the first state in India to report the very first case of COVID-19 on 30 January 2020. India has the 2nd highest disease burden and continues to witness one of the fastest-growing COVID-19 pandemics in the world [Table 1]. In India, as of 5 November 2020, the cases of COVID-19 has passed over 8 million with a death toll of 124K, with Maharashtra, Karnataka and Andhra Pradesh reporting the highest number of cases [Figure 1].[3] Presently the disease numbers are still rising in some places after showing a declining trend in most of the states while the government is opening the economy and removing any movement restrictions. The lockdowns and travel restriction enforced during initial months were soon found to be not sustainable as a long term solution. There are successful models within India that could be reapplied to tame the disease in regions seeing rise in cases within the country and even in other low resource countries across the globe.
Table 1.
Number of infections, deaths, Case fatality rate (CFR) of various countries and Kerala
| Country | Cases | Death | Recovered | CFR (%) |
|---|---|---|---|---|
| USA | 10,058,586 | 242,230 | 6,391,208 | 3.04 |
| Brazil | 5,632,505 | 162,035 | 5,064,344 | 3.13 |
| Italy | 862,681 | 40,638 | 322,925 | 13.29 |
| France | 1,661,853 | 39,865 | 126,329 | 11.22 |
| Canada | 255,809 | 10,436 | 211,237 | 7.13 |
| China | 86,184 | 4,634 | 81,131 | 5.44 |
| Russia | 1,733,440 | 29,887 | 1,296,124 | 1.72 |
| India | 8,462,080 | 125,605 | 7,819,886 | 1.80 |
| Maharashtra | 17,10,314 | 44,965 | 15,62,342 | 3.19 |
| Dharavi | 3750 | NA | 3182 | NA |
| Kerala | 4,73,469 | 1,641 | 3,88,504 | 0.40 |
*On 11/07/20 (https://www.worldometers.info/coronavirus/)
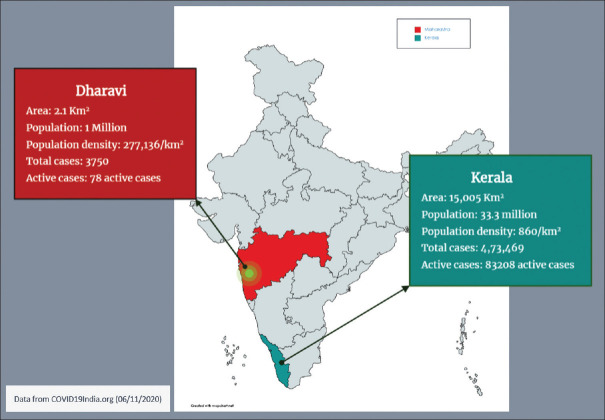
Figure 1.
Stages of Transmission of SARS CoV-2 in India
Through this article, we aim to discuss the success story of two Indian regions, Kerala (State of India) and Dharavi (densely populated sub-urban region in the state of Maharashtra).
Lesson from Kerala Response to Coronavirus
Kerala has one of the India's best performing health care system. It has performed exceptionally well during previous outbreaks e.g., Nipah virus (NiV) outbreak (2018) for which WHO also praised Kerala for its emergency preparedness. Kerala government and Public health responses team worked synchronously in 3 domains during Nipah virus outbreak i.e., Coordination structure, Performance of surveillance & interventions, and Assessment of reduction of transmission.[4]
Kerala's a Used a Multipronged Approach Against COVID-19
Surveillance activities
The core principles used for disease control were monitoring the spread in the localities, study the patterns of spread, and stringent application of methods to contain the disease.[5,6] Kerala started by screening at every portal of entry such as Airports, rail-routes, sea-routes, They separated symptomatic and asymptomatic patients, Symptomatic passenger send to dedicated COVID hospital for further treatment and asymptomatic passengers were advised for strict home quarantine. Kerala government is doing three types of surveillance Sentinel (4414), Pooled sentinel (164898), Airport surveillance (77231).[7] The State had already gained experienced in contact tracing during the NiV outbreak. For stringent contact tracing, multiple steps were taken; field teams were involved, and route map were developed and follow up of all contacts was ensured. As per the standard definition, anyone who came in contacts to laboratory confirmed COVID-19 case is considered as a primary contact. Similarly, individuals who were in contact of primary contacts would be labeled as secondary contact. Also, all contacts were mandatory put into quarantine to prevent the community spread. This was the “Cluster care” method to mitigate the spread of the virus by strengthening testing, treatment, quarantine. Cluster are formed based on unexpected surge in COVID-19 cases at a particular area, followed by cluster divided into three zones for better coordination and focus. Each cluster is assigned to specific health officials. Contact tracing of the cluster is started based on the findings of positive cases. This is followed by enhanced active search and testing all contacts, home isolation of confirmed and asymptomatic/mildly symptomatic cases, and home quarantine of contacts. To date (August 29, 2020) 1643633 were tested, out of which 71701 were found to be positive cases.[8] ICMR already did a study for sero surveillance in 3 district Palakkad, Ernakulum, Thrissur in 1193 population but the results have not yet been shared. A second ICMR sero surveillance has started in same district.[9]
Continuing treatment services
To cope up with COVID-19 pandemic. Kerala launched COVID first line treatment centers (CFLTC) in each district in coordination with the Local self-government institution (LSGI). The CFLTC were linked with designated COVID hospital established during the pandemic. CFLTC Staff consist of Block Medical officers, CFLTC Nodal officers, Medical officers, staff nurse, Lab technician, Field staff, pharmacist, Attendant, Data entry operators, Ambulance drivers, Security staff volunteers. The main role of CFLTC is to provide institutionalized care and treatment for mild or asymptomatic patients of COVID positive patients. In addition, State health services efficiently continued treatment services to the patients suffering from diseases other than COVID- 19 like hemophilia, thalassemia, and chronic renal disorders and so on. A Triage system was setup in CFLTC i.e., with Category A, B, C.
