Abstract
Objectives
In response to the coronavirus disease 2019 (COVID-19) pandemic, older adults are advised to follow social distancing measures to prevent infection. However, such measures may increase the risk of loneliness. The current study aimed to investigate (a) whether social distancing measures, particularly limiting close social interactions, are associated with loneliness among older adults, and (b) whether the association between social distancing measures and loneliness is moderated by sociodemographic characteristics.
Method
Data were from the fourth wave (April 29 to May 26, 2020) of the nationally representative Understanding America Study COVID-19 Survey. We used data on adults 50 years or older (N = 3,253). Logistic regression models of loneliness were performed. Five indicators of social distancing measures were considered: (a) avoiding public spaces, gatherings, or crowds; (b) canceling or postponing social activities; (c) social visits; (d) no close contact (within 6 feet) with people living together; and (e) with people not living together.
Results
Cancelling or postponing social activities and avoiding close contact with people living together were associated with 33% (odds ratio [OR] = 1.33, confidence interval [CI] = 1.06−1.68, p < .05) and 47% (OR = 1.47, CI = 1.09−1.99, p < .05) greater odds of loneliness, respectively. Furthermore, limiting close contact with coresidents increased the probability of loneliness more for males, non-Hispanic Whites, and those with higher levels of education and income.
Discussion
Efforts should be made to help older adults maintain social connectedness with close others by virtual communication methods. Our findings also call special attention to vulnerable groups at elevated risks of loneliness, emphasizing the need for tailored interventions.
Keywords: COVID-19, Psychosocial, Social distancing behaviors, Social isolation
In early March, the World Health Organization (WHO) declared the novel coronavirus (COVID-19) a global pandemic, and the Centers for Disease Control and Prevention (CDC) began encouraging Americans to practice “social distancing” measures to reduce transmission risk (CDC, 2020a). Recommendations around social distancing included avoiding public places as well as reducing physical contact with friends and nonhousehold family members (CDC, 2020b; WHO, 2020). With no vaccine and limited treatment options, social distancing became the primary strategy for reducing the chance of infection, particularly among high-risk groups such as older adults and those with preexisting health conditions. The lethality of COVID-19 is highest among those over age 50 (CDC, 2020a; Dowd et al., 2020), and particularly among older adults with impaired immune function and preexisting comorbidities (Dowd et al., 2020). Although social distancing has been a valuable tool for limiting the adverse impacts of COVID-19 in the population (Courtemanche et al., 2020), significant concerns have emerged that social distancing will increase loneliness among older adults as a result of reducing their contact with their community of friends and family (American Psychological Association, 2020; Berg-Weger & Morley, 2020; Hwang et al., 2020; Marziali et al., 2020; Miller, 2020; Tyrrell & Williams, 2020).
Prior to the COVID-19 pandemic, the prevalence of loneliness was already high in older adults. A quarter of community-dwelling individuals aged 65 or older were socially isolated, and 43% of adults aged 60 or older reported feelings of loneliness (National Academies of Sciences, Engineering, and Medicine [NASEM], 2020). Loneliness is often referred to as the “unpleasant experience that occurs when a person’s network of social support is deficient in some important way, either qualitatively or quantitatively” (Peplau & Perlman, 1982) and largely captures an individual’s perceptions of social isolation (Hawkley & Cacioppo, 2010). There is convincing evidence of the importance of social connections for older adults’ health and well-being, especially through feelings of loneliness. Loneliness has been linked to cognitive impairment, poor immune functioning, worse cardiovascular health, and increased mortality risk (NASEM, 2020). Therefore, it is important to understand whether the act of socially distancing during a pandemic would increase feelings of loneliness among older adults, which social distancing measures are more critical, and who would be at greater risk.
Our study is guided by two theoretical frameworks: (a) the Social Psychology Theory of Loneliness (Peplau & Perlman, 1979) and (b) the Socioemotional Selectivity Theory (Carstensen, 1995). The Social Psychology Theory of Loneliness draws upon an attributional approach, where loneliness arises as a discrepancy between one’s desired and actual levels of social contact. The restrictions of COVID-related social distancing may create this discrepancy, especially for those who adhere to the recommendations. For some older adults, socially distancing may dramatically reduce their day-to-day interactions, effectively shrinking their network and impacting the quality and quantity of their social support (Huxhold et al., 2014). Moreover, the experience of socially distancing, or even the expectation that one should be socially distanced due to their age, may be disturbing for older adults who feel they are being cut off from society. This sense of disconnection, as well as a sense that one is a burden, have been cited as potential explanations for the increased rates of suicide observed among older adults during the 2003 SARS outbreak (Chan et al., 2006; Cheung et al., 2008; Yip et al., 2010). Each social distancing measure, however, may not have equal effects on older adults’ loneliness. According to the Socioemotional Selectivity Theory, older individuals place greater emphasis on the quality of social relationships and prioritize interacting with close social partners. Indeed, prior work demonstrated that high quality of social contacts such as in-person interactions was more strongly associated with loneliness for older adults than online-based interactions (L. R. Green et al., 2001; M. J. Green et al., 2020, preprint; Pinquart & Sörensen, 2003). Taken all together, we hypothesize that social distancing measures during the COVID-19 pandemic that particularly limit high-quality relationships will be associated with loneliness (Hypothesis 1).
Importantly, loneliness is not a universal aspect of aging and can vary considerably across subpopulations of older adults (Armitage & Nellums, 2020; NASEM, 2020). The Social Psychology Theory of Loneliness explains that the likelihood of loneliness may be correlated with sociodemographic backgrounds. In support of this idea, studies have found notable differences in loneliness among sociodemographic groups: people living alone and/or who are not married/partnered and people who have lower socioeconomic status have a greater risk of loneliness (Cohen-Mansfield et al., 2016; NASEM, 2020). Thus, when considering the impact of social distancing measures on the older adult population, it is important to take into account the factors that predispose older adults to feelings of loneliness. Some older adults may be more vulnerable to certain distancing measures than others, and it is important to identify those who are most vulnerable to the potential adverse impacts of social distancing. Previous researchers argued that reduced social contact due to COVID-19 can impose additional hardship on older individuals who had already been socially isolated and at greater risk of being lonely (Marziali et al., 2020; Miller, 2020). To this end, we hypothesize that the association of social distancing measures with loneliness will be moderated by sociodemographic characteristics, such that social distancing would increase the probability of feeling lonely more for those with limited resources and networks than their counterparts (Hypothesis 2).
