Abstract
Objective: Current meta-analysis aims to understand the effect of oral supplementation of vitamin D on intensive care unit (ICU) requirement and mortality in hospitalized COVID-19 patients.
Methods: Databases PubMed, preprint servers, and google scholar were searched from December 2019 to December 2020. Authors searched for the articles assessing role of vitamin D supplementation on COVID-19. Cochrane RevMan tool was used for quantitative assessment of the data, where heterogeneity was assessed using I2 and Q statistics and data was expressed using odds ratio with 95% confidence interval.
Results: Final meta-analysis involved pooled data of 532 hospitalized patients (189 on vitamin D supplementation and 343 on usual care/placebo) of COVID-19 from three studies (Two randomized controlled trials, one retrospective case-control study). Statistically (p<0.0001) lower ICU requirement was observed in patients with vitamin D supplementation as compared to patients without supplementations (odds ratio: 0.36; 95% CI: 0.210-0.626). However, it suffered from significant heterogeneity, which reduced after sensitivity analysis. In case of mortality, vitamin D supplements has comparable findings with placebo treatment/usual care (odds ratio: 0.93; 95% CI: 0.413-2.113; p=0.87). The studies did not show any publication bias and had fair quality score. Subgroup analysis could not be performed due to limited number of studies and hence dose and duration dependent effect of vitamin D could not be evaluated.
Conclusions: Although the current meta-analysis findings indicate potential role of vitamin D in improving COVID-19 severity in hospitalized patients, more robust data from randomized controlled trials are needed to substantiate its effects on mortality.
Introduction
Evidence suggest that 25-hydroxy vitamin D—a major circulatory metabolite of vitamin D—stimulates production of protective peptide in response to any viral or bacterial infection.1 In case of vitamin D deficiency, this mechanism is hampered and makes host susceptible to the variety of infection including respiratory tract infections. Effect of vitamin D supplementation on acute respiratory tract infection has been established by many randomized controlled trials.2,3 It was observed that irrespective of age, sex and study duration, vitamin D supplementation reduces risk of acute respiratory tract infection in all the patients.4,5 The benefits were also found to be dose-dependent and profound in individuals with deficiency of vitamin D at baseline.5,6
Novel coronavirus—COVID-19—is a respiratory disease that causes inflammation and irritation in upper and lower respiratory tract. In severe cases, it travels through alveoli and as a response there is respiratory inflammation that can be visualized on chest X-ray or CT image as ‘ground-glass opacity’.7 These characteristics share similarities with previously reported respiratory infections and hence remedies showing promising effect in management of them were also explored for potential use during COVID-19 infections. Initially, it was observed that the COVID-19 patients with vitamin D deficiency had poorer outcomes with longer stay in the intensive care unit (ICU) and are at higher mortality rates than their counterparts.8 Numerous attempts in the form of systematic reviews and meta-analysis assess the potential role of vitamin D deficiency in COVID-19 infection, severity and mortality.9–11 However majority of the reviews remained inconclusive and highlighted the need for more primary studies in the form of randomized controlled trials.9–11 Similarly, unlike other respiratory tract diseases, evidence showing effect of supplementation of oral vitamin D on improving the outcome of COVID-19 is still limited to few trials with smaller sample size. Current meta-analysis aimed to synthesize cumulative evidences from the studies reporting the effect of vitamin D supplementation on ICU stay and mortality outcomes in patients suffering from COVID-19 infections.