Category A is symptomatic, Category B is symptomatic, Category C is with severe symptoms are referred to COVID hospitals. Simultaneously Telemedicine shall be used in CFLTC to ensure that specialist consultation is provided to the required patients in CFLTC. COVID Brigade is formed in Kerala state to take charge of CFLTC due to shortage of manpower. The brigade consist of volunteer doctors, nurses and other health workers to be trained for intensifying the fight against COVID-19.[10,11]
Community participation
The Kerala state has highest literacy rates amongst all the states in India which has probably helped the habitants to understand their responsibility during this health crisis. Also, this made easy for the state officials to generate awareness about the “Do's” and “Don'ts” during this pandemic. So far, the empowered women self-help groups -namely “Kudumbashree members” proved to be of extremely useful and visited door to door to all households, gave special attention to the elderly, stressed on psychological wellbeing and provided continuity of care. In addition, they are also supporting Government initiatives related to COVID such as providing foods to the patients in COVID centers, preparing PPE kits e.g., face shields, delivering essential medications in situation of lockdown and so on. 'Ottakalla Oppamundu’ it means “You are not alone, I am with you” is a program for providing Psychosocial support to the people in quarantine, isolation, school children and other categories of population as well as to the community in general. So far, more than 1 million people have been benefited by psychosocial support (PSS) group.[12]
Advocacy and social mobilization for behavioral change
The state sponsored establishment called as “Corona Safe Network,” is constantly motivated to ensure COVID-19 awareness amongst its people. Corona Literacy Mission is a special section of Corona Safe Network which translated the most UpToDate content from the WHO website to Malayalam (language spoken in Kerala). An awareness campaign 'Break the Chain’ was successful in promoting the importance of hand hygiene, physical distancing, and cough etiquette. Hand washing stations were installed in strategic locations, including exit and entry points of railway stations etc.[13] The state's chief minister gave the call: “Physical distance and social unity- that is our slogan at this time.”
Such measures by the Kerala government were of extremely helpful in maintaining a low number of active cases that prevented overwhelming medical facilities and critical care units. On 23 June, in recognition of pandemic efforts, the UN felicitated the State Health Minister K.K. Shailja on the occasion of UN Public Service Day.[14] The state is seeing recent reemergence of cases, but it has already taken effective action once, learnt its lessons and hopefully control it again.[15] A Washington post story expressed that intensive testing and rigid contact tracing was the key strategy to control Coronavirus in Kerala state,[16] that flattened the epidemiological curve within 100 days.[17]
“Dharavi Model: Mission Dharavi Chasing the Virus”
Dharavi fought the coronavirus with a strategy of attack not defense, leading to flattening of the curve within 2 months , which many experts deemed nearly impossible.[18] One of the most established methods to prevent person to person transmission, “social distancing” was and still is very difficult to practically follow in the most crowded and dense slum of Asia. Almost 80% of the population of Dharavi depend on the 450 community toilets. Groups of 8-10 people share houses measuring 10 × 10 feet. Among these houses function many small-scale factories on the 2nd and 3rd floors. Dharavi has approximately 5000 Goods and services tax enterprises, 15000 one room small scale factories, and also acts as nidus for many international exports and contributes to the State revenue with an annual turnover of 1 billion USD [Figure 2].[19]
Figure 2.