A handful of empirical studies examined changes in loneliness or its correlates during the early stage of the pandemic (Losada-Baltar et al., 2020; Luchetti et al., 2020; Tull et al., 2020). In a study of 1,310 Spanish adults (ages 18–88 years) conducted in March, Losada-Baltar and colleagues (2020) found that less contact with relatives was related to higher loneliness. From March 27 to April 5, Tull and colleagues (2020) conducted a nationwide survey of 500 American adults (ages 20–74 years) and found that adults living in areas under stay-at-home orders reported more loneliness. Although it is assumed that individuals practice more social distancing measures under stay-at-home orders, this study did not directly measure the behaviors and activities of the participants. Prior studies have also not focused specifically on loneliness at older ages. Thus, it remains unknown whether specific social distancing measures are associated with loneliness in older adults. To address this research gap, we use data from a nationally representative sample of U.S. adults that have been collecting information on individual experiences, behaviors, and activities throughout the COVID-19 epidemic to examine the link between various social distancing measures and loneliness among adults aged 50 or older.
Method
Data and Sample
We used data from the Understanding America Study (UAS) COVID-19 Survey. The UAS survey is an ongoing longitudinal national probability-based internet panel of approximately 9,000 noninstitutional U.S. adults administered by the Center for Economic and Social Research, University of Southern California. It has been collecting information at multiple time points each year on economic, labor, attitudinal, and health measures since 2014. Panel members are recruited using a random selection of households from a postal service list of addresses, which covers all households in the United States. The selected household receives a study invitation package where someone in the household is asked to complete the survey using a supplied log-in code via a computer, tablet, or smartphone. To ensure full coverage of the U.S. population, the UAS provides an internet-connected tablet to any household lacking internet access and/or devices.
To better understand how COVID-19 affects American households, the UAS COVID-19 national survey started tracking the impact of the pandemic on March 10, 2020. The survey was designed to provide insight into the impact of the virus on behaviors, employment and finances, and physical and psychosocial health and well-being. Among the 8,493 eligible panel members invited to the COVID survey in March, 6,884 (81%) completed the baseline survey. Follow-up surveys were fielded every 2 weeks beginning April 1, 2020. Over the 2-week survey period, about 7% of the respondent pool was asked each day to fill out the survey within 2 weeks. More than 90% completed the survey within 2 weeks for each wave, and most completed it on the day they received it.
This study used the fourth wave of the UAS COVID data, collected from April 29 to May 26 because it was the first time a measure of loneliness was included in the survey. While other subsequent waves included loneliness, we found no significant change over time for loneliness (see Figure 1). Therefore, we limit our sample to Wave 4 for this analysis. As of the start date of Wave 4 (April 29), 6,968 eligible panel members consented to participate in the survey. Among them, 6,354 completed the survey in time, resulting in a participation rate of 75% for the total pool of the UAS panel and 91% for this wave. The study is limited to adults 50 years or older, which further reduced the sample to 3,348 respondents. After excluding an additional 95 respondents who had missing information on covariates (2.8% of the age-eligible sample), the final analytical sample consisted of 3,253 respondents. The participant flow chart is shown in Supplementary Figure 1.
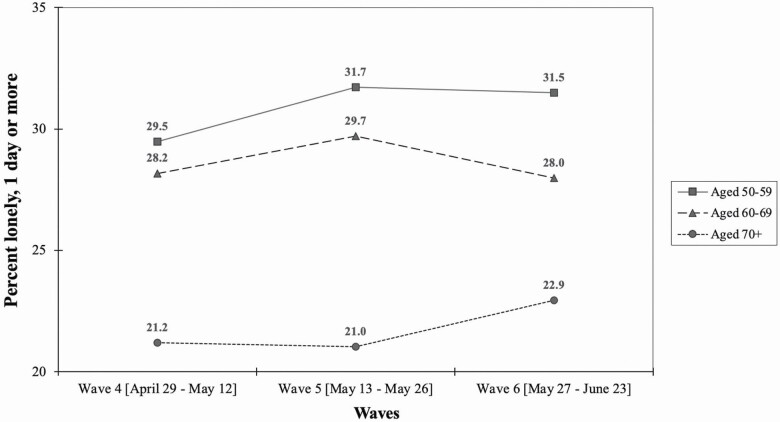
Figure 1.
Changes in loneliness over time.
Measures
Loneliness
Loneliness was measured with a single-item question: “In the past 7 days, how often have you felt lonely?” Response options were 1 = not at all or less than 1 day, 2 = 1−2 days, 3 = 3−4 days, and 4 = 5−7 days. We coded participants as being lonely if they reported experiencing loneliness for 1 or more days. Single-item measures of loneliness have been used in previous studies on older adults’ loneliness (Pinquart & Sorensen, 2001) and have been shown to have high concordance with multiple-item loneliness scales (Fokkema et al., 2012).
COVID-19-related social distancing measures
Participants were asked about their social activities with the following question: In the last 7 days, have you (1) gone out to a bar, club, or other places where people gather; (2) gone to a friend, neighbor, or relative’s residence; (3) had visitors such as friends, neighbors, or relatives at your residence; (4) attended a gathering with more than 10 people; (5) been placed in isolation or quarantine; (6) had close contact (within 6 feet) with people who live with you; (7) had close contact (within 6 feet) with people who do not live with you; (8) canceled or postponed personal or social activities; and (9) avoided public spaces, gatherings, or crowds? The response options were yes, no, and unsure, and unsure responses were excluded from the analyses. We did not use questions about (1) going out, (4) attending gatherings, (5) or being quarantined because so few participants answered yes (ranged 1.6%–5.1%). With the remaining six items, we created five different indicators of COVID-19-related social distancing measures.
First, we created two dichotomous variables and coded each as 1 if participants reported that they have (a) avoided public spaces, gatherings, or crowds and (b) canceled or postponed personal or social activities. As a measure of (c) social visits, we combined information on whether the participant had had visitors with whether they had gone to others’ residence to create a dichotomous variable coded 1 if there were no visits. Other cases—only had visitors, only gone to others’ residence, and both—were coded as 0. Finally, as a measure of close contact (within 6 feet), we utilized information on whether the participant had close contact with other people. Two dichotomous variables were created and each coded as 1 if the participant reported that they did not have close contact (d) with people living together and (e) with people not living together.
Sociodemographic characteristics
We included several sociodemographic risk factors for loneliness. Age was measured in years, and it was further grouped into three groups in multivariate analyses: ages 50–59, ages 60–69, and ages 70 or older. Gender was coded 0 for male and 1 for female. Race/ethnicity was classified as non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, and others (American Indian, Alaska Native, Hawaiian/Pacific Islander, or Mixed). We also included an indicator of household composition: (1) single-person household, (2) spouse/partner only household, (3) spouse/partner and other family and/or nonfamily household, and (4) nonspouse/partner family and/or nonfamily household (nonfamily members include tenant and roommate/housemate). Educational attainment was classified as high school or less education, some college education without a bachelor’s degree, and a bachelor’s degree or more education. Annual household income was categorized into four groups, roughly representing quartiles: less than $30,000, $30,000–$59,999, $60,000–$99,999, and $100,000 or more.
Government’s requirement for social distancing
Participants were asked about their awareness of social distancing policies with the following question: “Are Federal, state, or local governments currently requiring you to limit non-essential travel?” The responses were coded 1 for yes and 0 for no or unsure.