Materials and methods
In accordance with the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA), current systematic review and meta-analysis were conducted.11 ‘Cochrane Handbook for Systematic Reviews of Interventions’ was followed for planning and conducting the review.12,13
Search strategies and data extraction
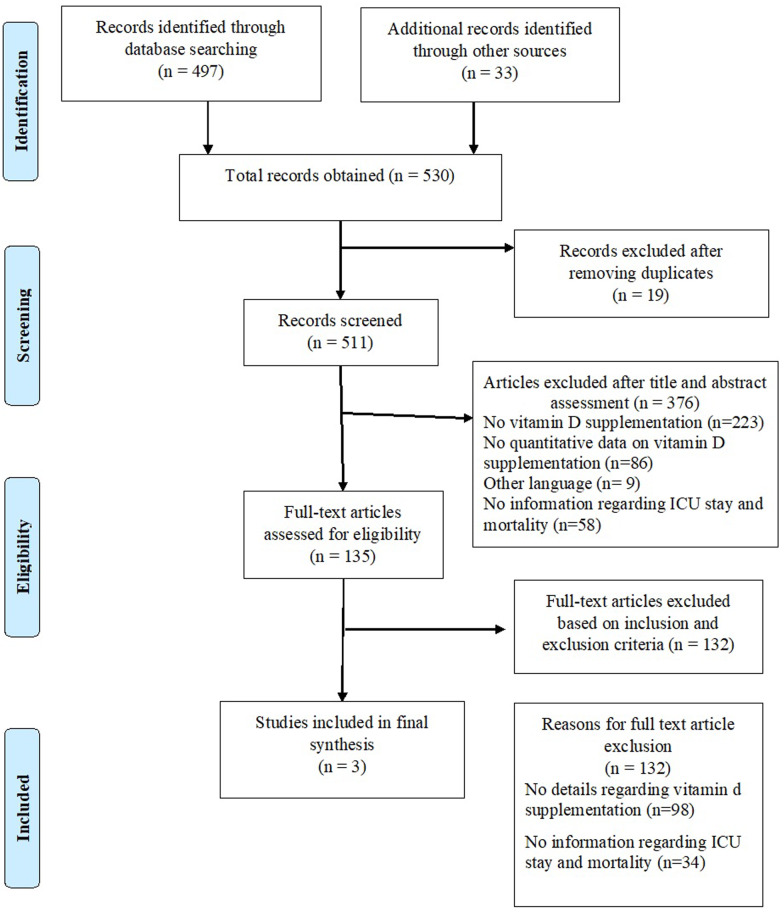
For retrieving eligible articles reporting effect of vitamin D supplementation on COVID-19 outcome, MEDLINE (through PubMed and CENTRAL using MeSH Terms), Google Scholar, and Preprint servers were searched. Search terms related to vitamin D supplementation and COVID-19 were designed to obtain relevant articles from the databases. The articles published between December 2019 and 17 December 2020 were independently screened by two reviewers. Initially articles were screened using title and abstract; after this, eligible articles were evaluated separately by two reviewers using full text. We aimed to include any study that assessed effect of vitamin D supplementation (irrespective of dose and form) on ICU admission and mortality in laboratory-confirmed COVID cases. Discordance between the authors was settled by discussion, and any difference of opinion that arose was resolved through mutual consensus. Articles published in English language were included in the study. Other language articles were also included if English summary was available. Included articles were also looked for additional studies through reference list searching, and any eligible article found was included in the review. Relevant details from each screened article were extracted in an electronic data collection matrix by two reviewers independently. After final selection, three articles were found eligible for the review; of them, two were randomized controlled trials and one was retrospective study. The detailed PRISMA chart regarding search is presented as Figure 1.
Figure 1.
PRISMA.
Risk of bias assessment
The randomized controlled trials were assessed for risk of bias using Cochrane tool,12 and quality of each trial was studied by all two reviewers and any discrepancy was addressed through re-evaluation and consensus among the authors. Quality score was generated using various criteria—randomization, double-blinding and dropouts on five methodological domains—random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential threats to validity. Based on the score generated on different aspects, the studies were categorized into low risk, moderate risk and high risk categories. For the observational study “Risk of Bias Assessment tool for Nonrandomized Studies (RoBANS)”14 for the controlled observational studies, as recommended by the Cochrane Handbook for Systematic Reviews of Interventions was used. The study was assessed based on six factors: (i) the selection of participants, (ii) confounding variables, (iii) measurements of exposure, (iv) blinding of outcome assessments, (v) incomplete outcome data and (vi) selective outcome reporting. Based on the factors, the study was categorized into either high, unclear or low risk of bias category.
