Abstract
Background:
Patient understanding of plan of care is associated with positive outcomes in ambulatory settings. In hospital medicine settings, patient-physician agreement on plan of care (concordance) has been limited and difficult to improve. This study examined the impact of adding a hospitalist to interdisciplinary rounds (IDR) on physician-patient-nurse concordance and the relationship between concordance and outcomes.
Methods:
IDR were conducted by core teams made up of unit-based nurses, a case manager, and a pharmacist. Over time, with cohorting, hospitalists were included in IDR (hospitalist IDR) for some patients assigned to unit-based hospitalists. In developing hospitalist IDR, researchers emphasized using an IDR checklist, including a patient communication plan. Patient-nurse-physician interviews were used to assess concordance in the domains of diagnosis, tests and procedures, and expected discharge date. Using two-hospitalist review, agreement was rated as none, partial, or complete, and a total concordance score was calculated for each patient in both IDR groups. Multivariate analysis was used to examine the relationship between concordance, IDR type, patient factors, and utilization outcomes.
Results:
For 658 patients, the mean concordance score was 11.71 out of a possible 18. There was no difference in concordance between hospitalist and core IDR groups (11.68 vs. 11.84, p = 0.7). Higher total concordance score was associated with lower lengths of stay (p < 0.001) and readmission rates (p = 0.001). Total concordance had a negative association with patient age (p = 0.04).
Conclusion:
Concordance did not change with IDR type. Higher concordance appears to be related to positive utilization outcomes. Future studies are needed to evaluate potential interventions to improve concordance.
Improving patient understanding of their prescribed plan of care has been an area of increasing focus in recent years.1-3 One measure of patients’ understanding of care is the agreement between patient and clinicians on aspects of their care processes. Patient-physician agreement on plan of care (concordance) has been measured in several studies in the outpatient setting,4-6 hospital medicine,7-9 and surgical settings.10 In several of these studies, concordance between physician and patient was used as a surrogate for patient understanding of plan of care. Concordance was also used as a measure of the quality of communication or development of a shared mental model among clinical team members.
Concordance of plan of care has been measured between physicians and nurses8,9 and between physicians and patients.7 These studies have shown that patient knowledge of plan of care is limited.7 Also, cohorting physicians to units9 or time spent communicating with nurses8 did not substantially improve concordance. In hospitalized patients, understanding of, and agreement to, plan of care are necessary, given the need for self-care in the post-acute hospitalization period, yet they are hard to achieve. This may be attributed to sickness causing impairment in understanding and retention,11 shortening hospital stays,12 hospitalists who are not typically known to patients, and the dynamic nature of inpatient teams.7 Outpatient studies have demonstrated that patient knowledge could contribute to positive patient outcomes.13-15 We can cautiously extrapolate these findings to inpatient studies, although continuity of care may play a role in the positive outcomes in ambulatory settings. Hospitalists face the challenge of having to develop a shared mental model despite the limitations of patient understanding in acute care settings. So it would be of value to understand the strength of the shared mental model in hospital medicine units, interventions to improve it, and its relationship to outcomes. We were interested in assessing the shared mental model of plan of care as concordance between physicians, patients, and nurses. Given the complex nature of hospital unit operations that typically include more nurse-patient interactions (hourly nurse rounding) than physician-patient interactions, we believe the true assessment of the shared mental model lies in triadic concordance between the three roles at the bedside.
In many inpatient settings, the multidisciplinary team responsible for care on a given unit conducts daily huddles in which care team members discuss each patient during a process known as interdisciplinary rounds (IDR).16 IDR in our institution began in 2009. Initial implementation called core IDR included a bedside nurse, a nurse coordinator or charge nurse acting as rounds manager,16 a case manager, a social worker, and a pharmacist. Nurses and rounds managers were historically unit based (in other words, all clinical assignment was localized to one unit). During IDR implementation, case managers, social workers, and pharmacists were also assigned to units. Between 2012 and 2014, due to hospitalist engagement, hospitalists were added to IDR. This led to the development of hospitalist IDR. However, hospitalist localization to units was difficult due to the need to balance census, given that units ranged in size between 30 and 40 patients. Average hospitalist census was 15 patients. As a result, most units had two hospitalists who carried the majority of patients and an additional one to two floater (multiunit) hospitalists that had a few spillover patients from unit-based hospitalist lists. Therefore, each unit had a variable proportion of core and hospitalist IDR on a daily basis. Hospitalist list distributors typically started with filling up the lists of unit-based hospitalists. When unit-based hospitalists reached their goal census of 15 patients, the distributors would fill the overflow hospitalist lists. There was no patient selection process to fill these lists. Prior to the implementation of hospitalist IDR, two units piloted bedside hospitalist IDR to include patients; however, IDR were moved to nursing districts due to team member concerns about longer time spent in bedside IDR. IDR implementation also included a rounding checklist (Appendix 1, available in online article). During implementation of IDR in nursing districts, emphasis was placed on patient and family communication, and teams were asked to identify an appropriate team member who would communicate with the patient/family every day. IDR leadership was provided at a department level and also at a unit level by the unit nurse manager, medical director, and rounds manager.