Analytical Strategy
First, we examined the bivariate associations between COVID-19-related social distancing measures and reported loneliness. Next, to better understand the effects of social distancing on loneliness, we fit a series of multivariate logistic regression models. The models included sociodemographic characteristics and five COVID-19-related social distancing measures. There was no difference between models with each measure entered separately and a model with all measures included simultaneously. Finally, to determine whether the effects of social distancing measures would be different by sociodemographic factors, we included interaction terms between each sociodemographic characteristic and social distancing measures that were significant in the previous model. To further explore a significant interaction term, post-hoc pairwise comparisons of marginal predictions were made using contrasts that enable group differences (i.e., male vs female) to be estimated for each response (i.e., yes vs no) to a social distancing measure (MacKinnon, 2008). Differences were tested with Wald chi-squared tests. Sample weights were applied to adjust for differential sampling probabilities and survey nonresponse. Analyses were conducted using STATA version 16.0.
Results
Changes in Loneliness Over Time
Figure 1 depicts the estimated prevalence of loneliness across the survey waves collected from April 29 to June 23. At Wave 4, about 28%−29% of adults aged 50−69 reported feelings of loneliness for 1 day or more in the past 7 days, which was relatively higher than 21% of adults aged 70 or older. However, the prevalence of loneliness did not change substantially over time. Therefore, as previously stated, we limit our sample to Wave 4 for the subsequent analyses.
Sample Characteristics
Table 1 shows the characteristics of the analytical sample. The mean age was 63.5 years and ranged from 50 to 101. About 36% were aged 50–59, 39% were aged 60–69, and the remaining 25% were aged 70 and older. Non-Hispanic Whites were the largest group (72%). For racial/ethnic minorities, the sample consisted of 11% non-Hispanic Blacks, 11% Hispanics, 4% Asians, and 3% others (i.e., American Indian, Alaska Native, Hawaiian/Pacific Islander, or Mixed). About 43% lived with spouse/partner, 21% were from single-person households, 23% lived with spouse/partner and other family and/or nonfamily household, and the remaining 13% lived with nonspouse/partner family and/or nonfamily household. Most respondents reported having a high school diploma or less (41%). Among higher levels of education, 27% reported some college without a bachelor’s degree, and 32% reported obtaining a bachelor’s or greater. Household income levels were distributed fairly evenly across categories, with most reporting making between $30,000 and $59,999 (29%) and least reporting making over $100,000 (22%). More than half of the sample (62%) reported that their Federal, state, or local governments required limiting nonessential travels. Overall, a majority of respondents reported engaging in each social distancing measure: 88% reported avoiding public spaces, gathering, or crowds and 58% reported canceling or postponing social activities. At more personal levels, more than half of the respondents reported no social visits (55%). Lastly, 25% of respondents reported not having close contact with people living together, and 61% reported not having close contact with people not living together. The estimated prevalence of loneliness, defined as feelings of loneliness at least 1 day in the past 7 days, was 27%. More specifically, 15% of the sample felt lonely for 1−2 days, 7% reported feelings of loneliness for 3−4 days, and 5% for 5−7 days.
Table 1.
Descriptive Characteristics of the Analytic Sample (N = 3,253)
| Variables | (M ± SD) or N | % |
|---|---|---|
| Sociodemographic characteristics | ||
| Age (range: 50–101) | (63.5 ± 8.91) | |
| Aged 50–59 | 1,232 | 35.6 |
| Aged 60–69 | 1,209 | 39.0 |
| Aged 70–79 | 651 | 19.7 |
| Aged 80+ | 161 | 5.7 |
| Gender (female) | 1,753 | 46.0 |
| Race/ethnicity | ||
| Non-Hispanic White | 2,531 | 71.7 |
| Non-Hispanic Black | 223 | 10.5 |
| Hispanic | 232 | 10.7 |
| Non-Hispanic Asian | 107 | 4.2 |
| Others | 160 | 2.9 |
| Household composition | ||
| Single person | 700 | 21.4 |
| Spouse/partner only | 1,409 | 43.2 |
| Spouse/partner and other family and/or nonfamily | 719 | 22.6 |
| Nonspouse/partner family and/or nonfamily | 425 | 12.8 |
| Education | ||
| High school or less | 695 | 41.3 |
| Some college | 1,248 | 26.6 |
| Bachelor’s degree or more | 1,310 | 32.1 |
| Household income level | ||
| <$30,000 | 725 | 26.3 |
| $30,000–$59,999 | 878 | 28.9 |
| $60,000–$99,999 | 821 | 23.3 |
| $100,000+ | 829 | 21.5 |
| Governments’ requirement for social distancing | ||
| Yes | 1,931 | 61.8 |
| No or unsure | 1,322 | 38.2 |
| COVID-19-related social distancing measures | ||
| Avoided public spaces, gatherings, or crowds | 2,873 | 87.6 |
| Canceled or postponed social activities | 1,865 | 57.9 |
| No social visits with friends, neighbors, or relatives | 1,784 | 54.9 |
| Close contact (within 6 feet) with other people | ||
| No close contact with people living together | 820 | 25.4 |
| No close contact with people not living together | 1,883 | 60.5 |
| Prevalence of loneliness (≥1 day) | 916 | 26.8 |
| Not at all or <1 day | 2,337 | 73.2 |
| 1–2 days | 539 | 15.2 |
| 3–4 days | 224 | 6.8 |
| 5–7 days | 153 | 4.8 |
Note: Mean (M), SD, and N were unweighted, while % was weighted.
