Abstract
Background
Emerging cross-sectional reports find that the COVID-19 pandemic and related social restrictions negatively affect lifestyle behaviours and mental health in general populations.
Aims
To study the longitudinal impact of COVID-19 on work practices, lifestyle and well-being among desk workers during shelter-at-home restrictions.
Methods
We added follow-up after completion of a clinical trial among desk workers to longitudinally measure sedentary behaviour, physical activity, sleep, diet, mood, quality of life and work-related health using validated questionnaires and surveys. We compared outcomes assessed before and during COVID-19 shelter-at-home restrictions. We assessed whether changes in outcomes differed by remote working status (always, changed to or never remote) using analysis of covariance (ANCOVA).
Results
Participants (N = 112; 69% female; mean (SD) age = 45.4 (12.3) years; follow-up = 13.5 (6.8) months) had substantial changes to work practices, including 72% changing to remote work. Deleterious changes from before to during shelter-at-home included: 1.3 (3.5)-h increase in non-workday sedentary behaviour; 0.7 (2.8)-point worsening of sleep quality; 8.5 (21.2)-point increase in mood disturbance; reductions in five of eight quality of life subscales; 0.5 (1.1)-point decrease in work-related health (P < 0.05). Other outcomes, including diet, physical activity and workday sedentary behaviour, remained stable (P ≥ 0.05). Workers who were remote before and during the pandemic had greater increases in non-workday sedentary behaviour and stress, with greater declines in physical functioning. Wake time was delayed overall by 41 (61) min, and more so in workers who changed to remote.
Conclusions
Employers should consider supporting healthy lifestyle and well-being among desk workers during pandemic-related social restrictions, regardless of remote working status.
Keywords: Diet, mood, pandemic, physical activity, sedentary behaviour, sleep, work-related health
Key learning points.
What is already known about this subject:
To limit transmission of COVID-19, governments enacted social restrictions that limited in-person work to essential workers.
In cross-sectional surveys of general adult populations, social restrictions related to COVID-19 are reported to have deleterious effects on lifestyle behaviours, such as more sedentary behaviour, less physical activity, reduced sleep quality and unhealthy eating, along with reduced mental health.
What this study adds:
During COVID-19, desk worker practices were profoundly impacted, including more sedentary/less active work, increased remote work and changes to the social and physical work environment such as less in-person interactions and less formal workstations.
Compared to approximately 1 year before the pandemic, desk workers tended to increase sedentary time and had reduced sleep quality, worse mood, decreased quality of life and decreased work-related health during the COVID-19 shelter-at-home period; yet, diet and physical activity did not change and typical wake time was delayed.
Contrary to our hypothesis that desk workers switching to remote work would have the greatest adverse changes, similar changes were observed across remote working categories (i.e. never, changed to or always) and, if anything, always remote workers had the greatest deleterious changes.
What impact this may have on practice or policy:
Employers should consider programmes or interventions to support healthy lifestyle and well-being among desk workers during pandemic-related social restrictions to maximize occupational health and performance.
These programmes should target all desk workers, regardless of remote working status.
Introduction
The COVID-19 pandemic has resulted in drastic social distancing measures. In Pittsburgh, PA, USA, a shelter-at-home mandate was in place from March through May of 2020, restricting non-essential activities to attenuate the spread of the novel coronavirus. Yet, among health behaviour researchers, there has been wide-spread speculation of potential adverse health impacts of such restrictions, including unfavourable changes to the 24-h activity cycle (less physical activity, more sitting, reduced sleep quality), more screen time and unhealthy eating and worsened mental health [1–3]. Indeed, initial evidence from cross-sectional and survey studies [4–10] has corroborated the occurrence of these adverse effects to health behaviours and well-being. However, longitudinal investigation of these unintended consequences of social restriction would strengthen conclusions.
In addition to population-level effects, social restrictions may have specific effects among desk workers. One consequence of shelter-at-home mandates was a shift to remote work for non-essential workers. Even as restrictions are loosened, remote work continues to be encouraged or required by many US companies and may remain so indefinitely [11]. This underscores that the significance of understanding the health effects of remote work practices is not limited to the effects of the COVID-19 pandemic response. Technology has changed the capabilities of conducting remote work by addressing most limitations; in fact, prior to the global pandemic, up to 87% of American workers reported that they would like to work remotely at least some of the time but only 20% reported working remotely one or more days per week [12]. As work is a major determinant of daily activity and social interaction [13,14], the effect of changing from in-office to remote work on lifestyle behaviours and well-being is an area in need of research.