Demographic details of the Dharavi and Kerala
Indian council of Medical Research (ICMR) in their recent report mentioned that urban slum areas have approximately double the chance of developing a local coronavirus outbreak as compared to urban areas.[20] Urban slums have always been susceptible to disease and need novel solutions in the settings of resource scarcity. Dharavi had an early emergence of the outbreak once it set foot in Mumbai, with a 12% growth rate, and 491 cases in April. The average doubling rate in April was just 18 days. With each passing month, the average doubling rate kept showing improving trend (In August- 406 days, in July- 300 days, in June-108 days, and in May-43 days). Similarly, the Dharavi's average growth rate of COVID-19 cases showed trend of declining values from 4.3% in May to 0.24% in August.[21] In spite of the near impossible nature of the task the local administration and civic bodies successfully curtailed the outbreak with the 4Ts: Tracing, Tracking, Testing and Treating. WHO has been applauding the Dharavi Model and countries like Philippines starting to follow the model.[22,23]
Aggressively Minimizing Infection: Trace, Track, Test and Treat
The local health officials in Dharavi were very prompt and as soon as the 1st case was confirmed, the municipality corporation barricaded the area, sanitized all 425 community washrooms, initiated door to door screening, inspection was reinforced, private and community physicians in the hot spot were engaged, with help of NGOs community kitchens, quarantine and treatment facilities were established and a strict lockdown was ensured with 24 checkpoints.[18]
Mumbai's G North ward, which is Dharavi, reduced spread of COVID 19 significantly by the use of contact tracing.[24] Contact tracing lead to most of the positive cases already being in quarantine, thereby effectively minimizing the chain of transmission. Initially outbreak was led by dispersed cases all over the slum with no linkage. The administration managed this by pro-actively screening door to door to find out any missed cases. BMC set up fever clinics to trace and test anyone with symptoms. These fever camps were set up in different areas of the slum everyday so as to reach as many slum dwellers as possible. The fever clinics covered 47,500 houses. Mobile vans also helped screen around 14970 people. Special attention and care were provided to the 8246 seniors. Many private and community physicians volunteered for their service, and they were provided adequate protective devices, gloves, pulse oximeters, temperature measuring scanners, and face masks to screen people in all high-risk areas.[25]
Strict enforcement of the lockdown was ensured by the aid of 24 checkpoints, monitored entry and exit points, drones, and volunteer “COVID Yoddhas” or “COVID warriors”. Only the sick patients were allowed outside with 90% being treated within Dharavi. Schools, sports complexes, marriage halls were converted into institutional quarantine centers for suspected people to stay. These facilities made sure that the quarantined got free meals, medicines, vitamins, and “Laughter yoga” sessions., A 200-bed hospital was set up with oxygen supply within 14 days to cater to the patients in Dharavi. Ration Kits, food packets and Community kitchens were made available so that no one was left hungry.[26,27]
The learnings from the Dharavi model
This model was low cost and sustainable so it can be replicated in other low resource settings and low-income countries. Because of community engagement and participation there is very little threat of resistance or non-cooperation from the community.
While being cautiously optimistic, the surveillance and monitoring must continue with the easing of travel restrictions and opening of the economy. The Dharavi Mission model had limited the number of cases to mostly single digits till now. Recently, few hot spots with reports of increasing infection has been detected.[28] Dharavi has four extremely dense populated localities; the Matunga Labour Camp, Kumbharwada, Kala Killa, and Koliwada. These localities are being monitored continuously by Brihanmumbai Municipal Corporation, even after flattening of the COVID-19 curve in mid-June.[29]
Government and health officials of these locations were very serious from the beginning of the pandemic and knew that the threat of second and subsequent surge doesn't go away in settings of overcrowding, water scarcity, sharing of public toilets, poor waste management systems and deprivation. In all, Dharavi has been engaged in a strong and successful fightback against COVID-19 crisis and has also set an example the importance of comprehensive planning and execution of operational guidelines to rest of the states of India.[30,31]
The role of primary care physician
Primary care physicians (PCPs) have always been an important pillar of our health care system. Their importance as “trustworthy and reliable source of information” has never been felt like this before across the globe.[32] They are the first point of contact in most cases, hence their responsibility during this pandemic has increased exponentially to stay updated about the current affairs both at the regional, national and global platform.
