Abstract
Objective
The purpose of this article was to summarize the available evidence from systematic reviews on telerehabilitation in physical therapy.
Methods
We searched Medline/PubMed, EMBASE, and Cochrane Library databases. In addition, the records in PROSPERO and Epistemonikos and PEDro were consulted. Systematic reviews of different conditions, populations, and contexts—where the intervention to be evaluated is telerehabilitation by physical therapy—were included. The outcomes were clinical effectiveness depending on specific condition, functionality, quality of life, satisfaction, adherence, and safety. Data extraction and risk of bias assessment were carried out by a reviewer with non-independent verification by a second reviewer. The findings are reported qualitatively in the tables and figures.
Results
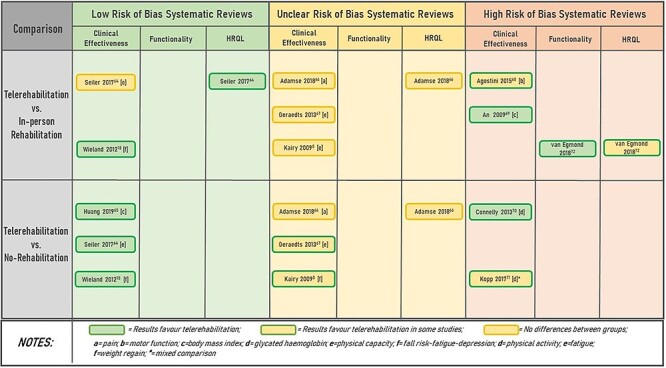
Fifty-three systematic reviews were included, of which 17 were assessed as having low risk of bias. Fifteen reviews were on cardiorespiratory rehabilitation, 14 on musculoskeletal conditions, and 13 on neurorehabilitation. The other 11 reviews addressed other types of conditions and rehabilitation. Thirteen reviews evaluated with low risk of bias showed results in favor of telerehabilitation versus in-person rehabilitation or no rehabilitation, while 17 reported no differences between the groups. Thirty-five reviews with unclear or high risk of bias showed mixed results.
Conclusions
Despite the contradictory results, telerehabilitation in physical therapy could be comparable with in-person rehabilitation or better than no rehabilitation for conditions such as osteoarthritis, low-back pain, hip and knee replacement, and multiple sclerosis and also in the context of cardiac and pulmonary rehabilitation. It is imperative to conduct better quality clinical trials and systematic reviews.
Impact
Providing the best available evidence on the effectiveness of telerehabilitation to professionals, mainly physical therapists, will impact the decision-making process and therefore yield better clinical outcomes for patients, both in these times of the COVID-19 pandemic and in the future. The identification of research gaps will also contribute to the generation of relevant and novel research questions.
Keywords: Digital Health, E-Health, Remote Physical Therapy, Telehealth, Telemedicine, Telerehabilitation
Introduction
Rehabilitation is necessary to improve people’s ability to live, work, and learn as much as possible and to maximize their functionality and quality of life. The impact extends to the community, society, and the economy.1,2 While rehabilitation is a comprehensive, multicomponent, and multidisciplinary intervention, the specific health condition and other determinants of the health system or resources available determine the minimum components required, which often include physical therapy.
Physical therapist interventions are required when movement and function are threatened to develop, maintain, and reestablish movement and functional capacity under the consideration that functional movement is fundamental to health and an optimal quality of life.3
Despite the knowledge of the benefits of rehabilitation and physical therapy, these services are under-used.4 If to this is added, on the one hand, that services or patient resources are scarce,5 and on the other that high demand leads to the saturation of services and the generation of waiting lists,6 the limitation of access becomes a reality.
In this scenario, where rehabilitation is necessary but insufficiently implemented, alternative rehabilitation models have been created using new resources such as digital practice to improve coverage. Thus, telerehabilitation, considered a branch of telehealth, is set up as a system for the control or monitoring of remote rehabilitation using telecommunications technologies, the purpose of which is to increase accessibility and improve continuity of care in vulnerable, geographically remote populations with disabilities with the potential for saving time and resources in health care.7,8
In the context of infection by SARS-CoV-2 and the spread of the COVID-19 pandemic, health services have had to adapt and prioritize safe delivery of care, limiting outpatient care. Thus, in addition to finding a way to address patients affected by COVID-19, an innovative method had to be found to provide rehabilitation or physical therapy.9,10 Although the main task is to contain the spread of the infection and treat patients affected by COVID-19, health systems cannot ignore other health problems that will inevitably require attention in the future. This crisis will undoubtedly impact the way health services work, and telerehabilitation could become a standard way of working since the previously identified barriers have had to be quickly overcome.11,12
There are several telerehabilitation models implemented globally.13,14 There are also many studies that have examined its effectiveness. To date, so many telerehabilitation trials are available that many systematic reviews have summarized the scattered and contradictory findings.15–23
To provide support to rehabilitation professionals, mainly physical therapists, with the best evidence available, this study aims to summarize the available information from systematic reviews on telerehabilitation in physical therapy in terms of clinical effectiveness, functionality, and quality of life. Additionally, adherence, satisfaction, and safety outcomes are evaluated.
Methods
An overview was conducted in a rapid review format adhering to the PRISMA declaration for systematic reviews.24 The protocol is registered in PROSPERO under number CRD42020185640, and the methodology has already been extensively described elsewhere.25 Likewise, the critical methods aspects of the overview are described below.
Data Sources and Searches
A systematic search was carried out in electronic databases (Medline/PubMed, EMBASE, Cochrane Library) up to May 4, 2020. The search strategy is available in Supplementary Table 1. In addition, the records in PROSPERO and the filtered databases Epistemonikos and PEDro were consulted. No restriction on language or date was applied.
Study Selection
Systematic reviews about several conditions of interest (musculoskeletal, neurological, respiratory, cardiovascular, etc), populations (infants, children, adults, and the elderly), and contexts (primary, secondary, and tertiary or specialist attention) were considered eligible if they included an explicit systematic review methodology and the primary studies included were clinical trials. If a systematic review included studies with other designs, they were considered only if they contained disaggregated data from clinical trials.
Systematic review protocols and conference proceedings were excluded if the full text was not available.
The intervention must have been telerehabilitation by physical therapy, defined as the provision of rehabilitation with interventions in any area of physical therapy carried out remotely or outside a usual session by a therapist distant from the patient and using telecommunications technologies. A systematic review was included if it considered comprehensive telerehabilitation with at least 1 component of physical therapy or if it contained a physical therapy treatment only. Physical therapy had to be therapeutic exercises, functional training, manual therapy, respiratory techniques and exercises, integumentary repair and protection techniques, electrotherapy and physical agents, or education as defined by the World Confederation for Physical Therapy.3
Reviews were excluded if they focused on physical activity without considering clinical outcomes (eg, blood pressure control) and on self-management of health conditions (eg, hypertension) where exercise and its effect on a clinical outcome were not included. Similarly, reviews were excluded that considered mobile applications and monitors (eg, pedometer) without involving the active action of a physical therapist. Finally, systematic reviews assessing virtual reality, without remote supervision by a therapist and not performed outside the health center, were also excluded.
Regarding comparisons, reviews were included if the telerehabilitation was compared with usual rehabilitation (in-person rehabilitation or center-based rehabilitation) or no rehabilitation (including usual care and waiting list).
Primary outcomes that had to be included in the reviews were clinical effectiveness for each condition (eg, decreasing low-back pain). Functionality was defined as the physical abilities that enable functional independence and enhance health-related quality of life (HRQL). Secondary outcomes were satisfaction with the care, adherence, and adverse effects.
The selection process was performed in the Rayyan software26 by 2 investigators, first screening by title and abstract and then by reviewing full texts of the relevant records. The discrepancies were resolved by a third reviewer with more than 10 years of experience.
Data Extraction and Quality Assessment
The relevant information from each eligible document was extracted through the REDCap platform (Research Electronic Data Capture software).27 The risk of bias of the included reviews was assessed with the Risk of Bias in Systematic Reviews (ROBIS) tool.28 ROBIS was applied in 3 consecutive phases. First, the relevance of the review for the research question was assessed. Then, concerns with the review process were identified for 4 domains: study eligibility criteria, identification and selection of the studies, data collection and study appraisal, and synthesis and findings. Finally, a judgment of overall bias in the review was generated. Both the data extraction and the appraisal with ROBIS were performed by 1 investigator, and a non-independent verification was carried out by a second experienced investigator. Additionally, information related to the methodological quality or risk of bias of the primary studies contained in the reviews assessed as having a low risk of bias was extracted to consider this aspect in formulating the conclusions of the overview.