We acknowledge that bedside IDR would lead to the most improvement in concordance over core IDR, but we believe hospitalist IDR provide an opportunity for incremental increase in triadic concordance through better nurse-physician communication. Therefore, we hypothesized that hospitalist inclusion in morning IDR, along with a focus on patient and family communication, would give physicians and nurses more opportunities to discuss a unified plan of care with patients and families; this would improve team communication and thereby triadic concordance. We studied whether hospitalist IDR compared to core team IDR are associated with improved concordance between patients, physicians, and nurses, and whether improved concordance is associated with improved outcomes in hospital utilization and patient experience.
METHODS
Setting and Participants
The study was conducted on four general medicine units at an independent, tertiary care, academic medical center in Newark, Delaware, from April 2014 to June 2015. IDR are conducted Monday through Friday. Diagnosis, plan of care for the day and the hospital stay, and anticipated discharge date were addressed in hospitalist IDR, along with a safety and quality checklist (Appendix 1). The discussion points were similar in core team IDR, but because the physician was absent, diagnosis and plan of care were obtained by chart review (when available) from progress notes and information carried forward by nursing handoffs.
In this prospective cohort study, we enrolled patients, their hospitalists, and their nurses as interview participants. Study patients were adult ( > 18 years) general medicine inpatients admitted through the emergency department from April 2014 to June 2015. Step-down patients, teaching patients, hospice patients, confidential patients, confused patients, and patients otherwise having difficulty communicating (hard of hearing, limited English proficiency) were excluded. Patients admitted from the emergency department Monday through Thursday, 9:00 a.m. to 7:00 p.m., were eligible to ensure consistent staffing and next-day IDR occurrence for all patients in the cohort. Informed consent was obtained for interviews. Hospitalists and nurses taking care of enrolled patients were also interviewed after informed consent was obtained. The study was approved by the Institutional Review Board at ChristianaCare Health Services.
Enrollment Procedure
Patients admitted to the study units from emergency department were screened for eligibility by a research nurse the day after admission. The research nurse then met with rounds managers on all units after morning rounds and collected data on study patients. IDR status was assigned to patients based on type of IDR that was completed on the second day of hospitalization. Switching from one medicine unit to another was not ordinarily allowed; as a result, IDR type switches were extremely rare. We therefore did not collect data on switching units. Research assistants completed next-level screening by speaking with the bedside nurse. Their input was final in excluding patients for inability to participate due to confusion, aggressive behavior, or acute symptomology that might make interview participation difficult. Research assistants met all patients screened through this process. Final patient enrollment occurred at the patient’s bedside with obtaining informed consent. Research assistants were undergraduate students trained and supervised by a research nurse with overall project management responsibility. Each research assistant observed the research nurse conducting a minimum of five patient interviews and was observed interviewing at least five patients before independently conducting interviews.
Interview Procedure
We used a modified version of the survey instrument used in previously completed inpatient medicine concordance studies.7 Interviews addressed three major domains of plan of care, in addition to questions related to physician and nurse identification, and health literacy assessment using a Single Item Literacy Screener (SILS).17 The SILS is a modified health literacy instrument that was developed to efficiently identify patients who have difficulty with a central aspect of health literacy: reading health-related materials. The goal of this instrument is to identify patients who need help with written or printed material, regardless of the etiology (for example, limited education, language barrier, physical impairment).The question responses are on a five-point Likert scale from never to always. The clinical interview domains included patients’ knowledge of (1) their diagnosis, (2) tests and procedures planned on the day of interview, and (3) their anticipated discharge date. Research assistants aborted interviews if the patient could not follow the survey despite repeated explanation. Responses were captured verbatim. After the patient interview, research assistants interviewed consenting nurses and physicians separately using the three domains of plan of care as above. Names of staff members were not collected as data points to maintain anonymity and for blinding. However, nurses and physicians frequently were in both groups, and there was no group of hospitalists or nurses that was limited to either core IDR or hospitalist IDR. Every effort was made to conduct hospitalist, patient, and nurse interviews in temporal proximity to one another to minimize confounding due to evolving plans as discordance. All data were entered into electronically readable forms (TeleForm) and were scanned into the research database. See Appendix 2 (available in online article) for the research assistant interview guide.
