Abstract
BACKGROUND AND IMPORTANCE
The Zap-X system (Zap Surgical Systems Inc, San Carlos, California) is a radically new surgical robot designed for brain and head and neck radiosurgery. It represents the first new dedicated brain stereotactic radiosurgery platform in almost half a century optimizing the goals of safety, speed, and accuracy. The Zap-X system was used in a required Chinese National Medical Products Administration clinical study. In early January 2020, 2 patients were treated with the Zap-X robot prior to a national COVID-19 lockdown. Both were closely followed via clinical exam and magnetic resonance imaging (MRI) imaging. Prospectively collected data were used to generate this report.
CLINICAL PRESENTATION
Two female patients, each harboring either a trigeminal schwannoma or petroclival meningioma, were treated with the Zap-X robot. Respective tumor volumes were 2.60 and 4.02 cm3. A radiation dose of 13 Gy was prescribed to the 50% isodose line. At 8 mo of follow-up, preoperative symptoms were either resolved or stable and MRI imaging demonstrated a 31% and 56% reduction in lesion volume, respectively. In both patients, symptoms improved, and tumor volumes decreased, whereas no major complication was observed.
CONCLUSION
Given only 2 patients and short-term follow-up, any conclusions about the safety and efficacy of the Zap-X radiosurgery robot are preliminary. However, in the absence of any other published outcomes to date, this small case series may be of interest to many radiosurgical specialists.
Keywords: Stereotactic radiosurgery, Intracranial, Tumor, Meningioma, Schwannoma
ABBREVIATIONS
- DVH
dose volume histogram
- MRI
magnetic resonance imaging
- SRS
stereotactic radiosurgery
Stereotactic radiosurgery (SRS) is a widely accepted procedure for managing most brain and nonbrain tumors, as well as other lesions. The Zap-X uses image-guided targeting and a compact S-band linear accelerator to deliver high-dose precision radiosurgery to intracranial and cervical spine lesions.
CLINICAL PRESENTATION
Methodology
Under Institutional Review Board supervision, patient consent for Zap-X treatment was obtained. In early January 2020, 2 previously untreated female patients ages 17 and 45, each with a skull base lesion, were the first 2 undergoing radiosurgical treatment with the Zap-X system 1 in China. As per study protocol, patients were followed-up both clinically and with contrast magnetic resonance imaging (MRI) at 3 mo and then again at 8 mo post-SRS.