Social Distancing Measures and Loneliness
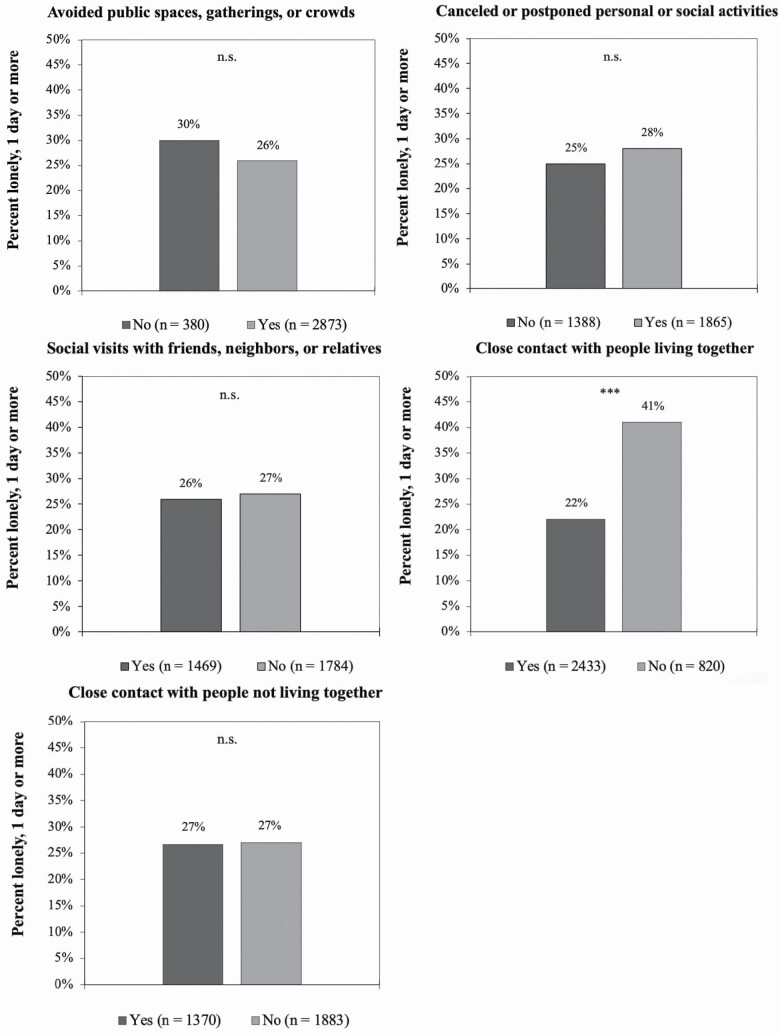
The bivariate associations between social distancing measures and loneliness are presented in Figure 2. The bars represent the weighted percentage of respondents who reported that they were lonely by each social distancing measure, and the numbers in parentheses represent the unweighted number of people who belonged to each category. For avoiding public spaces, gatherings, or crowds, 88% (n = 2,873) of the total participants answered yes and 12% (n = 380) answered no. Among those who answered yes, 26% reported a feeling of loneliness, which is slightly lower than 30% who answered no. However, these differences were not statistically significant. A total of 1,865 participants reported that they canceled or postponed social activities. Among them, 28% reported a feeling of loneliness, which was higher than the 25% of those who did not cancel social activities, though these differences were not statistically significant (p = .08). With regard to social visits, 1,784 participants answered no, and among them, 27% reported a feeling of loneliness. In contrast, 26% of those who answered yes reported feeling lonely, and there was no statistical difference. We did find a statistically significant difference in loneliness among respondents who reported having close contact (within 6 feet) with people living together. A total of 820 respondents did not have close contact with people living together, and they had almost twice the levels of loneliness as respondents who did have close contact (41% vs 22%). However, no significant difference in loneliness was observed between people who had close contact with people not living together and those who did not (both 27%).
Figure 2.
Loneliness by COVID-19-related social distancing measures. (A) Avoided public spaces, gatherings, or crowds. (B) Canceled or postponed social activities. (C) Social visits with friends, neighbors, or relatives. (D) Close contact (within 6 feet) with people living together. (E) Close contact (within 6 feet) with people not living together. Note: ***p < .001. n.s. = not statistically significant; bars represent the weighted percent of respondents who reported that they were lonely by each social distancing measure, and numbers in parentheses represent the unweighted number of people who belonged to each category.
Logistic Regression Model of Loneliness
Results from the logistic regression model of loneliness are reported in Table 2. Odds ratios (ORs) are presented with 95% confidence intervals (CIs). ORs below 1 indicate a lower likelihood of reporting loneliness, while ORs greater than 1 indicate a greater likelihood of reported loneliness. We found several significant associations of loneliness with age, gender, race/ethnicity, household composition, and household income. Adults aged 50–59 and 60–70 were more likely to report loneliness than adults aged 70+, with 92% greater odds and 55% greater odds, respectively. Females were 56% more likely to report loneliness. Non-Hispanic Blacks and Hispanics were less likely to report feeling lonely than non-Hispanic Whites (41% less likely for blacks and 60% less likely for Hispanics). Compared to respondents living with a spouse/partner only, those from a single household and those living with others only had increased odds of reporting being lonely by 135% and 99%, respectively. Lastly, compared to older adults making $100k, those making less than $30k were more likely to report being lonely. No significant associations were observed for educational attainment and governments’ requirement for social distancing with loneliness.
Table 2.
Logistic Regression Models of Loneliness, the Understanding America Study (N = 3,253)
| Variables | Odds ratio | 95% CI |
|---|---|---|
| Sociodemographic characteristics | ||
| Age (ref: aged 70+) | ||
| Aged 50–59 | 1.92*** | 1.40−2.62 |
| Aged 60–69 | 1.55** | 1.16−2.08 |
| Female | 1.56*** | 1.24−1.96 |
| Race/ethnicity (ref: White) | ||
| Black | 0.59* | 0.39−0.89 |
| Hispanic | 0.40** | 0.24−0.68 |
| Asian | 0.73 | 0.37−1.42 |
| Other | 0.56 | 0.27−1.14 |
| Household composition (ref: with a spouse/partner only) | ||
| Single | 2.35*** | 1.66−3.31 |
| Spouse/partner and other family and/or nonfamily | 1.17 | 0.85−1.60 |
| Nonspouse/partner family and/or nonfamily | 1.99*** | 1.40−2.82 |
| Education (ref: bachelor’s+) | ||
| High school or less | 1.05 | 0.79−1.41 |
| Some college | 0.89 | 0.69−1.15 |
| Household income (ref: $100k+) | ||
| <$30k | 1.47* | 1.004−2.16 |
| $30k–$59,999 | 1.32 | 0.93−1.86 |
| $60k–$99,999 | 1.07 | 0.76−1.49 |
| Government’s requirement for social distancing | ||
| Yes | 1.10 | 0.88−1.38 |
| COVID-19-related social distancing measures | ||
| Avoided public spaces, gatherings, or crowds | 0.76 | 0.54−1.08 |
| Canceled or postponed social activities | 1.33* | 1.06−1.68 |
| No social visits with friends, neighbors, or relatives | 1.13 | 0.89−1.43 |
| No close contact with people living together | 1.47* | 1.09−1.99 |
| No close contact with people not living together | 0.98 | 0.77−1.25 |
| Significant interaction effects | ||
| Gender | ||
| Female × No close contact with people living together | 0.55* | 0.34−0.87 |
| Race/ethnicity (ref: White) | ||
| Black × No close contact with people living together | 0.40* | 0.19−0.85 |
| Hispanic × No close contact with people living together | 0.90 | 0.28−2.82 |
| Asian × No close contact with people living together | 0.64 | 0.16−2.56 |
| Other × No close contact with people living together | 0.92 | 0.22−3.86 |
| Education (ref: bachelor’s+) | ||
| High school or less × No close contact with people living together | 0.40** | 0.23−0.71 |
| Some college × No close contact with people living together | 0.66 | 0.39−1.13 |
| Household income (ref: $100k+) | ||
| <$30k × No close contact with people living together | 0.48 | 0.23−1.00 |
| <$30k–$59,999 × No close contact with people living together | 0.45* | 0.21−0.95 |
| <$60k–$99,999 × No close contact with people living together | 0.50 | 0.22−1.12 |
Notes: Estimates were weighted.