Physician Review Procedure
Two pairs of board-certified hospitalists [S.M. and H.R.; C.U. and S.N.] were trained to review all patient-hospitalist-nurse interviews. Reviewer training resembled training in similar studies.7 Reviewers were blinded to type of IDR, unit, and all patient, nurse, and hospitalist identifying information. Each hospitalist independently reviewed interview responses to assess agreement on three domains of plan of care among patient-physician, patient-nurse, and nurse-physician pairs. Agreement was rated as complete, partial, or none. Details of rating are included in Appendix 3. The research nurse reviewed independent ratings to identify disagreements. To maximize inter-rater reliability, all identified disagreements were adjudicated by the principal investigator [V.S.B.] with each pair of physicians present in person. At the end of the adjudication process, all disagreements were resolved by consensus.
Data Analysis
We did not collect process metrics and qualitative metrics regarding IDR for this study. Based on operational data, IDR were conducted between 9:00 a.m. and 11:00 a.m. on all units; most units spent 60 to 90 minutes in total, with 30 to 40 patients per unit. Unit managers, medical directors, and nurse coordinators provided stable leadership support to IDR from 2012 to 2015. Interviews were conducted Tuesday through Friday for all enrolled patients. The research team had a cohort of research assistants on a rotating schedule; as a result, no days for data collection were missed with the exception of holidays. Data were collected on nearly 100% of scheduled weekdays during the 15-month period.
Concordance Score
We coded no agreement, partial agreement, and complete agreement as “0,” “1,” and “2,” respectively. Each relationship (physician-nurse, physician-patient, and nurse-patient) allowed one opportunity to attain complete agreement, leading to a range of scores from 0 to 6. Each domain of plan of care (diagnosis, anticipated discharge date, and tests and procedures) allowed one opportunity to attain complete agreement, leading to a range of scores from 0 to 6. Using this framework, we calculated a single concordance score for each patient across three relationships and three domains, leading to a range of scores from 0 to 18, similar to previous studies7 (Appendix 4).
Covariates and Outcome Metrics
From each patient’s electronic health record, we collected demographic data, including age, gender, race, payer, and initial admission status (inpatient vs. observation). Expected mortality risk obtained from the Vizient (formerly University HealthSystem Consortium) database was also used as a surrogate measure for illness severity.18, 19 Expected mortality risk is defined as the probability of death during a single episode of care. The probability is calculated from discharge abstracts and includes adjustments for differences in patient severity using the All Patient Refined Diagnosis Related Groups (APR-DRG), developed by 3M Health Information Systems.20 Patient identification of hospitalist and SILS score were also included as covariates. Some of the study patients were also admitted through an interdisciplinary admissions process, and this information was also used as a covariate. Length of stay (LOS), readmission rates, and individual Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores were obtained from administrative databases.
Statistical Analyses
We treated total concordance score as a continuous variable in analyses. We used univariate analyses to assess relationship between concordance and covariates, including age, gender, race, ethnicity, payer, SILS score, IDR type, unit, hospitalist group, knowing name of hospitalist, and expected mortality. In multivariate analyses, we examined the relationship between concordance and age, gender, race, ethnicity, payer, SILS score, IDR type, unit, hospitalist group, knowing name of hospitalist, and expected mortality individually, while adjusting for the remaining factors. We used logistic regression to analyze 30-day readmissions adjusted for age, gender, race, ethnicity, payer, SILS score, IDR type, unit, hospitalist group, knowing name of hospitalist, and expected mortality. We used a linear model assuming a gamma distribution to analyze the relationship between total concordance and LOS adjusted for age, gender, race, ethnicity, payer, SILS score, IDR type, unit, hospitalist group, and expected mortality. Because LOS was skewed in this sample, a graph of log (LOS) vs. concordance is given with a loess line showing the trend. We compared the mean concordance scores across three dyad pairs (physician-nurse, physician-patient, and nurse-patient) in core IDR and hospitalist IDR groups. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina).