Changes in tumor volume were determined via serial contrast MRI. For relative comparison purposes, volumes were approximated using idealized ellipsoids, the Coniglobus formula approximation, enabling the quantification of relative volume changes over time. Importantly, this technique provides a different tumor volume baseline than the more precise, slice by slice, axial measurement calculated by treatment planning.
Case Presentation and Treatment
Case 1
This 17-yr-old female presented with 6 mo of intermittent left-sided facial pain occasionally accompanied by 3 to 4 min of facial numbness.
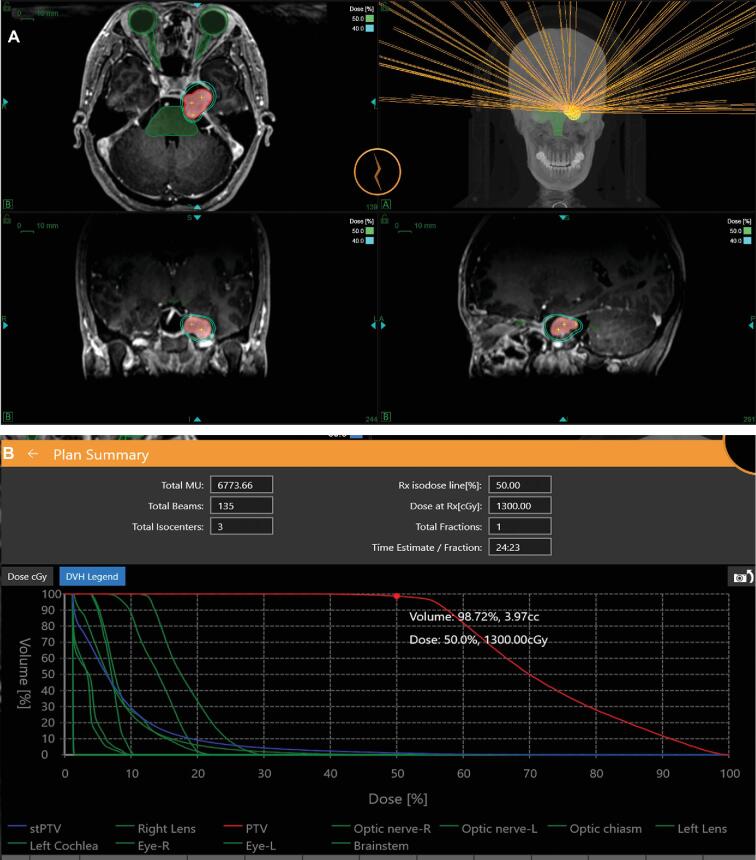
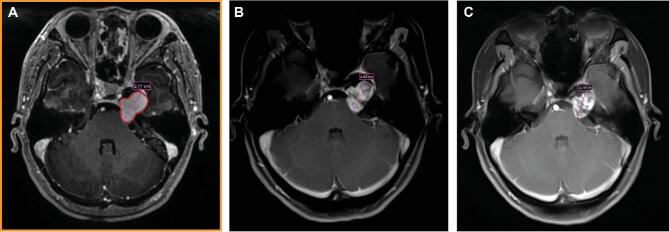
MRI showed a multilobulated lesion with mass effect involving the left middle and posterior fossae. Based on characteristic imaging and symptomatology, a presumptive trigeminal schwannoma of the left middle and posterior cranial fossae was diagnosed. On January 8, 2020, Zap-X radiosurgery was administered to a 4.02 cm3 tumor volume prescribing 13 Gy to the 50% isodose line (Figure1A and 1B). A total of 3 mo postradiosurgery, the patient reported persistent mildly bothersome left facial numbness but also the complete remission of pain. Brain MRI imaging showed no significant change in tumor size; neither brain edema nor necrosis were visualized. At 8 mo postradiosurgery, the maximum tumor dimension was found to have decreased from 2.7 to 2.2 cm (Figure 2A-2C), and the tumor volume decreased by 31% from 4.20 to 2.90 cm3. In addition, a stereotypic loss of central contrast enhancement within the tumor volume was noted at 8 mo of follow-up.
FIGURE 1.
A, Zap-X radiosurgery treatment plan and B, dose volume histogram (DVH) for Case 1.
FIGURE 2.
Contrast MRI images of Case 1: A, before; B, 3 mo postradiosurgery; and C, 8 mo post-Zap-X radiosurgery.
Case 2
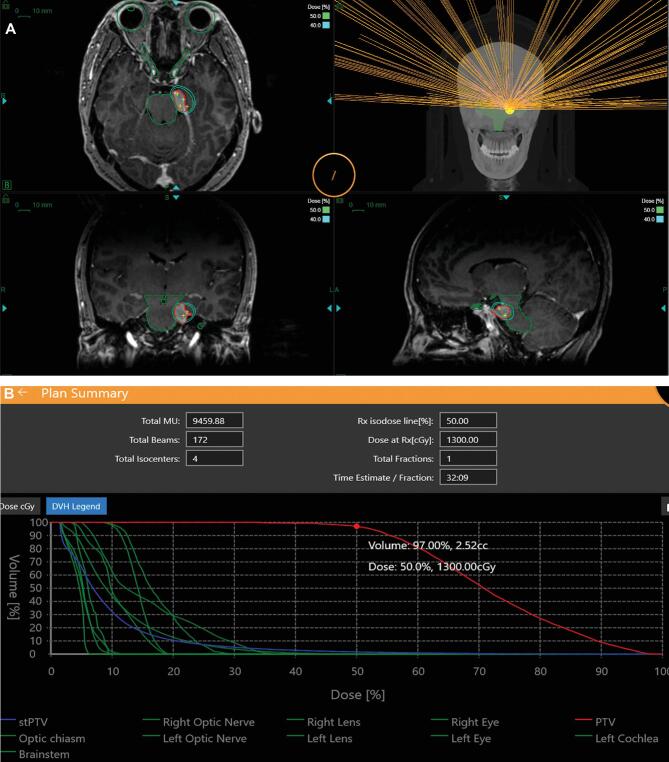
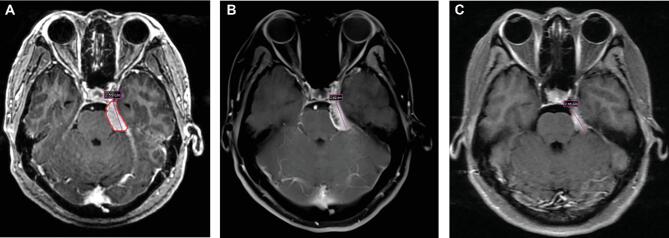
This 45-yr-old female presented with 8 mo of intermittent headaches and dizziness. Contrast brain MRI revealed a left-sided skull base lesion displacing adjacent anatomical structures diagnostically consistent with petroclival meningioma. Single-session Zap-X radiosurgery was performed on January 8, 2020, to a 2.60 cm3 target volume prescribing 13 Gy to the 50% isodose line (Figure 3A and 3B). A total of 3 mo postradiosurgery, the patient complained briefly of worsening headaches which remitted spontaneously. At 3 mo post-SRS, follow-up contrast brain MRI revealed no significant change in tumor size, no discernible brain edema or brain necrosis. Meanwhile, at 8 mo post-SRS, the maximum axial tumor dimension was found to have decreased from 2.6 to 2.2 cm (Figure 4A-4C) and relative tumor volume by 56% from 3.40 to 1.50 cm3.