Data Synthesis and Analysis
A qualitative report of the characteristics and effectiveness findings is summarized in the figures and tables by clinical area of rehabilitation or physical therapist interventions. In the design and presentation of the tables and figures, the risk of bias of the included reviews is considered.
Role of the Funding Source
The funder played no role in the design, conduct, or reporting of this study.
Results
Study Selection
In the initial search of electronic databases, 3298 potential studies were identified. Additionally, 8 records were identified through searches of filtered databases. After elimination of duplicates, 3089 unique entries were obtained, which were screened by title and abstract, excluding 2830 studies because they did not meet at least 1 of the eligibility criteria of our overview. Of the 259 studies reviewed in full text, 206 were excluded, with 53 systematic reviews finally being included. Supplementary Figure 1 shows the PRISMA flowchart and the reasons for excluding studies at the full-text stage are presented in Supplementary Table 2.
Characteristics of Included Studies
Twenty-one reviews were performed in Europe, 12 in Oceania, 11 in North America, 7 in Asia, 1 in Africa, and 1 in South America. All 53 reviews included 754 studies, of which 425 were included because they were clinical trials and considered outcomes of interest. Regarding synthesis, 26 were systematic reviews with qualitative synthesis only and 27 included a meta-analysis.
The most common areas of physical therapy included were: cardiorespiratory rehabilitation (15 studies), musculoskeletal rehabilitation (14 studies), and neurorehabilitation (13 studies). The other 11 reviews addressed other or mixed types of conditions and rehabilitation.
Most of the studies included adults (n = 41), older people (n = 2), the infant population (n = 2), and others (n = 8). In addition to physical therapists, other professionals participated, including psychologists (24 reviews), nurses (15 reviews), physicians (13 reviews), occupational therapists (8 reviews), and speech therapists (4 reviews).
Characteristics of Interventions
The most common interventions were therapeutic exercises (48), functional training (27), and education (25). Three reviews included only synchronous interventions, and 1 included solely asynchronous interventions. Most of the reviews (49) included mixed interventions. The majority of the platforms implemented to deliver the rehabilitation were webpages in 43 reviews, phone calls in 37 reviews, teleconference software in 31 reviews, and messaging services in 14 reviews. Virtual reality, understood as its use with remote assistance by the therapist, was also used and reported in 9 reviews.
Comparisons
The comparisons evaluated were telerehabilitation versus in-person rehabilitation (or usual rehabilitation) in 24 reviews, telerehabilitation versus no rehabilitation (or usual care or waiting list) in 27 reviews, and mixed comparisons (eg, telerehabilitation plus in-person intervention versus in-person intervention alone) in 22 reviews.
Outcomes
The most-reported outcomes were clinical effectiveness in 48 reviews, functionality in 35 reviews, quality of life in 32 reviews, user satisfaction and adherence in 15 reviews each, and adverse events in 13 reviews.
Characteristics by Area
Specific characteristics of included reviews are presented in Table 1 for musculoskeletal, neurological, cardiopulmonary, and other health conditions.
Table 1.
Characteristic of Included Reviewsa
| Author/Year | Search Date | Specific Population/Ages | No. of Studies Included in Original Review | No. of Studies Included in Overview b | Physical Therapist Intervention | Characteristics of Telerehabilitation | Type of Synthesis |
|---|---|---|---|---|---|---|---|
| Telerehabilitation in musculoskeletal conditions | |||||||
| Cottrell et al, 201729 | November 2015 | Any diagnosed primary musculoskeletal condition/>19 y | 13 | 7 | Therapeutic exercises, functional training and education | Mixed (synchronous and asynchronous) phone, internet | Qualitative and quantitative |
| Dario et al, 201730 | August 2015 | Non-specific low-back pain/>19 y | 11 | 8 | Therapeutic exercises and education | Mixed (synchronous and asynchronous) phone, internet | Qualitative and quantitative |
| Heapy et al, 201536 | September 2014 | Chronic, noncancer, nonheadache pain/> 19 y | 44 | 4 | Therapeutic exercises and functional training | Mixed (synchronous and asynchronous) phone, internet | Qualitative |
| Jansson et al, 202022 | February 2020 | Total hip arthroplasty and total knee arthroplasty/>19 y | 9 | 7 | Therapeutic exercises, functional training, and education | Mixed (synchronous and asynchronous) phone, internet, devices | Qualitative |
| Jiang et al, 201840 | May 2016 | Total knee arthroplasty/>65 y | 4 | 4 | Therapeutic exercises | Synchronous internet, devices | Qualitative and quantitative |
| Joice et al, 201737 | 1996 to May 2016 | Total knee arthroplasty/19 y or more | 17 | 3 | Therapeutic exercises | Mixed (synchronous and asynchronous) phone, internet | Qualitative |
| Grona et al, 201838 | December 2016 | Chronic musculoskeletal disorders (>3 mo duration)/>19 y | 17 | 2 | Therapeutic exercises and education | Synchronous internet | Qualitative |
| Schäfer et al, 201831 | July 2017 | Symptomatic unilateral or bilateral Osteoarthritis of knee/all ages | 7 | 6 | Therapeutic exercises | Synchronous phone, devices | Quantitative |
| Nicholl et al, 201732 | 2000 to March 2016 | Non-specific low-back pain/19 y or more | 9 | 3 | Therapeutic exercises, manual therapy, physical therapy, and education | Mixed (synchronous and asynchronous) phone, internet | Qualitative |
| Pastora-Bernal et al, 201739 | 2000 to October 2016 | Surgical procedures as result of orthopedic condition/>19 y | 15 | 9 | Therapeutic exercises | Mixed (synchronous and asynchronous) phone, internet | Qualitative |
| Pietrzak et al, 201316 | November 2011 | Osteoarthritis/>19 y | 5 | 3 | Therapeutic exercises and use of physical agents | Mixed (synchronous and asynchronous), internet | Qualitative |
| Shukla et al, 201733 | 2014 | Total knee arthroplasty/>65 y | 6 | 2 | Therapeutic exercises and functional training | Mixed (synchronous and asynchronous) phone, internet | Qualitative and quantitative |
| Srikesavan et al, 201934 | January 2016 | Clinical diagnosis of rheumatoid arthritis/>19 y | 4 | 3 | Therapeutic exercises, functional training, manual therapy, and education | Mixed (synchronous and asynchronous) phone, internet, devices | Qualitative |
| Wang et al, 201935 | November 2018 | Total hip arthroplasty and total knee arthroplasty/>19 y | 21 | 14 | Therapeutic exercises and functional training | Mixed (synchronous and asynchronous) phone, internet, devices | Qualitative and quantitative |
| Telerehabilitation in neurological conditions | |||||||
| Appleby et al, 201944 | November 2019 | Stroke survivors/> 18 y | 13 | 10 | Neurorehabilitation | Mixed (synchronous and asynchronous) Videoconferencing, virtual reality, messaging, phone, devices | Qualitative |
| Camden et al, 201947 | March 2018 | Children with disabilities/>12 y | 23 | 4 | Neurorehabilitation | Mixed (synchronous and asynchronous) webpage, videoconferencing, virtual reality, phone, devices | Qualitative |
| Chen et al, 201545 | March 2015 | Stroke survivors/> 18 y | 11 | 8 | Neurorehabilitation | Mixed (synchronous and asynchronous) phone, videoconferencing, robot-assisted rehabilitation, virtual reality | Quantitative |
| Di Tella et al, 202050 | December 2018 | Multiple sclerosis/all ages | 10 | 5 | Integrated rehabilitation approach (ITA) | Mixed (synchronous and asynchronous) phone, email, web platform | Quantitative |
| Johansson et al, 201117 | November 2009 | Stroke survivors/> 18 y | 9 | 2 | Neurorehabilitation | Mixed (synchronous and asynchronous) webpage, videoconferencing, devices | Qualitative |
