Abstract
A significant number of coronavirus disease SARS-CoV-2 (COVID-19) patients continue to have symptoms related to COVID-19 after the acute phase of illness. This post-COVID condition is sometimes called ‘post-COVID syndrome’, ‘long COVID’ or ‘post-acute COVID-19’. Persistent psychiatric symptoms among COVID-19 survivors such as depression, anxiety, post-traumatic symptoms and cognitive impairment may be related to psychological factors and neurobiological injury. COVID-19 related neurological symptoms including anosmia, ageusia, dizziness, headache and seizures may persist for a long time after the acute COVID-19 illness. Many COVID-19 survivors experience persistent physical symptoms such as cough, fatigue, dyspnea and pain after recovering from their initial illness. There is a high probability that symptoms of psychiatric, neurological and physical illnesses, as well as inflammatory damage to the brain in individuals with post-COVID syndrome increase suicidal ideation and behavior in this patient population. COVID-19 survivors without post-COVID syndrome may also be at elevated suicide risk. Studies of suicidality in COVID-19 survivors are urgently needed and will be a new area of suicide research. An appropriate management of psychiatric, neurological and medical conditions may reduce suicide risk among COVID-19 survivors with or without post-COVID syndrome.
Introduction
The coronavirus disease SARS-CoV-2 (COVID-19) pandemic began in China in 2019 and quickly spread around the world.1,2 The public health, economic, social and emotional impact of the pandemic is enormous.1,2 By the time of writing of this article, more than 72 million people around the world were infected with COVID-19, and more than 1.6 million people died of COVID-19.3 The uncertainty about the path, duration, extent and effect of the pandemic could lead to the global recession which will probably be long lasting, with no country escaping its impact.
Over the course of the illness, many individuals with COVID-19 experience fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting and diarrhea.1 Severe COVID-19 infections requiring hospitalization may involve acute respiratory distress syndrome (ARDS), acute cardiac events, shock and multiorgan failure.
Lately, observations have emerged that a significant number of COVID-19 patients continue to have symptoms related to COVID-19 after the acute phase of illness.4,5 According to the UK COVID Symptom Study, about 10% of patients who have tested positive for the COVID-19 virus continue to be sick beyond 3 weeks, and a smaller percentage for months.4 This post-COVID condition is not clearly defined. It is sometimes called ‘post-COVID syndrome’, ‘long COVID’ or ‘post-acute COVID-19 syndrome’.5 It has been proposed to define post-acute covid-19 as extending beyond 3 weeks from the onset of first symptoms and chronic covid-19 as extending beyond 12 weeks.5 We need to attend to these growing longer-term medical and psychosocial consequences of COVID-19.
Psychiatric issues
Persistent psychiatric disorders among COVID-19 survivors may be related to psychological factors and neurobiological injury.6,7 In many cases, it is probably difficult to separate the impact of psychological factors from neurobiological effects.
Multiple lines of evidence suggest that the psychiatric sequelae of a coronavirus disease are a significant clinical challenge.2,4,5 A study of psychiatric consequences of SARS-COV-1 performed at 31–50 months after the infection demonstrated an occurrence of 54.5% of posttraumatic stress disorder (PTSD), 39% of depression, 32.5% of panic disorder and 15.6% of obsessive–compulsive disorder, a tremendous increase from the preinfection prevalence of any psychiatric diagnoses of 3%.8 A recent UK study showed that at 2–3 months from disease onset COVID-19 patients were more likely to report symptoms of moderate to severe anxiety and depression in comparison to controls.9 A study in Italy showed that 1 month after hospital treatment a considerable percentage of COVID-19 patients self-rated in the psychopathological range: 28% for PTSD, 31% for depression, 42% for anxiety, 20% for obsessive–compulsive symptoms and 40% for insomnia.10
Some COVID-19 patients need to be admitted to an intensive care unit (ICU).1 Psychiatric conditions, such as PTSD, depression, anxiety, sleep abnormalities and cognitive impairments, are frequent among people who required a hospitalization to an ICU.11 Up to 33 and 43% of patients treated in an ICU, respectively, develop PTSD and depression.12 Neurocognitive deficits have been observed in 73% of ARDS survivors at the time of hospital discharge, and 47% at 2 years later.13
Psychological effects
For many people to learn that they are infected with COVID-19 evokes significant emotional stress.6 The experience of the potentially lethal and untreatable disease is the cause of a severe distress, which may induce a mental illness or aggravate a pre-existing psychiatric disorder.2,6,14 Symptoms of COVID-19, especially serious symptoms, worry about infecting other people, social isolation and concerns about loss of income and the ability to work in the future may result in a severe emotional distress which may persist for a long time.
