Abstract
Objectives
We aimed to evaluate the use of an eHealth platform and a self-management outpatient clinic in patients with RA in a real-world setting. The effects on health-care utilization and disease activity were studied.
Methods
Using hospital data of patients with RA between 2014 and 2019, the use of an eHealth platform and participation in a self-management outpatient clinic were studied. An interrupted time series analysis compared the period before and after the introduction of the eHealth platform. The change in trend (relative to the pre-interruption trend) for the number of outpatient clinic visits and the DAS for 28 joints (DAS28) were determined for several scenarios.
Results
After implementation of the platform in April 2017, the percentage of patients using it was stable at ∼37%. On average, the users of the platform were younger, more highly educated and had better health outcomes than the total RA population. After implementation of the platform, the mean number of quarterly outpatient clinic visits per patient decreased by 0.027 per quarter (95% CI: −0.045, −0.08, P = 0.007). This was accompanied by a significant decrease in DAS28 of 0.056 per quarter (95% CI: −0.086, −0025, P = 0.001). On average, this resulted in 0.955 fewer visits per patient per year and a reduction of 0.503 in the DAS28.
Conclusion
The implementation of remote patient monitoring has a positive effect on health-care utilization, while maintaining low disease activity. This should encourage the use of this type of telemedicine in the management of RA, especially while many routine outpatient clinic visits are cancelled owing to COVID-19.
Keywords: rheumatology, self-management, telemedicine, remote monitoring, eHealth, disease activity, health-care utilization
Key messages
Real-world implementation of remote monitoring can reduce the number of hospital visits, while maintaining disease control.
Mainly younger and more highly educated patients, with lower disease activity, participate in telemedicine.
The combination of self-management and telemedicine has the potential to replace labour-intensive outpatient clinic visits.
Introduction
The World Health Organization estimates that by 2030 there will be a shortage of 18 million health workers, owing to further increase in health-care utilization [1]. In Western countries, the increasing prevalence of chronic diseases is a growing burden to an already overextended health-care system [2]. For rheumatic services, the demand is exceeding supply, as reflected by long waiting lists in many countries [3]. The expectation is that this demand will continue to increase over the coming years [4]. Simultaneously, the workforce is declining because of an ageing population, while developments in labour productivity in health care are lagging [5, 6]. Therefore, structural changes are needed to deliver an increasing amount of care with the same capacity of people and resources [7]. According to the Dutch Health Authority, a more rapid introduction of digitalization in health care is needed [8]. Digitalization can help to optimize health care by improving the lagging productivity [6] Both the potential and importance of digitalization have become even clearer in recent months, because it was impossible to deliver care as usual owing to the arrival of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [9].
For instance, telemedicine (i.e. delivery of health-care services through the use of information and communication technologies in a situation where the actors are in different locations: remote monitoring [10]) can be used to replace, in part, outpatient visits and other labour-intensive care [7, 8]. The management of RA lends itself for the use of remote monitoring. RA is a chronic disease that often requires lifelong hospital visits. Owing to the routine character (every 3–6 months) of these hospital visits and the variable disease course of RA, patients are often doing well at the time of consultation, and little action is needed [11]. At the same time, routine outpatient visits are unable to support patients if they experience a flare of their disease in between visits [12]. By supporting self-management and providing education about the disease in general, patients will gain more insight into the individual course of their disease. This will help patients to manage their disease better, which, in turn, will improve their health outcome [13].
The first studies evaluating remote monitoring for the treatment of rheumatic diseases are promising, with high patient satisfaction and equal or higher effectiveness compared with the face-to-face approach [14, 15]. The use of patient-reported outcome measures (PROMs) to assess disease activity and patient-initiated visits makes it possible to achieve similar disease control with fewer outpatient clinic visits [16, 17]. However, research settings the patients participating in these remote monitoring programmes are often a selective group. This group consists of patients who are younger or less sick [15], often with a higher level of education [18]. This selection reflects that there is still a large group who feels reluctant to participate in remote monitoring programmes and telemedicine [19].
However, telemedicine is not merely a change in organization and coordination of care; it is a different way of thinking about care as a system, and the position of patients in it [20]. A prerequisite for telemedicine to be successful is that the patient becomes a partner in care [7].
Therefore, to support patients in their self-management behaviour and improve patient engagement, the eHealth platform Reumanet Bernhoven was introduced in April 2017 [21]. Reumanet Bernhoven is an eHealth platform that helps patients and health professionals to manage rheumatic disease. The aim of this platform is to increase the number of patients who feel adequately equipped to perform self-management and to improve patient engagement at a population level.
At the same time, research shows that successful disease monitoring by the patient helps to replace lifelong physician-initiated visits with patient-initiated visits [15]. This will reduce the number of routine visits of patients with stable disease, creating more time to review patients with an active disease in a timely manner. In order to teach patients the competencies required for successful self-management, the self-management outpatient clinic (SMOC) was started in March 2018 in Bernhoven. In the SMOC, patients are coached by a trained nurse specialist to use their own abilities to self-monitor their disease (facilitated through the eHealth platform). This aims to reduce the number of unnecessary hospital visits, while maintaining disease control.
