Abstract
Background
Electronic health (e-health) approaches such as telemedicine, mobile health, virtual healthcare and electronic health records are considered to be effective in increasing access to healthcare services, reducing operational costs and improving the quality of healthcare services during the coronavirus disease 2019 (COVID-19) outbreak, a pandemic resulting from the spread of a novel coronavirus discovered in December 2019. In this context, the aim of this study was to identify the most important factors influencing decision making on the implementation of e-health in Gulf Cooperation Council (GCC) member states (Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and the United Arab Emirates), which are in the process of digitizing healthcare services.
Methods
This study reviewed the literature to identify the important factors influencing decision making on e-health. In addition, a questionnaire-based survey was conducted in order to identify the most important criteria to be considered in decision making on e-health. The survey link was forwarded to 978 healthcare practitioners and 42 experts (purposive sampling), from which a final sample of 892 (864 practitioners and 28 experts) was achieved, reflecting a response rate of 87.45%.
Results
Of the 44 factors identified under seven themes (strategic, quality, management, technology, function characteristics, economic, sociocultural and demographic factors), 22 factors were identified to be the most important criteria.
Conclusions
Findings from this study suggest that decision making in relation to e-health is a complex process that requires consideration of various factors. It was also found that attention should be paid to sociocultural and demographic factors, which may need to be considered in increasing healthcare access during the COVID-19 outbreak.
Keywords: COVID-19, decision making, e-health, healthcare services
Introduction
The goal of the healthcare system in any country is to facilitate access to healthcare services and support healthy lifestyles so that people can effectively participate in socio-economic activities.1 However, the complexity of healthcare infrastructure, the competitive economy of healthcare operations and services and the need to deliver high-quality services can lead to continuous development and reengineering of healthcare operations, strategies, goals and managerial approaches.2 The coronavirus disease 2019 (COVID-19) pandemic has strained the healthcare systems in many countries, affecting individuals suffering from other diseases due to the limitations in healthcare resources, finance and operations management.3–5 In addition, the confirmed COVID-19 cases have been steadily increasing since it emerged in China in December 2019. As of 24 August 2020, there are 31.4 million COVID-19 cases with 967 164 deaths globally.6 The rising number of cases may create additional burdens on healthcare resources that may further affect already strained healthcare systems across the globe.
The Gulf Cooperation Council (GCC) member states have implemented various proactive plans and timely decisions to limit the spread of infection in response to the COVID-19 outbreak, such as suspension of flights, closure of educational institutes, curfews and lockdowns of major cities and provision of free-of-charge healthcare to patients.7,8 However, in the past few months there has been a steady increase in cases in all the member states,6 which is one of the major concerns affecting healthcare management. The COVID-19 outbreak has severely affected the healthcare industry in the GCC states. There was 50% decrease in visits to emergency departments, a 50% decrease in regular care services, an 80% decrease in outpatient admissions, a 50% decrease in inpatient admissions and a decrease of 70% in primary care and 65% in secondary care delivery services.11 As a result, access to primary and secondary healthcare services were severely affected, which may affect patients suffering from chronic diseases and those who require regular diagnosis and monitoring of diseases such as diabetes, coronary heart diseases, dialysis etc.
Reliance on e-health approaches such as telemedicine, mobile health, online consultation and remote monitoring may reduce the burden on the delivery of healthcare services and provide support for patients suffering from chronic diseases. However, most of the GCC member states are in the process of digitization of the healthcare industry, which may be one of the challenges in the implementation of e-health.7,8 There is wide range of factors that can impact the implementation of e-health approaches such as telemedicine. These can be categorized under various themes or categories, including organizational (funding, training, processes), technological (risk, security, privacy, infrastructure) and social (insurance, user acceptance, regulations), for effective management of the challenges associated with these factors.9,10 Other factors such as internet connectivity, mobile usage, awareness of the people in relation to e-health services and privacy and security concerns are a few factors that can affect the implementation of e-health services.12,13 As a result, there is a need for shared decision making14 in identifying the factors that should be considered in implementing e-health strategies for improving the delivery of healthcare services.15 This article focuses on identifying the most important criteria affecting decision making in implementing e-health strategies in GCC member states.