Neurobiological damage
Viral infection of the brain may have many neurological and psychiatric consequences, contributing to both the acute phase of COVID-19 and its potential sequelae.7,15 The combination of systemic inflammation, hypoxia resulting from respiratory failure and neuroinflammation may precipitate or worsen psychiatric disorders.7,15 Neuroinflammation is an important etiological factor for many neuropsychiatric and neurocognitive diseases, including depression, psychosis, autism, alcohol and drug abuse, sleep disorders, neurodegenerative disorders and epilepsy.
Depressive symptoms appear to be common in patients with post-COVID syndrome.7,9,10,15 Major depression is one of the most frequent neuropsychiatric disorders related to inflammatory damage to the brain.7,15 Considerable evidence has linked depressive symptoms to pro-inflammatory factors and neuroglial failure.7,15
Neurologic manifestations of COVID-19 reported to date include encephalopathy, stroke, anosmia, ageusia, dizziness, headache, Guillen–Barre Syndrome, Miller Fisher Syndrome and skeletal muscle injury/myalgia.16,17 Besides, multiple epileptic conditions have been observed in patients with COVID-19 including new-onset seizures, convulsive seizures, myoclonic seizures, status epilepticus and new-onset refractory status epilepticus. COVID-19 related neurological symptoms may persist for a long time after the acute COVID-19 illness.18
Physical ailments
A significant number of individuals experience persistent physical symptoms after recovering from their initial illness.19,20 A recent study in Switzerland showed persistence of symptoms in a third of ambulatory patients 30–45 days after diagnosis.19 Fatigue, dyspnea and loss of taste or smell were the main persistent symptoms. A study in the USA showed that most common persistent symptoms included cough, fatigue and dyspnea.20 Other studies also indicate that COVID-19-related symptoms such as weight loss, dyspnea, asthenia, chest pain, palpitations, headache, cutaneous signs, arthralgia, myalgia, digestive disorders and fever may persist among COVID-19 survivors for weeks or months.21
A recent study of patients in Italy hospitalized for COVID-19 found that, an average of 60 days after onset of symptoms, 87.4% still had virus-related symptoms, with 55% having three or more symptoms, especially fatigue, dyspnea and joint and chest pain.22 Persistent fatigue, weakness, poor exercise tolerance, pain, neurological sequelae and the negative psychological effects of prolonged ICU stays have been observed among ARDS survivors.14
Post-COVID syndrome in medical professionals
Health care professionals frequently get infected with COVID-19.23–25 According to a recent report, at least 120 physicians in Western Europe and Asia-Pacific countries died of the coronavirus disease.24 A recent large study in the U.K. found that relative to non-essential workers, health care professionals had a higher risk of severe COVID-19.25 Post-COVID syndrome in health care professionals decreases their ability to provide medical care and aggravates a shortage of physicians and nurses.