RESULTS
Patient Characteristics in Concordance Groups
A total of 658 patients were included in the analysis. Appendix 5 shows a consort diagram accounting for patients from enrollment to analysis. The mean (standard deviation [SD]) concordance score for the sample was 11.71 (3.90) out of a total possible of 18. The mean (SD) of expected risk of mortality was 0.01 (0.03).
IDR and Concordance
The mean total concordance score in core team IDR ( n = 108) and hospitalist IDR (n = 550) was 11.84 and 11.68, respectively (p = 0.7). Adjusted analyses also showed no significant difference between the two IDR groups. Table 1 shows patient characteristics and covariates in core IDR and hospitalist IDR groups. Pair subgroup (physician-nurse, patient-nurse, and patient-physician) analyses of concordance also showed no significant difference in both IDR groups (Table 2).
Table 1.
Patient Characteristics in IDR Groups
| Covariate | Core IDR (n = 108) |
Hospitalist IDR (n = 550) |
P Value |
|---|---|---|---|
| Age (years) mean (SD) | 62.4 (15.7) | 61.0 (15.9) | 0.42 |
| Expected mortality (expected probability of death in an episode of care) mean (SD) | 0.009 (0.013) | 0.01 (0.028) | 0.55 |
| Female n (%) | 62 (57.4) | 291 (52.9) | 0.39 |
| Race n (%) | 0.04 | ||
| Black | 28 (25.9) | 118 (21.5) | |
| White | 76 (70.4) | 427 (77.6) | |
| Other | 4 (3.7) | 5 (0.9) | |
| Ethnicity n (%) | 0.06 | ||
| Hispanic | 4 (3.7) | 14 (2.5) | |
| Not-Hispanic | 101 (93.5) | 533 (96.9) | |
| Unknown | 3 (2.8) | 3 (0.5) | |
| Unit of rounding n (%) | < 0.001 | ||
| 5B | 7 (6.5) | 176 (32.0) | |
| 5C | 11 (10.2) | 185 (33.6) | |
| 5D | 24 (22.2) | 167 (30.4) | |
| 6E | 66 (61.1) | 22 (4.0) | |
| Hospitalist group n (%) | 0.51 | ||
| Employed | 31 (28.7) | 141 (25.6) | |
| Private | 77 (71.3) | 409 (74.4) | |
| Payer n (%) | 0.74 | ||
| Commercial | 25 (23.1) | 154 (28.0) | |
| Medicaid | 16 (14.8) | 73 (13.3) | |
| Medicare | 64 (59.3) | 305 (55.5) | |
| Other | 3 (2.8) | 18 (3.3) | |
| SILS score n (%) | 0.12 | ||
| Never need help | 58 (53.7) | 341 (62.0) | |
| Rarely need help | 19 (17.6) | 83 (15.1) | |
| Sometimes need help | 20 (18.5) | 63 (11.5) | |
| Often need help | 3 (2.8) | 33 (6.0) | |
| Always need help | 8 (7.4) | 30 (5.5) | |
| Knowing hospitalist’s name n (%) | 0.03 | ||
| Correct | 14 (13.0) | 121 (22.0) | |
| Don’t know/incorrect | 94 (87.0) | 429 (78.0) |
IDR, interdisciplinary rounds; SD, standard deviation; SILS, Single Item Literacy Screener.
Table 2.
Total Concordance and Relationship Subgroup Concordance in IDR Groups
| Total Concordance |
Patient/Physician Concordance |
Patient/Nurse Concordance |
Physician/Nurse Concordance |
|||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | p | Mean (SD) | p | Mean (SD) | p | Mean (SD) | p | |
| Core IDR | 11.84 (+/− 4.11) | 0.7 | 3.55 (+/− 1.77) | 0.34 | 3.78 (+/− 1.70) | 0.31 | 4.52 (+/− 1.37) | 0.48 |
| Hospitalist IDR | 11.68 (+/− 3.87) | 3.56 (+/− 1.68) | 3.80 (+/− 1.60) | 4.33 (+/− 1.42) | ||||
IDR, interdisciplinary rounds; SD, standard deviation.
