Abstract
Background
To investigate the knowledge, attitudes and anxiety toward COVID-19 among Chinese college students studying in China and abroad.
Method
A structured questionnaire, comprised of demographic characteristics, knowledge and attitudes toward COVID-19 and the State–Trait Anxiety Inventory (STAI), was used to collect data for 566 domestic students and 126 students studying abroad.
Results
Domestic students were better than students abroad in knowledge of epidemiology and manifestations. Domestic students showed a significant higher enthusiasm for voluntary services than students abroad, including medical science popularization, community services, traffic dispersion, logistics transportation and being volunteers for vaccine trials. The scores (Mean ± SD) of S-AI and T-AI among students abroad were 59.48 ± 8.63 and 54.10 ± 7.20, respectively, which were significantly higher than those of domestic students (39.46 ± 8.16 and 39.25 ± 7.72).
Conclusions
Our study showed a better understanding of knowledge, more positive attitudes and less anxiety toward COVID-19 among domestic students, compared with students studying abroad. In light of this information, more attention and appropriate psychological and social intervention should be paid to college students with anxiety, especially those studying abroad.
Keywords: anxiety, Chinese university students, coronavirus disease 2019, knowledge, voluntary services
Introduction
An outbreak of novel coronavirus pneumonia occurred in December 2019 in Wuhan, Hubei province and rapidly spread throughout China, which has also spread worldwide. The World Health Organization (WHO) named the disease as coronavirus disease 2019 (COVID-19), and the International Committee on the Taxonomy of Viruses named the virus as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 Respiratory droplets and direct contact were the main transmission routes.2 A study of 1354 Canadian adults in early February 2020 showed ~40% of the participants were worried or very worried about SARS-CoV-2, even with only four confirmed cases in Canada at that time.3 Likewise, the fear of COVID-19 was greater than that of seasonal flu outbreaks globally, although flu had killed considerably more individuals. The fear of the unknown and uncertainty can definitely lead to the development of mental disorders and adverse behaviors, such as increased alcohol and tobacco consumption.4 Emotional coping is crucial to this process.
Globally, as of 3:29 pm CEST, 12 October 2020, there have been 37 423 660 confirmed cases of COVID-19, including 1 074 817 deaths, reported to WHO.5 Previous studies showed that mental disorders, such as stress, anxiety and depression, had been found in medical staff and the general population.6,7 A study aiming to better understand the levels of psychological impact in the initial stage of the COVID-19 outbreak administered the Depression, Anxiety and Stress Scale (DASS-21) with 1210 individuals in 194 cities of China. Moderate-to-severe depressive symptoms, anxiety symptoms and stress level were found in 16.5, 28.8 and 8.1% of the participants, respectively.8 However, some positive interventions, such as viewing heroic acts, speeches from experts, and knowledge of the disease and prevention, were associated with positive psychological impact.9,10 Therefore, it is important to call for appropriate clinical and mental health interventions. It is equally important to find and know the actual psychological status of the groups potentially targeted for such interventions because different groups can perceive the risk differently.11 In other words, investigating the psychological impacts of COVID-19 on different groups is the key point to make strategies to reduce the psychological combinations of COVID-19.
Previous studies in the H1N1 influenza epidemic in 2009 showed that the Australian university population was not worried about the pandemic and did not even consider it serious. They still believed that the younger individual (20–34 year old) were not susceptible to H1N1 influenza, although their own age group was found to be the one most affected by previous flu pandemics.12,13 Different countries have adopted different measures to prevent the COVID-19 epidemic. Different countries have adopted different measures to deal with the new crown epidemic. Measures in China, such as closing classes in the entire school system, home quarantine and studying online, were diametrically opposed to measures in the United States of America (USA), such as continuing offline classes. Higher levels of anxiety and depression were predicted in the wake of the stay-at-home order, since confinement could produce or exacerbate such psychological problems.14,15
Psychological symptoms of COVID-19 on general population have been studied in previous researches; however, the impact of COVID-19 on Chinese college students has not been evaluated, especially the comparison between Chinese domestic students and students studying abroad. Therefore, the aim of the present study is to comprehensively evaluate the knowledge, attitudes and anxiety toward COVID-19 among domestic and overseas Chinese college students and call for appropriate psychological and social intervention for college students with anxiety.