| Khan et al, 201541 | July 2014 | Multiple sclerosis/> 18 y | 9 | 7 | Neurorehabilitation | Mixed (synchronous and asynchronous). Videoconferencing, virtual reality | Qualitative |
| Laver et al, 202042 | June 2019 | Stroke survivors/all ages | 22 | 9 | Neurorehabilitation | Mixed (synchronous and asynchronous) webpage, videoconferencing, virtual reality, devices, phone | Quantitative |
| Rintala et al, 201843 | December 2015 | Multiple sclerosis/> 18 y | 11 | 7 | Integral rehabilitation | Mixed (synchronous and asynchronous) devices, virtual reality, web platform, phone | Quantitative |
| Rintala et al, 201951 | May 2018 | Stroke survivors/all ages | 13 | 7 | Neurorehabilitation | Mixed (synchronous and asynchronous) devices, virtual reality, web platform, phone | Qualitative and quantitative |
| Sarfo et al, 201820 | June 2017 | Stroke survivors/not reported | 22 | 18 | Neurorehabilitation | Mixed (synchronous and asynchronous) phone, devices, webpage, educational platform, virtual reality | Qualitative |
| Schröder et al, 201946 | January 2018 | Stroke survivor/> 18 y | 7 | 4 | Motor training, balance training | Mixed (synchronous and asynchronous) devices, virtual reality | Qualitative |
| Tchero et al, 201848 | January 2018 | Stroke survivors/> 18 y | 15 | 7 | Integral rehabilitation | Mixed (synchronous and asynchronous) web platform, videoconferencing, devices | Qualitative and quantitative |
| Xiaoyan et al, 201949 | January 2019 | Stroke survivors/> 18 y | 11 | 7 | Therapeutic exercise | Mixed (synchronous and asynchronous) devices, virtual reality, videoconferencing | Qualitative and quantitative |
| Telerehabilitation in cardiopulmonary conditions | |||||||
| Almojaibel et al, 201619 | September 2014 | COPD/>19 y | 7 | 2 | Pulmonary rehabilitation (aerobic and resistance exercise, incentive of physical activity) | Mixed (synchronous and asynchronous) internet, devices | Qualitative |
| Brørs et al, 201956 | January 2003 to March 2018 | Coronary artery disease/>19 y | 24 | 9 | Physical activity and exercise management through exercise plans, supervision, and counselling | Mixed (synchronous and asynchronous) internet, devices, other | Qualitative |
| Chan et al, 201662 | July 2015 | COPD and with cardiovascular disease/>19 y | 9 | 8 | Cardiac and pulmonary rehabilitation | Mixed (synchronous and asynchronous) phone, internet, devices | Qualitative and quantitative |
| Cristo et al, 201821 | Not reported | Cardiovascular diseases/>19 y | 7 | 3 | Cardiac rehabilitation (videogames, incentive of walking, Nordic training, cycle-ergometer) | Mixed (synchronous and asynchronous) devices | Qualitative |
| Frederix et al, 201563 | Not reported | Cardiac patients/not reported | 37 | 13 | Cardiac rehabilitation and telemonitoring | Synchronism not reported phone, internet, devices |
Qualitative and quantitative |
| Hamilton et al, 201860 | August 2016 | Acute coronary syndrome and at least 1 coronary risk factor/>19 y | 9 | 2 | Cardiac rehabilitation | Mixed (synchronous and asynchronous) phone | Qualitative |
| Huang et al, 201552 | April 2014 | Myocardial infarction, angina, or underwent vascularization/>19 y | 9 | 9 | Cardiac rehabilitation | Mixed (synchronous and asynchronous) phone, other | Qualitative and quantitative |
| Hwang et al, 201561 | August 2013 | Cardiopulmonary diseases/>18 y | 11 | 11 | Integral rehabilitation | Mixed (synchronous and asynchronous) phone | Qualitative |
| Jin et al, 201957 | April 2018 | Coronary heart disease with at least 3 mo follow-up/>19 y | 29 | 26 | Cardiac rehabilitation | Mixed (synchronous and asynchronous) phone, internet, devices, other | Qualitative and quantitative |
| Lundell et al, 201553 | August 2013 | COPD according to GOLD, ERS, ATS, or BTS/>40 y | 9 | 7 | Cardiovascular exercises, pedometer, pursed lips, relaxation exercises | Mixed (synchronous and asynchronous) phone, internet, devices | Qualitative and quantitative |
| McCabe et al, 201758 | November 2016 | COPD according to GOLD 2016 and at any stage of illness/>19 y | 3 | 3 | Incentive of physical activity (pedometer, web incentive, and digital coaching) | Mixed (synchronous and asynchronous) internet | Quantitative |
| Munro et al, 201315 | May 2013 | Cardiac patients/>19 y | 9 | 7 | Cardiac rehabilitation | Mixed (synchronous and asynchronous) phone, internet | Qualitative |
| Neubeck et al, 200959 | December 2008 | Coronary heart disease with at least 3 mo follow-up/>19 y | 11 | 11 | Cardiac rehabilitation | Mixed (synchronous and asynchronous) phone, internet | Qualitative and quantitative |
| Rawstorn et al, 201654 | May 2015 | Coronary heart disease/>19 y | 11 | 8 | Cardiac rehabilitation | Asynchronous phone | Qualitative and quantitative |
| Su et al, 202055 | April 2019 | Coronary heart disease/>19 y | 14 | 7 | Cardiac rehabilitation | Mixed (synchronous and asynchronous) website, mobile application, email, text message, phone | Qualitative and quantitative |
| Telerehabilitation in other health conditions or mixed reviews | |||||||
| Adamse et al, 201866 | 2015 | Chronic pain in adults/>19 y | 16 | 9 | Exercise, physical activity, or training prescription | Mixed (synchronous and asynchronous) phone, internet | Qualitative and quantitative |
| Agostini et al, 201568 | January 2014 | Different conditions with impaired motor function/all ages | 12 | 12 | Motor training | Mixed (synchronous and asynchronous) phone, internet, devices | Quantitative |
| An et al, 200969 | April 2009 | Children and adolescents with overweight/6–18 y | 8 | 8 | Physical activity incentive within comprehensive rehabilitation | Mixed (synchronous and asynchronous) internet | Qualitative |
| Connelly et al, 201370 | March 2013 | Type 2 diabetes in adults/>19 y | 15 | 5 | Physical activity, training or exercise prescription, education | Mixed (synchronous and asynchronous) internet | Qualitative |
| van Egmond et al, 201872 | November 2016 | Cardiac, orthopedic surgery, and oncological surgery/>19 y | 23 | 23 | Physical exercise training within comprehensive rehabilitation | Mixed (synchronous and asynchronous) phone calls, internet platform, videoconference and devices | Qualitative and quantitative |
| Geraedts et al, 201367 | July 2012 | Older adults/>19 y | 32 | 25 | Structured physical activity or exercise | Mixed (synchronous and asynchronous) phone, internet platform and devices | Qualitative |
| Huang et al, 201965 | August 2014 | Adults/>19 y | 25 | 25 | Exercise or physical activity incentive, education | Mixed (synchronous and asynchronous) internet-based system, phone, text messaging, videoconferencing | Quantitative |
| Kairy et al, 20098 | February 2007 | Cardiac, respiratory, musculoskeletal, or neurological conditions/>19 y | 28 | 4 | Therapeutic exercise, functional training within comprehensive rehabilitation | Mixed (synchronous and asynchronous) internet, mobile phone, devices and software | Qualitative |
| Kopp et al, 201771 | November 2015 | Cancer survivors/all ages | 6 | 3 | Cardiorespiratory and physical training, education | Mixed (synchronous and asynchronous) phone, devices, apps, webpage, virtual reality, email, text messaging, video games | Qualitative |
| Seiler et al, 201764 | November 2016 | Cancer survivors with fatigue/>19 y | 15 | 2 | Resistance and aerobic exercise training | Mixed (synchronous and asynchronous) online interventions or smartphone apps | Qualitative |
| Wieland et al, 201218 | May 2011 | Overweight or obesity/>18 y | 18 | 13 | Physical activity and exercise education within a weight maintenance programs | Mixed (synchronous and asynchronous) computer-based intervention requiring user to interact directly with computer | Qualitative and quantitative |
a ATS = American Thoracic Society; BTS = British Thoracic Society; COPD = Chronic Obstructive Pulmonary Disease; ERS = European Respiratory Society; GOLD = Global Initiative for Chronic Obstructive Lung Disease. bClinical trial including physical therapy intervention and comparison group with in-person intervention, no intervention (usual care or wait list), or mixed intervention.