To address these research questions, we leveraged a unique opportunity in the ongoing Reducing Sedentary Behaviour and Blood Pressure (RESET BP) randomized clinical trial. In this 3-month sedentary behaviour reduction intervention trial among desk workers, we had previously measured sedentary behaviour, moderate-to-vigorous intensity physical activity, sleep, diet, mood, quality of life and work health outcomes before social restrictions related to COVID-19 were instituted in the USA. We then repeated these assessments during the COVID-19 shelter-at-home period among participants who had already completed the trial. Our primary hypotheses were that the COVID-19 shelter-at-home restrictions would negatively affect self-reported health behaviours (sedentary behaviour, physical activity, sleep and diet) and well-being (mood, quality of life and work health). Further, using the natural variability in engagement in remote work during the shelter-at-home restrictions, we evaluated secondary hypotheses that desk workers changing to remote working status during the pandemic would experience greater changes in health behaviours and well-being compared to those with stable on-site or those already remote working statuses.
Methods
This natural experiment leveraged pre-existing ‘baseline’ data, collected upon completion of participation in the RESET BP trial (clinicaltrials.gov: NCT03307343). Beginning in January 2018, the RESET BP trial randomized desk workers with elevated, untreated blood pressure, who self-reported ≥20 h of deskwork and <150 min of moderate-to-vigorous intensity physical activity per week to either a 3-month multicomponent sedentary behaviour reduction intervention or a no-treatment control group. Final RESET BP trial measurements were considered baseline because these were the most recent data collected before COVID-19 and participants had completed participation in the intervention prior to this assessment. We conducted an additional survey from May to June 2020, during COVID-19 shelter-at-home in Pennsylvania, USA, in participants who had completed the trial; these data were considered ‘follow-up’.
RESET BP participants who had completed the trial were recontacted by study personnel and, if interested, provided informed consent, and completed the follow-up electronic survey. All procedures were approved by the University of Pittsburgh Human Research Protection Office. Of 134 participants invited, 112 consented to participate, were employed in February 2020 (immediately prior to the shelter-at-home period) and completed at least part of the follow-up survey (83%). With the rolling recruitment of the parent trial, average (SD) time between the pre-COVID-19 baseline and the COVID-19 follow-up was 13.5 (6.8) months.
Participants were asked to report employment characteristics immediately before (i.e. February 2020) and during COVID-19 shelter-at-home (i.e. at the time of survey data collection) to describe changes in work practices. These included work duration, work-time activity patterns and the social and physical environment of their workplace.
To collect harmonious data with other researchers studying the broad effects of COVID-19, we used the Epidemic-Pandemic Impacts Inventory (EPII) [4]. The EPII asks participants to report perceived personal and household impacts of the pandemic across a variety of domains, including work, education, home life, social activities, health, economic stability and positive changes. We summed the number of items reported within each domain and reported these as the mean and proportion of domain items. We further reported the prevalence of individual items within the four personal domains with the highest reported impact.
Lastly, longitudinal assessments conducted before and during COVID-19 shelter-at-home included self-reported lifestyle behaviours and well-being. Lifestyle behaviours were assessed by validated instruments, i.e. workday and non-workday sedentary behaviour measured by the Sedentary Behaviour Questionnaire [15]; moderate-to-vigorous intensity physical activity measured by the Paffenbarger Physical Activity Questionnaire [16]; and sleep quality, duration and timing by the Pittsburgh Sleep Quality Index [17]. Dietary habits were measured by the Diet Screener Questionnaire [18]. Well-being measures included validated instruments for health-related quality of life (Short Form (SF)-36 [19]), mood (Profile of Mood States [20]) and work health outcomes (Work and Health Questionnaire) [21].
We computed appropriate descriptive statistics (means and standard deviations for continuous data; frequencies and percentages for categorical data) to characterize the sample and summarize measures before and during COVID-19, as well as changes. We used paired samples t- and sign tests to assess statistical significance of paired continuous variables, McNemar tests for paired dichotomous variables and Bowker’s tests for paired categorical variables to assess significance of overall pre- to during COVID-19 change. To compare ‘before COVID-19’ to ‘during COVID-19’ changes in measures across the three groups defined by change in remote work practices (always: ≥50%; switched to: from <50 to ≥50%; never: <50% remote work), we fitted a series of analysis of covariance (ANCOVA) models with change in each measure as the dependent variable, group as the independent factor of interest and ‘before COVID-19’ value of the measure as a covariate. For heavily skewed moderate-to-vigorous intensity physical activity data, we used the non-parametric Kruskal–Wallis test. SAS version 9.4 (SAS Institute, Inc., Cary, NC) was used for statistical analyses.
Results
Participants were, on average, in their mid-40s and mostly female, white, non-Hispanic and had a college degree or higher (Table 1). Most participants had professional/managerial/technical jobs in academia or private industry. As a result of COVID-19, many participants continued full-time desk work, but most changed to remote work. A small proportion of participants reported reduced hours or more substantial work disruptions such as furlough or termination.
Table 1.
