Abstract
Background
Coronavirus disease (COVID)-secure workplace guidance, including the prompt self-isolation of those with COVID-19 symptoms, is fundamental to disease control in workplaces. Despite guidance, a large number of workplace outbreaks have been observed. This study aimed to identify the proportion of symptomatic staff members attending workplaces after symptom onset or testing, and associated factors.
Methods
This study of symptomatic COVID-19 cases associated with London workplaces used London Coronavirus Response Centre (LCRC) records from routine telephone calls with cases and employers, from 17th July to 10th September. For each case, symptoms, date of onset, date of testing and the last attendance at work were extracted. Univariable logistic regression was performed to investigate whether age, gender or occupation was associated with workplace attendance after the onset of symptoms.
Results
Out of 130 symptomatic COVID-19 cases, 42 (32.3%) attended the workplace after their reported date of symptom onset, including 16 (12.3%) with recorded COVID-19 symptoms. Five staff members attended after COVID-19 testing. Males were 66% less likely to attend the workplace after the onset of COVID-19 symptoms compared to females (odds ratio 0.34, P = 0.05). Age and occupation were not predictive for workplace attendance after the onset of symptoms.
Conclusion
A minority of symptomatic cases attended the workplace after the onset of COVID-19 symptoms, with a smaller proportion attending after testing. Males appeared less likely to attend the workplace after the onset of COVID-19 symptoms. This study highlights the need for ongoing COVID-19 secure workplace practices and prompt self-isolation after COVID-19 symptom onset or testing.
Keywords: communicable diseases, public health, health protection
Introduction
There have been a number of large outbreaks of coronavirus disease 2019 (COVID-19) associated with workplaces across Europe.1 On 17th July the British Prime Minister outlined a shift from national to local restrictions, and a phased easing of measures,2 stating that from 1st August employers would have more discretion over how their staff worked. After the easing of national restrictions, outbreaks associated with workplaces increased, whilst those linked to hospitals and care homes remained low.3 In addition, by the end of August 2020, the UK Food Standards Agency reported at least 40 active outbreaks in food processing plants.4
Many key workers have continued to attend workplaces throughout the pandemic. In April 2020, statistics released by the UK’s Office for National Statistics showed only half of adults in employment were working from home, as a result of the lockdown measures introduced.5 Given the recent increase in COVID-19 cases in the UK, the government was forced to delay a planned campaign to encourage staff to return to workplaces, continuing to encourage work from home where possible.6 Government guidance states that those with symptoms of COVID-19: fever, a new cough or anosmia/aguesia, must self-isolate for 10 days from the onset of symptoms, including whilst awaiting testing or test results.7 Emerging data have found that self-reported adherence to isolation among those with COVID-19 symptoms is low (18.2%, 95% CI 16.4–19.9%), and associated with a number of factors including being male, young and working in a key sector.10 With many unable to work from home and therefore attending workplaces, the prompt isolation of symptomatic individuals is fundamental to minimizing disease transmission in the workplace and the wider community.
Home to ~13% of the UK population, London is responsible for 23% of the UK economy.8 Professional, real estate, scientific and technical activities form 15.8% of the overall local economy.9 The current health protection response to COVID-19 in London involves National Health Service (NHS) Test & Trace working with local health protection and public health teams. The London Coronavirus Response Centre (LCRC), part of Public Health England (PHE), leads the response to situations that are deemed complex, including those involving cases that attended a workplace during their infectious period.
The primary aim of this analysis was to identify the proportion of confirmed cases of COVID-19 associated with London workplaces and reported to the LCRC that attended work after symptom onset, as well as the proportion attending after COVID-19 testing. Secondary aims included stratifying this group by age, gender and occupation, and investigating whether these factors were predictive for workplace attendance after symptom onset.