Patient Characteristics and Concordance
Table 3 shows means of concordance for categorical variables and association with concordance in univariate analyses. In multivariate analyses, patient age had a significant negative association with concordance (p = 0.04); expected mortality and identification of hospitalist did not have a significant association with concordance.
Table 3.
Patient Characteristics and Relationship with Concordance
| Covariate | Values | Total Concordance for Categorical Variables Mean (SD) |
Relationship with Concordance |
p Value |
|---|---|---|---|---|
| Age median (IQR) | 62.1 (50.6–71.7) | Older age associated with lower concordance | 0.04 | |
| Gender n (%) | No association | 0.25 | ||
| Male | 353 (53.6) | 11.86 (3.95) | ||
| Female | 305 (46.4) | 11.53 (3.83) | ||
| Race n (%) | No association | 0.31 | ||
| White | 503 (76.4) | 11.78 (3.85) | ||
| Black | 146 (22.2) | 11.46 (3.99) | ||
| Other | 9 (1.4) | 11.33 (5.07) | ||
| Identification of hospitalist n (%) | 0.80 | |||
| Correct | 135 (20.5) | 12.88 | No association | |
| Incorrect | 70 (10.6) | 11.81 | ||
| Don’t know | 453 (68.8) | 11.33 | ||
| Ethnicity n (%) | No association | 0.28 | ||
| Hispanic or Latino | 18 (2.7) | 13.5 (3.76) | ||
| Non-Hispanic or Latino | 634 (96.4) | 11.64 (3.89) | ||
| Unknown | 6 (0.9) | 12.66 (4.67) | ||
| Payer n (%) | No association | 0.12 | ||
| Commercial | 179 (27.2) | 12.27 (3.77) | ||
| Medicaid | 89 (13.5) | 11.62 (3.99) | ||
| Medicare | 369 (56.1) | 11.33 (3.95) | ||
| None/Other | 21 (3.2) | 13.76 (2.44) | ||
| SILS score n (%) | No association | 0.47 | ||
| Never need help | 399 (60.6) | 11.97 (3.84) | ||
| Rarely need help | 102 (15.5) | 11.46 (3.76) | ||
| Sometimes need help | 83 (12.6) | 11.12 (4.32) | ||
| Often need help | 36 (5.5) | 11.5 (3.37) | ||
| Always need | 38 (5.8) | 11 (4.34) | ||
| IDR status n (%) | No association | 0.70 | ||
| Core IDR | 108 (16.4) | 11.84 (4.11) | ||
| Hospitalist IDR | 550 (83.6) | 11.68 (3.86) | ||
| Hospital unit of admission n (%) | No association | 0.13 | ||
| 5B | 183 (27.8) | 11.79 (3.60) | ||
| 5C | 196 (29.8) | 11.27 (4.10) | ||
| 5D | 191 (29.0) | 11.77 (4.09) | ||
| 6E | 88 (13.4) | 12.34 (3.56) | ||
| Hospitalist group n (%) | ||||
| Employed group | 172 (26.1) | 12.13 (3.85) | No association | 0.09 |
| Private group | 486 (73.9) | 11.55 (3.92) | ||
| Expected mortality (expected probability of death in an episode of care) mean (SD) | 0.011 (0.03) | No association | 0.80 |
SD, standard deviation; IQR, interquartile range; SILS, Single Item Literacy Screener; IDR, interdisciplinary rounds.