Participant characteristics (N = 112)
| Mean (SD) or n (%) | |
|---|---|
| Age | 45.4 (12.3) |
| Gender | |
| Male | 35 (31) |
| Female | 77 (69) |
| Racea | |
| White | 98 (88) |
| Black | 8 (7) |
| Asian | 8 (7) |
| Native American | 1 (1) |
| Pacific Islander | 1 (1) |
| Ethnicity | |
| Non-Hispanic | 109 (97) |
| Hispanic | 3 (3) |
| Education | |
| High school | 2 (2) |
| Vocational training or some college | 22 (20) |
| College graduate | 48 (43) |
| Postgraduate degree | 40 (36) |
| Job category | |
| Sales or service | 5 (5) |
| Clerical/administrative support | 28 (25) |
| Professional/managerial/technical | 72 (64) |
| Other | 7 (6) |
| Job industry | |
| Academia | 56 (50) |
| Industry | 53 (47) |
| Government | 3 (3) |
| Employment status during shelter-at-home | |
| Full-time, same location | 25 (22) |
| Full-time, changed to remote | 66 (59) |
| Reduced hours, same location | 1 (1) |
| Reduced hours, changed to remote | 6 (5) |
| Was laid off or furloughed, but now back | 1 (1) |
| Currently laid off/furloughed/terminated | 6 (5) |
| Other | 7 (6) |
aCould report more than one race.
Among participants with continued work, changes in work practices from before to during COVID-19 shelter-at-home are reported and statistically compared in Table 1 (available as Supplementary data at Occupational Medicine Online). Only typical work duration (~8 h per day), frequency of taking a structured lunch break (median was ‘about half the time’) and proportion of time spent in heavy physical duties (2%) remained unchanged. From before to during COVID-19 shelter-at-home, more participants reported a flexible work schedule (55 to 70%, P < 0.01) and the option to work from home (28 to 91%, P < 0.001). The proportion of work that was performed remotely increased from 16 to 84% (P < 0.001). Work activity also differed significantly, including more sedentary work (more sitting, less standing and less light physical duties, all P < 0.001), less in-person, face-to-face interactions and more remote, face-to-face interactions (both P < 0.001), reduced interactions with friends during or after work (both P < 0.001) and a higher likelihood of leaving one’s desk during lunch (P < 0.05). Participants’ office environment also differed from before to during shelter-at-home; most notably, 2% versus 38% reported no formal workstation and 64% versus 15% reported having a height-adjustable workstation (both P < 0.001).
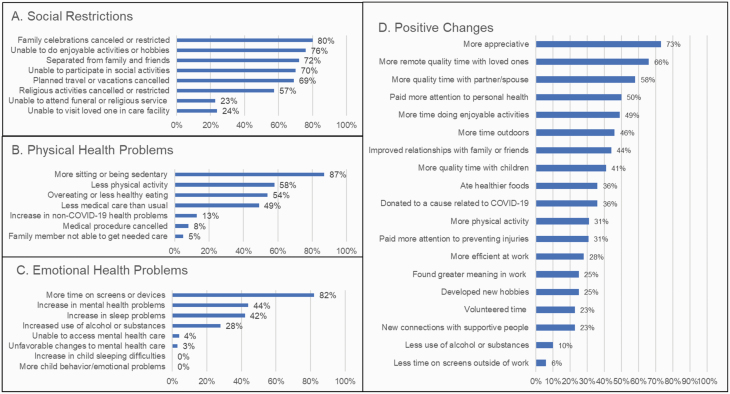
Participant-reported pandemic-related hardships for self and household are summarized by domain in Table 2 (available as Supplementary data at Occupational Medicine Online). For self, the highest proportion of hardships was reported for social (mean 4.9 of 10 items, 49%), physical health (mean 2.7 of 8 items, 34%) and emotional/well-being (mean 2.0 of 8 items, 25%) domains. For household, similar hardship domains were most frequent, though scores were lower. Positive changes were also commonly reported (e.g. for self, mean 7.0 of 19 items, 37%). Figure 1 reports the frequency of individual hardships (ranked from highest to lowest) among the four domains with the highest proportional scores. The most common social restrictions were cancellations (events or vacations), inability to do activities (hobbies or social) and separation from family and friends. Physical health problems most reported were sitting more, less physical activity, less healthy eating and reduced medical care. An increase in screen time was the most reported hardship in the emotional health domain. Positive changes reported by at least half of participants included being more appreciative, more quality time with loved ones and increased attention to personal health.
Figure 1.
Pandemic impacts reported by desk workers on self in the social restrictions (A), physical health problems (B), and emotional health problems (C) domains as well as positive changes (D).
From our longitudinal analysis comparing data collected before versus during the COVID-19 shelter-at-home, participants experienced several statistically significant changes (P < 0.05) in lifestyle parameters (Table 2). Participants increased sedentary behaviour during non-workdays, though sedentary behaviour during workdays and moderate-to-vigorous intensity physical activity did not change. Sleep quality, both the global score and its factor score, was worsened, though sleep duration and other factors were unchanged. Typical wake time was significantly delayed, while bedtime did not change. Dietary habits were largely unchanged, except for a reduced frequency of eating red meat during shelter-at-home.
