Dear Editor, Several studies have so far reported the adverse impact of coronavirus disease 2019 (COVID-19) on mental health in the general public [1, 2]. Patients with RA have a greater risk of infection due to immune dysregulation, immunosuppressive therapy and older age on average [3]. Consequently they are likely to be more concerned about COVID-19 than the general public. Our study aimed to explore the prevalence of anxiety and depression among patients with RA before and during the pandemic.
This study was based on the Kyoto University RA Management Alliance (KURAMA) cohort [4], which enrolled outpatients with RA from 1 May 2019 to 31 August 2020. This study was approved by the ethics committee of Kyoto University (approval number R0357). Anxiety and depression were measured using the Japanese version of the Hospital Anxiety and Depression Scale (HADS). The scale contains two seven-item subscales for anxiety and depression. For each scale, a cut-off score of 8–10 points indicates doubtful, whereas >11 points indicates a definite presence of these psychological conditions. We described the prevalence of anxiety and depression among patients before and during the pandemic. Also, a multivariable linear regression model was used to assess the association between the baseline characteristics and psychological scores during the pandemic. We used the following explanatory variables measured in 2019: age, sex, disease duration, 28-joint Disease Activity Score (DAS28), the HAQ, rheumatic drug use (biologic agents, MTX, glucocorticoids) and the baseline HADS score.
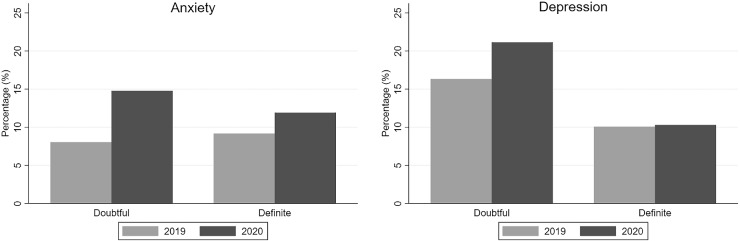
During the study period, 108 patients with RA completed the HADS measurements. The patients’ mean age was 65.7 years (s.d. 10.6) and 94 patients (87%) were female. The mean disease duration was 15.0 years (s.d. 10.6) and the mean DAS28 and HAQ were 2.87 (s.d. 1.18) and 0.55 (s.d. 0.67). A total of 57 patients (53%) were using biologic agents, 71 patients (66%) were using MTX and 27 patients (25%) were using glucocorticoids. Nearly 9% of patients with RA reported definite anxiety before the pandemic and the percentage increased to 12% in 2020 (Fig. 1). Additionally, 8% of patients reported doubtful anxiety in 2019 and the percentage increased to 15% in 2020. In contrast, the patients reporting definite depression remained at 10% during the study period; however, more patients reported doubtful depression in 2020 (Fig. 1). Anxiety during the pandemic was associated with the HAQ [β = 0.21 (95% CI 0.04, 0.38), P = 0.014], biologic drug use [β = 0.20 (95% CI 0.03, 0.40), P = 0.047] and the previous anxiety point [β = 0.88 (95% CI 0.53, 1.23), P < 0.001]. The depression point in 2020 was associated with the previous depression point [β = 0.51 (95% CI 0.21, 0.81), P < 0.001].
Fig. 1.
Prevalence of anxiety and depression in patients with RA before and during the COVID-19 pandemic
The anxiety level in patients with RA was higher than pre-pandemic levels; patients using biologic agents or with a higher physical disability score in the previous year had higher HADS anxiety scores during the pandemic. Depression levels did not change from before to during the pandemic in several patients with RA. However, the number of patients reporting suspected depression increased significantly after the COVID-19 pandemic began. Since patients with RA have a higher risk of infection than the healthy population, they are more likely to experience anxiety symptoms. Additionally, psychological pressure might further increase due to the perplexing nature of information on the benefits and harms of rheumatic drugs against the COVID-19. Consequently, patients with high disease activity can become highly prone to psychological distress and should be offered focussed care. As the pandemic continues, more patients are likely to experience anxiety and depression and healthcare professionals must remain vigilant for these psychological changes.
Rheumatology key message
• Healthcare professionals must be watchful for mental health changes in patients with RA during COVID-19.
Funding: The KURAMA cohort study is supported by a grant from Daiichi Sankyo. Daiichi Sankyo had no role in the design of the study, the collection or analysis of data, writing of the manuscript or the decision to submit the manuscript for publication. This work was also supported by the Japan Society for the Promotion of Science KAKENHI programme (grant JP19K11165).
Disclosure statement: The Department of Advanced Medicine for Rheumatic Diseases is supported by Nagahama City, Shiga, Japan, Toyooka City, Hyogo, Japan and five pharmaceutical companies (Mitsubishi Tanabe Pharma, Chugai Pharmaceutical, UCB Japan, AYUMI Pharmaceutical and Asahi Kasei Pharma). M.H. received a research grant and/or speaker fees from Bristol-Myers Squibb, Eisai, Eli Lilly and Mitsubishi Tanabe Pharma. R.W. has received speaker fees from Mitsubishi Tanabe Pharma, Pfizer, Sanofi, AbbVie, Asahi Kasei, Eisai, Eli Lilly, Bristol-Myers Squibb and Janssen. M.Tanaka received research grants and/or speaker fees from AbbVie, Asahi Kasei Pharma, Astellas Pharma, Ayumi Pharmaceutical, Bristol-Myers Squibb, Chugai Pharmaceutical, Eisai, Eli Lilly Japan, Pfizer, UCB Japan, Janssen Pharmaceutical, Mitsubishi Tanabe Pharma, Novartis Pharma and Taisho Pharma. H.I. received research grants and/or speaker fees from Bristol-Myers Squibb, Kyocera, Asahi-Kasei, Eisai, Mochida and Toyama. A.M. has received speaking fees and/or research grants from Eli Lilly Japan, Ono Pharmaceutical, Pfizer, UCB Japan, AbbVie, Asahi Kasei Pharma and Chugai Pharmaceutical. The remaining authors have declared no conflicts of interest.
References
- 1. Ettman CK, Abdalla SM, Cohen GH. et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Daly M, Sutin AR, Robinson E. Depression reported by US adults in 2017–2018 and March and April 2020. J Affect Disord 2021;278:131–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology (Oxford) 2013;52:53–61. [DOI] [PubMed] [Google Scholar]
- 4. Nakagami Y, Sugihara G, Takei N. et al. Effect of physical state on pain mediated through emotional health in rheumatoid arthritis. Arthritis Care Res (Hoboken) 2019;71:1216–23. [DOI] [PubMed] [Google Scholar]