Methods
Data collection
The data used for this analysis were obtained through existing LCRC records on recent workplace situations and associated cases. All COVID-19 cases attending workplaces in the 2 days prior to symptom onset (i.e. during their infectious period) were initially identified through tier two of NHS Test and Trace as part of the contact tracing process, and escalated to the LCRC for further management. Employers and staff were also able to contact the LCRC directly for support; helping to identify any cases associated with workplaces that were not escalated by NHS Test and Trace. Line managers (as reported by cases themselves) were initially contacted to conduct a risk assessment and for the provision of support on case and outbreak management. Through this contact with employers, the dates on which confirmed cases reported symptom onset and attendance at work were crosschecked. All data collected by cases and employers were entered into a single electronic data recording system (HP zone). Workplace situations were created if at least one confirmed case of COVID-19 was at work in the 2 days prior to feeling unwell, or afterwards.
Data Extraction
Eight weeks of data, from 17th July to 10th September, were retrospectively extracted from HP zone. The data used for this analysis were limited to workplaces other than hospitals, schools and care homes, since data collection, reporting and outbreak response varied across these settings. A confirmed case of COVID-19 was defined as a positive reverse transcriptase polymerase chain reaction (RT-PCR) test from an accredited laboratory that was uploaded onto the Second Generation Surveillance System (SGSS).
The free-text data recorded against each confirmed case of COVID-19 associated with a workplace, and the respective workplace situation to which that case was linked, were both analysed to obtain details. For each case, the recorded initial symptoms, date of symptom onset, date of RT-PCR testing, and the last reported attendance at work were extracted, alongside demographic and occupation details. These data were used to calculate whether symptomatic staff members attended work after symptom onset (i.e. on at least 1 day after reported symptom onset date), whether they attended after the onset of COVID-19-specific symptoms including fever, cough or anosmia/aguesia and whether they attended work after being tested for COVID-19.
Asymptomatic cases including those identified and tested as contacts of cases were excluded, as were individuals who were not members of staff (e.g. customers). Where the nature of initial symptoms was not recorded, it was assumed that no COVID-19-specific symptoms were present. Where there were inconsistencies between the case and employer for dates of attendance in the workplace, details provided by the employer were deemed more reliable and therefore used in analysis.
Statistical analysis
To investigate the trend in the number of workplace situations over the study period, a non-parametric test for ordered groups, an extension of the Wilcoxon rank-sum test, was used with the ‘nptrend’ command on STATA. The study population was stratified into those who did not attend the workplace after symptom onset, those who attended after symptom onset and those who attended after the onset of symptoms included in the current COVID-19 case definition.
Univariable logistic regression was undertaken on STATA to identify whether age, gender or occupation were associated with workplace attendance after symptom onset. These factors were selected on the basis of being of significant public health importance, and were relatively complete in the dataset. It was not possible to include ethnicity or deprivation using routinely collected data. Gender and occupation data were collected for all cases although it was not possible to obtain the age of nine cases. Occupational groups included in the regression were those most prevalent in the study population, including office, retail and construction. Three age groups were created for regression, comparing those aged 30–49 and ≥ 50 to a reference group (18–29 years). Separate regression models were created for workplace attendance after the onset of COVID-19 symptoms, and attendance after the onset of any symptoms. For all analyses, P-values < 0.05 were considered statistically significant.
Ethics
Public Health England has legal permission, provided by Regulation 3 of The Health Service (Control of Patient Information) Regulations 2002, to process patient confidential information for monitoring and managing incidents and outbreaks of communicable diseases. Data presented here were collected from routine health protection work as part of the COVID-19 response in London. All data were de-identified prior to analysis and the authors had all necessary administrative permissions to access the data.
Results
A total of 130 symptomatic COVID-19 cases associated with 104 workplace situations were identified over the 8-week period from 17th July to 11th September. There was a large increase in situations in the final week, commencing 4th September (Fig. 1). There was no general trend in situations associated with symptomatic cases, over the eight-week period (P = 0.99). The number of workplace situations where at least one staff member attended work after their reported symptom onset date showed a significant trend (P = 0.02), increasing over the first period (Weeks 1–3), falling in Weeks 4 and 5 and again increasing by Week 8. The proportion of workplace situations with at least one staff member attending work after symptom onset was highest in Week 1 (75%), lowest in Week 6 (26.7%) and remained similar in the final week of study (30.3%).
Fig. 1.