*p < .05. **p < .01. ***p < .001.
In terms of COVID-19-related social distancing measures, we did not find a significant association of avoiding public spaces, gatherings, or crowds with loneliness. However, we found a positive association between canceling social activities and loneliness. Respondents who canceled or postponed social activities were more likely to report being lonely (OR = 1.33, CI = 1.06−1.68, p < .05). Next, we found no statistical association between social visits and loneliness. Lastly, respondents who reported no close contact (within 6 feet) with people living together were more likely to report loneliness (OR = 1.47; CI = 1.09−1.99, p < .05), whereas there was no significant relationship between loneliness and close contact with people not living together.
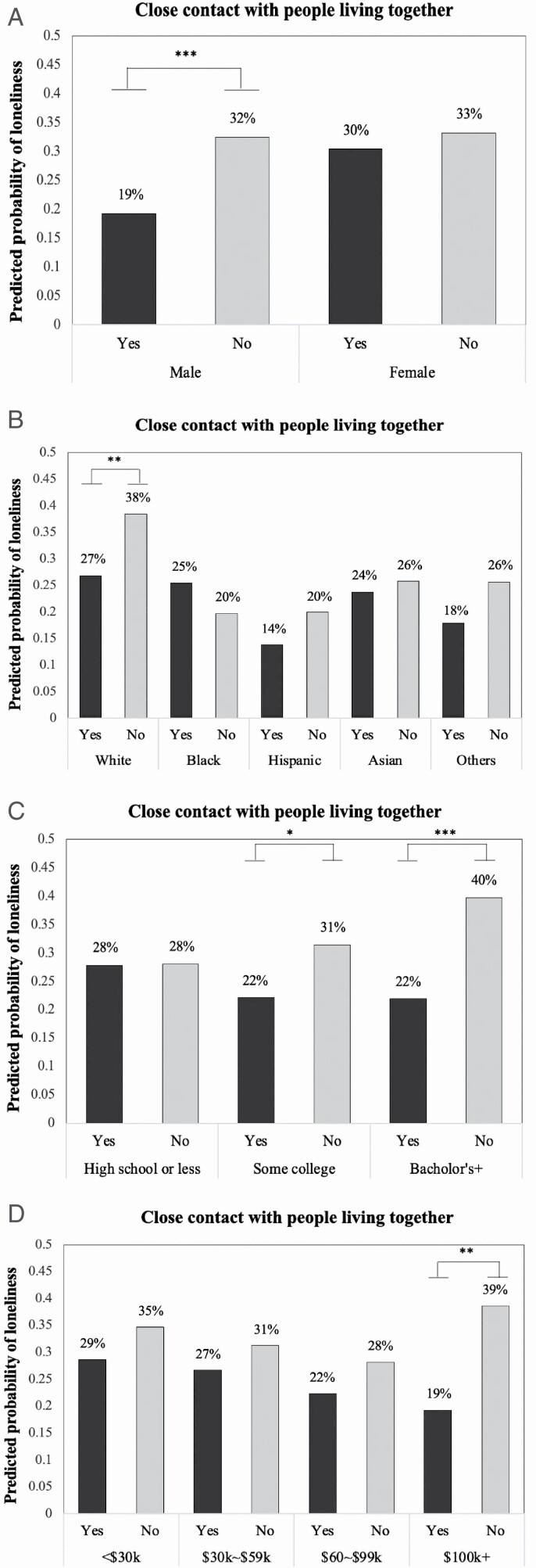
Interaction Effects by Sociodemographic Characteristics
Using the same modeling approach, we then examined interactions between sociodemographic characteristics and distancing measures on loneliness. We tested whether the strength of the associations of two social distancing measures shown to be related to loneliness in the previous model (i.e., canceling social activities and close contact with coresidents) differed by sociodemographic characteristics. Table 2 also presents statistically significant interaction effects (full model results are available upon request). No significant interaction effects were observed between canceling social activities and sociodemographic characteristics. However, there were a few notable interaction effects between close contact with people living together and sociodemographic characteristics: female (OR = 0.55, CI = 0.34−0.87, p < .05), Black (OR = 0.40, CI = 0.19−0.85, p < .05), high school or less education (OR = 0.40, CI = 0.23−0.71, p < .01), and household income of $30k−$59,999 (OR = 0.45, CI = 0.21−0.95, p < .05). To further explore the significant interaction terms, we plotted the predicted probabilities of loneliness and conducted post-hoc comparisons using contrasts. As shown in Figure 3, the effects of close contact with people living together were larger in males than females. Whereas the probability of reporting loneliness did not differ for females who had close contact or did not, males who had no close contact had a significantly greater probability of reporting loneliness than males who had contact (32% compared to 19%; χ 2 = 12.54, p < .001). Second, for race/ethnicity, whether having close contact with coresidents only had a statistically significant difference in loneliness for non-Hispanic Whites (χ 2 = 11.17, p < .01). The predicted probability for non-Hispanic Whites who reported no close contact was 38%, compared to 27% for non-Hispanic Whites who reported having close contact. Third, those with higher levels of education had larger increases in loneliness if they had no close contact with people living together (χ 2 = 18.14, p < .05 for college graduates and χ 2 = 21.19, p < .001 for those with bachelor’s degree). For example, the predicted probability for those with a bachelor’s degree who had no close contact was 40%, which was significantly greater than 22% among those who reported having close contact. Lastly, the effects of having no close contact with coresidents were stronger among people with higher levels of income. The respondents making more than $100k had a significantly greater probability of reporting loneliness if they had no close contact with coresidents than those who had close contact (39% compared to 19%; χ 2 = 12.44, p < .01).
Figure 3.
Predicted probability of loneliness by interactions between COVID-19-related social distancing measures and sociodemographic characteristics. (A) Gender differences. (B) Racial/ethnic group differences. (C) Education group differences. (D) Income group differences. Note: *p < .05. **p < .01. ***p < .001.
Supplementary Analyses
Given the wide range of ages of our sample and heterogeneous life situations between middle-aged and older adulthood (e.g., retirement, health status, and social network), it is important to examine whether the potential age differences exist in the association between social distancing measures and loneliness. To address this issue, we conducted sensitivity analyses by segregating the sample into the middle-aged group whose ages were between 50 and 64 and the older group aged 65 and older. As presented in Supplementary Table 1, we found some noteworthy differences between the age groups. Among those in the middle-aged group, canceling social activities were the only social distancing measures significantly associated with increased odds of loneliness (OR = 1.34, CI = 1.01−1.78, p < .05). However, among the older group, having no close contact with people living together significantly increased the odds of loneliness by 94% (OR = 1.94, CI = 1.20−3.16, p < .01).