This study has three aims: to evaluate the use of an eHealth platform and the different levels of participation; to study the influence of introducing an eHealth platform promoting self-management on disease activity and the number of hospital visits in the RA population; and to study the impact of remote monitoring on health-care utilization and the disease activity of patients with RA.
Methods
Design
This observational study evaluates the use of an eHealth platform and different levels of participation in the Department of Rheumatology at Bernhoven using a real-world design setting. It studies the effects of implementing an eHealth platform with regard to disease activity and health-care utilization using an interrupted time series design between July 2014 and October 2019. The study also analyses the patients participating in the SMOC and their disease activity and health-care utilization. Data on all patients with a clinical diagnosis of RA according to the 2010 ACR criteria were collected from the Reumanet Bernhoven registry and included in the analysis [22]. All patients had provided written informed consent for the use of their data for scientific purposes at an earlier time point. All procedures were performed in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. According to the medical ethical review committee of the region Arnhem-Nijmegen, this study does not require ethical approval, because only data used for daily clinical practice were collected (file number 2020-6729).
Reumanet Bernhoven
In April 2017, the eHealth platform Reumanet Bernhoven (Philips VitalHealth software, Ede, Netherlands) was launched [21]. The platform includes data on all patients diagnosed with RA under treatment at the Rheumatology Department in Bernhoven and is automatically available for the patient and the rheumatologist. With permission of the patient, other health professionals can also gain access (e.g. the nurse, general practitioner or physiotherapist). The platform provides the patient with disease-specific information in the form of a library, contains eHealth modules and provides insight into personal medical data, such as medication history and laboratory values. Patients can also monitor their disease activity by using PROMs. Reumanet Bernhoven also includes graphical overviews of disease activity and PROMs, lifestyle advice, and a chat function is available to send messages between the patient and health professional. To improve uptake of Reumanet Bernhoven, special attention was given to making the process as inclusive as possible. For example, educational classes on how to log in and use Reumanet Bernhoven were offered to support those who lacked skills, and reminders to fill out questionnaires were sent to patients at patient-specific time points.
Self-management outpatient clinic
The SMOC was initiated in March 2018. The aim of this outpatient clinic was to provide patients who were in remission or have low disease activity with the opportunity to self-manage their disease and thereby reduce the number of consultations at the Department of Rheumatology. Patients with a clinical diagnosis of RA, either in stable remission or with low disease activity, who were motivated to take part in the self-management programme and able to use Reumanet Bernhoven were invited to participate in the SMOC. After giving informed consent, the patient received information from a trained nurse specialist about the aim of the SMOC, how to use Reumanet Bernhoven, what to expect from the health professionals and how to contact the outpatient clinic in case they had questions. Patients participating in the SMOC were required to have one consultation with the rheumatologist per year and were asked to fill in the rheumatoid arthritis impact of disease (RAID) [23] to track their disease activity. Patients were obliged to undergo laboratory monitoring according to the guidelines of the drugs they were using. The samples could be taken at a location of the patient’s choice and were analysed at the laboratory of Bernhoven. The results of these tests were reviewed by the health-care professionals before sending a prescription for medication for the consecutive period. Patients were able to contact a nurse specialist if they felt the need to, for example, because of a self-monitored flare or an adverse event, and could obtain a consultation within a few days if the patient or nurse practitioner deemed this desirable.
Measures
Baseline characteristics were age, biological sex, educational status, work status, smoking status, alcohol use, disease duration, RF status, anti-CCP status, BMI and medication use. As a measure of health-care utilization, the number of RA-related outpatient clinic visits was used. The DAS28 was used by the rheumatologist as a measure for disease activity (score between 0 and 10, with a higher score indicating higher disease activity) [24]. The following PROMs were filled out: for functional capacity, the HAQ [25] was used (score between 0 and 3, with a higher score indicating worse function and greater disability); the 36-item short form health survey (SF-36) [26] was used to measure health-related quality of life (score between 0 and 100, with a higher score indicating a better health-related quality of life); and to assess the impact of RA from a patient perspective, the RAID was scored (score between 0 and 10, with a higher scores indicating worse impact of disease).
The following measurements and questionnaires could be entered by the patient: educational status, working status, smoking status, alcohol use, HAQ, SF36, RAID and visual analog scales for pain and tiredness.
Evaluation of self-management through use of the eHealth platform
To evaluate the utilization of the eHealth platform, we categorized the RA population based on the level of utilization. First, we divided the population into two groups: patients who had an email address and therefore had the possibility of logging into Reumanet Bernhoven (potential users) and those without the possibility of logging in (non-users). Second, we identified the subgroup of patients who had logged in (active users). Given that Reumanet Bernhoven offers the possibility of filling out yearly questionnaires, a 1-year cut-off was used to identify active users. Third, we identified those patients who regularly performed PROMs as part of follow-up within the SMOC.