Musculoskeletal Rehabilitation
Musculoskeletal rehabilitation was reported in 14 systematic reviews,16,22,29–40 including 6 reviews that reported meta-analyses. The majority of conditions included were low-back pain, hip arthroplasty, total knee arthroplasty, and osteoarthritis, and the most common outcomes reported were pain intensity as an expression of clinical effectiveness, functionality—mostly measured by the WOMAC tool—and HRQL.
Neurorehabilitation
Neurorehabilitation was reported in 13 systematic reviews,17,20,41–51 including 7 reviews that reported meta-analyses. The majority of conditions included were stroke, multiple sclerosis, and physical impairment in children. The most common outcomes reported were motor function, mobility, balance, activities of daily living, and HRQL.
Cardiorespiratory Rehabilitation
The cardiorespiratory rehabilitation was reported in 15 systematic reviews,15,19,21,52–63 including 9 reviews that reported meta-analyses. The majority of conditions included were coronary artery disease, heart failure, and chronic obstructive pulmonary disease (COPD). The most common outcomes reported were related to clinical effectiveness as exercise capacity and HRQL.
Others Health Conditions
Other types of rehabilitation were reported in 11 reviews,8,18,64–72 of which 5 included meta-analyses. The majority of conditions covered were associated with metabolic disorders (such as obesity or diabetes) and cancer. The most common outcome reported was physical or exercise capacity.
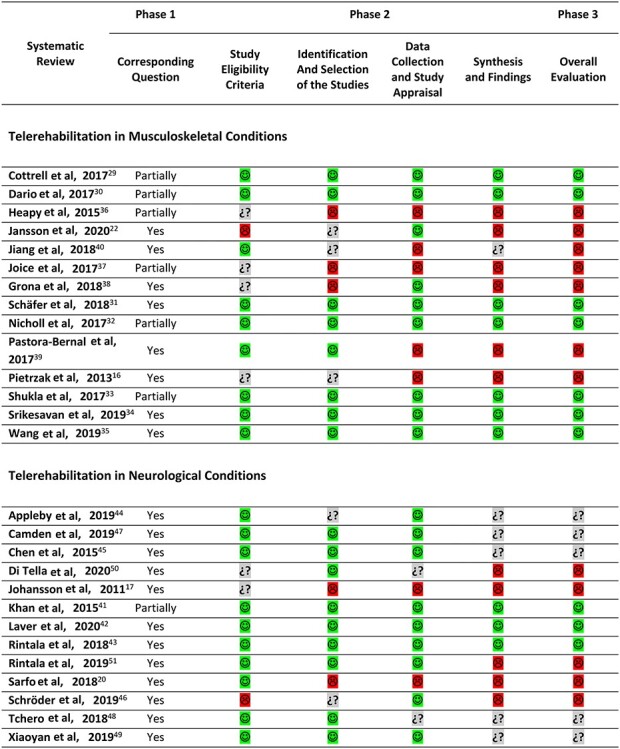
Risk of Bias
Of the 53 reviews included, 35 were relevant for the research question while the other 18 were partially relevant. Regarding the overall review process, 17 (32%) reviews were assessed as having a low risk of bias, 24 (45%) as having a high risk of bias, and 12 (23%) as having an unclear risk of bias in the evaluation with the ROBIS tool.
By clinical area, there were 7 of 14 (50%) musculoskeletal,16,22,36–40 4 of 13 (31%) neurological,17,20,50,51 and 7 of 15 (46%) cardiovascular15,19,21,60–63 reviews considered to be at high risk of bias, while 5 of 11 (46%) also had a high risk of bias assessment in reviews covering other health conditions.68–72 On the other hand, musculoskeletal, neurological, cardiovascular, and other health conditions were evaluated as being at low risk of bias in 7 (50%),29–35 3 (24%),41–43 4 (27%),52–55 and 3 (27%)18,64,65 reviews, respectively.
The domain with the greatest concerns was synthesis and findings, with 22 (42%) reviews assessing it as being at high risk of bias, and 12 (23%) reviews as being at an unclear risk of bias. Meanwhile, the domain with the best rating was that of data collection and study appraisal, with 37 (70%) reviews being evaluated as at low risk of bias.
The ratings for each of the 4 domains in the ROBIS tool and the overall evaluation for the included reviews by clinical area are presented in Table 2. Complementarily, Supplementary Table 1 shows the reported assessment of the methodological quality or risk of bias of the primary studies included, specifically in the systematic reviews evaluated as having a low risk of bias.
Table 2.
Risk of Bias of Systematic Reviews (ROBIS) Included by Clinical Areaa
|
|
|
|
Effect of Interventions
Supplementary Tables 4–7 show specific findings for several comparisons in each review included with the specification of outcomes and their measurements, source of results, conclusion of the review authors, and risk of bias overall evaluation.
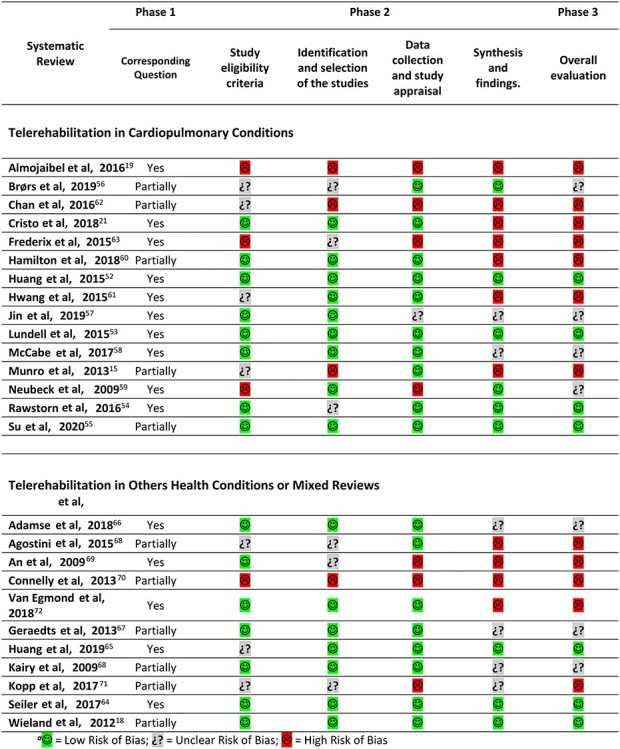
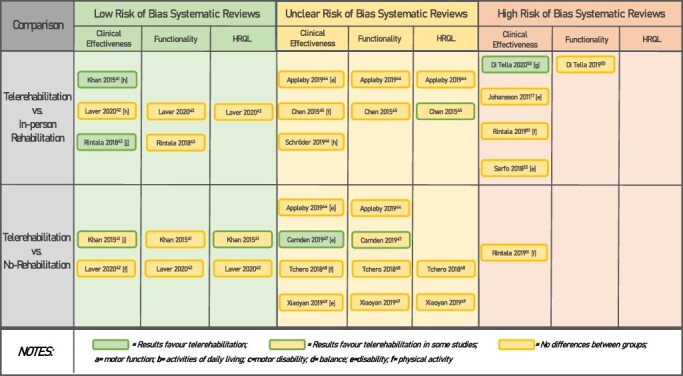
Musculoskeletal
A summary of results is presented in Figure 1. Only 1 low risk of bias review compared telerehabilitation with in-person rehabilitation. This review reported the effectiveness of telerehabilitation for clinical (pain intensity) and functionality outcomes and no difference between groups for HRQL in unspecified musculoskeletal conditions.29
Figure 1.
Summary of effectiveness results of telerehabilitation in musculoskeletal conditions by risk of bias assessment.