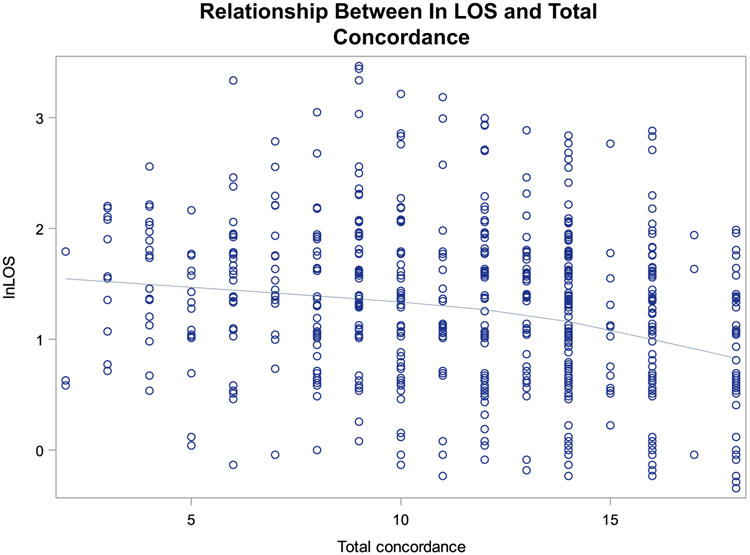
Concordance and Outcomes
LOS decreased as total concordance increased. The findings were similar in multivariate models adjusting for expected mortality and other patient characteristics (p < 0.001) (Figure 1). Higher concordance was also associated with lower 30-day readmission rates (p = 0.001). There was a 9% decrease in the odds of readmission for every point increase in total concordance score. We had fewer than 50 responses for HCAHPS scores on this sample (less than 10% response rate), and we did not include this in analyses as it was too small to be meaningful.
Figure 1:
This chart displays the relationship between In LOS (inpatient length of stay) and total concordance.
DISCUSSION
This prospective cohort study showed several new findings related to a shared mental model of plan of care in inpatient medicine. Concordance among hospitalists, patients, and nurses was generally limited. The addition of hospitalists to core team in IDR was not associated with higher concordance in this study, even in the physician-nurse subgroup. Higher concordance was associated with lower age. Higher concordance appeared to be associated with improved utilization outcomes such as a decrease in LOS and 30-day readmission rates when adjusted for illness severity.
Changing core IDR to hospitalist IDR was not sufficient to lead to improvement in concordance in this study. We hypothesized that adding a hospitalist to IDR would bring more concrete information to the team earlier in the day, leading to better patient-physician-nurse communication throughout the day. It is possible that bedside IDR are needed to lead to a true improvement in concordance. It is also possible that the limitation in hospitalist IDR may be due to IDR fidelity or inadequate adherence to patient and family communication after IDR. We did not measure either fidelity or adherence in this study. It is more surprising to see that physician-nurse concordance also did not improve with hospitalist IDR. One reason for this could be poor communication, due to either unnecessary IDR variability or individual communication skills. Another reason could be that hospitalists who did not participate in IDR have developed workflows to communicate with nurses, thereby reducing the difference in concordance between hospitalist and core IDR. In addition, we did not address individual physician and nurse communication practices that may have influenced understanding. In recent years, a number of studies have examined shared understanding of plan of care by looking at the shared understanding between patients and physicians7 and physicians and nurses8, 9 in hospital medicine. Concordance of plan of care is lacking for a substantial number of patients.7 Physician-nurse concordance is not achieved by cohorting physicians to units9 or increasing the amount of time spent communicating.8 This study adds that including hospitalists in IDR was not enough to improve total concordance or physician-nurse concordance. Comparing concordance with hospitalist IDR to bedside IDR will be important for future studies. In institutions without bedside IDR, it may be useful to study the benefit of a standardized patient/family communication plan on concordance.
Higher concordance was associated with patient age, a nonmodifiable factor. SILS score, illness severity, and knowing the hospitalist by name showed no relationship to concordance. Based on these findings, we hypothesize that patient age and probably other unmeasured factors may contribute to how information is processed by hospitalized patients. It is worth considering that patient communication may be difficult to improve using systemic interventions such as IDR and may have to be tailored to individual patients at the point of care with careful assessment of understanding at every step. This recommendation is consistent with patient education literature supporting the use of the teach-back method of teaching and real-time assessment of understanding.21, 22 Similar to other concordance studies, we measured concordance once, at the beginning of the hospital stay on the second day. As a result, we may have underestimated concordance overall; patients may understand better closer to the day of discharge. This may need to be assessed in future studies.
It is reasonable to think that less sick patients may need simpler explanations, leading to higher concordance. However, the lack of association between illness severity and concordance in this study contradicts this thinking. It is possible that engaged patients who receive good explanations may understand their care plans regardless of illness severity. Some sicker patients may be more engaged, as they are more worried. These findings have to be explored in larger studies. These considerations do not apply to confused patients, who were excluded from our study.