Interrupted time series analyses
To study the effect of the introduction of Reumanet Bernhoven on health-care utilization and disease activity, a single-centre interrupted time series analysis was performed on the total population and on the subgroup of patients who eventually participated in the SMOC. The interruption in the time series (quarterly intervals) was placed in April 2017 (i.e. the introduction of the platform). The interrupted time series design attempted to assess whether the Reumanet Bernhoven intervention had a significant effect on health-care utilization and DAS28 compared with the underlying trend. The pre-intervention trend served as the control [27]. Autocorrelation in the error distribution was tested by the Cumby–Huizinga general test for autocorrelation. Depending on the outcome of this test, one or more lags were added to the model. Statistical analyses were done in STATA v.15.1 (TX: StataCorp LLC, College Station).
Results
Participation in Reumanet Bernhoven and the self-management outpatient clinic
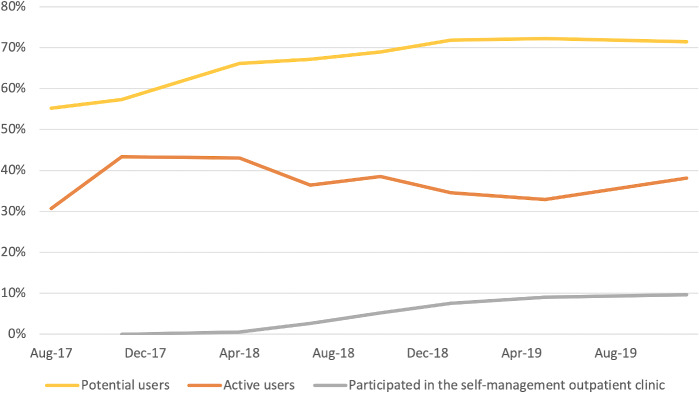
Since the initiation of the eHealth platform and the SMOC, the utilization of these programmes has increased gradually over time (Fig. 1). However, most of the uptake of Reumanet Bernhoven occurred in the quarter immediately after its introduction, and it was difficult to increase this number over time. By November 2019, 1145 patients with RA were treated at the Rheumatology Department of Bernhoven and therefore included in Reumanet Bernhoven. By then, 818 (71% of the RA population) had uploaded their email address and were able to log into Reumanet Bernhoven. Of those, 434 patients (38% of the RA population) had done so in the last year and were considered as active users of Reumanet Bernhoven. Of this group, 110 patients (10% of the RA population) were included in the SMOC (a flow diagram is provided as Supplementary Fig. S1, available at Rheumatology Advances in Practice online).
Fig. 1.
Utilization of Reumanet Bernhoven between August 2017 and November 2019
Patient characteristics of groups based on the usage of Reumanet Bernhoven
Table 1 shows the patient characteristics on 1 January 2019 of the total RA population (split into potential users and active users) and of the patients who participated in the SMOC between November 2017 and November 2019. It is noteworthy that the patients who used Reumanet Bernhoven and participated in the SMOC tended to be younger, more highly educated and have better health outcomes. Moreover, we observed that they seemed to use more medication, consume more alcohol and be more likely to have stopped smoking.
Table 1.
Patient characteristics on 1 January 2019 for the total RA population
| Patient characteristics | Total population | Potential users | Active users | Self-management clinic | ||||
|---|---|---|---|---|---|---|---|---|
| n = 1059 | n = 761 | n = 360 | n = 110 | |||||
| Age, years, mean (s.d.) | 64 (13) | 1059 | 61 (13) | 761 | 59 (11) | 360 | 57 (11) | 110 |
| Female, % | 67 | 705/1059 | 65 | 497/761 | 65 | 235/360 | 66 | 72/110 |
| BMI, kg/m2, mean (s.d.) | 27 (5.1) | 502 | 27 (5.1) | 370 | 27 (5.3) | 174 | 26 (4.8) | 65 |