Table 2.
Longitudinal impact of the COVID-19 pandemic on sedentary behaviour, physical activity, sleep and dietary habits
| Before shelter-at-home | During shelter-at-home | Change | P-value | |
|---|---|---|---|---|
| Sedentary behavioura | ||||
| Workday, h/day | 10.9 (3.8) | 11.3 (4.3) | 0.5 (4.4) | NS |
| Non-workday, h/day | 7.5 (3.6) | 8.7 (4.1) | 1.3 (3.5) | <0.001 |
| Physical activityb | ||||
| Moderate activity, min/week | 70 [30, 120] | 90 [10, 150] | 0 [−50, 70] | NS |
| Vigorous activity, min/week | 0 [0, 0] | 0 [0, 0] | 0 [0, 0] | NS |
| Moderate-to-vigorous activity, min/week | 80 [30, 150] | 95 [20, 180] | 0 [−60, 90] | NS |
| Sleepc | ||||
| Global sleep quality, pts | 5.0 (3.1) | 5.7 (3.5) | 0.7 (2.8) | <0.05 |
| Sleep efficiency factor, pts | 0.9 (1.2) | 1.1 (1.3) | 0.1 (1.2) | NS |
| Sleep quality factor, pts | 2.2 (1.9) | 2.5 (2.0) | 0.4 (1.6) | <0.05 |
| Daily disturbance factor, pts | 1.9 (0.9) | 2.1 (1.2) | 0.2 (1.1) | NS |
| Sleep duration, h | 6.7 (1.0) | 6.9 (1.0) | 0.2 (0.9) | NS |
| Bed time, hh:mm (min) | 10:47 p.m. (69) | 10:52 p.m. (80) | 7 (56) | NS |
| Wake time, hh:mm (min) | 06:20 a.m. (67) | 7:02 a.m. (82) | 41 (61) | <0.001 |
| Dietary habitsd | ||||
| Fruits and vegetables, cups/day | 2.6 (0.8) | 2.5 (0.7) | −0.1 (0.6) | NS |
| Added sugars, tsp/day | 14.9 (4.4) | 15.1 (5.1) | 0.1 (3.5) | NS |
| Sugars from sugar-sweetened beverages, tsp/day | 5.6 (3.3) | 5.8 (3.5) | 0.1 (1.9) | NS |
| Dairy, cup/day | 1.5 (0.6) | 1.6 (0.5) | 0.0 (0.4) | NS |
| Whole grains, oz/day | 0.8 (0.4) | 0.8 (0.3) | −0.0 (0.3) | NS |
| Calcium, mg/day | 961 (201) | 958 (175) | 2 (123) | NS |
| Fibre, g/day | 16.7 (3.5) | 16.4 (3.3) | −0.3 (2.3) | NS |
| Red meat, times/week | 2.5 (2.2) | 2.0 (1.5) | −0.4 (1.6) | <0.01 |
| Processed meat, times/week | 1.5 (1.9) | 1.5 (1.5) | −0.1 (1.8) | NS |
Data are reported as mean (SD), median [25th, 75th percentile] or time (hh:mm). Measured by the aSedentary Behaviour Questionnaire [15], the bPaffenbarger Physical Activity Questionnaire [16], the cPittsburgh Sleep Quality Index [17] and the dDiet Screener Questionnaire [18]. Before shelter-at-home N = 111; during shelter-at-home N = 100–104; change N = 99–103.
Statistically significant longitudinal changes were observed for mood, quality of life and work health (Table 3). Total mood disturbance increased significantly, reflecting unfavourable changes in subscales of anger, depression, esteem-related affect, vigour and confusion (all P < 0.05). For quality of life, pain, social functioning, emotional well-being, emotional role limitations and energy/fatigue all worsened significantly while general health and physical health subscales were unchanged. The overall work health score worsened, reflecting unfavourable changes in subscales of productivity, concentration and satisfaction (work, personal life and supervisor) (all P < 0.05). Notably, the impatience/irritability subscale and stress did not change significantly (P > 0.05).
Table 3.