Seven low risk of bias reviews compared telerehabilitation with a control group without rehabilitation. Of these, 6, 4, and 1 reviews reported no difference between groups for clinical effectiveness evaluated as pain intensity,29–31,33–35 functionality,29,30,34,35 and HRQL,34 respectively. On the other hand, 2 reviews showed differences between groups in all primary studies included in favor of telerehabilitation for functionality in patients with osteoarthritis of knee31 and with low-back pain.32 Another 5 reviews reported better results of telerehabilitation for HRQL, specifically in low-back pain,30,32 symptomatic osteoarthritis of the knee,31 total knee,33,35 and hip arthroplasty.35 Additionally, 1 review reported clinical effectiveness for pain in 1 of 3 primary studies and for pain-related disability in non-specific low-back pain.32 Only 1 review considered the other outcomes, reporting no differences for satisfaction and adherence but more adverse effects for the intervention group.35
Another 6, 3, and 3 reviews evaluated as having a high risk of bias, reported no differences between telerehabilitation and in-person rehabilitation groups for clinical effectiveness,22,36–40 functionality,36,37,39 and HRQL,22,37,38 respectively. For the same comparison, 3 reviews reported better functionality in the telerehabilitation group,16,38,40 and 1 review showed same result in some primary studies included.22 On the other hand, for the telerehabilitation versus no-rehabilitation comparison, 1 high-risk-of-bias review showed better health status with telerehabilitation,36 and another high-risk-of-bias review reported better effectiveness for pain and functionality in some primary studies included.16
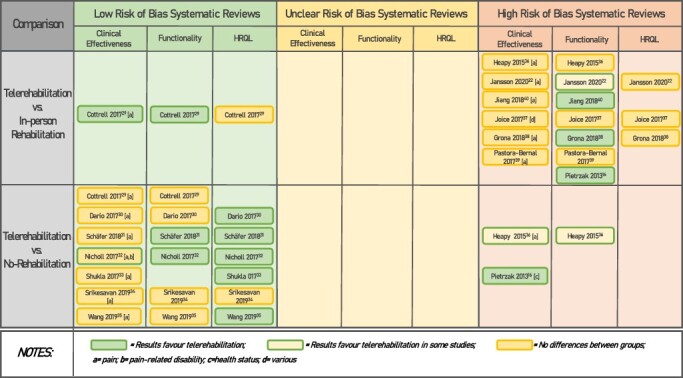
Neurorehabilitation
A summary of results is presented in Figure 2. Three low-risk-of-bias reviews compared telerehabilitation with in-person rehabilitation. One, 2, and 1 reviews reported no difference between groups for clinical effectiveness evaluated as balance,42 functionality,42,51 and HRQL,42 respectively. Two reviews showed better results in telerehabilitation groups for balance41 and physical activity51 in patients with multiple sclerosis. Two reviews considered other outcomes showing no adverse effects41 and no differences for satisfaction42 in the telerehabilitation group.
Figure 2.
Summary of effectiveness results of telerehabilitation in neurological conditions by risk of bias assessment.
Two low-risk-of-bias reviews compared telerehabilitation with a control group without rehabilitation. Of these, 1, 2, and 1 reviews reported no difference between groups for clinical effectiveness evaluated as balance,42 functionality,41,42 and HRQL,42 respectively. One review about multiple sclerosis reported clinical effectiveness for disability in 2 of 3 primary studies and for HRQL in 2 of 4 primary studies.41 Two reviews considered the other outcomes reporting no adverse effects41,42 and no differences42 or better satisfaction41 in the telerehabilitation group.
Three, 2, and 1 reviews evaluated as having an unclear risk of bias reported no differences for clinical effectiveness,44–46 functionality,44,45 and HRQL,44 respectively, between telerehabilitation and in-person rehabilitation groups. For the same comparison, 1 review showed mixed results for HRQL in patients with stroke.45 On the other hand, for the telerehabilitation versus no-rehabilitation comparison, 1 unclear-risk-of-bias review showed better motor function in children with disabilities in the telerehabilitation group and also reported better effectiveness for functionality in some of the primary studies included.47
Finally, of 4 high-risk-of-bias reviews, 1 review about multiple sclerosis reported better results for motor disability in the telerehabilitation group compared with the in-person group and no differences for functionality.50 The other 3 reviews reported no differences between groups for clinical effectiveness in stroke survivors17,20,51 in the same comparison. Additionally, 1 review at high risk of bias showed no differences between telerehabilitation and no-rehabilitation groups for activities of daily living in stroke survivors.51
Cardiopulmonary Rehabilitation
A summary of results is presented in Figure 3. Four reviews were evaluated as having a low risk of bias. Only 1 review with patients with coronary heart disease found better results for the telerehabilitation group compared with in-person rehabilitation in clinical effectiveness measured as all-cause mortality.52 On the other hand, 1 review with patients with COPD53 and 2 reviews with coronary heart disease patients54,55 reported no differences in clinical effectiveness between groups, regardless of the comparison group. One review included the HRQL outcome, reporting no differences between cardiac telerehabilitation and in-person cardiac rehabilitation,52 and another review also about cardiac rehabilitation showed mixed results for HRQL for both telerehabilitation versus in-person and telerehabilitation versus no-rehabilitation comparisons.55 Finally, 1 review showed better adherence for telerehabilitation compared with usual care.54
Figure 3.

Summary of effectiveness results of telerehabilitation in cardiopulmonary conditions by risk of bias assessment.
Another 4 reviews were evaluated as having an unclear risk of bias. Two of them, comparing telerehabilitation and in-person rehabilitation in patients with coronary heart disease, reported contradictory results. One review found a better HRQL in the telerehabilitation group and no> differences for clinical effectiveness measured as exercise capacity.56 In contrast, the other review reported no differences between groups for HRQL in most of the primary studies included, but better clinical effectiveness measured as prevention of all-cause mortality.57 On the other hand, for the telerehabilitation versus no-rehabilitation comparison, 2 and 1 unclear-risk-of-bias reviews showed better clinical effectiveness56,59 with telerehabilitation and no difference between groups,58 respectively. Two reviews reported better results for HRQL56,59 in some primary studies included.
Seven reviews were evaluated as having a high risk of bias. Of these, 2 reviews60,61 presented no differences between groups for exercise capacity when telerehabilitation was compared with in-person rehabilitation. One review15 reported better results with telerehabilitation for clinical outcomes and same comparison, and mixed results were reported for HRQL.15,60,61 For the telerehabilitation versus no-rehabilitation comparison, 2, 1, and 1 reviews showed better effectiveness for clinical outcomes,21,63 functionality,21 and HRQL,61 respectively. Another 2 and 1 reviews reported no differences between groups for clinical effectiveness19,62 and HRQL,19 respectively. Finally, 1 review obtained mixed results for clinical effectiveness.61
Other Health Conditions
A summary of results is presented in Figure 4. Three low-risk-of-bias reviews evaluated telerehabilitation (more extensive than telemedicine) versus usual care. One reported clinical effectiveness to decrease body mass index,65 another found that an eHealth intervention was effective at managing fatigue in cancer survivors,64 and the last review, about overweight or obesity, reported lower weight regain in the intervention group.18 Two reviews also compared telerehabilitation with an in-person intervention, 1 of them reported no differences between groups for physical capacity but better results for HRQL in the telerehabilitation group,64 and the other found better clinical effectiveness with telerehabilitation.18
Figure 4.
Summary of effectiveness results of telerehabilitation in others health conditions by risk of bias assessment.
Three reviews evaluated as having unclear risk of bias and comparing telerehabilitation with in-person intervention reported no difference between groups for clinical effectiveness8,66,67 and HRQL.66 The same reviews also compared telerehabilitation with no intervention, and while one found no difference for pain and HRQL,66 the other 2 reported mixed results for clinical effectiveness.8,67
Three and 1 reviews with a high risk of bias compared telerehabilitation with an in-person intervention and no intervention, respectively. From the first comparison, 1 reported a better result for clinical effectiveness measured as body mass index with telerehabilitation69 and the other reported mixed results.68 A third review showed better functionality in patients undergoing surgery and mixed results for HRQL in primary studies.72 For the second comparison, 1 review found better glycated hemoglobin control in adults with type 2 diabetes with telerehabilitation.70
Finally, 1 review with no comparison identified reported mixed results for physical activity in cancer survivors.71
Discussion
Fifty-three systematic reviews on telerehabilitation in physical therapy were included in this overview, 27 of which also included meta-analyses. These reviews covered different areas of the practice of physical therapy, mainly in the musculoskeletal, neurological, and cardiopulmonary areas.