Additionally, we conducted a sensitivity analysis using a cutoff of 3 days or more for feeling lonely (persistent feelings). Findings are presented in Supplementary Table 2. While canceling or postponing social activities remained significantly associated with loneliness (OR = 1.84, CI = 1.31−2.58, p < .001), avoiding close contact with people living together was no longer significant. Instead, avoiding public spaces, gatherings, or crowds was found to be associated with lower odds of loneliness (OR = 0.69, CI = 0.37−0.99, p < .05).
Discussion
In response to the COVID-19, the CDC and WHO guidelines proposed several social distancing measures, which include (a) avoiding public spaces, gatherings, or crowds; (b) canceling or postponing social activities; (c) social visits; and (d) close contact (within 6 feet) with others (CDC, 2020b; WHO, 2020). Health professionals identified older adults as a high-risk group early in the COVID-19 pandemic and advised them to follow recommended social distancing measures to reduce their chance of infection (Armitage & Nellums, 2020; Berg-Weger & Morley, 2020; Brooke & Jackson, 2020). These risk mitigation strategies may simultaneously be disturbing and limit older adults’ social connections. Drawing on the Social Psychology of Loneliness Theory and the Socioemotional Selectivity Theory, the current study hypothesized that the COVID-19 social distancing measures, particularly limiting close social interactions, would increase the risk of loneliness among older adults (Hypothesis 1) and that adhering to social distancing measures will have greater negative effects on loneliness for people with sociodemographic backgrounds that characterize lack of social resources and networks (Hypothesis 2).
With a nationally representative sample of adults aged 50 and older, we found evidence that canceling or postponing social activities and avoiding close contact with people living together are related to increased feelings of loneliness. This is in line with the attributional framework of the Social Psychology Theory of Loneliness, and in accordance with existing literature on older adults’ loneliness, which suggested that insufficient interpersonal contact and lack of social connection are strong risk factors for loneliness (Cohen-Mansfield et al., 2016; NASEM, 2020; Petersen et al., 2016). More relevant to COVID-19, previous empirical studies reported consistent findings that less contact with relatives and being under stay-at-home orders were associated with higher loneliness (Losada-Baltar et al., 2020; Tull et al., 2020). Importantly, we found that not all social distancing measures were related to loneliness: avoiding public spaces and social visits were not significant predictors of loneliness. This can be understood in line with the Socioemotional Selectivity Theory (Carstensen, 1995), positing that the quality of social interactions with significant others is more important than the quantity of contacts for older individuals. Our findings indicate that loneliness may be affected by social distancing behaviors disturbing close connectedness, but not so much by social distancing in public.
In addition to the direct effects of social distancing measures on loneliness, our study examined their interacting effects with sociodemographic characteristics. Having no close contact with coresidents had larger effects on feelings of loneliness for males (compared to females), non-Hispanic Whites (compared to other racial/ethnic groups), and those with higher levels of education and income. These findings emphasize the heterogeneous nature of COVID-19-related experiences across subpopulations of older adults, and in line with predisposing factors of loneliness suggested in the Social Psychology Theory of Loneliness. Previous studies have shown the vulnerability of males and non-Hispanic Whites to social isolation. Males tend to have weaker social ties than females (Arber et al., 2003), and they become more susceptible to social isolation after retirement (Davidson et al., 2003). In comparison to Blacks and Hispanics, non-Hispanic Whites have a greater risk of being isolated, partly due to racial/ethnic differences in social networks (Cudjoe et al., 2020). Blacks and Hispanics receive more social support from kin and family members, whereas non-Hispanics Whites are more involved in friendship ties (Ajrouch et al., 2001; Becker et al., 2003). It was notable that those with higher levels of education and income had greater increases in the probability of reporting loneliness if they had no close contact with people living together. These findings support previously suggested assumptions that the requirements of social distancing may also be detrimental to people without previous experience of social isolation because they may be unfamiliar and less prepared to cope with such circumstances (Brooke & Jackson, 2020; Miller, 2020). Our results call special attention to these certain groups who have been vulnerable to the risk of isolation and/or who have limited resources to cope with the adoption of social distancing behaviors.
Our findings have important policy implications for understanding the impact of social distancing on the psychological well-being of older adults. Efforts can be made by a variety of different actors. Social service providers and health care professionals should be aware of the pronounced negative effects of social distancing measures limiting social connections with close others. Technology-based interventions can facilitate older adults’ virtual communication with social network members. At a community level, intergenerational programs may help older neighbors in need of social contact (Morrow-Howell et al., 2020). Regular video or phone calls by volunteers can be an effective medium for homebound older persons to maintain social ties and reduce feelings of loneliness. From a clinical perspective, telemedicine consultations can be provided via outgoing calls, reaching out to vulnerable older adults, and conducting a phone screening for social isolation (Jawaid, 2020). However, it should be noted that these virtual options are not available to everyone, especially for individuals with a lack of human or financial resources (Baker et al., 2018). Therefore, policies should aim to address the digital divide by increasing the provision or reimbursement of technological devices as well as providing support for internet costs and connectivity. Moreover, in preparation for the post-COVID-19 era, professional mental health support should help older adults to reestablish social connections and resolve any lingering feelings of loneliness (Gaeta & Brydges, 2020).
We provide evidence that not all social distancing behaviors will have an equal impact across the older adult population. Instead, careful consideration should be given to how social distancing measures may create an uneven burden for the most vulnerable older adults. Programs and interventions should consider who is experiencing the most adverse impacts, and how to best serve those communities. In line with the recommendations for loneliness interventions by NASEM (2020), it is important to identify individuals at highest risk, understand their specific needs, and target the underlying factors causing loneliness. For example, our findings showed that avoiding close contact with people living together increased the probability of loneliness not only for those who were already at greater risk of being lonely (i.e., males and Whites), but also for people who were less likely to have previous experience of social isolation (i.e., those with higher levels of education and income). However, the nature of loneliness that they experience can be fundamentally different for the two groups—it may be more chronic for the former and more acute for the latter. More research is required to understand the underlying cause and how to best tailor intervention strategies for each group. Considering these key differences, policies and programs can reduce the risk of acquiring COVID-19 (or other future pandemics) for older adults, while not exacerbating disparities in psychological distress.
Our study has a few notable strengths. While other studies that assess the psychological impacts of social distancing measures have largely focused on community-based samples or aggregate in larger geographical units, our study uses a diverse, nationally representative sample, which allows more robust interpretation at the national level and a careful examination of population heterogeneity. Additionally, these data were collected during a key period of the pandemic, providing insight into the impact of behavioral change on psychological well-being as they occurred. Lastly, our focus on older adults provides some of the first insights into how social distancing practices during COVID-19 impacted this vulnerable group. But, importantly, we also explore variability among older adults to show the differential impact of social distancing measures among key subgroups that have become and will continue to be increasingly important as the older age population diversifies.
