Abstract
Inhaled corticosteroids (ICS), prednisolone and antibiotics all play a crucial role in the management of respiratory diseases. The aim of this study was to analyse whether the declaration of the COVID-19 pandemic affected prescribing rates, as public health measures were implemented to reduce transmission of SARS-CoV-2. Monthly practise-level prescribing data published by NHS Digital were analysed. At the point, the COVID-19 outbreak was declared a pandemic, ICS prescriptions rose significantly. This was followed by a decrease in ICS and prednisolone prescribing in the following months. There was no difference in the antibiotic prescribing trend.
Keywords: antibiotics, COVID-19, inhalers, prednisolone, prescribing
Introduction
Inhaled corticosteroids (ICS) and prednisolone are used in the treatment of respiratory diseases including asthma and chronic obstructive pulmonary disease.1,2 They improve lung function, symptoms and quality of life, and reduce exacerbations. Antibiotics are often prescribed in respiratory disease during periods of infection (upper or lower, including pneumonia) or exacerbations.3
On 11 March, the WHO declared that the novel SARS-CoV-2 virus was at pandemic levels. In the UK, a number of public health measures such as social distancing and lockdown were introduced to minimize viral transmission. We sought to assess whether or not the initial outbreak of COVID-19 was associated with a change in the prescription rates of ICS, prednisolone and antibiotics in primary care in England.
Methods
The data were extracted using the OpenPrescribing (https://openprescribing.net/) database from January 2017 to October 2020. OpenPrescribing provides a search interface onto the raw monthly practise-level prescribing data published by NHS Digital making access to this complex information easier. We used prescribed ‘items’ as a measure of prescribing. A prescription item refers to a single supply of medicine prescribed on a prescription form. If a prescription form includes three medicines, it is counted as three prescription items. Interrupted time series analysis (ITSA) allows the effect of interventions to be analysed taking into account underlying trends. We conducted ITSA using segmented least-squares regression with the number of prescribed items per 1000 registered patients per month as the dependent variable and adjusted for seasonality by including each calendar month as an independent variable in the model. We set the ‘intervention’ time as March 2020, the month of the declaration of COVID-19 as a pandemic by the WHO. All data management and statistical analyses were performed in R v4.0.3 and significance level alpha was set to 0.05.
Results
ITSA results are presented in both tabular (Table 1) and graph (Fig. 1) formats. At the beginning of the observation period, the monthly rate of ICS prescription was 28.8 per 1000 registered patients (from 95%CI 27.8 to 29.8; P < 0.001). The declaration of COVID-19 as a pandemic coincided with an abrupt increase by 8 ICS prescriptions per 1000 patients ( from 95%CI 5 to 11). Thereafter, ICS prescriptions decreased monthly by −1.1 (from 95%CI: −1.7 to −0.6; P < 0.0001) per 1000 registered patients which is a greater decreased trend compared to the pre-pandemic period. The rate of prednisolone prescribing was relatively constant, at around 10.3 per 1000 per registered patients per month (coefficient = −0.01, P = 0.11). There was no change when the pandemic was declared (P = 0.08), but there was a decreased month-to-month trend of −0.4 (from 95%CI -0.6 to −0.1; P < .01) per 1000 registered. The trend of antibiotic prescribing was not affected by the pandemic (P = 0.15).
Table 1.
Change in the number of prescriptions per 1000 registered patients in England according to the seasonal adjusted segmented regression models considering as intervention the declaration of COVID-19 as pandemic in March 2020.
| Coefficients | 95%CI | P-value | |
|---|---|---|---|
| ICS prescriptions per 1000 patientsa | |||
| Intercept | 28.8 | 27.8 to 29.8 | <0.0001 |
| Baseline trend | −0.1 | −0.1 to −0.01 | 0.017 |
| Level change after the intervention | 8.0 | 5 to 11 | <0.0001 |
| Trend changes after the intervention | −1.1 | −1.7 to −0.6 | <0.0001 |
| Prednisolone prescriptions per 10 00 patients | |||
| Intercept | 10.3 | 9.9 to 10.7 | <0.0001 |
| Baseline trend | −0.01 | −0.03 to 0.03 | 0.11 |
| Level change after the intervention | 1.3 | −0.1 to 2.2 | 0.08 |
| Trend change after the intervention | −0.4 | −0.6 to −0.1 | 0.002 |
| Antibiotics prescriptions per 10 00 patientsb | |||
| Intercept | 20.8 | 19.8 to 21.8 | <0.0001 |
| Baseline trend | −0.1 | −0.2 to −0.1 | <0.0001 |
| Level change after the intervention | 0.6 | −2.2 to 3.3 | 0.7 |
| Trend change after the intervention | −0.5 | −0.1 to 0.01 | 0.053 |
aFluticasone Propionate, Budesonide, Beclomethasone Dipropionate, Ciclesonide, Mometasone Furoate.
bAmoxicillin, Doxycycline, Co-Amoxiclav, Erythromycin.