Materials and methods
This case–control study was conducted between February 2020 and August 2020, which was performed after approval from the ethics committees of the Xiangya Hospital, Central South University. The purpose of the study was explained to the participants prior to distributing the questionnaire. Informed consents were obtained and all questionnaires were administered anonymously.
Study population
All the participants in our study were enrolled via online questionnaire named Wenjuanxing, a platform providing functions equivalent to Amazon Mechanical Turk. Group A was comprised of Chinese domestic college students, and Group B was comprised Chinese students studying abroad. Participants were required to be over 18 years old and have no history of transnational in the past 2 months. Participants who had alcohol or caffeine addiction, chronic physical disease and a history of neurological disease which affected cognitive function were excluded. Only students going abroad within 2 years were included in Group B. Most of the students (90.48%) in Group B were selected students studying in USA because of the diametrically opposite measures taken by China and USA in the face of COVID-19. The same questionnaires which were all performed in Chinese were used for both groups and a total of 692 valid questionnaires were returned.
Assessment tools
The questionnaire consisted of four domains, including demographic characteristics, knowledge, attitudes (scientific research, volunteer services and Chinese doctor–patient relationships) and degree of anxiety toward COVID-19.
Data Collection Form
The Data Collection Form, a detailed interview form with questions about the general information of the participants, was prepared by the researchers for the purpose of this study. Gender, age, studying stage, major, living situation and presence of influenza-like symptoms were included in theform.
Self-reported assessments
The items in the second domain were extracted from the Guidelines for the Diagnosis and Treatment of 2019-nCoV Infection by the National Health Commission (Trial Version 5), which included epidemiological and clinical knowledge. The attitudes toward social events associated with COVID-19 involved three aspects—scientific research, volunteer services and doctor–patient relationships in China. The items of attitudes toward the impacts of COVID-19 on Chinese doctor-patient relationships were as follows: (i) your opinions on the harmony of doctor–patient relationship in China; (ii) your opinions on whether COVID-19 will improve doctor–patient relations in China; (iii) knowledge of recent violence against Chinese medical staff; (iv) your opinions on the occupational risk of Chinese medical staff and (v) your views on the necessity of security screening in hospitals. Each item was rated based on the degree of agreement from 1 to 5 (strongly disagree to strongly agree).
The State–Trait Anxiety Inventory
State–Trait Anxiety Inventory (STAI) was developed by Spielberger in 1970 to assess the degrees of anxiety symptoms of individuals.16 The Chinese version of the STAI has been verified to have high internal consistency with Chinese population, whose coefficient alphas were reported to be 0.90 and 0.81, respectively, for the Chinese State anxiety (S-AI) and Trait anxiety (T-AI).17,18 The score range for both S-AI and T-AI is 20–80 points, and a higher score represents more severe symptoms of anxiety.
Statistical analysis
All demographic data were analyzed descriptively. Continuous data were presented as means and standard variations (Mean ± SD) and nominal data were presented as frequencies and percentages. The differences between the mean scores in demographic characteristics and each item were tested with two independent sample t-test. The Chi-Square test was used for comparison of groups regarding categorical variables. SPSS 19.0 package program was used for statistical analysis and P < 0.05 was considered statistically significant.
Results
Demographic data of samples
A total of 607 domestic college students were approached in Group A with 41 (6.8%) refusing to be interviewed and 566 (93.2%) agreeing. A total of 141 individuals in Group B were approached. Out of these, 15 (10.6%) refused and 126 (89.4%) agreed. There were no significant differences between two groups except for the age and living situation (Supplementary Table S1).
Knowledge toward COVID-19
Supplementary Table S2 showed significant differences in the perspectives on the effective means for inactivating SARS-CoV-2, such as ether (P < 0.001) and chlorine disinfectants (P = 0.008), as well as clinical manifestations (P = 0.044) and laboratory examination (P = 0.023).
Attitudes toward scientific research and hot topics in social events during COVID-19
Scientific research
Reading articles online (42.05 and 44.44%) and writing papers (27.56 and 31.75%) became the most frequent methods of research in Group A and B, correspondingly. As shown in Supplementary Table S3, the proportion of writing and revising project application among domestic students was higher than the overseas students group (P = 0.032). The proportion of adjusting or improving the experimental plan was just the opposite (P = 0.026).