Literature review
Various studies16–20 were identified that have investigated factors affecting the decision making on e-health implementation. Factors related to system function such as ease of use, accuracy, privacy and security; quality factors such as training and specialization; and integration factors such as compatibility and flexibility were identified to be important in evaluating health information systems.16 These factors are considered to be very important given the rising impact of COVID-19 across the globe, which led to a rapid increase in the adoption of e-health applications in the past few months. The sudden increase in e-health adoption has led to increased stress on policy makers and healthcare service delivery organizations, as they have to consider various factors and address various issues in developing e-health technologies with immediate need. Factors including strategic (core business, flexibility, image), economic (cost reduction, economies of scale, growth), technical (skill, management of operational processes, new products) and geopolitical (distance, political issues, language barriers) were identified to be influencing decision making in outsourcing e-health applications in Iran.17 In addition, an attempt was made in Saudi Arabia18 to categorize various factors, including management factors (save management time, reduce management load, need for specialized management, increase the speed of implementation, function difficult to manage, safety management, consolidation or decentralization);
technological factors (achieve flexibility with changing technology, initiate innovative ideas and techniques, Improve the technology for competitive advantage, technology requirements, uncertainty, need for specialized expertise, acquire new skills or technical knowledge); and function characteristics (complexity of function, function integration and structure, lack of spare parts, function difficult to control).18
Analyses of the factors in various studies have not only considered the technical aspects, but also all other factors, including management, functional characteristics, economic, strategic and quality. Using a systematic review, 29 subfactors affecting decision making on e-health-related services were identified under four main factors: strategic, quality, management and technological.2 In contrast, influencing factors were analysed based on their priority among healthcare professionals, health information professionals and managers, who identified that service-related factors were preferred by healthcare professionals while operational factors were preferred by managers.19 However, these studies have undermined the influence of sociocultural and demographic factors, such as population demographics, religion, social norms and lifestyles,20,21 which may also influence decision making on e-health. Considering the growing impact of COVID-19 and increasing reliance on e-health technologies, it is of immediate importance to identify the various factors affecting decision making on e-health in different geopolitical and cultural contexts so that necessary and effective strategies can be developed to improve the e-health implementation process, which can improve the healthcare service accessibility during the COVID-19 outbreak.
Studies22–29 have identified challenges that can influence the implementation of e-health approaches. For instance, introducing new e-health technologies in healthcare are essential for improving efficiency, but at the same time it is also essential to train both healthcare practitioners and people to use these technologies.22 With an increased stress and work burden on healthcare workers from treating COVID-19 patients, there is a need to systematically organize training programs without affecting healthcare service delivery. Focusing on the challenges involved with technology adoption, the older population may not be aware (technical skills) of the new technologies and may not be able (physically) to use these technologies, which may impact the implementation of e-health approaches and healthcare services during the pandemic. Focusing on the GCC member states, including Saudi Arabia and the United Arab Emirates (UAE), issues related to information technology infrastructure, policies and regulations, cultural acceptance, finance management and resource (personnel) management were a few of the challenges identified in implementing e-health.23,24 Issues such as user adoption (satisfaction and ease of use), training, privacy and security were the major issues identified that are influencing the implementation of e-health applications in GCC member states.25,26 Trust, health literacy, internet literacy and users’ attitudes were other factors affecting e-health adoption in Bahrain27 and Kuwait.28
Methods
The purpose of this study is to identify the important factors affecting decision making in implementing e-health strategies in GCC member states during the COVID-19 pandemic. To achieve this objective, an online questionnaire-based survey was used to collect data related to major factors, including strategic, quality, management, technological, functional characteristics and economic, that influence decision making on e-health strategies.2 In addition, sociocultural and demographic factors were included in the questionnaire. The questionnaire was designed using different factors/items in relation to these components, including seven items related to strategic factors, three items on technology factors, three items on function characteristics, seven items on economic factors and 13 items on sociocultural and demographic factors. Each item was designed to be rated using 5-point Likert scale29 (1, strongly disagree; 2, disagree; 3, neutral; 4, agree; 5, strongly agree). The questionnaire was initially designed in English, a copy of which is in Appendix A. The questionnaire was then translated into Arabic using two professional Arabic translators. The Arabic version of the questionnaire was designed using the QuestionPro application (QuestionPro, Austin, TX, USA) and a survey link was generated for accessing the survey. A pilot study was conducted with eight healthcare practitioners (six nurses, two healthcare information professionals, two physicians). Based on the feedback from the pilot study participants, a few changes were made in relation to the questions’ formulation and grammatical errors in Arabic were addressed. In addition, Cronbach's α for all items in four components was identified to be >0.83, revealing good consistency. Ethical approval was obtained from the institutional review board of the Imam Abdulrahman Bin Faisal University (Damman, Saudi Arabia) and informed consent was obtained from each participant before beginning the survey, where they checked a box providing their consent (agree and continue) to participate after reading a brief introduction.