| Anti-CCP positive, % | 56 | 418/761 | 53 | 300/566 | 56 | 138/248 | 64 | 59/92 |
| RF positive, % | 61 | 443/723 | 59 | 308/526 | 63 | 147/233 | 61 | 54/88 |
| Smoking status | ||||||||
| Current smoker, % | 19 | 61/322 | 18 | 33/186 | 13 | 20/151 | 5 | 3/55 |
| Stopped smoking, % | 46 | 149/322 | 51 | 95/186 | 54 | 82/151 | 62 | 34/55 |
| Never smoked, % | 35 | 112/322 | 31 | 58/186 | 33 | 49/151 | 33 | 18/55 |
| Consumes alcohol, % | 62 | 198/322 | 70 | 131/186 | 70 | 105/151 | 76 | 42/55 |
| Highest education | ||||||||
| High, % | 12 | 38/318 | 15 | 28/186 | 18 | 27/151 | 31 | 17/55 |
| Middle, % | 25 | 79/318 | 31 | 58/186 | 30 | 45/151 | 27 | 15/55 |
| Low, % | 63 | 201/318 | 54 | 100/186 | 52 | 79/151 | 42 | 23/55 |
| Health outcome | ||||||||
| DAS28, median (IQR) | 2.6 (2.0–3.4) | 863 | 2.6 (2.0–3.2) | 642 | 2.5 (1.9–3.1) | 339 | 2.1 (1.7–2.7) | 109 |
| HAQ, median (IQR) | 0.50 (0.12–1.3) | 272 | 0.38 (0–1.0) | 182 | 0.38 (0–0.94) | 169 | 0.32 (0–0.75) | 78 |
| SF36 PCS, median (IQR) | 43 (35–51) | 166 | 44 (37–52) | 133 | 44 (37–52) | 129 | 48 (40–53) | 63 |
| SF36 MCS, median (IQR) | 50 (42–58) | 166 | 50 (42–56) | 133 | 51 (42–56) | 129 | 54 (47–60) | 63 |
| Medication use | ||||||||
| Biologic users, % | 20 | 214 | 22 | 171 | 24 | 87 | 30 | 33 |
| csDMARD users, % | 75 | 797 | 75 | 569 | 77 | 277 | 85 | 94 |
| No DMARD therapy, % | 18 | 196 | 19 | 145 | 17 | 61 | 6 | 7 |
Patient characteristics are split into the potential users, the active users, and the patients who participated in the self-management outpatient clinic between November 2017 and November 2019.
csDMARD: conventional synthetic DMARD; DAS28: disease activity score for 28 joints; IQR: interquartile range; SF: short form; PCS: physical component score; MCS: mental component score.
Interrupted time series analyses of the introduction of Reumanet Bernhoven
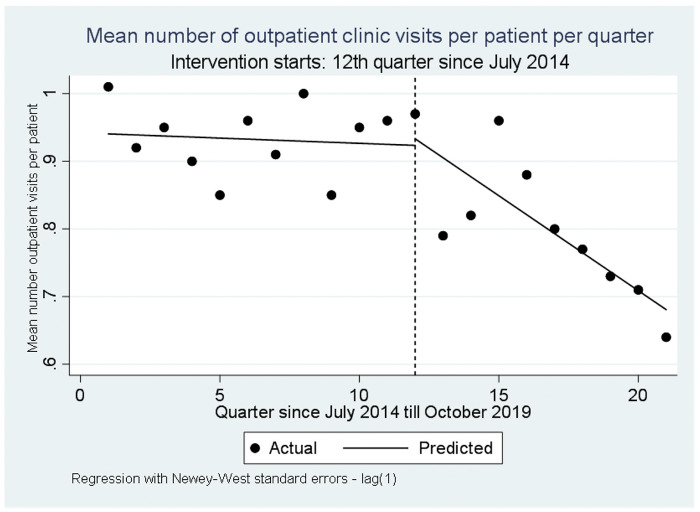
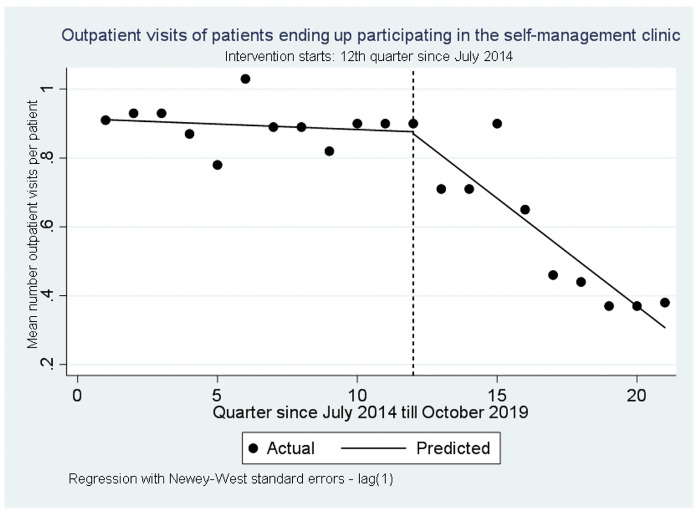
The mean number of outpatient clinic visits in the total RA population in July 2014 was estimated at 0.94 visits per patient per quarter (Fig. 2). Before the introduction of the eHealth platforms, there was a non-significant decreasing trend in the number of quarterly visits of −0.002 per quarter (95% CI: −0.123, 0.009, P = 0.766). After the introduction of the eHealth platform, the mean number of quarterly outpatient clinic visits decreased significantly each quarter by 0.027 (relative to the pre-interruption trend; 95% CI: −0.045, −0.08, P = 0.007). The decline in quarterly visits was even more prominent in the subgroup who eventually participated in the SMOC (Fig. 3). In July 2014, they had a comparable mean number of outpatient clinic visits of 0.91 per patient per quarter. Before the introduction of the eHealth platform, their mean number of outpatient clinics visits decreased non-significantly by 0.003 per quarter (95% CI: −0.009, 0.003, P = 0.297). After the introduction of the eHealth platform, the trend for the number of quarterly visits decreased significantly by 0.059 per quarter (relative to the pre-interruption trend; 95% CI: −0.078, −0.040, P < 0.001).