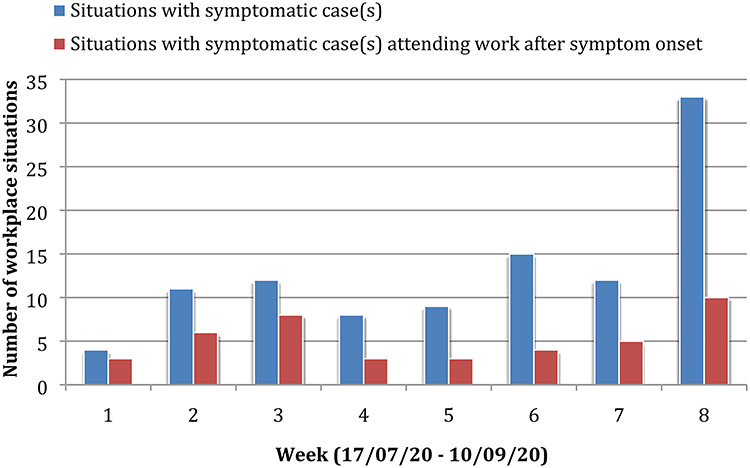
Trend in London workplace situations associated with symptomatic COVID-19 cases.
Workplace attendance after symptom onset
Across the study population (n = 130), most were male (63.8%), the most common age group was 25–36 years (37.7%) and the most common occupations were office, retail and construction. A total of 42 (32.3%) cases attended the workplace after their reported date of symptom onset, including 16 with recorded COVID-19 symptoms and 26 without. Of these 42 cases, the exact nature of initial symptoms was unknown for 11 individuals. Symptoms reported and considered as non-COVID-19 symptoms, included fatigue, sore throat, muscle pain, general malaise and ‘cold-like’ symptoms. Of those with recorded COVID-19 symptoms, eight had fever, five had anosmia and/or aguesia, one had cough and two had both fever and cough.
Table 1 shows that the majority of those who did not attend the workplace with symptoms were male (61.4%), compared to a minority for those who attended after COVID-19 symptom onset (37.5%). Cases were distributed across a range of ages, with the most common age group being 26–35 years for all subgroups. The most prevalent occupational groups for those that did not attend after symptom onset were office, retail and construction. For those that attended after COVID-19 symptom onset, office and retail were the most prevalent with only one (6.3%) in construction.
Table 1.
Stratification of COVID-19 cases associated with workplaces by gender, age and occupation
| Risk factor | Workplace non-attendance after symptoms (n = 88) (%) | Workplace attendance after any symptoms (n = 42) (%) | Workplace attendance after COVID-19 symptoms (n = 16) (%) |
|---|---|---|---|
| Gender | |||
| Male | 54 (61.4) | 23 (54.8) | 6 (37.5) |
| Female | 34 (38.6) | 19 (45.2) | 10 (62.5) |
| Age | |||
| 18–25 | 22 (25.0) | 4 (9.5) | 2 (12.5) |
| 26–35 | 28 (31.8) | 15 (35.7) | 6 (37.5) |
| 36–45 | 20 (22.7) | 9 (21.4) | 2 (12.5) |
| 46–55 | 8 (9.1) | 6 (14.3) | 2 (12.5) |
| 56+ | 6 (6.8) | 3 (7.1) | 2 (12.5) |
| Occupation | |||
| Office | 19 (21.6) | 10 (23.8) | 4 (25.0) |
| Retail | 18 (20.5) | 8 (19.0) | 4 (25.0) |
| Construction | 17 (19.3) | 5 (11.9) | 1 (6.3) |
| Police/armed forces | 7 (8.0) | 4 (9.5) | 1 (6.3) |
| Restaurant/bar | 6 (6.8) | 4 (9.5) | 2 (12.5) |
| Transport | 4 (3.4) | 2 (4.8) | 0 |
| Cleaning | 3 (3.4) | 1 (2.4) | 1 (6.3) |
| Hair & beauty | 3 (3.4) | 2 (4.8) | 1 (6.3) |
| Dental/pharmacy | 4 (4.5) | 1 (2.4) | 0 |
| Warehouse/factory | 3 (3.4) | 0 | 0 |
| Other | 4 (4.5) | 5 (11.9) | 2 (12.5) |
Table 2.