FIGURE 3.
A, Zap-X radiosurgery treatment plan and B, DVH for Case 2.
FIGURE 4.
Contrast MRI images of Case 2: A, before; B, 3 mo postradiosurgery; and C, 8 mo post-Zap-X radiosurgery.
DISCUSSION
Key Results
At last clinical follow-up 8 mo post-SRS, pretreatment symptoms had largely resolved for both patients, excepting some persistent left-sided facial numbness in Case 1; such persistent numbness has been previously reported with SRS-treated trigeminal schwannoma.2 Meanwhile, MRI imaging showed neither radiation-induced brain injury nor more limited brain edema. Follow-up contrast MRI revealed a decrease in estimated tumor volume, which is often a favorable finding presaging ultimate long-term tumor control in most benign brain tumors.
Clinical success was judged by a decrease in symptoms, the absence of complications, and a reduction in tumor volume. Radiosurgery was deemed a technical success by virtue of the clinical outcome and both a safe and efficient treatment delivery.
Technological Analysis
Although the preliminary findings we report herein need to be confirmed in a multitude of additional patients, the outcomes are not surprising. On a technical basis, the Zap-X has been designed from the ground up to offer state-of-the-art brain radiosurgery. The combination of lower beam energy (3 MV), more solid angle gyroscopic crossfire, robust variable 15-cm thick (tungsten) cylindrical collimation, and shorter source-to-axis-distance enable a radiosurgery platform with exceptional penumbra.3 Meanwhile, the Zap-X’s image-to-image x-ray correlation technology ensures spatially accurate SRS delivery. In aggregate, these technical attributes enable the precision delivery of ionizing radiation combined with a surrounding steep dose gradient. The Zap-X also includes a first of its kind real-time megavoltage dose detector device that measures and verifies transit dosimetry.4
Generalizability
Despite the small number of patients being treated, our findings and results are consistent with conventional radiosurgical treatments of a wide variety of intracranial pathologies.
Limitations
The present report involves only 2 patients with short follow-up, which prevent any statistically significant conclusions.
CONCLUSION
The treatment of 2 benign skull base lesions with the Zap-X radiosurgical robot was without early adverse effects and resulted in image-based visible tumor shrinkage. Despite its preliminary nature, this verification of the safety and short-term efficacy of the Zap-X in these two brain tumor patients provides some reassurance that the technology may perform as expected.
Funding
This study did not receive any funding or financial support.
Disclosures
Dr Adler and Dr Weidlich are employed or under contract with Zap Surgical Systems Inc. The other authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Contributor Information
Longsheng Pan, Department of Neurosurgery, The First Medical Center of Chinese PLA General Hospital, Beijing, China.
Baolin Qu, Department of Radiation Oncology, The First Medical Center of Chinese PLA General Hospital, Beijing, China.
Jingmin Bai, Department of Radiation Oncology, The First Medical Center of Chinese PLA General Hospital, Beijing, China.
Lichao Huang, Department of Neurosurgery, The First Medical Center of Chinese PLA General Hospital, Beijing, China.
Jinyuan Wang, Department of Radiation Oncology, The First Medical Center of Chinese PLA General Hospital, Beijing, China.
Chengcheng Wang, Department of Radiation Oncology, The First Medical Center of Chinese PLA General Hospital, Beijing, China.
Xiangkun Dai, Department of Radiation Oncology, The First Medical Center of Chinese PLA General Hospital, Beijing, China.
Georg Weidlich, Zap Surgical Systems Inc, San Carlos, California.
John R Adler, Department of Neurosurgery, Stanford University School of Medicine, Palo Alto, California.
REFERENCES
- 1. Weidlich GA, Bodduluri RM, Achkire Y, Lee C, Adler JR. Characterization of a novel 3 megavolt linear accelerator for dedicated intracranial stereotactic radiosurgery. Cureus. 2019;11(3):1-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sakamoto GT, Borchers DJ 3rd, Xiao F, Yang HJ, Chang SD, Adler JR Jr. Cyberknife radiosurgery for trigeminal schwannomas. Neurosurgery. 2009;64(Suppl_2):A14-A18. [DOI] [PubMed] [Google Scholar]
- 3. Weidlich GA, Schneider M, Adler JR. Characterization of a novel revolving radiation collimator. Cureus. 2018;10(2):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jenkins CH, Kahn R, Weidlich GA, Adler JR. Radiosurgical treatment verification using removable megavoltage radiation detectors. Cureus. 2017;9(11):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]