Discussion
Depression, anxiety disorders, PTSD, sleep abnormalities and cognitive impairments are associated with suicidal behavior.26,27 For example, lifetime risk of suicide among individuals with untreated depression ranges from 2.2% to 15%.26 Individuals suffering from depression are at 25 times greater risk for suicide than the general population.26 Physical illnesses including neurological conditions are also associated with non-lethal suicide attempts and suicide death.27–29 For example, chronic pain conditions have been associated with suicidal behavior.28 One study found that nearly 9% of suicide victims in 18 U.S. States from 2003 to 2014 had documentation of chronic pain in their records and that the percentage of suicide victims with chronic pain grew during the study time frame.28 Also, people with seizure disorders have a higher risk of suicide ideation and suicidal behaviors than the general population.27,29
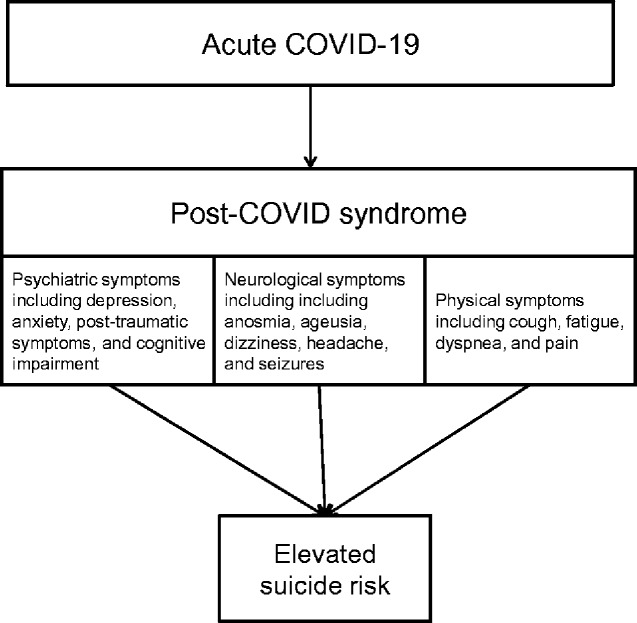
There is a high probability that symptoms of psychiatric, neurological and physical illnesses, as well as inflammatory damage to the brain in individuals with post-COVID syndrome increase suicidal ideation and behavior in this patient population (Figure 1). COVID-19 survivors without post-COVID syndrome may also be at elevated suicide risk. Studies of suicidality in COVID-19 survivors are urgently needed and will be a new area of suicide research. We need to study what factors may increase suicide risk among the COVID-19 survivors during and after the recovery. We also need to investigate whether there is a long-term increased suicide risk among COVID-19 survivors. Currently, health care professionals and public health authorities are focused on taking care of COVID-19 patients and containing the coronavirus’s spread in the general population. Care for mental disorders and psychiatric research may be somewhat deprioritized during the COVID-19 crisis. It has been noted that from January to July 2020 ‘635 000 people died from COVID-19. However, the number of deaths by suicide is not much lower, 462 000. If governments invested in suicide research and prevention only 5% of what they invest in dealing with COVID-19, we could save thousands of lives’.30
Figure 1.
Risk of suicide in individuals with post-COVID syndrome.
It is to be hoped that the studies of possible suicidality among individuals with post-COVID syndrome and other COVID-19 survivors will improve our understanding of psychiatric condition and suicide risk among COVID-19 survivors and help to develop suicide prevention interventions for this population. It is important to note that an appropriate management of psychiatric, neurological and medical conditions may reduce suicide risk among COVID-19 survivors with or without post-COVID syndrome.
Conflict of interest. None declared.
References
- 1. Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol 2020; doi:10.1038/s41579-020-00459-7. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sher L. The impact of the COVID-19 pandemic on suicide rates. Q J Med 2020; 113:707–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. John Hopkins University. Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering at John Hopkins University, 2020. https://coronavirus.jhu.edu/map.html (14 December 2020, date last accessed).
- 4. COVID Symptom Study. How long does COVID-19 last? Kings College, London, 2020. https://covid19.joinzoe.com/post/covid-long-term?fbclid=IwAR1RxIcmmdL-EFjh_aI- (11 December 2020, date last accessed).