PCPs hold the key role in educating the ground taskforce, keeping a track of surveillance systems, triaging the contacts and patients and many more. There role would be more crucial during Nov-Feb when common cold is usually at its peak, which is the amongst the closest mimicker to COVID-19.[33] While cases are going down in India, it is important to keep a note about the second COVID-19 surge which many countries have started to witness.[34] We should be vigilant and ready for second surge and PCPs are important assets of the taskforce.[35]
Conclusion
As both these places, Kerala and Dharavi have shown that this pandemic can be controlled with timely, coordinated action with the participation of the community. There are similar examples from within India and around the world where low resource settings have been successful in containing this ravaging pandemic. The pillars of all these success stories have been effective quarantine, isolation, contact tracing, multi-sectoral involvement and community participation. These models could help health administrators plan an effective strategy to control new infection foci in other areas too. But this is a long haul, and the efforts need to continue till an effective vaccine or therapy is widely and easily available.
Key Points
-COVID-19 has hit hard the semi-urban regions which are densely populated and have low socioeconomic strata, however “Dharavi Model” has shown that a well-structured algorithm and dedicated task force can reduce the COVID-19 related morbidity and mortality to a significant level.
- Success of Dharavi and Kerala models in containing COVID-19 spread indicates that decentralization of resources, door to door contact tracing, and re-enforcing the role of ground level workers are key factors for successful and timely containment of disease.
Ethical statement
The article does not contain participation of any human being and animal.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Emergency-committee-regarding-the-outbreak-of-novelcoronavirus-(2019-ncov) 2005. [Last accessed on 2020 Jun 20]. Available from: https://www.who.int/news-room/detail/30-01-2020-statementon-the-second-meetingof-the-international-healthregulations .
- 2.Worldometer. COVID-19 coronavirus pandemic. 2020. Available from: https://www.worldometers.info/coronavirus/
- 3.Coronavirus daily updates, 2020. Available from: https://www.covid19india.Org .
- 4.Fact sheet Nipah virus infection, World Health Organization, South East Asia region. [Last accessed on 2020 Aug 28]. Available from: https://www.who.int/southeastasia/outbreaks-and-emergencies/healthemergency-information-risk-assessment/surveillanceand-risk-assessment/nipah-virus-outbreak-in-kerala .
- 5.India Today. Community transmission in Kerala. Available from: https://www.indiatoday.in/india/story/coronavirus-community-transmission-in-kerala-govtresumes-scrutiny-1703448-2020-07-23 .
- 6.World Health Organization. Global Surveillance for COVID-19 Caused by Human Infection with COVID-19 Virus: Interim Guidance, 20 March 2020. Geneva: World Health Organization; 2020. [Google Scholar]
- 7.Directorate of Health service, Government of Kerala, 2020. Available from: https://dashboard.kerala.gov.in/testingview-public.php .
- 8.Directorate of Health service, Government of Kerala, 2020. Available from: https://dashboard.kerala.gov.in/index.php .
- 9. Available from: https://www.thehindu.com/news/national/kerala/sero-surveillance-survey-yields-unexpected-results/article31948214.ece .
- 10.Directorate of Health service, Government of Kerala, 2020. Available from: https://dhs.kerala.gov.in/wp-content/uploads/2020/06/SOP-CFLTC-140.06.20.docx.pdf .
- 11.COVID-19 Jagratha. Available from: https://covid19jagratha.kerala.nic.in/home/covidBrigade .
- 12.Directorate of Health service, Government of Kerala, 2020. Available from: http://dhs.kerala.gov.in/wp-content/uploads/2020/08/Bulletin-HFWD-English-August-29.pdf .
- 13.World Health Organization. South East Asia News. Responding to COVID-19-Learnings from Kerala. Available from: https://www.who.int/india/news/feature-stories/detail/responding-to-covid-19---learnings-from-kerala .
- 14.Jalan J, Sen A. Containing a pandemic with public actions and public trust: The Kerala story. Indian Econ Rev. 2020;55:105–24. doi: 10.1007/s41775-020-00087-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Times of India. Highest single day spike in Kerala. Available from: https://timesofindia.indiatimes.com/city/thiruvananthapuram/highest-single-day-spike-in-keralawith-over-3000-covid-19-cases/articleshow/77964850.cms .
- 16.The Washington Post. Available from: https://www.washingtonpost.com/world/aggressive-testing-contacttracing-cookedmeals-how-the-indian-state-of-keralaflattened-its-coronavirus-curve/2020/04/10/3352e470-783e-11ea-a311-adb1344719a9_story.html .
- 17.Thankappan KR. Combating corona virus disease 2019 and comorbidities: The Kerala experience for the first 100 days. Int J Noncommun Dis. 2020;5:36–42. [Google Scholar]
- 18.Golechha M. COVID-19 containment in Asia's largest urban slum Dharavi-Mumbai, India: Lessons for policymakers globally. J Urban Health. 2020:1–6. doi: 10.1007/s11524-020-00474-2. doi: 10.1007/s11524-020-00474-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Times of India. Explained: How Mumbai's Dharavi flattened the Covid-19 curve. Available from: https://timesofindia.indiatimes.com/india/explained-how-mumbais-dharaviflattened-the-covid-19-curve/articleshow/76910062.cms .