Fig. 2.
Outpatient clinic visits in the total RA population
The mean number of outpatient clinic visits per patient per quarter in the total RA population between July 2014 and October 2019.
Fig. 3.
Outpatient clinic visits of the patients who would end up participating in the self-management outpatient clinic
The mean number of outpatient clinic visits per patient per quarter of the patients who would end up participating in the self-management outpatient clinic between July 2014 and October 2019.
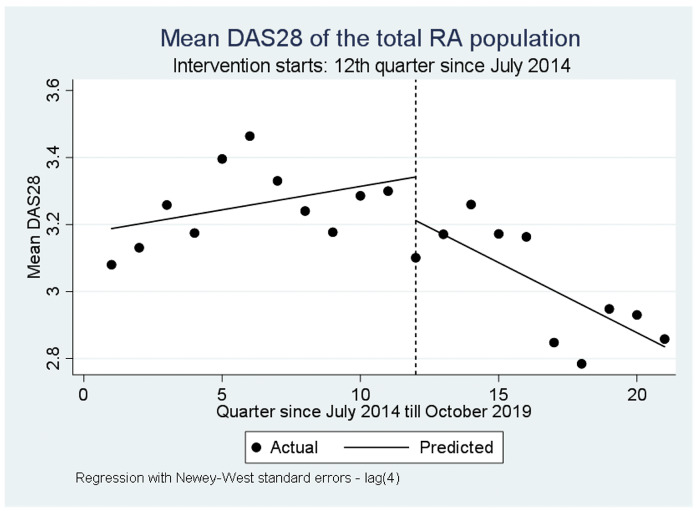
The mean DAS28 of the total RA population in July 2014 was estimated to be 3.19 (Fig. 4). Before the introduction of the eHealth platform, there was an non-significant increase in the DAS28 of 0.014 per quarter (95% CI: −0.006, 0.034, P = 0.164). After the introduction of the eHealth platform, the mean DAS28 decreased significantly (relative to the pre-interruption trend) by 0.056 per quarter (95% CI: −0.086, −0025, P = 0.001).
Fig. 4.
DAS28 of the total RA population
The mean DAS for 28 joints (DAS28) of the total RA population between July 2014 and October 2019.
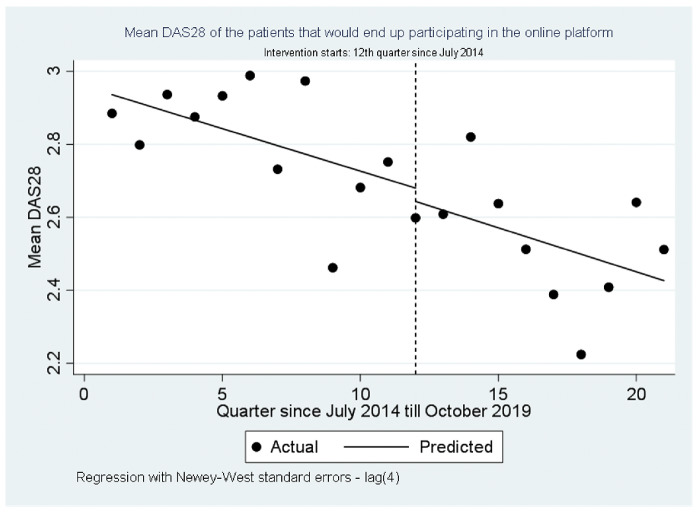
The mean DAS28 of the subgroup of patients who would end up participating in the SMOC was estimated to be 2.94 in July 2014 (Fig. 5). Their mean DAS28 decreased significantly by 0.023 per quarter (95% CI: −0.041, −0.005, P = 0.015) before the introduction of the eHealth platform. After the introduction of the eHealth platform, the quarterly post-interruption trend of the DAS28 (relative to the pre-interruption trend) stayed approximately the same (CI: −0.036, 0.047, P = 0.962).
Fig. 5.
DAS28 of the patients who would end up participating in the self-management outpatient clinic
The mean DAS for 28 joints (DAS28) of the patients who would end up participating in the self-management outpatient clinic between July 2014 and October 2019.
Discussion
After the implementation of Reumanet Bernhoven, there was a significant decrease in the number of outpatient clinic visits over time, without compromising disease control. Participation in the SMOC reduced the health-care utilization even more, without affecting the pre-existing decreasing trend in DAS28 present in this group. During this period, both the percentage of potential Reumanet Bernhoven users and the percentage of patients participating in the SMOC increased, whereas the percentage of patients regularly using Reumanet Bernhoven did not increase after the initial uptake. On average, the users of Reumanet Bernhoven were younger, more highly educated and had better health outcomes. This difference was even more evident in those who participated in the SMOC.