Longitudinal impact of the COVID-19 pandemic on mood, quality of life and work health
| Before shelter-at-home | During shelter-at-home | Change | P-value | |
|---|---|---|---|---|
| Mood disturbancea | ||||
| Total mood disturbance, pts | −6.0 (19.9) | 2.2 (25.3) | 8.5 (21.2) | <0.001 |
| Tension subscale, pts | 5.7 (5.1) | 6.7 (5.9) | 1.0(5.5) | NS |
| Anger subscale, pts | 4.1 (3.8) | 5.0 (5.0) | 1.0 (4.5) | <0.05 |
| Fatigue subscale, pts | 5.3 (4.3) | 5.8 (4.7) | 0.5 (4.2) | NS |
| Depression subscale, pts | 2.2 (3.2) | 3.5 (4.3) | 1.5 (3.9) | <0.001 |
| Esteem-related affect subscale, pts | 14.9 (2.5) | 13.9 (2.8) | −1.1 (2.6) | <0.001 |
| Vigour subscale, pts | 11.6 (4.2) | 10.3 (5.1) | −1.4 (4.9) | <0.01 |
| Confusion subscale, pts | 3.3 (2.9) | 4.3 (3.5) | 1.1 (2.7) | <0.001 |
| Quality of lifeb | ||||
| General health, pts | 70.5 (15.1) | 69.9 (16.5) | −1.0 (12.0) | NS |
| Physical functioning, pts | 92.1 (14.5) | 91.7 (16.0) | 0.1(18.4) | NS |
| Role limitations due to physical health, pts | 93.7 (22.5) | 88.1 (26.4) | −5.6 (29.8) | NS |
| Pain, pts | 87.1 (14.7) | 81.7 (18.1) | −5.1 (14.7) | <0.001 |
| Emotional well-being, pts | 77.5 (14.8) | 71.4 (17.9) | −6.9 (16.0) | <0.001 |
| Social functioning, pts | 90.5 (17.4) | 84.1 (19.4) | −6.8 (22.4) | <0.01 |
| Role limitations due to emotional health, pts | 87.4 (26.2) | 74.8 (36.2) | −14.9 (37.0) | <0.001 |
| Energy/fatigue, pts | 57.6 (17.9) | 54.5 (19.6) | −3.6 (17.2) | <0.05 |
| Work healthc | ||||
| Total work health score, pts | 7.6 (1.1) | 7.3 (1.3) | −0.5 (1.1) | <0.001 |
| Productivity subscale, pts | 7.4 (1.2) | 7.1 (1.6) | −0.4 (1.2) | <0.01 |
| Impatience/irritability subscale, pts | 8.1 (1.7) | 8.2 (1.8) | 0.1 (1.9) | NS |
| Concentration/focus subscale, pts | 7.9 (1.9) | 7.6 (2.0) | −0.4 (1.7) | <0.05 |
| Work satisfaction subscale, pts | 7.2 (1.4) | 6.7 (1.8) | −0.6 (1.0) | <0.01 |
| Satisfaction with supervisor subscale, pts | 7.7 (2.1) | 7.2 (2.4) | −0.7 (2.7) | <0.05 |
| Personal life satisfaction subscale, pts | 8.0 (1.6) | 7.3 (2.1) | −0.8 (2.0) | <0.001 |
| Stress (single item), pts | 4.9 (2.5) | 4.7 (2.7) | −0.2 (3.1) | NS |
A secondary objective was to evaluate whether changes in remote working status altered the longitudinal impact of the COVID-19 pandemic on desk worker outcomes using ANCOVA. Thus, changes from pre- to during COVID-19 shelter-at-home were compared across participants by the following remote work status categories: always remote (n = 15), changed to remote (n = 74) and never remote (n = 14). Follow-up time and demographic characteristics (age, gender, race/ethnicity, education) were similar across categories (all P > 0.05). For sedentary behaviour, physical activity and sleep (Table 4), few changes from pre- to during shelter-at-home were statistically different across remote work categories. Increases in non-workday sedentary behaviour were highest in the ‘always remote’ category (P < 0.05) and wake times were most prominently shifted later in workers who changed to remote (P < 0.01). Similarly, few differences in pandemic-related changes were observed across remote work categories for mood, quality of life or work health (Table 5). ‘Always remote’ participants reported greater declines in physical functioning (P < 0.01) along with greater increases in stress (P < 0.05).
Table 4.