Although there are global reviews and overviews that assess the effectiveness of telerehabilitation in some specific conditions,7,13,73–75 to our knowledge this is first comprehensive overview that compiles results on the effectiveness of telerehabilitation, including various clinical areas in the remit of the physical therapist. This makes the available evidence so widely applicable in different areas of rehabilitation even more so today where, in addition to having greater access to various technologies, it has been made urgently necessary for such rehabilitation services to reach users without them having to leave the home because they are geographically remote and due to the COVID-19 pandemic. This latter global situation has clearly produced a collateral damage to the users of rehabilitation and physical therapy services.76,77 The reported experiences in this scenario, although scarce,78 reveal opportunities and challenges that must be faced, such as technological barriers, ethical and legal regulations, health insurance coverage, and cultural difficulties that preclude the understanding that telehealth and digital practice can be an effective means of rehabilitation.79
The population for which there is effectiveness data is mainly adult, with few studies on children or adolescents. In the musculoskeletal area, the conditions they address include chronic musculoskeletal pain, arthroplasties, osteoarthritis, and low-back pain in addition to surgically treated orthopedic conditions. On the other hand, in the area of neurorehabilitation, the evidence focuses on stroke and multiple sclerosis. In the cardiopulmonary area, the conditions are those typically included in cardiac rehabilitation, such as coronary disease, or pulmonary rehabilitation, such as COPD. In other health conditions, the most frequently addressed were cancer and ageing, with these being observed as emerging areas.
With respect to the means by which telerehabilitation is implemented, the most frequently studied is the use of the mobile telephone with its messaging services and telephone calls, with knowledge emerging of the effectiveness of the applications available on smartphones as a digital practice tool. The internet, including web pages mainly with educational content, videos, or interactive gaming, is also frequently studied. Studies have investigated electronic devices that are basically used as remote monitors with physical therapy interventions. Also studied were specialized platforms (eg, for videoconferencing), especially when synchronous communication is required. Finally, and especially in the neurological area, virtual reality has been positioned as an intervention tool, also within telerehabilitation, and was included in this work only if reviews explicitly stated that virtual reality was used outside a health center.
Other factors must be considered in the extrapolation of the results. One is the fact that the reviews generally include studies from the past 2 decades, during which there has been great technological growth at the same time as the widespread use of these media by the population, which makes the first studies in the area very different from the most recent. The other factor is that most of the reviews and their primary studies were concentrated in Europe, North America, and Oceania, with little information originating from low-resource settings, which could affect the feasibility of using the technologies on a more global scale because these may be the places that have the least access as well as conventional rehabilitation and would benefit most from its implementation and reduce health disparities.
Although the knowledge available with these systematic reviews is broad and up to date, care must be taken in the interpretation of the results, basically due to the risk of bias present in the design process, conducting and analysis of the results from the systematic reviews, as well as the risk of inherent bias in the primary studies included in them. Only one-third of the reviews were assessed as having a low risk of bias, from which interpretations and extrapolations can be established with more certainty. Of these, however, in almost one-half of the clinical trials included, the evaluations of the quality or the risk of bias were deficient, which is why the uncertainty about the conclusions of the reviews continues to be high.
Although the establishment of the eligibility criteria, identification of primary studies, and data collection were not elements of great concern, the main issue with the systematic reviews included in this overview has to do with the process of synthesizing and interpreting the results. A specific aspect identified regards the results being synthesized in many reviews with no consideration as to which comparison groups were included in the clinical trials (eg, no rehabilitation or in-person or usual rehabilitation in a health center, an aspect that is a significant source of heterogeneity). To correct this problem to some extent, efforts were made to disaggregate data from the primary studies included in the reviews where it was feasible to do so, because tables were available, and there was a direct relation between the information they contained and the information in the text and the references of the studies, which only left a couple of reviews with a mixed comparison in results.
Another aspect of relevance in the interpretation of the findings was the lack of consideration of the risk of bias of the primary studies in establishing the conclusions of some of the reviews included, which may confuse readers, especially because the tendency in these cases is to overestimate the effects of telerehabilitation on physical therapy. One way to be able to draw valid conclusions in systematic reviews is to associate the results of the reviews or meta-analyses, that is, the estimator of the effect, their magnitude and accuracy, with the risk of bias. This is called certainty of evidence, which can be addressed in the process of interpreting the findings with the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) tool,80 which was used in no more than one-third of the reviews included.
Consideration must be given to interpreting the results of no differences between groups, a finding present in more than one-half of the reviews. This may be due to the fact there were effectively no differences between the groups or to statistical power achieved with the sum of patients in the studies included in the reviews being insufficient to find differences. The importance here is that—although assuming that telerehabilitation is not inferior to in-person rehabilitation or, on the other hand, that telerehabilitation produces the same effects as not doing rehabilitation—caution should be taken in interpreting this finding in light of the accuracy of the results, that is, the size of the sample reached.
This overview has some limitations related basically to having been conducted as a rapid review, and within these limitations it should be recognized that the grey literature was not searched and that the data extraction process and evaluation of the risk of bias were not performed in duplicate, in addition to having been conducted by a large group of reviewers, which could have affected the reliability of the data. To minimize this bias, a second reviewer with experience in systematic reviews extracted data and assessed the risk of bias.
Another limitation to consider in the extrapolation of the results is the fact that physical therapy can be delivered alone or within a more comprehensive rehabilitation program. Although this distinction was not specifically considered in the selection criteria of most reviews or in the description of interventions, it could be observed that physical therapy was often provided with other rehabilitation interventions.
Although the aim of this overview was broad, it was possible to cover, but it must be clearly understood that the scope of the interventions included are about physical therapy and related with therapeutic or secondary prevention and not those of assessment or primary prevention.
Implications for Clinical Practice
The available evidence shows that telerehabilitation could be comparable or better than the conventional methods of rehabilitation to reduce pain and improve physical function in musculoskeletal conditions generally. Additionally, telerehabilitation could improve functionality in patients with osteoarthritis in the knee and non-specific low-back pain in addition to improving quality of life in patients with non-specific low-back pain, osteoarthritis in the knee, and total arthroplasty in the knee and hip.
In the area of neurorehabilitation, telerehabilitation seems to contribute to balance and to increasing the levels of physical activity in patients with multiple sclerosis, but its contribution in terms of balance, functionality, and quality of life in patients with stroke is unclear.
On the other hand, cardiac rehabilitation via telematic means is possibly better than in-person cardiac rehabilitation at reducing mortality by any cause and also seems to contribute to a better ability to exercise and HRQL. On the other hand, pulmonary telerehabilitation could have results similar to conventional rehabilitation in terms of reducing dyspnea in patients with COPD.
Finally, the interventions performed by physical therapists using technological media could be effective at reducing overweight and obesity as well as improving the physical capacity and quality of life in cancer survivors.
Clinicians must bear in mind that these conclusions come from 17 low-risk-of-bias reviews while there are another 36 reviews with methodological issues and contradictory results. Regardless of this, and in a context where it is not possible to perform center-based or in-person rehabilitation—because patients cannot access a health center, the health centers cannot provide services to all those who need it, or, during the COVID-19 pandemic, where outpatient or in-person services have been reduced or suspended in many health centers—telerehabilitation seems to be a suitable and feasible strategy to implement. On this point it must be recognized that the previously identified barriers had to be circumvented quickly, making it increasingly more likely that this form of rehabilitation service will become a new standard during and after this pandemic.
Implications for Research
This rapid overview provides evidence that it is necessary to continue research in the area of telerehabilitation. On the one hand, systematic reviews must improve their processes of planning, execution, and synthesis of results, incorporating solid methodologies such as the GRADE approach. Future overviews in specific clinical areas could incorporate a global quantitative synthesis of results, doing new meta-analyses and even performing analyses of indirect comparisons. On the other hand, and perhaps most critically, is that clinical trials are conducted under strict considerations of internal validity and with optimal sample sizes. It is important to recognize that the results of a systematic review are only as valid as the results of the primary studies included. Another suggestion on this point is that non-inferiority studies be conducted, with their well-developed methodological particularities, so that they may conclude that telerehabilitation is not inferior to standard rehabilitation. Finally, a challenge to face is that these primary studies must be conducted in various resource settings, especially in the more precarious ones where there is less information.