Our real-world data match positive results from clinical trials investigating self-management supported by eHealth applications and patient-initiated visits for the treatment of rheumatic diseases [14–18]. We found a decrease in health-care utilization after the implementation of telemedicine. This was accompanied by a clinically non-significant improvement in health outcome, showing at least non-inferiority compared with care as usual. This adds to the growing body of evidence concluding that telemedicine methods can be implemented safely in RA. These findings are also relevant in the treatment of other rheumatic diseases and even other chronic diseases. Owing to SARS-CoV-2, many routine outpatient clinic visits have been cancelled, and the expectation is that it might take years before things get back to normal. Therefore, eHealth applications can be used to support patients in their increased need for self-management, whereas patient-initiated visits can help to select those patients who need to be seen at the outpatient clinic.
The inclusiveness of telemedicine remains an important issue. The goal of Reumanet Bernhoven was to improve patient engagement and to increase the number of patients who feel adequately equipped to perform self-management. To achieve this, particular attention was given to making the process as inclusive as possible during the implementation of Reumanet Bernhoven. These efforts led to an increase in the percentage of patients who were able to log into the eHealth platform (from 55 to 71% of the population). However, most of the active users engaged early on, and the percentage who used the eHealth platform remained stable at ∼37%. This illustrates that more efforts are needed in order to motivate more patients to participate in this self-management programme. This low percentage corresponds to other real-world data, where only 34% of the patients engaged in self-management [13]. At the same time, our data show that it is a select group that participates in telemedicine, i.e. the younger, more highly educated patients with low disease activity. This matches findings from systematic reviews assessing the participants of patient-initiated follow-up and eHealth programmes for the treatment of chronic diseases [15, 28]. This selective use of telemedicine, whereby eHealth is least used by the people who need it most, risks widening the gap between those at risk of social health inequalities and the rest of the population [28, 29]. The effects of selective use of telemedicine on inequality and access to care should therefore be monitored.
Different factors influence whether a patient will participate in self-management. For instance, patients with chronic rheumatic diseases perceive different levels of self-management as suitable for themselves and therefore do not always see themselves as partners in care [30]. Lack of information and lack of self-monitoring skills are perceived as barriers to perform self-management [30]. The high number of people with low health literacy and low health skills (29% of the Dutch population) further complicates self-management [31–33]. Therefore, further implementation of telemedicine requires good guidance, offering a tailor-made approach and focusing on those at risk of social health inequalities [29]. Concurrently, we think that it is important to acknowledge that, at least at the moment, not all patients are capable of performing self-management and telemedicine. Adequate selection of which level of self-management can be expected of an individual patient is essential. In our opinion, this task is best performed by a nurse specialist affiliated with the SMOC. They often have more time and skills to explore patients’ conditions and needs. In addition, patients often experience a special relationship of trust with their nurse specialist that allows for a tailor-made approach aimed at tackling the aforementioned barriers [25]. Using this relationship of the nurse with the patient can help to increase the participation in self-management and telemedicine.
Interestingly, we have noticed in recent months an increase in patients who have actively enquired regarding the possibilities of performing telemedicine. This increase has coincided with the SARS-CoV-2 pandemic in The Netherlands. Owing to SARS-CoV-2, there has been an increase in Internet use by the elderly, the group currently under-represented in Reumanet Bernhoven users [34]. Simultaneously, the outpatient clinic had to close down somewhat, reducing the possibility for outpatient clinic visits. The fact that Reumanet Bernhoven was still readily available might have helped people to overcome the barriers normally perceived. This change in patients participating in telemedicine should be monitored closely, because changes in the composition of the participating population could influence the effectiveness of telemedicine. Before telemedicine can be applied for the whole population, we should know the effectiveness of telemedicine in the groups currently unlikely to participate.
This study evaluated the use of Reumanet Bernhoven and participation in the SMOC in a real-world setting. A strength of this study is that it offered the opportunity to assess which patients chose to use these programmes in daily clinical practice. Participants in the programme were clearly a self-selected group, which is currently the daily reality [15, 28]. As previously mentioned, efforts will have to focus on increasing the number of participants of the programme. A limitation of observational data is the difficulty in assessing the causality of interventions. Given that the study period was lengthy, external factors, such as advances in treatment options or changes in treatment guidelines, could potentially influence disease activity and, to a lesser extent, the number of hospital visits. An interrupted time series design is capable of identifying these underlying trends and isolates the effect of the introduction of Reumanet Bernhoven [35]. By using the pre-interruption trend as a control, the observed differences are more likely to be attributable to the studied interventions. This strengthens the confidence that the observed effect can be attributed to the introduction of Reumanet Bernhoven, especially because, as far as we know, during that time period no changes in other factors that could explain the underlying trend for health-care utilization occurred.