Longitudinal changes in on sedentary behaviour, physical activity, sleep and dietary habits by remote working category
| Always remote (n = 15) | Changed to remote (n = 74) | Never remote (n = 14) | P-value | |
|---|---|---|---|---|
| Sedentary behavioura | ||||
| Workday, h/day | 0.8 (6.9) | 0.5 (4.0) | 0.5 (4.1) | NS |
| Non-workday, h/day | 2.6 (4.9) | 0.9 (2.7) | 1.3 (3.2) | <0.05 |
| Physical activityb | ||||
| Moderate activity, min/week | −5 [60, 180] | 0 [−60, 65] | 0 [0, 45] | NS |
| Vigorous activity, min/week | 0 [0, 0] | 0 [0, 0] | 0 [0, 0] | NS |
| Moderate-to-vigorous activity, min/week | 35 [−60, 180] | 10 [−64, 90] | 0 [0, 45] | NS |
| Sleepc | ||||
| Global sleep quality, pts | 1.4 (3.0) | 0.6 (2.9) | 0.3 (1.8) | NS |
| Sleep efficiency factor, pts | 0.5 (1.6) | −0.0 (1.2) | 0.3 (1.3) | NS |
| Sleep quality factor, pts | 0.5 (1.9) | 0.4 (1.7) | −0.2 (1.1) | NS |
| Daily disturbance factor, pts | 0.5 (1.0) | 0.2 (1.1) | 0.1 (1.0) | NS |
| Sleep duration, min | −0 (48) | 18 (60) | −12 (42) | NS |
| Bed time, min | 2 (37) | 14 (52) | −7 (60) | NS |
| Wake time, min | 24 (36) | 48 (54) | 2 (53) | <0.01 |
| Dietary habitsd | ||||
| Fruits and vegetables, cups/day | −0.1 (0.6) | −0.1 (0.7) | −0.1 (0.4) | NS |
| Added sugars, tsp/day | −0.0 (4.5) | 0.0 (3.5) | 0.7 (3.1) | NS |
| Sugars from sugar-sweetened beverages, tsp/day | 0.7 (1.4) | 0.1 (2.0) | −0.5 (1.8) | NS |
| Dairy, cup/day | −0.0 (0.8) | 0.0 (0.4) | 0.0 (0.3) | NS |
| Whole grains, oz/day | −0.0 (0.2) | −0.0 (0.3) | −0.1 (0.3) | NS |
| Calcium, mg/day | −12 (212) | 4.2 (114) | 10 (70) | NS |
| Fibre, g/day | −0.6 (1.7) | −0.2 (2.5) | −0.9 (1.9) | NS |
| Red meat, times/week | −1.0 (2.1) | −0.4 (1.5) | 0.0 (1.8) | NS |
| Processed meat, times/week | −0.1 (1.3) | −0.1 (1.8) | −0.3 (2.5) | NS |
Table 5.
Longitudinal changes in mood, quality of life and work health by remote working category
| Always remote (n = 15) | Changed to remote (n = 74) | Never remote (n = 14) | P-value | |
|---|---|---|---|---|
| Mood disturbancea | ||||
| Total mood disturbance, pts | 15.7 (29.0) | 8.4 (21.1) | 6.0 (11.1) | NS |
| Tension subscale, pts | 1.4 (6.5) | 1.2 (5.6) | −0.3 (3.9) | NS |
| Anger subscale, pts | 1.5 (4.8) | 1.4 (4.8) | −0.2 (2.4) | NS |
| Fatigue subscale, pts | 2.5 (5.0) | 0.1 (4.1) | 0.8 (3.8) | NS |
| Depression subscale, pts | 3.3 (6.6) | 1.4 (3.6) | 0.3 (2.1) | NS |
| Esteem-related affect subscale, pts | −1.5 (3.0) | −1.1 (2.6) | −1.2 (2.0) | NS |
| Vigour subscale, pts | −2.1 (6.6) | −1.0 (4.6) | −3.7 (3.7) | NS |
| Confusion subscale, pts | 1.8 (2.9) | 1.1 (2.8) | 0.6 (1.4) | NS |
| Quality of lifeb | ||||
| General health, pts | −0.8 (13.2) | −0.7 (12.4) | −3.8 (8.0) | NS |
| Physical functioning, pts | −14.6 (31.3) | 3.0 (15.2) | −3.1 (10.7) | <0.01 |
| Role limitations due to physical health, pts | −1.9 (37.4) | −2.1 (24.7) | −15.4 (37.6) | NS |
| Pain, pts | −2.7 (10.6) | −5.6 (15.9) | −4.4 (13.4) | NS |
| Emotional well-being, pts | −2.0 (20.8) | −7.5 (15.2) | −4.3 (15.9) | NS |
| Social functioning, pts | −6.7 (33.7) | −7.6 (18.7) | 0.0 (29.8) | NS |
| Role limitations due to emotional health, pts | −10.3 (43.9) | −14.3 (35.7) | −19.4 (26.4) | NS |
| Energy/fatigue, pts | −6.7 (22.1) | −1.8 (16.1) | −9.2 (18.2) | NS |
| Work healthc | ||||
| Total work health score, pts | −0.4 (1.2) | −0.5 (1.1) | −0.5 (0.9) | NS |
| Productivity subscale, pts | −0.2 (1.6) | −0.4 (1.1) | −0.5 (1.0) | NS |
| Impatience/irritability subscale, pts | −0.5 (1.3) | 0.2 (2.0) | −0.2 (1.6) | NS |
| Concentration/focus subscale, pts | −0.9 (2.2) | −0.4 (1.6) | −0.3 (1.2) | NS |
| Work satisfaction subscale, pts | −0.1 (2.3) | −0.7 (1.8) | −0.4 (1.7) | NS |
| Satisfaction with supervisor subscale, pts | 0.7 (3.4) | −1.0 (2.7) | −0.2 (1.5) | NS |
| Personal life satisfaction subscale, pts | −1.4 (2.4) | −0.8 (1.8) | −0.4 (2.3) | NS |
| Stress (single item), pts | 2.1 (3.6) | −0.6 (2.9) | −0.4 (2.9) | <0.05 |
Discussion
In this natural experiment that added a follow-up assessment among desk workers who had completed a clinical trial, we aimed to evaluate the immediate impact of COVID-19 shelter-at-home on health behaviours and well-being. We found that, though most participants remained in full-time employment, their daily work experiences and personal lives changed substantially. Changes included more remote work at less formal workstations, reduced in-person social interactions during work and leisure time and health behaviour changes that were both negative (e.g. increased sitting and screen time) and positive (e.g. paying more attention to personal health). Using validated questionnaires with an average 13.5-month follow-up interval, we confirmed our hypotheses that the restrictions implemented due to the pandemic would negatively impact health behaviours and well-being. Negative impacts included more sedentary behaviour on non-workdays, reduced sleep quality, increased mood disturbance, reduced quality of life and reduced work health. While no dietary habits were found to worsen, red meat consumption was reduced; this could reflect reduced local meat availability during the COVID-19 survey period. Importantly, some factors did not worsen from pre- to