Statistical analysis
Statistical analysis was performed using Review Manager (RevMan) Version 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). The software was used for pooling the data and deriving cumulative effect of the intervention on outcome of interest. The results were specifically assessed for presence of heterogeneity using Q statistics (significant at P < 0.10). I2—a quantitative measure of heterogeneity—was used to categorize studies into various levels of heterogeneity (high: 75–100%, medium: 50–70% and low: 0–50%). In case of I2 more than 50% two-tailed values of random-effect model were considered to measure the impact of an intervention, whereas fixed effect model was applied for the cases having I2 <50%. Cumulative results showing improvement in ICU need and mortality rates with vitamin D supplementation are presented using forest plots. Publication bias was assessed using both quantitative and qualitative methods. The presence or absence of statically significant bias was concluded from the quantitative results of Egger’s and Begg and Mazumdar rank correlation test, whereas visual inspection of bias was undertaken using Funnel plot. Forest plot was used to display the relative treatment effect and its 95% CI for each study.
Results
The final systematic review and meta-analysis included three studies,15–17 two randomized controlled trials and one retrospective case–control study. The detailed characteristics of the study are presented in Table 1. The review included details from 532 hospitalized COVID-19 positive patients. Though all the studies used oral supplementation of vitamin D, the duration and dosage of treatment varied. The details are provided in Table 1. The methodological quality of included studies was reasonably fair, as all three studies had a low risk of bias.
Table 1.
Characteristics of the studies included in the meta-analysis
| Sr No | Author | Country | Study type | Intervention (N) | Control (N) | Intervention | Control | Intervention details and duration | Outcome | ICU admission in intervention arm (%) | ICU admission in control arm (%) | Mortality in intervention arm (%) | Mortality in control | Mortality in control arm (%) | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Castillo et al.,15 2020 | Spain | Parallel pilot randomized open label, double-masked clinical trial | 50 | 26 | Oral calcifediol | Usual care | Oral capsule (0.532 mg) at the day of admission; 0.266 mg on Days 3 and 6; then weekly until discharge or ICU stay | ICU admission; death | 2 | 50 | 0 | 2 | 7.7 | Low |
| 2 | Murai et al.,16 2020 | Brazil | Multicenter, double-blind, randomized, placebo-controlled trial | 120 | 120 | Oral vitamin D | Placebo | Single 11 oral dose of 200 000 IU of vitamin D3 | Hospital length of stay, death, admission to ICU, mechanical ventilation requirement, serum level of vitamin D and biomarkers | 15.83 | 20.83 | 6.67 | 6 | 5 | Low |
| 3 | Hernández et al.,17 2020 | Spain | Retrospective case–control study | 19 | 197 | Oral vitamin D | Usual care | 3 Months (dose details are not available) | Admission to the intensive care unit, requirements for mechanical ventilation, or mortality | 5.263 | 25.38 | 10.53 | 20 | 10.15 | Low |
The cumulative effect of vitamin D supplementation on ICU admission and mortality in hospitalized patients of COVID-19 were assessed using meta-analysis. It was observed that there is a statistically significant (P < 0.0001) difference between ICU admission rate in patients with vitamin D supplements as compared to patients without the supplementations (odds ratio: 0.36; 95% CI: 0.210–0.626; Table 2; Figure 2). Though all three studies favored the intervention arm, the degree of impact varied among the studies and that resulted in heterogeneity as indicated by higher I2 (82.94%) and deviation from funnel shape (Figure 4). Removal of one study, Murai et al., has reduced the heterogeneity and indicated significant reduction in the overall ICU needs with vitamin D supplementation. However, the studies were free from any significant publication bias as assessed by Egger’s and Begg’s tests (Table 3).
Table 2.