Predictive factors for attending workplace after COVID-19 symptom onset
| Odds Ratio | 95% CI | P-value | |
|---|---|---|---|
| Gender | |||
| Female | 1.00 | – | – |
| Male | 0.34 | 0.11–1.00 | 0.05 |
| Age | |||
| Age 18–29 | 1.00 | – | – |
| Age 30–49 | 1.17 | 0.32–4.28 | 0.82 |
| Age ≥ 50 | 1.59 | 0.32–7.90 | 0.57 |
| Occupation | |||
| Non-office | 1.00 | – | – |
| Office | 1.12 | 0.35–4.00 | 0.78 |
| Non-retail | 1.00 | – | – |
| Retail | 1.39 | 0.41–4.74 | 0.60 |
| Non-construction | 1.00 | – | – |
| Construction | 0.30 | 0.04 – 2.36 | 0.25 |
Univariable logistic regression found that males were 66% less likely (OR 0.34, 95% CI 0.11–1.00) to attend the workplace with COVID-19 symptoms, compared to females, although this was of borderline statistical significance. Age and occupation (including office, retail or construction roles) were not significantly associated with workplace attendance after COVID-19 symptom onset. None of the investigated factors were significantly associated with workplace attendance after the onset of any symptoms (Table 3).
Table 3.
Predictive factors for attending workplace after onset of any symptoms
| Odds ratio | 95% CI | P-value | |
|---|---|---|---|
| Gender | |||
| Female | 1.00 | – | – |
| Male | 0.69 | 0.33–1.47 | 0.34 |
| Age | |||
| Age 18–29 | 1.00 | – | – |
| Age 30–49 | 1.36 | 0.55–3.33 | 0.51 |
| Age ≥ 50 | 2.00 | 0.64–6.29 | 0.24 |
| Occupation | |||
| Non-office | 1.00 | – | – |
| Office | 1.13 | 0.47–2.72 | 0.78 |
| Non-retail | 1.00 | – | – |
| Retail | 0.92 | 0.36–2.31 | 0.85 |
| Non-construction | 1.00 | – | – |
| Construction | 0.56 | 0.19 – 1.65 | 0.30 |
Workplace attendance after symptom onset and COVID-19 test
Analysis of the recorded dates of testing and attendance at work revealed that five symptomatic staff members attended the workplace after their test date whilst awaiting results (3.8%), although none of these had recorded COVID-19 symptoms. This included three males and two females, all aged between 26 and 36 years old and working in a range of occupations.
Discussion
Main findings
There was no significant trend in London workplace situations associated with symptomatic cases over the eight-week period, despite a steep rise in the final week coinciding with the increase in London-wide COVID-19 cases from early September. The most prevalent occupations were in office, retail and construction, likely influenced by the phased reopening of businesses in London that extended into the study period, and the inability of those in key sectors to work from home.
Of the 130 symptomatic staff members associated with London workplace COVID-19 situations from 17th July to 11th September 2020, 42 (32.3%) attended the workplace after their reported date of symptom onset, including 16 (12.3%) with recorded COVID-19 symptoms. The majority of those who did not attend the workplace with symptoms were male (61.4%), compared to 37.5% of those attending after COVID-19 symptom onset. Univariable logistic regression revealed that males were less likely to attend the workplace after COVID-19 symptom onset compared to females (OR 0.34, 95% CI 0.11–1.00), although this was of borderline statistical significance. Age and occupation were not predictive for workplace attendance after the onset of any symptoms or COVID-19 symptoms. A small minority of symptomatic staff members (3.8%) attended the workplace after being tested for COVID-19 with RT-PCR and whilst awaiting results, although none of these had recorded COVID-19 specific symptoms.
Timely exclusion from work and risk factors
A pre-print time series of cross-sectional online surveys between March and August 2020, including 31 787 people, found that self-reported adherence to self-isolation was low (18.2%, 95% CI 16.4–19.9%). This low compliance rate was derived from asking whether symptomatic respondents had left home since developing symptoms. When respondents were asked about their intention to self-isolate if they were to develop symptoms of COVID-19, compliance was much higher at ~70%. Our analysis, including only symptomatic cases associated with London workplaces, found that the majority did not attend work after symptom onset. Therefore, whilst emerging data has found that many with COVID-19 symptoms were not self-isolating entirely, our findings importantly suggest that workplace attendance is unlikely to be responsible for the majority of this non-compliance.