In conclusion, the implementation of Reumanet Bernhoven, an eHealth platform aimed at supporting patients in their self-management need, resulted in less health-care utilization, while maintaining disease control. Making use of patient-initiated visits in patients with stable disease activity resulted in an even larger reduction of health-care utilization. Policy-makers should use the momentum telemedicine has gained recently owing to the SARS-CoV-2 pandemic to embed telemedicine firmly into the health-care system, in particular, with the expected cutbacks in mind, required owing to the pandemic. Concomitantly, health-care professionals need to remain vigilant to ensure that those currently unable to participate in telemedicine receive the care they need.
Supplementary Material
Acknowledgements
W.D.M., S.A.A.R.D., C.V., A.H., E.M.M.A. and P.L.C.M.R. were involved in the conception and design of the study. W.D.M., C.V. and S.A.A.R.D. acquired the data. W.D.M., S.A.A.R.D., C.V., A.H., E.M.M.A. and P.L.C.M.R. analysed and interpreted the data. W.D.M. drafted the article. W.D.M., S.A.A.R.D., C.V., A.H., E.M.M.A. and P.L.C.M.R. revised the article critically for important intellectual content. W.D.M., S.A.A.R.D., C.V., A.H., E.M.M.A. and P.L.C.M.R. gave final approval of the version to be published. All authors had access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. W.D.M. attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. He is the guarantor.
Funding: This study was supported by a grant from Stichting RUN. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by Stichting RUN is intended or should be inferred.
Disclosure statement: The authors have declared no conflicts of interest.
Data availability statement
De-identified participant data are available upon reasonable request.
Supplementary data
Supplementary data are available at Rheumatology Advances in Practice online.
References
- 1. World Health Organization. Working for health and growth: investing in the health workforce. Report of the High-Level Commission on Health Employment and Economic Growth. WHO PRESS 2016. Available online at: https://apps.who.int/iris/bitstream/handle/10665/250047/9789241511308-eng.pdf;jsessionid=A9FC5F1E8A2C649EE815314BD7A9714B?sequence=1.
- 2. World bank, World Health Organization. Half the world lacks access to essential health services, 100 million still pushed into extreme poverty because of health expenses. WHO Press 2017. Available online at: https://www.who.int/news/item/13-12-2017-world-bank-and-who-half-the-world-lacks-access-to-essential-health-services-100-million-still-pushed-into-extreme-poverty-because-of-health-expenses#:~:text=of%20health%20expenses-,World%20Bank%20and%20WHO%3A%20Half%20the%20world%20lacks%20access%20to,poverty%20because%20of%20health%20expenses&text=Currently%2C%20800%20million%20people%20spend,child%20or%20other%20family%20member.
- 3. Delaurier A, Bernatsky S, Baron M, Légaré J, Feldman DE.. Wait times for rheumatology consultation: is rheumatoid arthritis prioritized? J Clin Rheumatol 2012;18:341–4. [DOI] [PubMed] [Google Scholar]
- 4. Dejaco C, Lackner A, Buttgereit F. et al. Rheumatology workforce planning in western countries: a systematic literature review. Arthritis Care Res 2016;68:1874–82. [DOI] [PubMed] [Google Scholar]
- 5. Ursum J, Rijken M, Heijmans M, Cardol M, Schellevis F. Zorg voor chronisch zieken, Organisatie van zorg, zelfmanagement, zelfredzaamheid en participatie. Nivel 2011. Available online at: https://www.nivel.nl/sites/default/files/bestanden/Rapport-zorg-voor-chronisch-zieken.pdf. [Google Scholar]
- 6. Adang E, Jeurissen P. kritische-houding-ten-aanzien-van-innovaties-in-de-zorg-noodzakelijk. ESB 105(4785). 2020. Available online at: https://esb.nu/esb/20059805/kritische-houding-ten-aanzien-van-innovaties-in-de-zorg-noodzakelijk
- 7. Nederlandse Vereniging van Ziekenhuizen. Zorg voor 2020. 2016 Nederlandse Vereniging van Ziekenhuizen. Available online at https://www.talmor.nl/wp-content/uploads/2016/04/1A10-12-Strategiedocument-Zorg-voor-2020.pdf.