Fig. 1.
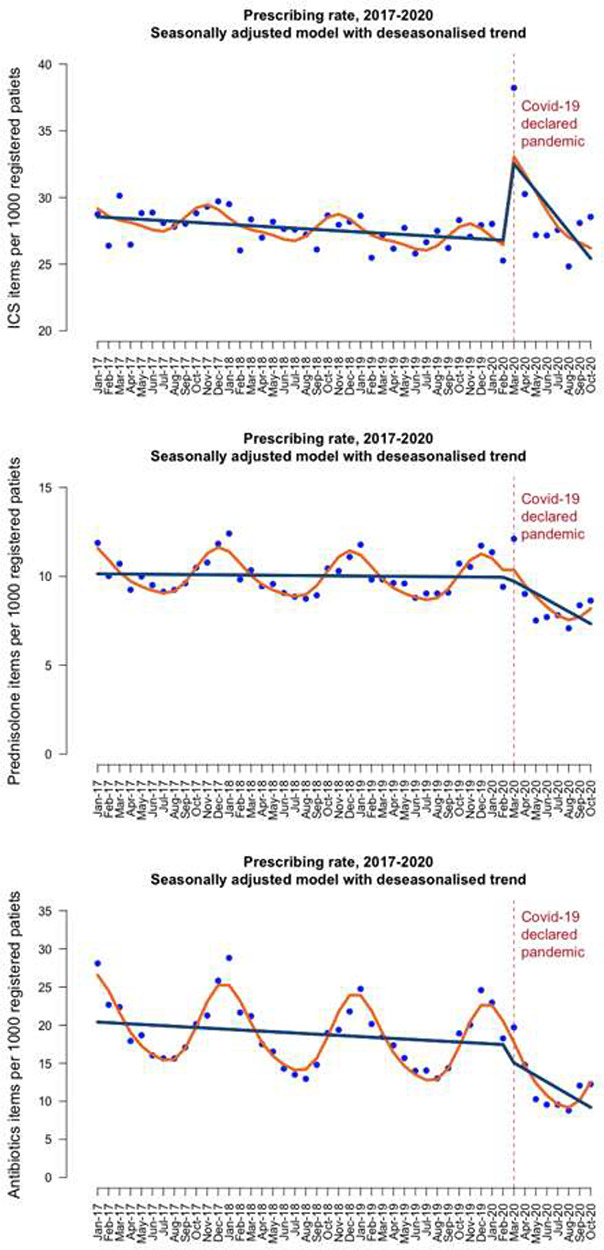
Seasonal model of primary care prescribing rates per 1000 registered patients across England for inhaled corticosteroids (top), prednisolone (middle), and antibiotics (bottom) from January 2017 to October 2020. Wavy line shows the predicted trend based on the seasonally adjusted regression model; Straight line shows the deseasonalised trend.
Discussion
Our results suggest that the COVID-19 pandemic was associated with a large initial increase in ICS prescriptions, followed by a decline towards the baseline. Antibiotic and prednisolone prescription rates fell. The obvious explanation for these findings is that adherence to ICS increased at the early stages of the pandemic, perhaps in response to fears that people with airways disease were more at risk of COVID-19. However, antibiotic and prednisolone prescription rates were not affected indicating that there was no increased rate of airways disease exacerbations in the community, and lockdown (or increased compliance) was associated with reduced viral transmission. Lockdown had a profound effect on the prevalence of normal viral pathogens, including influenza, RSV, rhinovirus, metapneumovirus and paraflu.4,5
Prescription rates of the antibiotics, prednisolone and ICS were relatively stable over the time course of our study and show seasonal variation, which is unsurprising given that most respiratory viruses are more prevalent in the winter. Establishing whether the apparent drop in airways disease exacerbations was due to better compliance or the effects of social distancing are difficult. Other authors have described an increased rate of compliance with inhaled medication during the pandemic6 and there has been debate about whether ICS are protective, or not, against COVID-19.7,8 Our data support the notion that many patients with airways disease are not fully complaint with therapy9; it is unlikely that stark increase in ICS prescriptions was due to new diagnoses of airways disease at the same time point. Appropriate use of daily controller medications is important for patients with respiratory illnesses during the COVID-19 pandemic.10 A key strength of our analysis is that it covers a time period of several years and complete data for all prescription items dispensed in England. A weakness is that a prescription does not equate to actual activation (or good technique) with an inhaler.