Limitations
Our study includes several limitations. First, we do not have information to evaluate the effect of social distancing practices on loneliness for older adults in assisted living facilities. Social distancing practices may be most severe and likely have the greatest impact on the loneliness of older adults in these residential care settings. While UAS may have included some residents of nursing homes because any person with a valid address could be included in the study, no available variable identifies nursing home residents. Second, we cannot account for the number of COVID-19 cases in the community in the current study. Older adults living in places with zero or few cases may not have felt they needed to engage in social distancing measures and may thus have been spared any of the potential negative psychosocial consequences of messaging related to, or adoption of, these measures. Third, the UAS first asked about loneliness at Wave 4, which corresponded to the end of April and early May. Loneliness may have increased more rapidly in an earlier period of the pandemic, such as when social distancing behaviors were first implemented, or close to the peak of the first wave when the perceived risk may have been greater. However, evidence from other COVID-19-specific studies suggests that this may not be the case: loneliness remained relatively stable throughout this brief period (Luchetti et al., 2020). Fourth, while the UAS provided internet and computers to residents to complete the surveys, the data may exclude older adults with low technology literacy or with a preventative disability who never consented to participate in the panel. Low literacy adults tend to be of lower socioeconomic status or racial/ethnic minorities. Given the large inclusion of people with lower socioeconomic status and of racial/ethnic minorities, we do not suspect that this exclusion to be large and systematic, having minimal impact on our results. Fifth, although we conducted the sensitivity analyses with two age groups (the middle-aged group vs the older group aged 65+), small sample sizes did not allow us to further examine any age group differences in the interaction effects between social distancing measures and sociodemographic characteristics. Future studies with a larger sample of each sociodemographic group would provide a better understanding of how social distancing measures are differently associated with loneliness depending on one’s age and other sociodemographic backgrounds. Lastly, due to data limitations, we used a single-item measure for loneliness. Thus, loneliness may be underreported and underestimated. Nevertheless, our more simplified measure of loneliness still showed a strong relationship with social distancing measures. However, we use caution in these interpretations. We do not claim any causal argument, given that these data are cross-sectional.
Conclusion
In conclusion, the current research addresses emerging concerns about the possible risks related to COVID-19 social distancing measures for older adults. Our findings showed that particular social distancing measures—canceling social activities and no close contact with people living together—were significantly associated with increased loneliness. While intended to protect vulnerable groups, social distancing measures may damage important individual–societal connections through negatively impacting social support, as observed for other disasters. This study draws awareness of this concern. In addition, the negative effects of avoiding close contact were more pronounced in certain subgroups of older adults (males, non-Hispanic Whites, people with higher levels of education, and those with higher incomes). These findings provide preliminary evidence that can be used to inform tailored intervention strategies to prevent the potential adverse effects of implementing social distancing measures, particularly for those who lack interpersonal resources and coping experiences.
Funding
This study was supported by funding from the National Institutes of Health National Institute on Aging (grant numbers T32-AG000037 and P30AG017265).
Conflict of Interest
None declared.
Supplementary Material
Acknowledgments
The current research draws data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research at the University of Southern California (USC). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or Understanding America Study (UAS). The collection of the UAS COVID-19 tracking data is supported in part by the Bill & Melinda Gates Foundation and by grant U01AG054580 from the National Institute on Aging.
Contributor Information
Eun Young Choi, Leonard Davis School of Gerontology, University of Southern California, Los Angeles, USA.
Mateo P Farina, Leonard Davis School of Gerontology, University of Southern California, Los Angeles, USA.
Qiao Wu, Leonard Davis School of Gerontology, University of Southern California, Los Angeles, USA.
Jennifer Ailshire, Leonard Davis School of Gerontology, University of Southern California, Los Angeles, USA.
Author Contributions
E. Y. Choi planned the study, performed statistical analyses, and wrote the paper. M. P. Farina and J. Ailshire helped to plan the study, including the instrumentation, and contributed to writing the paper. Q. Wu helped the data analysis and contributed to writing the paper.
References
- Ajrouch, K. J., Antonucci, T. C., & Janevic, M. R. (2001). Social networks among blacks and whites: The interaction between race and age. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56(2), S112–S118. doi: 10.1093/geronb/56.2.S112 [DOI] [PubMed] [Google Scholar]
- American Psychological Association . (2020). COVID-19 isn’t just a danger to older people’s physical health.https://www.apa.org/news/apa/2020/03/covid-19-danger-physical-health
- Arber, S., Davidson, K., & Ginn, J. (2003). Changing approaches to gender and later life. In Arber S., Davidson K., & Ginn J. (Eds.), Gender and ageing: changing roles and relationships (pp. 41–14). Open University Press. [Google Scholar]
- Armitage, R., & Nellums, L. B. (2020). The COVID-19 response must be disability inclusive. The Lancet. Public Health, 5(5), e257. doi: 10.1016/S2468-2667(20)30076-1-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker, S., Warburton, J., Waycott, J., Batchelor, F., Hoang, T., Dow, B., Ozanne, E., & Vetere, F. (2018). Combatting social isolation and increasing social participation of older adults through the use of technology: A systematic review of existing evidence. Australasian Journal on Ageing, 37(3), 184–193. doi: 10.1111/ajag.12572 [DOI] [PubMed] [Google Scholar]
- Becker, G., Beyene, Y., Newsom, E., & Mayen, N. (2003). Creating continuity through mutual assistance: Intergenerational reciprocity in four ethnic groups. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58(3), S151–S159. doi: 10.1093/geronb/58.3.s151 [DOI] [PubMed] [Google Scholar]
- Berg-Weger, M., & Morley, J. E. (2020). Loneliness and social isolation in older adults during the COVID-19 pandemic: Implications for gerontological social work. The Journal of Nutrition, Health & Aging, 24(5), 456–458. doi: 10.1007/s12603-020-1366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke, J., & Jackson, D. (2020). Older people and COVID-19: Isolation, risk and ageism. Journal of Clinical Nursing, 29(13–14), 2044–2046. doi: 10.1111/jocn.15274 [DOI] [PubMed] [Google Scholar]
- Carstensen, L. L. (1995). Evidence for a life-span theory of socioemotional selectivity. Current Directions in Psychological Science, 4(5), 151–156. doi: 10.1111/1467-8721.ep11512261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) . (2020a, February 11). Coronavirus disease 2019 (COVID-19). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html [Google Scholar]