during the COVID-19 shelter-at-home including lifestyle behaviours (e.g. workday sedentary behaviour, physical activity and most diet habits) and some subscales of mood (e.g. fatigue), quality of life (e.g. general health) and work health (e.g. stress). Moreover, contrary to our hypotheses, a change to remote work was not associated with worse changes in health behaviours and well-being. Few differences were observed across remote working categories and these indicated, if anything, that workers who were already remote and remained so experienced the greatest negative impact from the pandemic. Wake time was shifted significantly later among workers who switched to remote work, which could be viewed as a positive change resulting from commuting time no longer curtailing workday sleep [22].
The current study is strengthened by our longitudinal design that capitalized on previously collected, validated instruments measuring lifestyle and well-being to measure the impact of the COVID-19 pandemic during the initial shelter-at-home period. Weaknesses include the small, homogenous sample of desk workers with elevated blood pressure who were previously enrolled in a randomized clinical trial to reduce sedentary behaviour. Though this may limit generalizability, this sample provides detailed insight into desk workers’ unique experiences during this pandemic and likely improves the validity of our comparisons across remote working categories. A significant study limitation is that the effect of previous participation in the sedentary behaviour reduction intervention (either in the active intervention or control group) on our findings is difficult to estimate, though the impact is likely attenuated by using data collected after completing study participation as the baseline assessment. We speculate this likely increased awareness of sedentary behaviour and access to height-adjustable workstations before the pandemic, since all participants were offered a sit-stand desk attachment or monetary compensation at the end of the study. As such, our results may be most generalizable to desk workers with access to a sit-stand desk in the workplace. We expect there would have been limited effects on other outcomes. Also, though we used validated questionnaires, the follow-up self-report assessments of sedentary behaviour, physical activity, sleep and diet measures are known to suffer from biases such as social desirability or poor recall and this could have affected findings.
There have been multiple reviews and commentaries speculating that the COVID-19 pandemic could have detrimental effects on health behaviours and well-being [3], though fewer studies have measured these effects. Cross-sectional data from the USA [4] and Australia [5] suggest that the changes in health behaviours such as increased sitting and unhealthy eating, less physical activity, and reduced sleep quality and mental health reported by our participants are consistent with general populations. One longitudinal study used a convenience sample from a smartphone app across 187 countries and reported daily steps declined by 27.3% within 30 days of the global pandemic [9]. Survey studies from Europe also suggest sleep timing shifted later and sleep quality worsened during COVID-19 social restrictions [6,10]. Survey studies from the USA [7] and UK [8] using sampling weights to yield comparable pre- and post-COVID-19 samples reported marked increases in psychological distress. Taken together, our findings are consistent with the available research, though our study is the first to our knowledge that specifically studies the experiences of desk workers and thus provides novel, longitudinal data in this population.
Our findings offer two important implications for policymakers. First, desk workers are suffering from pandemic-related adverse effects and, from our longitudinal data, these include more sitting, reduced sleep quality and unfavourable changes in mood, emotional well-being, productivity, concentration and work/life satisfaction. As these factors are associated with work performance and long-term health [23], it is in the best interest of employers to recognize and offer support to counteract these effects. Second, desk workers shifting to remote work did not have more pronounced adverse effects on lifestyle and well-being. Though only speculation, our finding that remote workers remaining remote had the worst changes to lifestyle behaviours and well-being could be a result of greater disruptions in the household and in workflow during shelter-at-home. We did not collect information on changes in extra-occupational duties, or cohabitation by children, partners, other family or housemates during the shelter-at-home, which could have had complex effects on the work, lifestyle and well-being outcomes we measured. These mechanisms should be considered in future research. While longer-term and additional studies of remote work are needed to confirm these results are durable and occur in the absence of a concurrent pandemic, these data offer preliminary evidence that a shift to remote work does not necessarily lead to an unhealthy lifestyle with reduced well-being.