Analysing prescription trends and their relationship with outcomes such as admission, other medication use and hospital attendances could offer insight into the effect of large-scale interventions. For example, the impact from the introduction of monoclonal therapies on population prednisolone use, or the potential effect of moving to combined long-acting beta-agonist/ICS on salbutamol use could be measured, helping stakeholders establish the true effect size of such interventions, outside clinical trials.
Authors’ Contributors
C.V.C. had full access to all the study data and takes full responsibility for the integrity of the data and the accuracy of the data analysis. Conception and design: T.M.M., D.E.S.; acquisition of data: C.V.C.; analysis of data: C.V.C.; interpretation of data: C.V.C., T.M.M., T.E.L., D.E.S.; drafting the article: C.V.C., D.E.S.; revision for important intellectual content: C.V.C., T.M.M., D.E.S. All authors approved this version to be published.
Data availability
All the datasets and R scripts are available on the https://doi.org/10.6084/m9.figshare.13482318
Conflict of Interest
None declared.
Funding
None declared.
Christos V. Chalitsios, PhD candidate & research assistan
Tricia M. McKeever, Prof. of Epidemiology & Medical Statistics
Tessa E. Langley, Associate Prof. of Health Economics
Dominick E. Shaw, Prof. of Respiratory Medicine
Contributor Information
Christos V Chalitsios, Division of Respiratory Medicine, Clinical Science Building, School of Medicine, University of Nottingham, Nottingham NG5 1PB, UK; Division of Epidemiology and Public Health, Clinical Science Building, School of Medicine, University of Nottingham, Nottingham NG5 1PB, UK.
Tricia M McKeever, Division of Epidemiology and Public Health, Clinical Science Building, School of Medicine, University of Nottingham, Nottingham NG5 1PB, UK.
Tessa E Langley, Division of Epidemiology and Public Health, Clinical Science Building, School of Medicine, University of Nottingham, Nottingham NG5 1PB, UK.
Dominick E Shaw, Division of Respiratory Medicine, Clinical Science Building, School of Medicine, University of Nottingham, Nottingham NG5 1PB, UK.
References
- 1. Global Initiative for Asthma (GINA) . Global strategy for asthma management and prevention. Global Initiative for Asthma, Fontana-on-Geneva Lake, WI, 2020.
- 2. Global Initiative for Chronic Obstructive Lung Disease . 2021. https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf (2 February 2021, date last accessed)
- 3. Hill AT, Gold PM, El Solh AA et al. Adult outpatients with acute cough due to suspected pneumonia or influenza: CHEST guideline and expert panel report. Chest 2019;155(1):155–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hatoun J, Correa ET, Donahue SMA et al. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics 2020;146(3):e2020006460. [DOI] [PubMed] [Google Scholar]
- 5. Royal College of General Practitioners . RSC: communicable and respiratory disease report for England. 2020. https://www.rcgp.org.uk/-/media/Files/CIRC/WeeklyReport_Summer_wk31_2020.ashx (2 February 2021, date last accessed).
- 6. McAuley H, Hadley K, Elneima O et al. COPD in the time of COVID-19: an analysis of acute exacerbations and reported behavioural changes in patients with COPD. ERJ Open Res In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Halpin DMG, Singh D, Hadfield RM. Inhaled corticosteroids and COVID-19: a systematic review and clinical perspective. Eur Respir J 2020;55:2001009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singh D, Halpin DMG. Inhaled corticosteroids and COVID-19-related mortality: confounding or clarifying? Lancet Respir Med 2020;8(11):1065–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jentzsch NS, Camargos P, Sarinho ESC et al. Adherence rate to beclomethasone dipropionate and the level of asthma control. Respir Med 2012;106:338–43. [DOI] [PubMed] [Google Scholar]
- 10. Shaker MS, Oppenheimer J, Grayson M et al. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract 2020;8(5):1477–1488.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the datasets and R scripts are available on the https://doi.org/10.6084/m9.figshare.13482318