- 20. Available from: https://swarajyamag.com/insta/icmrserosurvey-just-073-per-cent-of-population-had-evidenceof-past-exposure-to-coronavirus .
- 21.Hindustan Times. After Thursday spike of 17 Covid cases, Dharavi report 3 on Friday. Available from: https://www.hindustantimes.com/india-news/after-Thursday-s-spikeof-17-covid-cases-dharavi-reports-3-on-friday/storyqibWuylVRof9p3MefOShXK.html .
- 22.WHO lauds BMC's efforts to check Covid transmission in Dharavi. Indian Express. July 2020. Available from: https://indianexpress.com/article/india/who-lauds-bmcs-effortsto-check-covid-transmission-in-dharavi-6501337/
- 23.India Today. Chase the virus: Philippines govt to follow India's ‘Dharavi model’ to fight Covid-19. Available from: https://www.indiatoday.in/india/story/chase-the-virusphilippines-govt-to-follow-india-s-dharavi-model-to-fightcovid-19-1712398-2020-08-18 .
- 24.India Today. Contact tracing reduced spread of Covid-19 in Dharavi by 42%, says BMC. Available from: https://www.indiatoday.in/india/story/contact-tracingreduced-spread-of-covid-19-in-dharavi-by-42-saysbmc-1666608-2020-04-13 .
- 25.Times of India. Explained How Mumbai's Dharavi flattened the Covid-19 curve. Available from: https://timesofindia.indiatimes.com/india/explained-how-mumbais-dharaviflattened-the-covid-19-curve/articleshow/76910062.cms .
- 26.Times of India. Available from: http://timesofindia. indiatimes.com/articleshow/76910062.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst .
- 27.The Logical Indian. Tracing, Tracking, Testing, Treating: How Mumbai's Dharavi Flattened COVID-19 Curve. Available from: https://thelogicalindian.com/good-governance/mumbais-dharavi-flattened-covid-19-curve-22259 .
- 28.Mumbai mirror. COVID-19 Dharavi sees slight jump in fresh cases, Dadar report 19 new cases. Available from: https://mumbaimirror.indiatimes.com/coronavirus/news/covid-19-dharavi-sees-slight-jump-in-fresh-cases-dadar-reports-19-new-cases/articleshow/77852923.cms .
- 29.Hindustan Times. Parliament monsoon session. Available from: https://www.hindustantimes.com/india-news/suspension-of-question-hour-unjust-cpi-leader-writes-torajya-sabha-chairman/story-zqiX0WaTvxiBxboCEvTAHK.html .
- 30.WHO. 2019 Novel Coronavirus (2019-nCoV): Strategic preparedness and response plan. Geneva, Switzerland, 2020. Available from: https://www.who.int/publicationsdetail/strategic-preparedness-and-response-plan-for-thenewcoronavirus .
- 31.Sahu KK, Mishra AK, Lal A, Sahu SA. India Fights Back: COVID-19 Pandemic. Heart Lung. 2020;49:446–8. doi: 10.1016/j.hrtlng.2020.04.014. doi: 10.1016/j.hrtlng.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kearon J, Risdon C. The role of primary care in a pandemic: Reflections during the COVID-19 pandemic in Canada. J Prim Care Community Health. 2020;11:2150132720962871. doi: 10.1177/2150132720962871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sahu KK, Mishra AK, Martin K, Chastain I. COVID-19 and clinical mimics. Correct diagnosis is the key to appropriate therapy. Monaldi Arch Chest Dis. 2020:90. doi: 10.4081/monaldi.2020.1327. doi: 10.4081/monaldi.2020.1327. [DOI] [PubMed] [Google Scholar]
- 34.Benham TL, Hart A, Bortolin M, Court M, Groves J, Kraus A, et al. Preparing for the second surge: Preventing posttraumatic stress disorder and building resilience for health care workers in the face of COVID-19. Disaster Med Public Health Prep. 2020:1–4. doi: 10.1017/dmp.2020.371. doi: 10.1017/dmp.2020.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sahu KK, Kumar R. Preventive and treatment strategies of COVID-19: From community to clinical trials. J Family Med Prim Care. 2020;9:2149–57. doi: 10.4103/jfmpc.jfmpc_728_20. [DOI] [PMC free article] [PubMed] [Google Scholar]