Voluntary services
Supplementary Table S3 indicated that domestic students showed a significant higher enthusiasm for voluntary services than overseas students, which was reflected in medical science popularization (P = 0.011), community services (P < 0.001), traffic dispersion (P = 0.001) and logistics transportation (P = 0.025). In addition, 40.28% of domestic college students expressed their willingness to be a volunteer for vaccine trials of COVID-19, which was significantly higher than 19.05% of overseas Chinese students (P < 0.001).
Chinese doctor–patient relationships
There were no significant differences in attitudes toward the impacts of COVID-19 on improving doctor-patient relationships in China between two groups (Supplementary Table S4). Overall, both groups still held negative attitudes toward doctor-patient relationships in China. Further investigations showed significant differences in the information access of intense relationships (Fig 1A), such as transmitting from Weibo (p = 0.02) or friends of QQ and Wechat (P = 0.02), or their own experience (p < 0.001). Nearly 80% of both the two groups thought patient factors was the main cause of intense relationship in China (Fig. 1B).
Fig. 1.
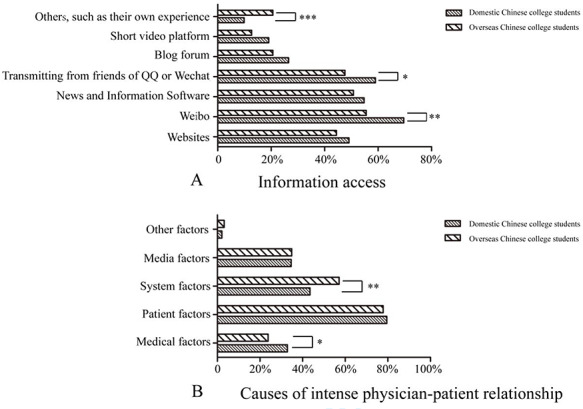
Information access (A) and analysis on the causes (B) of physician–patient relationship in China by domestic and overseas Chinese college students. (* indicates P < 0.05; ** indicates P < 0.01; *** indicates P < 0.001).
Degrees of anxiety
A total of 332 out of 566 domestic students and 110 out of 126 overseas students agreed to participant in the STAI. The scores (Mean ± SD) of S-AI and T-AI among overseas Chinese students were 59.48 ± 8.63 and 54.10 ± 7.20, respectively, which were significantly higher than those of domestic students (39.46 ± 8.16 and 39.25 ± 7.72) (P < 0.001), indicating greater anxiety faced by Group B (Fig. 2A and B).
Fig. 2.
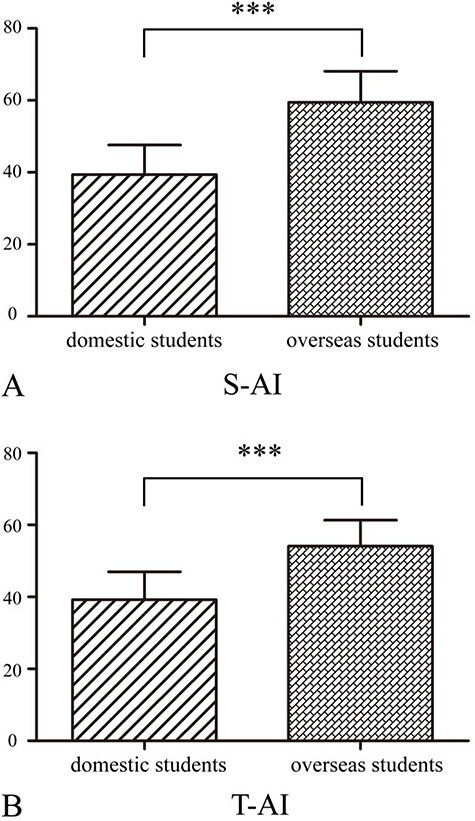
S-AI (A) and T-AI (B) of domestic and overseas Chinese college students. (*** indicates P < 0.001).
Discussion
This study is one of the first to investigate the knowledge, attitudes and anxiety toward COVID-19 among Chinese college students studying in China and USA. Our study showed a better understanding of knowledge, more positive attitudes and less anxiety toward COVID-19 among domestic students compared with Chinese students studying abroad. More attention and appropriate psychological and social intervention should be paid to college students with anxiety, especially those studying abroad.