Meta-analysis summary for vitamin D supplementation and ICU requirement
| Study | Intervention | Controls | Odds ratio | 95% CI | z | P | Weight (%) |
|
|---|---|---|---|---|---|---|---|---|
| Fixed | Random | |||||||
| Castillo et al.,15 2020 | 1/50 | 13/26 | 0.0204 | 0.00244–0.171 | 8.02 | 29.86 | ||
| Murai et al.,16 2020 | 19/120 | 25/120 | 0.715 | 0.370–1.382 | 83.28 | 39.64 | ||
| Hernández et al.,17 2020 | 1/19 | 50/197 | 0.163 | 0.0213–1.255 | 8.70 | 30.51 | ||
| Total (fixed effects) | 21/189 | 88/343 | 0.363 | 0.210–0.626 | −3.645 | <0.001 | 100.00 | 100.00 |
| Total (random effects) | 21/189 | 88/343 | 0.158 | 0.0171–1.452 | −1.631 | 0.103 | 100.00 | 100.00 |
Figure 2.
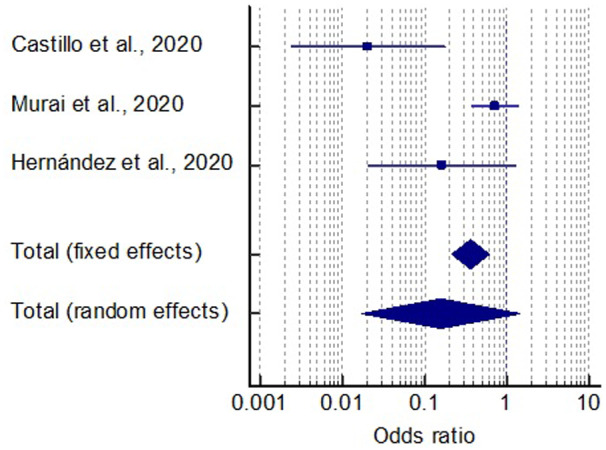
Forest plot for vitamin D supplementation on ICU stay.
Figure 3.
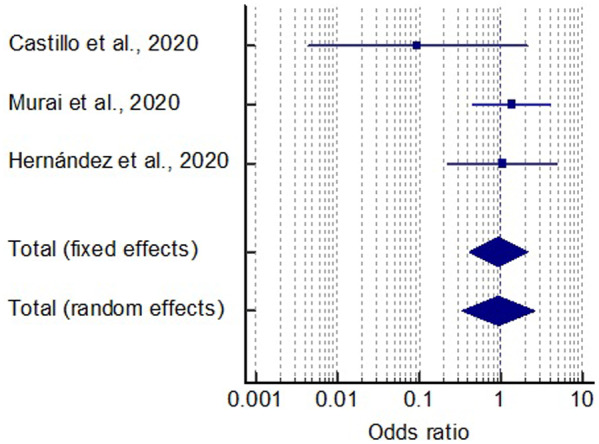
Forest plot for vitamin D supplementation on mortality.
Table 3.
Publication bias analysis
| ICU admission and vitamin D supplementation | |
|---|---|
| Egger’s test | |
| Intercept | −3.4604 |
| 95% CI | −21.9819 to 15.0610 |
| Significance level | P = 0.2538 |
| Begg’s test | |
| Kendall’s Tau | −1.0000 |
| Significance level | P = 0.1172 |
| Mortality and vitamin D supplementation | |
| Egger’s test | |
| Intercept | −2.4958 |
| 95% CI | −9.4871 to 4.4954 |
| Significance level | P = 0.1381 |
| Begg’s test | |
| Kendall’s Tau | −1.0000 |
| Significance level | P = 0.1172 |
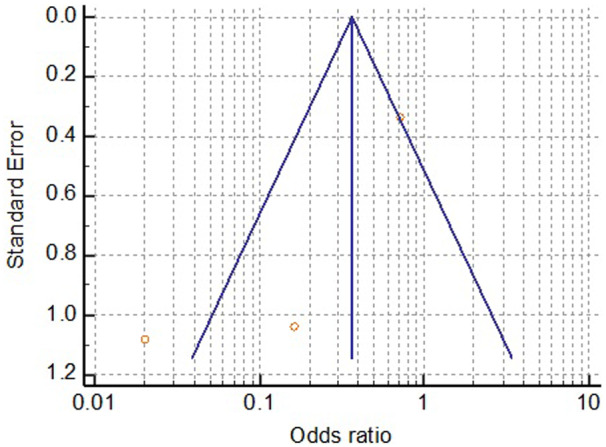
Meta-analysis of morality proportion in both groups was assessed and compared. It was found that vitamin D supplements have no effect on mortality as compared to placebo treatment/usual care (odds ratio: 0.93; 95% CI: 0.413–2.113; P = 0.87; Table 4; Figure 3). The findings were consistent with no heterogeneity as indicated by I2 (21.71%; P = 0.27). Even the funnel plot showed a satisfactory distribution of the studies (Figure 5). Similarly, Egger’s and Begg’s tests showed the absence of any significant publication bias (P > 0.05).