The study by Smith et al.10 also found that non-adherence to self-isolation was associated with: men, younger age groups, having a dependent child in the household, lower socio-economic grade, greater hardship during the pandemic and working in a key sector.10 In contrast, we found a borderline significant association between being female and attending work after the onset of COVID-19 symptoms. The disparity between men and women in sickness absence has been extensively studied, with women traditionally thought to be responsible for more workplace absences than men.11 A 2019 report by FirstCare shows that the gap in UK sickness absences is closing. The number one cause of absences in the UK in 2019 was mental health, which affected more women than men.12 When looking at sickness absences for colds, cough and flu-like symptoms, men and women are similar. Although surveys have shown that women are more likely to see COVID-19 as a very serious health problem13compared to men, how this relates to workplace attendance after COVID-19 symptom onset appears unclear. An analysis by McKinsey & Company found that women’s jobs are 1.8 times more vulnerable to the pandemic than men’s jobs. Women make up 39% of global employment but account for 54% of overall job losses during the COVID-19 crisis.14 Further research is warranted to better understand how gender relates to workplace attendance after COVID-19 symptom onset, and whether the findings reported here are robust to adjustment for confounders, including age, occupation and socioeconomic status.
We did not find that younger age groups were more likely to attend the workplace after the onset of symptoms. In part this may be as the majority of the study population was relatively young. However, all five cases that attended after testing had been performed were aged 25–36 years, in keeping with previous findings suggesting the young are less likely to follow COVID-19 restrictions compared to the elderly.10,15 Although financial concerns may increase workplace attendance after symptom onset for those in low-income jobs or on zero hours contracts, as acknowledged by the UK self-isolation payment scheme launched toward the end of August16we found no significant differences across the occupations studied. In large part, this is likely as the study population predominantly consisted of individuals working in key sectors, in jobs of relatively similar pay and status.
Strengths and limitations
This study had several important strengths. First, it involves data collected in real-time as part of the health protection response to COVID-19 in London. The dataset is therefore unique in capturing all known COVID-19 workplace situations across London and confirmed symptomatic COVID-19 cases associated with them. Second, unlike much of the existing literature, it did not rely solely on self-reported data. Although dates of symptom onset and dates of workplace attendance were initially self-reported by cases during contact tracing, after escalation to the LCRC, dates of attendance were crosschecked with employers during discussions led by experienced health protection professionals. Third, data were obtained through routine telephone calls made by public health staff to COVID-19 cases and associated workplaces, often on multiple occasions when employers were not contactable initially. Although this involved a degree of voluntary participation, it was an active rather than a passive data collection system, thereby minimizing selection and attrition bias.
The foremost limitation of this study was an inability to adjust for confounders, such as ethnicity and deprivation, when investigating the risk factors for workplace attendance after symptom onset. This was because of a relatively small sample due to the design (not solely reliant on public survey methods) and the true population incidence of COVID-19 associated with workplaces, in a limited geographical area, at a time of severe social restrictions. Secondly, since this was a retrospective study, there was the potential for recall bias. However, this was minimised by checking details given by cases with follow-up discussions with employers or managers. Thirdly, given the time-pressures associated with routine health protection work during an epidemic as well as the need to prioritise, data on specific symptoms were incompletely recorded for some cases. It was cautiously assumed that if unrecorded COVID-19 symptoms were not present, meaning the true proportion of cases attending work after the onset of COVID-19 symptoms may be higher than reported here.
Implications for public health and future research
COVID-19 cases are thought to be most infectious just before or around the time of symptom onset, continuing to be infectious for ~10 days afterwards.17 Our findings emphasize the need for COVID-19 secure workplace practices as well as clear public health messaging around the importance of workplace exclusion and self-isolation at the onset of COVID-19 symptoms. A small number of cases with non-COVID-19 symptoms attended the workplace after testing, suggesting that the messaging on self-isolation after testing (regardless of symptoms) should be strengthened.