Supplementary Material
Author Contributions
Concept/idea/research design: P. Seron, M.J. Oliveros
Writing: P. Seron, M.J. Oliveros, R. Gutierrez-Arias, R. Fuentes-Aspe, R. Torres-Castro, C. Merino-Osorio, J. Inostroza, R. Solano, G. Marzuca-Nassr, R. Aguilera, P. Lavados-Romo, F. Soto, C. Sabelle, G. Villarroel, P. Gomolán, S. Huaiquilaf, P. Sanchez
Data collection: P. Seron, M.J. Oliveros, R. Gutierrez-Arias, R. Fuentes-Aspe, R. Torres-Castro, C. Merino-Osorio, P. Nahuelhual, J. Inostroza, Y. Jalil, R. Solano, G. Marzuca-Nassr, R. Aguilera, P. Lavados-Romo, F. Soto, C. Sabelle, G. Villarroel, P. Gomolán, S. Huaiquilaf, P. Sanchez
Data analysis: P. Seron, M.J. Oliveros, R. Gutierrez-Arias, R. Fuentes-Aspe, R. Torres-Castro
Project management: P. Seron, M.J. Oliveros, R. Gutierrez-Arias, R. Fuentes-Aspe
Fund procurement: P. Seron
Consultation (including review of manuscript before submitting): Y. Jalil, F. Soto
Funding
This work was supported by a grant from the Fondecyt Program of National Agency for Research and Development (ANID), Chile (Grant number 1181734).
Systematic Review Registration
This protocol is registered in PROSPERO (CRD42020185640).
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
References
- 1. World Health Organization . World Report on Ageing and Health. 2015. Accessed July 2020. https://www.who.int/ageing/events/world-report-2015-launch/en/.
- 2. World Health Organization . Rehabilitation in Health Systems. 2017. Accessed July 2020. https://www.who.int/disabilities/rehabilitation_health_systems/en/.
- 3. World Confederation for Physical Therapy . Policy statement: description of physical therapy. 2017. Accessed June 2020. https://www.wcpt.org/policy/ps-descriptionPT
- 4. Falvey JR, Murphy TE, Gill TM, Stevens-Lapsley JE, Ferrante LE. Home health rehabilitation utilization among Medicare beneficiaries following critical illness. J Am Geriatr Soc. 2020;68:1512–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zziwa S, Babikako H, Kwesiga D, et al. Prevalence and factors associated with utilization of rehabilitation services among people with physical disabilities in Kampala, Uganda. A descriptive cross sectional study. BMC Public Health. 2019;19:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Deslauriers S, Déry J, Proulx K, et al. Effects of waiting for outpatient physiotherapy services in persons with musculoskeletal disorders: a systematic review. Disabil Rehabil. 2019;43:611–620. [DOI] [PubMed] [Google Scholar]
- 7. Rogante M, Grigioni M, Cordella D, Giacomozzi C. Ten years of telerehabilitation: a literature overview of technologies and clinical applications. Neuro Rehabilitation. 2010;27:287–304. [DOI] [PubMed] [Google Scholar]
- 8. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31:427–447. [DOI] [PubMed] [Google Scholar]
- 9. Bettger JP, Resnik LJ. Telerehabilitation in the age of COVID-19: an opportunity for learning health system research. Phys Ther. 2020;100:1913–1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Turolla A, Rossettini G, Viceconti A, Palese A, Geri T. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys Ther. 2020;100:1260–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Quigley A, Johnson H, McArthur C. Transforming the provision of physiotherapy in the time of COVID-19: a call to action for telerehabilitation. Physiother Can. 2020;73:e20200031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alpalhão V, Alpalhão M. Impact of COVID-19 on physical therapist practice in Portugal. Phys Ther. 2020;100:1052–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. 2017;4:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hailey D, Roine R, Ohinmaa A, Dennett L. Evidence of benefit from telerehabilitation in routine care: a systematic review. J Telemed Telecare. 2011;17:281–287. [DOI] [PubMed] [Google Scholar]
- 15. Munro J, Angus N, Leslie SJ. Patient focused internet-based approaches to cardiovascular rehabilitation—a systematic review. J Telemed Telecare. 2013;19:347–353. [DOI] [PubMed] [Google Scholar]
- 16. Pietrzak E, Cotea C, Pullman S, Nasveld P. Self-management and rehabilitation in osteoarthritis: is there a place for internet-based interventions? Telemed e-Health. 2013;19:800–805. [DOI] [PubMed] [Google Scholar]
- 17. Johansson T, Wild C. Telerehabilitation in stroke care—a systematic review. J Telemed Telecare. 2011;17:1–6. [DOI] [PubMed] [Google Scholar]
- 18. Wieland L, Falzon L, Sciamanna C, et al. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochrane Database Syst Rev 2012;8:CD007675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Almojaibel A. Delivering pulmonary rehabilitation for patients with chronic obstructive pulmonary disease at home using telehealth: a review of the literature. Saudi J Med Med Sci. 2016;4:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-rehabilitation after stroke: an updated systematic review of the literature. J Stroke Cerebrovasc Dis. 2018;27:2306–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cristo D d, Nascimento NP d, Dias AS, Sachetti A. Telerehabilitation for cardiac patients: systematic review. Int J Cardiovasc Sci. 2018;31:443–450. [Google Scholar]
- 22. Jansson MM, Rantala A, Miettunen J, Puhto AP, Pikkarainen M. The effects and safety of telerehabilitation in patients with lower-limb joint replacement: a systematic review and narrative synthesis. J Telemed Telecare. 2020;1357633X20917868. [DOI] [PubMed] [Google Scholar]
- 23. Liu P, Li G, Jiang S, et al. The effect of smart homes on older adults with chronic conditions: a systematic review and meta-analysis. Geriatr Nurs (Minneap). 2019;40:522–530. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Serón P, Oliveros MJ, Fuentes-Aspe R, Gutiérrez-Arias R. Efectividad de la telerehabilitación en terapia física: protocolo de una revisión global en tiempos que exigen respuestas rápidas. Medwave. 2020;20:e7970. [DOI] [PubMed] [Google Scholar]
- 26. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Whiting P, Savović J, Higgins JPT, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017;31:625–638. [DOI] [PubMed] [Google Scholar]
- 30. Dario AB, Moreti Cabral A, Almeida L, et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17:1342–1351. [DOI] [PubMed] [Google Scholar]
- 31. Schäfer AGM, Zalpour C, Von Piekartz H, Hall TM, Paelke V. The efficacy of electronic health-supported home exercise interventions for patients with osteoarthritis of the knee: systematic review. J Med Internet Res. 2018;20:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nicholl BI, Sandal LF, Stochkendahl MJ, et al. Digital support interventions for the self-management of low back pain: a systematic review. J Med Internet Res. 2017;19:e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shukla H, Nair SR, Thakker D. Role of telerehabilitation in patients following total knee arthroplasty: evidence from a systematic literature review and meta-analysis. J Telemed Telecare. 2016;23:339–346. [DOI] [PubMed] [Google Scholar]
- 34. Srikesavan C, Bryer C, Ali U, Williamson E. Web-based rehabilitation interventions for people with rheumatoid arthritis: a systematic review. J Telemed Telecare. 2019;25:263–275. [DOI] [PubMed] [Google Scholar]
- 35. Wang X, Hunter DJ, Vesentini G, Pozzobon D, Ferreira ML. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20:506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Heapy AA, Higgins DM, Cervone D, Wandner L, Fenton BT, Kerns RD. A systematic review of technology-assisted self-management interventions for chronic pain: looking across treatment modalities. Clin J Pain. 2015;31:470–492. [DOI] [PubMed] [Google Scholar]
- 37. Joice MG, Bhowmick S, Amanatullah DF. Perioperative physiotherapy in total knee arthroplasty. Orthopedics. 2017;40:e765–e773. [DOI] [PubMed] [Google Scholar]
- 38. Grona SL, Bath B, Busch A, Rotter T, Trask C, Harrison E. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: a systematic review. J Telemed Telecare. 2018;24:341–355. [DOI] [PubMed] [Google Scholar]
- 39. Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ. Evidence of benefit of telerehabilitation after orthopedic surgery: a systematic review. J Med Internet Res. 2017;19:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jiang S, Xiang J, Gao X, Guo K, Liu B. The comparison of telerehabilitation and face-to-face rehabilitation after total knee arthroplasty: a systematic review and meta-analysis. J Telemed Telecare. 2018;24:257–262. [DOI] [PubMed] [Google Scholar]