The association between higher concordance and lower LOS and probability of readmissions is a useful finding. Outpatient studies have reported that patient-physician agreement can improve medication adherence,14 decrease drug errors in heart failure patients,23 improve patient and physician perception of improvement,24 and improve patient adherence to consultant recommendations in the geriatric setting.13 To our knowledge, there are no inpatient studies demonstrating a relationship between concordance and utilization outcomes. Even when adjusted for illness severity, this study showed that concordance may be related to a decrease in LOS. However, hospital efficiency is not generally thought to be a metric of patient knowledge of plan of care. We postulate that patients who are aware of the potential date of discharge are better prepared to be discharged, thereby leading to a planned and efficient discharge. This finding needs validation in larger, targeted studies.
Studies suggest that patient understanding of discharge-related plan of care can reduce readmissions through increased patient activation and engagement.25, 26 It is reasonable to assume a similar relationship between understanding of plan of care and patient experience. We did not have enough data to explore this relationship in this study. The relationship between concordance and patient experience should be explored in future studies. Similarly, further studies are needed to understand the relationship between concordance and other patient-centered outcomes, such as return to emergency room and 30-day mortality.
These findings have several implications for future research and clinical operations. Is concordance one of the variables that can influence outcomes? Our findings should be confirmed in larger studies. If concordance is useful, hospitals could strive toward improving patient understanding of care plan and aiming toward higher concordance from admission through discharge. Although plans evolve over time, sharing anticipated hospital trajectory could help with improving patient understanding and preparation for next steps. Because hospitals and hospitalists consistently make efforts to educate patients about their care, it may be worth considering real-time assessment of patient understanding and tailoring information delivery at the bedside. In addition, we did not examine the relationships between domains of concordance and total concordance. Such analyses may uncover hidden relationships between IDR and concordance and between concordance and outcomes. These deeper analyses may be useful to further this body of knowledge.
Limitations
This study has limitations. It was a single-center study; as a result, our findings may not be fully generalizable to other institutions. Because this was an observational study, it is difficult to establish clear links between exposure and outcomes. We did not assess education, financial status, psychological resilience, and baseline functional status that could play a role in utilization outcomes. However, we used SILS as a proxy for education and insurance as a proxy for financial factors, requiring a cautious interpretation of these findings. In addition, the association of higher concordance with lower LOS may be confounded by fewer tests and procedures, fewer hospitalist transitions, or lower complexity. We used illness severity to mitigate this, but there may be residual confounding. Although the plan of care survey has been used in several studies recently, it is not a formally validated survey tool. We made efforts to maximize reviewer inter-rater reliability, but bias may not have been completely eliminated. We made every effort to conduct physician, patient, and nurse interviews in temporal proximity to minimize bias due to evolving plans of care and consultant involvement on busy hospital medicine units. This type of bias could have falsely reduced concordance in certain cases in both IDR groups. We were unable to measure fidelity to the IDR process. However, there is no widely accepted way to study fidelity, and any tool chosen would have its own limitations. In addition, the study is limited by selection bias for patient interviews and recall bias for all interview participants.
CONCLUSION
Patient knowledge of plan of care as measured by physician, patient, and nurse agreement or concordance was limited in hospitalized patients. Including hospitalists in interdisciplinary rounds did not increase concordance. Concordance was associated with a nonmodifiable patient factor: age. It was also associated with important outcomes such as a decrease in LOS and readmission rates. These findings could have significant implications for patient education and information sharing in hospital medicine units. Future studies are needed to validate the role of a shared mental model of plan of care in hospital medicine, given the potential to improve outcomes.
Supplementary Material
Footnotes
Conflicts of Interest. All authors report no conflicts of interest.
SUPPLEMENTARY MATERIALS
Supplementary material to this article can be found online at doi: 10.1016/j.jcjq.2020.11.006.
Contributor Information
V. Surekha Bhamidipati, Department of Medicine, ChristianaCare, Newark, DE; InnovAge Pennsylvania LIFE, Philadelphia..
LeRoi S. Hicks, Department of Medicine, ChristianaCare; ChristianaCare Value Insti- tute..
Richard Caplan, ChristianaCare Value Institute..
Bailey Ingraham, ChristianaCare Value In- stitute..
Patty McGraw, Depart- ment of Medicine, ChristianaCare..
Edmondo J. Robinson, ChristianaCare; Moffitt Cancer Center, Tampa, Florida..