Many of those who identified as attending the workplace after symptom onset in our study did not have symptoms included in the COVID-19 case definition; fever, cough or anosmia/aguesia. Although these individuals went on to have a positive test result for COVID-19, current guidance did not mandate self-isolation at symptom onset, due to the nature of their symptoms. Further research is required to understand the implications of continued workplace attendance with symptoms not considered part of the current COVID-19 case definition, and whether they can be involved in disease transmission in workplace settings. The incidence of other viral respiratory diseases presenting with similar symptoms will increase over winter.18 It may not be practical or feasible to provide COVID-19 testing to all those with a range of mild symptoms. If non-specific symptoms (such as fatigue, myalgia or sore throat) commonly reported in COVID-1919 are found to play a role in COVID-19 transmission, then prompt exclusion from work may help to prevent and control institutional COVID-19 outbreaks.
When investigating risk factors for workplace attendance after COVID-19 symptom onset, future studies must attempt to adjust for important confounders including age, gender and socioeconomic status. Work schedule must also be considered, as it may be that those who did not attend work after symptom onset were not scheduled to. If this is the case, then there is a risk of overestimating compliance with self-isolation and workplace exclusion. To build the rich datasets that would allow such research, closer collaboration with employers may be necessary through prospective studies that are able to minimize recall bias.
Conclusions
Over the 8-week study period, the majority of symptomatic COVID-19 cases associated with workplaces in London did not attend the workplace after reported symptom onset. A total of 42 (32.3%) cases attended the workplace after their reported date of symptom onset, including 16 (12.3%) with recorded COVID-19 symptoms. Five staff members (3.8%) attended after non-COVID-19 symptom onset and COVID-19 RT-PCR testing. Males were borderline significantly less likely to attend the workplace after the onset of COVID-19 symptoms. Age and occupation were not strongly predictive for workplace attendance after the onset of any symptoms or COVID-19 symptoms. Further research is required to better understand the risk factors for workplace attendance after COVID-19 symptom onset. This study highlights the need for ongoing COVID-19 secure workplace practices and prompt self-isolation after COVID-19 symptom onset or testing.
Acknowledgements
We are extremely grateful to all staff members working for the LCRC during the period of study.
Vageesh Jain, Public Health Registrar (ST3)
Maria Waghorn, Academic Clinical Fellow in Public Health, UCL
Rachel Thorn-Heathcock, Consultant in Communicable Disease Control
Peter Lamb, Consultant in Health Protection
Anita Bell, Consultant in Health Protection
Sarah Addiman, Consultant in Health Protection
Contributor Information
Vageesh Jain, North East North Central London Health Protection Team & London Coronavirus Response Centre, Public Health England, SE1 8UG, UK; Academic Clinical Fellow in Public Health, University College London, WC1E 7HB, UK.
Maria Waghorn, North East North Central London Health Protection Team & London Coronavirus Response Centre, Public Health England, SE1 8UG, UK.
Rachel Thorn-Heathcock, South London Health Protection Team & London Coronavirus Response Centre, Public Health England, SE1 8UG, UK.
Peter Lamb, North East North Central London Health Protection Team & London Coronavirus Response Centre, Public Health England, SE1 8UG, UK.
Anita Bell, North East North Central London Health Protection Team & London Coronavirus Response Centre, Public Health England, SE1 8UG, UK.
Sarah Addiman, North East North Central London Health Protection Team & London Coronavirus Response Centre, Public Health England, SE1 8UG, UK.
References
- 1. European Centre for Disease Prevention and Control (ECDC) . COVID-19 Clusters and Outbreaks in Occupational Settings in the EU/EEA and the UK. 2020. Available at: https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-in-occupational-settings.pdf (24September 2020, date last accessed).
- 2. gov.uk . Prime Minister's Statement on Coronavirus (COVID-19): 17 July 2020. 2020. Available at: https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-17-july-2020 (25 September 2020, date last accessed).
- 3. The Guardian . Suspected Covid-19 Outbreaks in English Workplaces Double in a Week. 2020. Available at: https://www.theguardian.com/society/2020/jul/02/suspected-covid-19-outbreaks-in-english-workplaces-double-in-a-week (07 September 2020, date last accessed).