Table 4.
Meta-analysis summary for vitamin D supplementation and mortality
| Study | Intervention | Controls | Odds ratio | 95% CI | z | P | Weight (%) |
|
|---|---|---|---|---|---|---|---|---|
| Fixed | Random | |||||||
| Castillo et al., [15] 2020 | 0/50 | 2/26 | 0.0970 | 0.00448–2.100 | 7.72 | 10.56 | ||
| Murai et al., [16] 2020 | 8/120 | 6/120 | 1.357 | 0.456–4.037 | 61.38 | 55.00 | ||
| Hernández et al., [17] 2020 | 2/19 | 20/197 | 1.041 | 0.224–4.839 | 30.90 | 34.44 | ||
| Total (fixed effects) | 10/189 | 28/343 | 0.934 | 0.413–2.113 | −0.164 | 0.869 | 100.00 | 100.00 |
| Total (random effects) | 10/189 | 28/343 | 0.938 | 0.332–2.651 | −0.122 | 0.903 | 100.00 | 100.00 |
Figure 5.
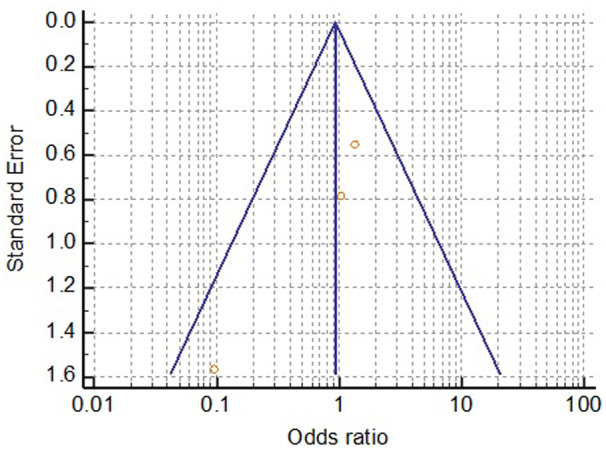
Funnel plot for vitamin D supplementation on mortality.
Figure 4.
Funnel plot for vitamin D supplementation on ICU stay.
Discussion
To the best of our knowledge, this is the first meta-analysis that synthesized cumulative evidences assessing impact of vitamin D supplementation on intensive care needs and mortality in hospitalized COVID-19 patients. It was observed that as compared to conventional care, vitamin D reduces severity of the disease; however, the results regarding improving mortality statistics could not reach to a statistically significant conclusion.
The first study conducted by Castillo et al.15 randomized 76 consecutive hospitalized COVID-19 patients in intervention to control group in ratio of 2:1 in Spain. The patients in the intervention arm received soft capsules of calcifediol (0.532 mg) on the day of admission through oral route and continued with the oral calcifediol (0.266 mg) on Days 3 and 7 and then weekly until discharge or ICU admission, whereas the patients in the control arm followed the standard treatment protocol with combination of hydroxychloroquine (400 mg every 12 h on the first day, and 200 mg every 12 h for the following 5 days) and azithromycin (500 mg orally for 5 days). Though baseline characteristics of patients in both the arms were matched, controls were more hypertensive (57.69% vs. 24.19%; P = 0.002). To adjust the effect of the confounders such as hypertension and diabetes, authors applied multivariate logistic regression analysis and found that the lower probability of ICU admission in intervention still remained significant [odds ratio = 0.03 (95% CI: 0.003 − 0.25)] as compared to control. Similarly, the mortality rates were also lower in patients treated with calciferol; however, it could not reach to a statistically significant level possibly due to extremely lower number of patients with adverse outcome. However, authors also acknowledged potential confounding effect of obesity and pre-existing deficiency of vitamin D as limitation of study. They recommended need of more extensive research with appropriately matched arms.