- 5. Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ 2020; 370:m3026. [DOI] [PubMed] [Google Scholar]
- 6. Sher L. Are COVID-19 survivors at increased risk for suicide? Acta Neuropsychiatr 2020; 32:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Steardo L Jr, Steardo L, Verkhratsky A. Psychiatric face of COVID-19. Transl Psychiatry 2020; 10:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lam MH, Wing Y, Yu MW. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med 2009; 169:2142–2147. [DOI] [PubMed] [Google Scholar]
- 9. Raman B, Cassar MP, Tunnicliffe EM, Filippini N, Griffanti L, Alfaro-Almagro F, et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge, 2020. https://www.medrxiv.org/content/10.1101/2020.10.15.20205054v1 (11 December 2020, date last accessed). [DOI] [PMC free article] [PubMed]
- 10. Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun 2020; 89:594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McGiffin JN, Galatzer-Levy IR, Bonanno GA. Is the intensive care unit traumatic? What we know and don't know about the intensive care unit and posttraumatic stress responses. Rehabil Psychol 2016; 61:120–31. [DOI] [PubMed] [Google Scholar]
- 12. Davydow DS, Katon WJ, Zatzick DF. Psychiatric morbidity and functional impairments in survivors of burns, traumatic injuries, and ICU stays for other critical illnesses: a review ofthe literature. Int Rev Psychiatry 2009; 21:531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF Jr. Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med 2005; 171:340–347. [DOI] [PubMed] [Google Scholar]
- 14. Tucker P, Czapla CS. Post-COVID stress disorder: another emerging consequence of the global pandemic. Psychiatric Times, 2020. https://www.psychiatrictimes.com/view/post-covid-stress-disorder-emerging-consequence-global-pandemic (5 October 2020, date last accessed).
- 15. Meyer JH, Cervenka S, Kim MJ, Kreisl WC, Henter ID, Innis RB. Neuroinflammation in psychiatric disorders: PET imaging and promising new targets. Lancet Psychiatry 2020; 7:1064–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dougherty ML. Epilepsy essentials: EEG findings associated with COVID-19. Pract Neurol, 2020. https://practicalneurology.com/articles/2020-sept/epilepsy-essentials-eeg-findings-associated-with-covid-19 (September 2020, date last accessed)
- 17. Rahman A, Niloofa R, De Zoysa IM, Cooray AD, Kariyawasam J, Seneviratne SL. Neurological manifestations in COVID-19: a narrative review. SAGE Open Med 2020; 8:2050312120957925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wijeratne T, Crewther S. Post-COVID 19 Neurological Syndrome (PCNS); a novel syndrome with challenges for the global neurology community. J Neurol Sci 2020; 419:117179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nehme M, Braillard O, Alcoba G, Aebischer Perone S, Courvoisier D, Chappuis F, et al. COVID-19 Symptoms: longitudinal evolution and persistence in outpatient settings. Ann Intern Med 2020. doi:10.7326/M20-5926. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. ; IVY Network Investigators. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a Multistate Health Care Systems Network—United States, March-June 2020. Morb Mortal Wkly Rep 2020; 69:993–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Carvalho-Schneider C, Laurent E, Lemaignen A, Beaufils E, Bourbao-Tournois C, Laribi S, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect 2020. doi:10.1016/j.cmi.2020.09.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Carfì A, Bernabei R, Landi F, for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA 2020; 324:603–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Donnelly SC. Post COVID syndrome (PCS) and healthcare workers: who cares for the carers? Q J Med 2020; 113:611–611. [DOI] [PubMed] [Google Scholar]
- 24. Yoshida I, Tanimoto T, Schiever N, Patelli F, Kami M. Characteristics of doctors' fatality due to COVID-19 in Western Europe and Asia-Pacific countries. Q J Med 2020; 113:713–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mutambudzi M, Niedwiedz C, Macdonald EB, Leyland A, Mair F, Anderson J, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med 2020. doi:10.1136/oemed-2020-106731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Centre for Suicide Prevention. Depression and suicide prevention, 2020. https://www.suicideinfo.ca/resource/depression-suicide-prevention/ (15 December 2020, date last accessed).
- 27. O'Rourke MC, Jamil RT, Siddiqui W. Suicide screening and prevention. [Updated 2020 Nov 30]. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2020. https://www-ncbi-nlm-nih-gov.eresources.mssm.edu/books/NBK531453/ (14 December 2020, date last accessed). [PubMed] [Google Scholar]
- 28. Petrosky E, Harpaz R, Fowler KA, Bohm MK, Helmick CG, Yuan K, et al. Chronic pain among suicide decedents, 2003 to 2014: findings from the National Violent Death Reporting System. Ann Intern Med 2018; 169:448–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Coughlin SS, Sher L. Suicidal behavior and neurological illnesses. J Depress Anxiety 2013;02:12443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zalsman G. President’s update—July 2020. https://suicide-research.org/ (11 December 2020, date last accessed).