- 8. van Lonkhuyzen L. Toezichthouder NZa: de zorg is te veel een verdienmodel geworden. Amsterdam, Nrc, 2020. [Google Scholar]
- 9. Rijksoverheid.nl. Het coronavirus en digitale zorg Rijksoverheid.nl. 2020. https://www.rijksoverheid.nl/onderwerpen/coronavirus-covid-19/zorg/digitale-zorg
- 10.World Health Organization.Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2). 2010. World Health Organization. ISBN: 978-92-4-156414-4. Available online PDF at: http://www.who.int/goe/publications/goe_telemedicine_2010.pdf
- 11. Hendrikx J, Fransen J, van Riel PL.. Monitoring rheumatoid arthritis using an algorithm based on patient-reported outcome measures: a first step towards personalised healthcare. RMD Open 2015;1:e000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Houtum L, Rijken M, Heijmans M, Groenewegen P.. Patient-perceived self-management tasks and support needs of people with chronic illness: generic or disease specific? Ann Behav Med 2015;49:221–9. [DOI] [PubMed] [Google Scholar]
- 13. Volpp K, Mohta N.. Patient engagement survey: improved engagement leads to better outcomes, but better tools are needed. NEJM Catalyst 2016; 2.3. [Google Scholar]
- 14. Piga M, Cangemi I, Mathieu A, Cauli A.. Telemedicine for patients with rheumatic diseases: systematic review and proposal for research agenda. Semin Arthritis Rheum 2017;47:121–8. [DOI] [PubMed] [Google Scholar]
- 15. Taneja A, Su'a B, Hill AG.. Efficacy of patient-initiated follow-up clinics in secondary care: a systematic review. Intern Med J 2014;44:1156–60. [DOI] [PubMed] [Google Scholar]
- 16. de Thurah A, Stengaard-Pedersen K, Axelsen M. et al. Tele-health followup strategy for tight control of disease activity in rheumatoid arthritis: results of a randomized controlled trial. Arthritis Care Res 2018;70:353–60. [DOI] [PubMed] [Google Scholar]
- 17. Hewlett S, Kirwan J, Pollock J. et al. Patient initiated outpatient follow up in rheumatoid arthritis: six year randomised controlled trial. BMJ 2005;330:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Myasoedova E, Crowson CS, Giblon RE. et al. Optimization of flare management in patients with rheumatoid arthritis: results of a randomized controlled trial. Clin Rheumatol 2019;38:3025–32. [DOI] [PubMed] [Google Scholar]
- 19. Knudsen LR, de Thurah A, Lomborg K.. Experiences with telehealth followup in patients with rheumatoid arthritis: a qualitative interview study. Arthritis Care Res 2018;70:1366–72. [DOI] [PubMed] [Google Scholar]
- 20. Eysenbach G. What is e-health? J Med Internet Res 2001;3:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. van Riel P, Zuidema RM, Vogel C, Rongen-van Dartel SAA.. Patient self-management and tracking: a European experience. Rheum Dis Clin North Am 2019;45:187–95. [DOI] [PubMed] [Google Scholar]
- 22. Aletaha D, Neogi T, Silman AJ. et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 2010;62:2569–81. [DOI] [PubMed] [Google Scholar]
- 23. Gossec L, Paternotte S, Aanerud GJ. et al. Finalisation and validation of the rheumatoid arthritis impact of disease score, a patient-derived composite measure of impact of rheumatoid arthritis: a EULAR initiative. Ann Rheum Dis 2011;70:935–42. [DOI] [PubMed] [Google Scholar]
- 24. Prevoo ML, van 't Hof MA, Kuper HH. et al. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 1995;38:44–8. [DOI] [PubMed] [Google Scholar]
- 25. Fries JF, Spitz PW, Young DY.. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol 1982;9:789–93. [PubMed] [Google Scholar]
- 26. Ware JE Jr, Sherbourne CD.. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 27. Linden A, Adams JL.. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract 2011;17:1231–8. [DOI] [PubMed] [Google Scholar]
- 28. Reiners F, Sturm J, Bouw LJW, Wouters EJM.. Sociodemographic factors influencing the use of ehealth in people with chronic diseases. Int J Environ Res Public Health 2019;16:645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Latulippe K, Hamel C, Giroux D.. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res 2017;19:e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zuidema RM, Repping-Wuts H, Evers AW, Van Gaal BG, Van Achterberg T.. What do we know about rheumatoid arthritis patients' support needs for self-management? A scoping review. Int J Nurs Stud 2015;52:1617–24. [DOI] [PubMed] [Google Scholar]
- 31. Rijksinstituut voor Volksgezondheid en Milieu. Niet iedereen kan regie voeren over eigen zorg. 2014. https://www.rivm.nl/nieuws/niet-iedereen-kan-regie-voeren-over-eigen-zorg
- 32. Buchbinder R, Hall S, Youd JM.. Functional health literacy of patients with rheumatoid arthritis attending a community-based rheumatology practice. J Rheumatol 2006;33:879. [PubMed] [Google Scholar]
- 33. Quinlan P, Price KO, Magid SK. et al. The relationship among health literacy, health knowledge, and adherence to treatment in patients with rheumatoid arthritis. HSS J 2013;9:42–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. RTLnieuws. Grote toename internetgebruik ouderen door coronacrisis. 2020. https://www.rtlnieuws.nl/tech/artikel/5141811/internet-gebruik-ouderen-bejaarden-videobellen
- 35. Penfold RB, Zhang F.. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 2013;13:S38–44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
De-identified participant data are available upon reasonable request.