- 4. Sky News . Coronavirus: Why are COVID-19 Outbreaks Happening in Food Factories? 2020. Available at: https://news.sky.com/story/coronavirus-why-are-covid-19-outbreaks-happening-in-food-factories-12058673 (25 September 2020, date last accessed).
- 5. Office for National Statistics . Coronavirus, the UK Economy and Society, Faster Indicators: 23 April 2020. 2020. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronavirustheukeconomyandsocietyfasterindicators/23april2020 (07 September 2020, date last accessed).
- 6. BBC . Coronavirus: Campaign to Encourage Workers Back to Offices. 2020. Available at: https://www.bbc.co.uk/news/uk-53942542 (30 August 2020, date last accessed).
- 7. Public Health England . Stay at Home: Guidance for Households with Possible or Confirmed Coronavirus (COVID-19) Infection. 2020. Available at: https://www.gov.uk/government/publications/covid-19-stay-at-home-guidance/stay-at-home-guidance-for-households-with-possible-coronavirus-covid-19-infection (30 August 2020, date last accessed).
- 8. The Guardian . London is Still the UK’s Golden Goose – and that Needs to Change. 2019. Available at: https://www.theguardian.com/commentisfree/2019/may/20/london-uk-economy-decentralisation (07 September 2020, date last accessed).
- 9. Greater London Authority . A Description of London's Economy. 2017. Available at: https://www.london.gov.uk/sites/default/files/description-londons-economy-working-paper-85.pdf (07 September 2020, date last accessed).
- 10. Smith L, Potts H, Amlot R, Fear N, Michie S, Rubin J. Adherence to the Test, Trace and Isolate System: Results from a time Series of 21 Nationally Representative Surveys in the UK (the COVID-19 Rapid Survey of Adherence to Interventions and Responses [CORSAIR] Study). 2020. Available at: https://www.medrxiv.org/content/10.1101/2020.09.15.20191957v1.full.pdf (25 September 2020, date last accessed).
- 11. Casini A, Godin I, Clays E, Kittel F. Gender difference in sickness absence from work: a multiple mediation analysis of psychosocial factors. Eur J Public Health 2013;23(4):635–42. [DOI] [PubMed] [Google Scholar]
- 12. FirstCare . UK Workforce Absence Trends 2019 Review. 2019. Available at: https://www.firstcare.uk/download-index-report-2019 (24 September 2020, date last accessed).
- 13. Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 related attitudes and behavior: Evidence from a panel survey in eight OECD countries. NBER Working Paper. 2020 Jun(w27359). [DOI] [PMC free article] [PubMed]
- 14. McKinsey & Company . COVID-19 and Gender Equality: Countering the Regressive Effects. 2020. Available at: https://www.mckinsey.com/featured-insights/future-of-work/covid-19-and-gender-equality-countering-the-regressive-effects (26 September 2020, date last accessed).
- 15. Nuffield Foundation . More than Half of Young Adults Not ‘Strictly’ Sticking to Lockdown Guidelines. 2020. Available at: https://www.nuffieldfoundation.org/news/more-than-half-of-young-adults-not-strictly-sticking-to-lockdown-guidelines (26 September 2020, date last accessed).
- 16. BBC . Coronavirus: Self-Isolation Payment for Low-Income Workers. 2020. Available at: https://www.bbc.co.uk/news/uk-53926977 (24 September 2020, date last accessed).
- 17. European Centre for Disease Prevention and Control (ECDC) . Transmission of COVID-19. 2020. Available at: https://www.ecdc.europa.eu/en/covid-19/latest-evidence/transmission (27 September 2020, date last accessed).
- 18. European Centre for Disease Prevention and Control (ECDC) . Coronaviruses. 2020. Available at: https://www.ecdc.europa.eu/en/covid-19/latest-evidence/coronaviruses (27 September 2020, date last accessed).
- 19. Sudre CH, Lee K, Lochlainn MN, Varsavsky T, Murray B, Graham MS, Menni C, Modat M, Bowyer RC, Nguyen LH, Drew DA. Symptom clusters in Covid19: A potential clinical prediction tool from the COVID Symptom study app. MedRxiv 2020. Jan 1. [DOI] [PMC free article] [PubMed]