Important occupational health research questions remain regarding the COVID-19 pandemic, associated changes in work practices, and their impact on health behaviours and well-being. While our study found that adverse impacts experienced by desk workers during the COVID-19 pandemic were not more apparent in those changing from in-office to remote work as we hypothesized, we measured short-term effects experienced during a shelter-at-home period of a novel pandemic. It is possible that this complex situation could have obscured adverse impacts of more remote work; therefore, long-term study of the health effects of remote working remains important. Future investigations should continue to capture longitudinal data that establish temporality, but also use more rigorous assessment methodologies (e.g. objective assessment of sedentary behaviour, physical activity and sleep), and include clinical or healthcare utilization outcomes (e.g. weight, blood pressure, glucose, medication use). Such data will inform best practices for programming to support occupational and general health among remote desk workers.
In conclusion, our research provides critical, longitudinal evidence that the COVID-19 shelter-at-home policies profoundly and negatively affected daily life, lifestyle behaviours and well-being among desk workers. Despite this overall effect, desk workers who switched to remote work during the follow-up period did not have worse experiences compared to desk workers remaining in-office or remaining remote. These data suggest that employers should consider support for all desk workers to improve lifestyle behaviours and well-being during pandemic-related social restrictions, regardless of remote or in-office status.
Funding
This research was supported by the National Institutes of Health (R01 HL147610, R01 HL134809 and P30 AG024827).
Competing interests
None declared.
Supplementary Material
Acknowledgements
We thank research associates Melissa Jones, Mara Egeler and Shannon McAdoo for their diligent work on this time-sensitive project.
References
- 1. Altena E, Baglioni C, Espie CAet al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res 2020;29:e13052. [DOI] [PubMed] [Google Scholar]
- 2. Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: how will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis 2020: S0033-0620(20)30077–3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mattioli AV, Sciomer S, Cocchi C, Maffei S, Gallina S. Quarantine during COVID-19 outbreak: changes in diet and physical activity increase the risk of cardiovascular disease. Nutr Metab Cardiovasc Dis 2020;30:1409–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grasso DJ, Briggs-Gowan MJ, Ford JD, Carter AS. The Epidemic–Pandemic Impacts Inventory (EPII). University of Connecticut School of Medicine, 2020.
- 5. Stanton R, To QG, Khalesi Set al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health 2020;17:4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res 2020;29:e13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. J Am Med Assoc 2020;324:93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pierce M, Hope H, Ford Tet al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020;7:883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tison GH, Avram R, Kuhar Pet al. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann Intern Med 2020;173:767–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Blume C, Schmidt MH, Cajochen C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr Biol 2020;30:R795–R797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bloom N. How working from home works out. Institute for Economic Policy Research (SIEPR) Policy Brief. June 2020. [Google Scholar]
- 12. Kate L, Tom H. Telework and its effects in the United States. In: Messenger JC, ed. Telework in the 21st Century. Cheltenham, UK: Edward Elgar Publishing, 2019; 128–170. [Google Scholar]
- 13. Mullane SL, Toledo MJL, Rydell SAet al. Social ecological correlates of workplace sedentary behavior. Int J Behav Nutr Phys Act 2017;14:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Quinn TD, Pettee Gabriel K, Siddique Jet al. Sedentary time and physical activity across occupational classifications. Am J Health Promot 2020;34:247–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. J Phys Act Health 2010;7:697–705. [DOI] [PubMed] [Google Scholar]
- 16. Ainsworth BE, Leon AS, Richardson MT, Jacobs DR, Paffenbarger RS Jr. Accuracy of the college alumnus physical activity questionnaire. J Clin Epidemiol 1993;46:1403–1411. [DOI] [PubMed] [Google Scholar]
- 17. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 18. Thompson FE, Midthune D, Subar AF, McNeel T, Berrigan D, Kipnis V. Dietary intake estimates in the national health interview survey, 2000: methodology, results, and interpretation. J Am Diet Assoc 2005;105:352–363; quiz 487. [DOI] [PubMed] [Google Scholar]
- 19. Hollingworth W, Deyo RA, Sullivan SD, Emerson SS, Gray DT, Jarvik JG. The practicality and validity of directly elicited and SF-36 derived health state preferences in patients with low back pain. Health Econ 2002;11:71–85. [DOI] [PubMed] [Google Scholar]
- 20. Curran SL, Andrykowski MA, Studts JL. Short form of the profile of mood states (POMS-SF): psychometric information. Psychol Assess 1995;7:80. [Google Scholar]
- 21. Shikiar R, Halpern MT, Rentz AM, Khan ZM. Development of the Health and Work Questionnaire (HWQ): an instrument for assessing workplace productivity in relation to worker health. Work 2004;22:219–229. [PubMed] [Google Scholar]
- 22. Basner M, Fomberstein KM, Razavi FMet al. American time use survey: sleep time and its relationship to waking activities. Sleep 2007;30:1085–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cooper C, Dewe P. Well-being—absenteeism, presenteeism, costs and challenges. Occup Med (Lond) 2008;58:522–524. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.