A double-blind, randomized, placebo-controlled trial in Brazil conducted by Murai et al.16 showed an effect of a single dose of 200 000 IU of vitamin D3 supplementation to hospital stay in severely ill COVID-19 patients. During the trial, 240 patients were equally randomized either in vitamin D supplementation or in placebo arm. The baseline demographic and clinical characteristics were comparable between both the arms. Though the supplementation was found to be safe and it improved serum 25-hydroxyvitamin D levels, it did not translate into any clinical benefits to the patient in the form of reduced hospital stay, the requirement of ICU support or mortality rate. Hence, the authors recommended against the use of vitamin D as adjuvant therapy in hospitalized COVID patients. Though it was found that requirement of oxygen therapy was low in patients treated with vitamin D as compared to placebo group (65.5% vs. 85.9%; P = 0.008). Removal of this study from overall analysis resulted in lowering of heterogeneity in cumulative findings of meta-analysis and yielded beneficiary effect on ICU needs with vitamin D.
Hernández et al.17 retrospectively assessed the role of vitamin D supplementation on 216 hospitalized COVID-19-positive patients in Spain. It was observed that 19 patients who were on vitamin D supplementation had drastically low requirement of ICU care as compared to their counterparts (5.3% vs. 25.4%); however, similar to other studies there was no difference in mortality (10.5% vs. 10.4%) between both the groups. The study also compared the serum levels of 25-hydroxyvitamin D in hospitalized COVID patients and compared it with the population-based controls of similar age and sex. It was found that the patients had significantly low levels of serum 25-hydroxyvitamin D as compared to population-based controls even in the presence of main confounding factors. However, the observational nature of the study was accepted as one of the important limitations. One important finding emerged from the study was that unlike other reports there was no relationship between serum 25-hydroxyvitamin D levels and the parameters of COVID-19 severity, such as ICU admission, the need for mechanical ventilation or mortality. This might be due to smaller number of events in the groups. However, it also highlights the need to assess vitamin D supplementation’s effect in a prospective manner using the randomized controlled trial study design.
SHADE study,18 a randomized controlled trial, assessed effect of high-dose vitamin D supplementation (60 000 IU of cholecalciferol—oral nano-liquid droplets) on 21-day recovery in COVID-19 patients. The authors found that greater proportion of vitamin D-deficient individuals with SARS-CoV-2 infection turned COVID-19 negative with a significant decrease in fibrinogen on high-dose cholecalciferol supplementation. However, they did not assess the role of supplementation on ICU requirement and mortality and hence were not included in the current meta-analysis.
Despite this heterogeneity among the studies, cumulative findings of the meta-analysis favored vitamin D supplementation for reduction of COVID-19 severity. However, more trials are required to substantiate the findings on other outcomes, especially community based and in-hospital trials should also be conducted in developing countries to assess potential of vitamin D supplementation in reducing hospitalization-, ICU- and ventilation needs and mortality rates.
Limitations
The quality of meta-analysis is directly proportionate to the quality of available secondary literature. As this meta-analysis is based on very early outcome reports exploring impact of vitamin D on various outcome indicators of COVID-19, it suffers from some inherent limitations as follows:
Number of trial available right now provides insufficient information regarding effect of various doses and appropriate duration of therapy on the outcome of interest. All three studies included in the meta-analysis used vitamin D supplementation for different duration and at different dosage. Evaluation of the impact using a standard protocol needs to be explored to understand exact effect of the intervention on various indicators.
The studies are also underpowered to assess the impact of supplementation in patients having severe deficiency of vitamin D at baseline. More robust randomized controlled trials with sufficient sample power are needed to obtain detailed understanding of these limitations.