REFERENCES
- 1.Thomas EN, Edwards L, McArdle P. Knowledge is power. A quality improvement project to increase patient understanding of their hospital stay. BMJ Qual Improv Rep. 2017. March 1 6:u207103.w3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calkins DR, et al. Patient-physician communication at hospital discharge and patients’ understanding of the postdischarge treatment plan. Arch Intern Med. 1997. May 12;157:1026–1030. [PubMed] [Google Scholar]
- 3.Horwitz LI, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013. October 14;173:1715–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Straand J, Sandvik H. Stopping long-term drug therapy in general practice. How well do physicians and patients agree? Fam Pract. 2001;18:597–601. [DOI] [PubMed] [Google Scholar]
- 5.Hermoni D, et al. Doctor-patient concordance and patient initiative during episodes of low back pain. Br J Gen Pract. 2000;50:809–810. [PMC free article] [PubMed] [Google Scholar]
- 6.Liaw ST, Young D, Farish S. Improving patient-doctor concordance : an intervention study in general practice. Fam Pract. 1996;13:427–431. [DOI] [PubMed] [Google Scholar]
- 7.O’Leary KJ, et al. Hospitalized patients’ understanding of their plan of care. Mayo Clin Proc. 2010;85:47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rothberg MB, et al. The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Intern Med. 2012;27:185–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mueller SK, et al. Impact of regionalized care on concordance of plan and preventable adverse events on general medicine services. J Hosp Med. 2016;11:620–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Temple W, et al. Concordance in communication between surgeon and patient. Can J Surg. 1998;41:439–445. [PMC free article] [PubMed] [Google Scholar]
- 11.Medicine Institute of. Health Literacy: A Prescription to End Confusion, Washington, DC: National Academies Press, 2004. Accessed Dec 12, 2020. https://www.ncbi.nlm.nih.gov/books/NBK216032/. [PubMed] [Google Scholar]
- 12.Organisation for Economic Co-operation and Development. Health at a Glance 2019: OECD Indicators, 2019. Accessed Dec 12, 2020. https://read.oecd.org/10.1787/4dd50c09-en?format=pdf.
- 13.Maly RC, et al. Implementation of consultative geriatric recommendations: the role of patient-primary care physician concordance. J Am Geriatr Soc. 2002;50:1372–1380. [DOI] [PubMed] [Google Scholar]
- 14.Kerse N, et al. Physician-patient relationship and medication compliance: a primary care investigation. Ann Fam Med. 2004;2:455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Small M, et al. Physician-patient concordance in pharmacological management of patients with COPD. COPD. 2015;12:473–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhamidipati VS, et al. Structure and outcomes of interdisciplinary rounds in hospitalized medicine patients: a systematic review and suggested taxonomy. J Hosp Med. 2016;11:513–523. [DOI] [PubMed] [Google Scholar]
- 17.Morris NS, et al. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006. March 24;7:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agency for Healthcare Research and Quality Archive. Mortality Risk Adjustment Methodology for University Health System Consortium. Meurer SJ, editor, March 2009. Accessed Dec 12, 2020. http://archive.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/mortality/Meurer.html . [Google Scholar]
- 19.Barbieri JS, et al. The Mortality review committee: a novel and scalable approach to reducing inpatient mortality. Jt Comm J Qual Patient Saf. 2013;39:387–395. [DOI] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality Archive. Mortality Risk Adjustment Methodology for University Health System’s Clinical Data Base, 2008. Accessed Dec 12, 2020 https://archive.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/mortality/Meurer.pdf. [Google Scholar]
- 21.Kemp EC, et al. Patients prefer the method of ″tell back-collaborative inquiry″ to assess understanding of medical information. J Am Board Fam Med. 2008;21:24–30. [DOI] [PubMed] [Google Scholar]
- 22.Kripalani S, Weiss BD. Teaching about health literacy and clear communication. J Gen Intern Med. 2006;21:888–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hulka BS, et al. Communication, compliance, and concordance between physicians and patients with prescribed medications. Am J Public Health. 1976;66:847–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Starfield B, et al. The influence of patient-practitioner agreement on outcome of care. Am J Public Health. 1981;71:127–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anthony MK, Hudson-Barr D. A patient-centered model of care for hospital discharge. Clin Nurs Res. 2004;13:117–136. [DOI] [PubMed] [Google Scholar]
- 26.Graumlich JF, Novotny NL, Aldag JC. Brief scale measuring patient preparedness for hospital discharge to home: psychometric properties. J Hosp Med. 2008;3:446–454. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.