Psychological problem has been one of the hottest topics in COVID-19. Unexpectedly, studies in the northern Spain showed higher mean levels of anxiety in the 18- to 25-year-age bracket, followed by the 26- to 60-year-age bracket and then the individuals more than 61 years old, which was different from the results found in H1N1.7,12 Considering the 18- to 25-year-age bracket was mostly university students, these symptoms were attributed to the wake of the stay-at-home and the additional stress to meet the need of adopting to the new online education environment without face-to-face classes.15,19 However, this study suggested almost no anxiety symptoms in university students in China who were required to stay at home and study online. Different measures adopted by national governments in the face of COVID-19 may explain the significant differences in STAI between the two groups.20 Secondly, studies have found that the possibility of patients and their caregivers suffering from psychological comorbidities decreases with the deeper understanding of the diseases,21 consistent with the above results. In addition, more new media use and media engagement with rumors were found to be associated with negative psychological outcomes, which might be another cause of the differences.22 Notably, further study showed that 53.97% of Chinese students studying abroad had been unfairly treated, including personal attacks, verbal attacks and asking to leave public places, as it was once thought that SARS-CoV-2 originated in China.23 Therefore, more attention should be paid to implement prevention and intervention programs, release timely public health communication from official sources and debunk misinformation associate with COVID-19 to mitigate the anxiety levels.24,25
Interestingly, significant differences were found in the strong willingness to engage in voluntary services among domestic students, although they knew the risk of infection and insomnia.26 On the one hand, the degree of gravity of the epidemic in different countries, which was associated with the extent of voluntary services, could definitely explain the differences.27 On the other hand, we attributed it to empathy, which was thought to be a unique ability of humans to feel, understand and share the emotional state of others,28 making it possible to resonate with others’ positive and negative feelings alike. During the initial stage of COVID-19, lots of medical staff across China chose to support Hubei province, the most severely affected areas in China, with little knowledge of SARS-CoV-2. These heroic acts, broadcast on media platforms in China repeatedly, strengthened the determination of general population to overcome problems caused by SARS-CoV-2 via empathy.9,10
Some limitations of this study must be acknowledged. Due to the respective sample size of Chinese studying abroad, the results cannot represent the mental health of the entire population of Chinese students studying abroad, which we hope to expand in future work. Also, the different stages of COVID-19 control among China and USA may affect the results. Participants may have concerns about the confidentiality of this study, which may have affected their responses.
Conclusion
This is the first study to investigate the knowledge, attitudes and anxiety toward COVID-19 among Chinese college students studying in China and USA. Better understanding of knowledge, more positive attitudes and less anxiety toward COVID-19 were found among domestic students, compared with students studying abroad. In light of this information, more attention and appropriate psychological and social intervention should be paid to college students with anxiety, especially those studying abroad.
Author contributions
The idea was put forward by Dr Yang and Dr Zhang. The design and distribution of the questionnaire were jointly completed by all authors. Dr Yang, Dr Chen and Dr Zhang were in charge of writing the article.
Supplementary Material
Acknowledgements
We would like to express our deepest gratitude to the domestic and overseas Chinese college students who completed the questionnaires. We would also be grateful to the team members, the volunteers and coordinators who assisted in this data collection.
Haojun Yang, M.D. Doctor
Zhuohui Chen, M.D. Doctor
Yishu Fan, M.D. Doctor
Xinhang Hu, M.D. Doctor
Tong Wu, M.D. Doctor
Shuntong Kang, M.D. Doctor
Bo Xiao, M.D. Professor
Mengqi Zhang, M.D. Professor
Contributor Information
Haojun Yang, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Zhuohui Chen, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Yishu Fan, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Xinhang Hu, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Tong Wu, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Shuntong Kang, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Bo Xiao, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Mengqi Zhang, Department of Neurology, Xiangya Hospital of Central South University, Changsha, Hunan 410008, China.
Funding
This research was funded by the Key Research and Development Program of Hunan Province (No. 2020SK2063), the Natural Science Foundations of Hunan Province (No. 2020JJ4134), and the National Natural Science Foundation of China (No. 81501025).
Conflict of interest
All authors declare that there are no conflicts of interest.