- 41. Khan F, Amatya B, Kesselring J, Galea M. Telerehabilitation for persons with multiple sclerosis. Cochrane Database Syst Rev. 2015;4:CD010508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. 2020;1:CD010255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rintala A, Hakala S, Paltamaa J, Heinonen A, Karvanen J, Sjögren T. Effectiveness of technology-based distance physical rehabilitation interventions on physical activity and walking in multiple sclerosis: a systematic review and meta-analysis of randomized controlled trials. Disabil Rehabil. 2018;40:373–387. [DOI] [PubMed] [Google Scholar]
- 44. Appleby E, Gill ST, Hayes LK, Walker TL, Walsh M, Kumar S. Effectiveness of telerehabilitation in the management of adults with stroke: a systematic review. PLoS One. 2019;14:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chen J, Jin W, Zhang XX, Xu W, Liu XN, Ren CC. Telerehabilitation approaches for stroke patients: systematic review and meta-analysis of randomized controlled trials. J Stroke Cerebrovasc Dis. 2015;24:2660–2668. [DOI] [PubMed] [Google Scholar]
- 46. Schröder J, van Criekinge T, Embrechts E, et al. Combining the benefits of tele-rehabilitation and virtual reality-based balance training: a systematic review on feasibility and effectiveness. Disabil Rehabil Assist Technol. 2019;14:2–11. [DOI] [PubMed] [Google Scholar]
- 47. Camden C, Pratte G, Fallon F, Couture M, Berbari J, Tousignant M. Diversity of practices in telerehabilitation for children with disabilities and effective intervention characteristics: results from a systematic review. Disabil Rehabil. 2019;0:1–13. [DOI] [PubMed] [Google Scholar]
- 48. Tchero H, Teguo MT, Lannuzel A, Rusch E. Telerehabilitation for stroke survivors: systematic review and meta-analysis. J Med Internet Res. 2018;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Xiaoyan Z, Pu W, Lijiao Y, et al. Home-based telerehabilitation for stroke survivors: a systematic review. Chinese J Evidence-Based Med. 2019;19:1226–1232. [Google Scholar]
- 50. Di Tella S, Pagliari C, Blasi V, Mendozzi L, Rovaris M, Baglio F. Integrated telerehabilitation approach in multiple sclerosis: a systematic review and meta-analysis. J Telemed Telecare. 2020;26:385–399. [DOI] [PubMed] [Google Scholar]
- 51. Rintala A, Päivärinne V, Hakala S, et al. Effectiveness of technology-based distance physical rehabilitation interventions for improving physical functioning in stroke: a systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2019;100:1339–1358. [DOI] [PubMed] [Google Scholar]
- 52. Huang K, Liu W, He D, et al. Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2015;22:959–971. [DOI] [PubMed] [Google Scholar]
- 53. Lundell S, Holmner Å, Rehn B, Nyberg A, Wadell K. Telehealthcare in COPD: a systematic review and meta-analysis on physical outcomes and dyspnea. Respir Med. 2015;109:11–26. [DOI] [PubMed] [Google Scholar]
- 54. Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102:1183–1192. [DOI] [PubMed] [Google Scholar]
- 55. Su JJ, Yu DSF, Paguio JT. Effect of eHealth cardiac rehabilitation on health outcomes of coronary heart disease patients: a systematic review and meta-analysis. J Adv Nurs. 2020;76:754–772. [DOI] [PubMed] [Google Scholar]
- 56. Brørs G, Pettersen TR, Hansen TB, et al. Modes of e-health delivery in secondary prevention programmes for patients with coronary artery disease: a systematic review. BMC Health Serv Res. 2019;19:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Jin K, Khonsari S, Gallagher R, et al. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2019;18:260–271. [DOI] [PubMed] [Google Scholar]
- 58. McCabe C, McCann M. Brady. AM. Management in chronic obstructive pulmonary disease (review). Cochrane Database Syst Rev. 2017;5:CD011425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Neubeck L, Redfern JU, Fernandez R, Briffa T, Bauman A, Ben FS. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review. Eur J Prev Cardiol. 2009;16:281–289. [DOI] [PubMed] [Google Scholar]
- 60. Hamilton SJ, Mills B, Birch EM, Thompson SC. Smartphones in the secondary prevention of cardiovascular disease: a systematic review. BMC Cardiovasc Disord. 2018;18:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Hwang R, Bruning J, Morris N, Mandrusiak A, Russell T. A systematic review of the effects of telerehabilitation in patients with cardiopulmonary diseases. J Cardiopulm Rehabil Prev. 2015;35:380–389. [DOI] [PubMed] [Google Scholar]
- 62. Chan C, Yamabayashi C, Syed N, Kirkham A, Camp PG. Exercise telemonitoring and telerehabilitation compared with traditional cardiac and pulmonary rehabilitation: a systematic review and meta-analysis. Physiother Can. 2016;68:242–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Frederix I, Vanhees L, Dendale P, Goetschalckx K. A review of telerehabilitation for cardiac patients. J Telemed Telecare. 2015;21:45–53. [DOI] [PubMed] [Google Scholar]
- 64. Seiler A, Klaas V, Tröster G, Fagundes CP. eHealth and mHealth interventions in the treatment of fatigued cancer survivors: a systematic review and meta-analysis. Psychooncology. 2017;26:1239–1253. [DOI] [PubMed] [Google Scholar]
- 65. Huang JW, Lin YY, Wu NY. The effectiveness of telemedicine on body mass index: a systematic review and meta-analysis. J Telemed Telecare. 2019;25:389–401. [DOI] [PubMed] [Google Scholar]
- 66. Adamse C, Dekker-Van Weering MGH, van Etten-Jamaludin FS, Stuiver MM. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. J Telemed Telecare. 2018;24:511–526. [DOI] [PubMed] [Google Scholar]
- 67. Geraedts H, Zijlstra A, Bulstra SK, Stevens M, Zijlstra W. Effects of remote feedback in home-based physical activity interventions for older adults: a systematic review. Patient Educ Couns. 2013;91:14–24. [DOI] [PubMed] [Google Scholar]
- 68. Agostini M, Moja L, Banzi R, et al. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare. 2015;21:202–213. [DOI] [PubMed] [Google Scholar]
- 69. An JY, Hayman LL, Park YS, Dusaj TK, Ayes CG. Web-based weight management programs for children and adolescents: a systematic review of randomized controlled trial studies. Adv Nurs Sci. 2009;32:222–240. [DOI] [PubMed] [Google Scholar]
- 70. Connelly J, Kirk A, Masthoff J, Macrury S. The use of technology to promote physical activity in type 2 diabetes management: a systematic review. Diabet Med. 2013;30:1420–1432. [DOI] [PubMed] [Google Scholar]
- 71. Kopp LM, Gastelum Z, Guerrero CH, Howe CL, Hingorani P, Hingle M. Lifestyle behavior interventions delivered using technology in childhood, adolescent, and young adult cancer survivors: a systematic review. Pediatr Blood Cancer. 2017;64:13–17. [DOI] [PubMed] [Google Scholar]
- 72. van Egmond MA, van der Schaaf M, Vredeveld T, et al. Effectiveness of physiotherapy with telerehabilitation in surgical patients: a systematic review and meta-analysis. Physiother (United Kingdom). 2018;104:277–298. [DOI] [PubMed] [Google Scholar]
- 73. Ambrosino N, Fracchia C. The role of tele-medicine in patients with respiratory diseases. Expert Rev Respir Med. 2017;11:893–900. [DOI] [PubMed] [Google Scholar]
- 74. Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2019;1:CD012732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Oldridge N, Pakosh M, Grace SL. A systematic review of recent cardiac rehabilitation meta-analyses in patients with coronary heart disease or heart failure. Future Cardiol. 2019;15:227–249. [DOI] [PubMed] [Google Scholar]
- 76. Negrini S, Grabljevec K, Boldrini P, et al. Up to 2.2 million people experiencing disability suffer collateral damage each day of COVID-19 lockdown in Europe. Eur J Phys Rehabil Med. 2020;56:361–365. [DOI] [PubMed] [Google Scholar]
- 77. Boldrini P, Garcea M, Brichetto G, et al. Living with a disability during the pandemic. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. 2020;56:331–334. [DOI] [PubMed] [Google Scholar]
- 78. Negrini S, Donzelli S, Negrini A, Negrini A, Romano M, Fabio Z. Feasibility and acceptability of telemedicine to substitute outpatient rehabilitation services in the COVID-19 emergency in Italy: an observational everyday clinical-life study. Arch Phys Med Rehabil. 2020;101:2027–2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Negrini S, Kiekens C, Bernetti A, et al. Telemedicine from research to practice during the pandemic. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. 2020;56:327–330. [DOI] [PubMed] [Google Scholar]
- 80. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.