Similarly, the baseline characteristics of the population enrolled in the studies were heterogeneous with respect to other comorbid conditions. Due to limited number of available evidences, assessment of vitamin D effect in these individual groups was not possible.
Conclusion
The findings of current meta-analysis suggest a potential role of vitamin D in reducing COVID-19 severity. However additional evidences with larger sample size and prospective study designs are needed to substantiate it further.
Conflict of interest. None declared.
References
- 1. Gruber-Bzura BM. Vitamin D and influenza-prevention or therapy? Int J Mol Sci 2018; 19:2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 2017; 356:i6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xiao L, Xing C, Yang Z, Xu S, Wang M, Du H, et al. Vitamin D supplementation for the prevention of childhood acute respiratory infections: a systematic review of randomized controlled trials. Br J Nutr 2015; 114:1026–34. [DOI] [PubMed] [Google Scholar]
- 4. Zisi D, Challa A, Makis A. The association between vitamin D status and infectious diseases of the respiratory system in infancy and childhood. Hormones (Athens) 2019; 18:353–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jolliffe DA, Camargo CA, Sluyter JD, Aglipay M, Aloia JF, Ganmaa D, et al. Vitamin D supplementation to prevent acute respiratory infections: systematic review and meta-analysis of aggregate data from randomised controlled trials. MedRxiv 2020; doi: 10.1101/2020.07.14.20152728. [DOI] [PubMed]
- 6. Aglipay M, Birken CS, Parkin PC, Loeb MB, Thorpe K, Chen Y, et al. , for the TARGet Kids! Collaboration. Effect of high-dose vs standard-dose wintertime vitamin D supplementation on viral upper respiratory tract infections in young healthy children. JAMA 2017; 318:245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kong W, Agarwal PP. Chest imaging appearance of COVID-19 infection. Radiol Cardiothorac Imaging 2020; 2:e200028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jain A, Chaurasia R, Sengar NS, Singh M, Mahor S, Narain S. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci Rep 2020; 10:20191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pereira M, Dantas Damascena A, Galvão Azevedo LM, de Almeida Oliveira T, da Mota Santana J. Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis. Crit Rev Food Sci Nutr 2020; 4:1–9. [DOI] [PubMed] [Google Scholar]
- 10. Pinzon RT, Angela Pradana AW. Vitamin D deficiency among patients with COVID-19: case series and recent literature review. Trop Med Health 2020; 48:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Das P, Samad N, Ahinkorah BO, Peprah P, Mohammed A, Seidu AA. Effect of Vitamin D deficiency on COVID-19 status: a systematic review. MedRxiv 2020; doi: 10.1101/2020.12.01.20242313.
- 12. Mathie RT, Lloyd SM, Legg LA, Clausen J, Moss S, Davidson JR, et al. Randomised placebo-controlled trials of individualised homeopathic treatment: systematic review and meta-analysis. Syst Rev 2014; 3:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higgins JP. 2011. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated July 2019]. The Cochrane Collaboration. www. cochrane-handbook. org (1 November 2020, date last accessed).
- 14. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol 2013; 66:408–14. [DOI] [PubMed] [Google Scholar]
- 15. Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, Alcalá Díaz JF, López Miranda J, Bouillon R, et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study. J Steroid Biochem Mol Biol 2020; 203:105751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CS, et al. Effect of vitamin D3 supplementation vs placebo on hospital length of stay in patients with severe COVID-19: a multicenter, double-blind, randomized controlled trial. MedRxiv 2020; doi: 10.1101/2020.11.16.20232397.
- 17. Hernández JL, Nan D, Fernandez-Ayala M, García-Unzueta M, Hernández-Hernández MA, López-Hoyos M, et al. Vitamin D status in hospitalized patients with SARS-CoV-2 infection. J Clin Endocrinol Metab 2020; doi: 10.1210/clinem/dgaa733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rastogi A, Bhansali A, Khare N, Suri V, Yaddanapudi N, Sachdeva N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study). Postgrad Med J 2020; 1–4. doi: 10.1136/postgradmedj-2020-139065. [DOI] [PubMed] [Google Scholar]