Ethical statement
This study was approved by the ethics committee of Xiangya Hospital, Central South University. Informed consents were obtained and all questionnaires were administered anonymously. Participants were allowed to withdraw from the study at any phase.
References
- 1. Yang H, Chi Y, Chen Z et al. Differential diagnosis and hospital emergency management for fastlane treatment of central nervous system infection under the COVID-19 epidemic in Changsha, China. Front Neurol 2020;11:555202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dong L, Tian JH, He SM et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her Newborn. JAMA 2020;323(18):1846–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Asmundson GJ, Taylor S. Coronaphobia: fear and the 2019-nCoV outbreak. J Anxiety Disord 2020;70:102–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shigemura J, Ursano RJ, Morganstein JC et al. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci 2020;74:281–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. WHO coronavirus disease (COVID-19) dashboard. [EB/OL]. [2020-07-21]. https://covid19.who. int.
- 6. Chen Q, Liang M, Li Y et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7(4):e15–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica 2020;36(4):e00054020. [DOI] [PubMed] [Google Scholar]
- 8. Wang C, Pan R, Wan X et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:17–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Depoux A, Martin S, Karafillakis E et al. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med 2020;27(3):taaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chao M, Xue D, Liu T et al. Media use and acute psychological outcomes during COVID-19 outbreak in China. J Anxiety Disord 2020;74:102248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Traunmüller C, Stefitz R, Gaisbachgrabner K, Schwerdtfeger A. Psychological correlates of COVID-19 pandemic in the Austrian population. BMC Public Health 2020;20(1):1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Van D, McLaws ML, Crimmins J et al. University life and pandemic influenza: attitudes and intended behaviour of staff and students towards pandemic (H1N1) 2009. BMC Public Health 2010;10:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lin Y, Huang L, Nie S et al. Knowledge, attitudes and practices (KAP) related to the pandemic (H1N1) 2009 among Chinese general population: a telephone survey. BMC Infect Dis 2011;11:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brooks SK, Webster RK, Smith LE et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395:912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cava MA, Fay KE, Beanlands HJ et al. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs 2005;22(5):398–406. [DOI] [PubMed] [Google Scholar]
- 16. Spielberger CD, Vagg PR. Psychometric properties of the STAI: a reply to Ramanaiah, Franzen, and Schill. J Pers Assess 1984;48(1):95–7. [DOI] [PubMed] [Google Scholar]
- 17. Shek DT. Reliability and factorial structure of the Chinese version of the state-trait anxiety inventory. J Psychopathol Behav Assess 1988;10(4):303–17. [Google Scholar]
- 18. Zhang J, Lamis DA, Yuanyuan K. Measuring Chinese psychological traits and social support with western developed instruments in psychological autopsy studies. J Clin Psychol 2012;68(12):1313–21. [DOI] [PubMed] [Google Scholar]
- 19. Antúnez Z, Vinet EV. Mental health problems among students of a regional Chilean university. Rev Med Chil 2013;141(2):209–16. [DOI] [PubMed] [Google Scholar]
- 20. Tang KHD. Movement control as an effective measure against Covid-19 spread in Malaysia: an overview. Z Gesundh Wiss 2020;13:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yang H, Feng Y, Zhu Z et al. Evaluation of anxiety, depression, and sleep quality among parents of children with epilepsy in southern China. Epilepsy Behav 2020;112:107340. [DOI] [PubMed] [Google Scholar]
- 22. Tasnim S, Hossain MM, Mazumder H. Impact of Rumors and misinformation on COVID-19 in social media. J Prev Med Public Health 2020;53(3):171–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nadeem MS, Zamzami MA, Choudhry H et al. Origin, potential therapeutic targets and treatment for coronavirus disease (COVID-19). Pathogens 2020;9(4):307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Islam MS, Sarkar T, Khan SH et al. COVID-19-related Infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hyg 2020;103(4):1621–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li Z, Ge J, Yang M et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun 2020;88:916–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li X, Yu H, Bian G et al. Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain Behav Immun 2020;87:140–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cheng HW, Li CW, Chan KY, Sham MK. The first confirmed case of human avian influenza A(H7N9) in Hong Kong and the suspension of volunteer services: impact on palliative care. J Pain Symptom Manage 2014;47(6):e5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen J. Empathy for distress in humans and rodents. Neurosci Bull 2018;34(1):216–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