- Centers for Disease Control and Prevention (CDC) . (2020b, April 24). Coronavirus disease 2019 (COVID-19)—Prevention & treatment. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html [Google Scholar]
- Chan, S. M. S., Chiu, F. K. H., Lam, C. W. L., Leung, P. Y. V., & Conwell, Y. (2006). Elderly suicide and the 2003 SARS epidemic in Hong Kong. International Journal of Geriatric Psychiatry, 21(2), 113–118. doi: 10.1002/gps.1432 [DOI] [PubMed] [Google Scholar]
- Cheung, Y. T., Chau, P. H., & Yip, P. S. (2008). A revisit on older adults suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong. International Journal of Geriatric Psychiatry, 23(12), 1231–1238. doi: 10.1002/gps.2056 [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield, J., Hazan, H., Lerman, Y., & Shalom, V. (2016). Correlates and predictors of loneliness in older adults: A review of quantitative results informed by qualitative insights. International Psychogeriatrics, 28(4), 557–576. doi: 10.1017/S1041610215001532 [DOI] [PubMed] [Google Scholar]
- Courtemanche, C., Garuccio, J., Le, A., Pinkston, J., & Yelowitz, A. (2020). Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Affairs (Project Hope), 39(7), 1237–1246. doi: 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- Cudjoe, T. K. M., Roth, D. L., Szanton, S. L., Wolff, J. L., Boyd, C. M., & Thorpe, R. J. (2020). The epidemiology of social isolation: National Health and Aging Trends Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(1), 107–113. doi: 10.1093/geronb/gby037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson, K., Daly, T., & Arber, S. (2003). Older men, social integration and organisational activities. Social Policy and Society, 2(2), 81–89. doi: 10.1017/S1474746403001118 [DOI] [Google Scholar]
- Dowd, J. B., Andriano, L., Brazel, D. M., Rotondi, V., Block, P., Ding, X., Liu, Y., & Mills, M. C. (2020). Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences of the United States of America, 117(18), 9696–9698. doi: 10.1073/pnas.2004911117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fokkema, T., De Jong Gierveld, J., & Dykstra, P. A. (2012). Cross-national differences in older adult loneliness. The Journal of Psychology, 146(1–2), 201–228. doi: 10.1080/00223980.2011.631612 [DOI] [PubMed] [Google Scholar]
- Gaeta, L., & Brydges, C. R. (2020). Coronavirus-related anxiety, social isolation, and loneliness in older adults in Northern California during the stay-at-home order. Journal of Aging & Social Policy. Advance online publication. doi: 10.1080/08959420.2020.1824541 [DOI] [PubMed] [Google Scholar]
- Green, L. R., Richardson, D. S., Lago, T., & Schatten-Jones, E. C. (2001). Network correlates of social and emotional loneliness in young and older adults. Personality and Social Psychology Bulletin, 27(3), 281–288. doi: 10.1177/0146167201273002 [DOI] [Google Scholar]
- Green, M. J., Whitley, E., Niedzwiedz, C. L., Shaw, R. J., & Katikireddi, S. V. (2020). Social contact and inequalities in depression and loneliness among older adults: A mediation analysis of the English Longitudinal Study of Ageing. medRxiv. doi: 10.1101/2020.07.01.20143990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley, L. C., & Cacioppo, J. T. (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huxhold, O., Miche, M., & Schüz, B. (2014). Benefits of having friends in older ages: Differential effects of informal social activities on well-being in middle-aged and older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(3), 366–375. doi: 10.1093/geronb/gbt029 [DOI] [PubMed] [Google Scholar]
- Hwang, T.-J., Rabheru, K., Peisah, C., Reichman, W., & Ikeda, M. (2020). Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics. Advance online publication. doi: 10.1017/S1041610220000988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jawaid, A. (2020). Protecting older adults during social distancing. Science (New York, N.Y.), 368(6487), 145. doi: 10.1126/science.abb7885 [DOI] [PubMed] [Google Scholar]
- Losada-Baltar, A., Jiménez-Gonzalo, L., Gallego-Alberto, L., Pedroso-Chaparro, M. del S., Fernandes-Pires, J., & Márquez-González, M. (2020). “We Are Staying at Home.” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e10–e16. doi: 10.1093/geronb/gbaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti, M., Lee, J. H., Aschwanden, D., Sesker, A., Strickhouser, J. E., Terracciano, A., & Sutin, A. R. (2020). The trajectory of loneliness in response to COVID-19. The American Psychologist, 75(7), 897–908. doi: 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon, D. P. (2008). Introduction to statistical mediation analysis. Lawrence Erlbaum Associates. [Google Scholar]
- Marziali, M. E., Card, K. G., McLinden, T., Wang, L., Trigg, J., & Hogg, R. S. (2020). Physical distancing in COVID-19 may exacerbate experiences of social isolation among people living with HIV. AIDS and Behavior. Advance online publication. doi: 10.1007/s10461-020-02872-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, G. (2020). Social distancing prevents infections, but it can have unintended consequences. Science | AAAS.https://www.sciencemag.org/news/2020/03/we-are-social-species-how-will-social-distancing-affect-us
- Morrow-Howell, N., Galucia, N., & Swinford, E. (2020). Recovering from the COVID-19 pandemic: A focus on older adults. Journal of Aging & Social Policy, 32(4–5), 526–535. doi: 10.1080/08959420.2020.1759758 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine (NASEM) . (2020). Social isolation and loneliness in older adults: Opportunities for the health care system. The National Academies Press. [PubMed] [Google Scholar]
- Peplau, L. A., & Perlman, D. (1979). Blueprint for a social psychological theory of loneliness. In Cook M. & Wilson G. (Eds.), Love and attraction: Proceedings of an International Conference (pp. 101–110). Pergamon. [Google Scholar]
- Peplau, L. A., & Perlman, D. (1982). Perspectives on loneliness. In Peplau L. A. & Perlman D. (Eds.), Loneliness: A sourcebook of current theory, research and therapy (pp. 1–18). Wiley. [Google Scholar]
- Petersen, J., Thielke, S., Austin, D., & Kaye, J. (2016). Phone behaviour and its relationship to loneliness in older adults. Aging & Mental Health, 20(10), 1084–1091. doi: 10.1080/13607863.2015.1060947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart, M., & Sorensen, S. (2001). Influences on loneliness in older adults: A meta-analysis. Basic and Applied Social Psychology, 23(4), 245–266. doi: 10.1207/S15324834BASP2304_2 [DOI] [Google Scholar]
- Pinquart, M., & Sörensen, S. (2003). Risk factors for loneliness in adulthood and old age—A meta-analysis. In Advances in psychology research (Vol. 19, pp. 111–143). Nova Science Publishers. [Google Scholar]
- Tull, M. T., Edmonds, K. A., Scamaldo, K. M., Richmond, J. R., Rose, J. P., & Gratz, K. L. (2020). Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Research, 289, 113098. doi: 10.1016/j.psychres.2020.113098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrrell, C. J., & Williams, K. N. (2020). The paradox of social distancing: Implications for older adults in the context of COVID-19. Psychological Trauma: Theory, Research, Practice and Policy, 12(S1), S214–S216. doi: 10.1037/tra0000845 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) . (2020). Coronavirus disease (COVID-19) advice for the public.World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. [Google Scholar]
- Yip, P. S., Cheung, Y. T., Chau, P. H., & Law, Y. W. (2010). The impact of epidemic outbreak: The case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis, 31(2), 86–92. doi: 10.1027/0227-5910/a000015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.