Recruitment
Healthcare practitioners, including nurses, physicians, healthcare information professionals, managers and professionals (decision makers) working under the Ministry of Health (MoH) in different GCC member states, were recruited through e-mails and social networking platforms, including WhatsApp and Facebook. In addition, professional online communities were used to forward the survey link in all the member states. The survey was conducted for a period of 4 weeks from 22 August to 11 September 2020.
Sample
Considering the purpose and objective of the study, which was to collect data from a specific group (healthcare practitioners and experts in e-health decision making), a purposive sampling approach was adopted.30 Accordingly, a non-probability sample was obtained based on the objective of the study, which mainly focused on identifying the factors affecting decision making on e-health strategies during the COVID-19 pandemic. The survey link was initially forwarded to 978 healthcare practitioners and 42 experts, of which 91 practitioners completed only part of the survey and 23 practitioners and 14 experts did not start the survey. After removing 154 incomplete responses, a final sample of 892 (864 practitioners and 28 experts) was achieved, reflecting a response rate of 87.45%. The sample was almost evenly distributed across the GCC member states: Saudi Arabia (186/892 [20.8%]), Oman (102/892 [11.4%]). Bahrain (135/892 [15.1%]), Kuwait (155/182 [17.4%]), Qatar (143/892 [16%]) and UAE (171/892 [19.2%]).
Analytical process
The survey was developed using the QuestionPro application31–32 and conducted for a period of 4 weeks. The data were analysed using seven themes: strategic, quality, management, technological, functional characteristics, economic and sociocultural and demographic factors. Relative frequencies for each item under these themes were used for analysing the data, which are presented in the following section.
Results
The final sample achieved for the study was 892. The demographic information of the participants is presented in Table 1. Among the participants, 28.4% were female (253/892) and 71.6% were male (639/892). Considering the age groups, 55.1% were 35–44 y (492/892), 35.9% were 25–34 years (321/892), 4.3% were 18–24 y (38/892), 3.9% were 45–54 y (35/892) and 0.6% were >54 y (6/892). Focusing on the education levels of the participants, 47.3% (422/892) had a bachelor's degree, 38.3% (342/892) had a master's degree, 6.5% (58/892) had a PhD, 6.3% (56/892) had a diploma and 1.6% (14/892) had other educational qualifications. Focusing on the professions of the participants, 39.3% (351/892) were nurses, 26.2% (234/892) were physicians, 1.4% (13/892) were information professionals, 12.4% (111/892) were consultants, 15.7% (140/892) were managers and 3.1% (28/892) worked for the MoH. Focusing on the participants’ work experience, 46.4% (414/892) had 5–10 y work experience, 26.5% (237/892) had 2–5 y experience, 17.4% (155/892) had >10 y experience and 9.6% (86/892) had <5 y experience. It should be noted that most of the participants were highly experienced and it is assumed they would have greater awareness of healthcare operations.
Table 1.
Frequency distribution of key variables
| Variables | n (%) |
|---|---|
| Gender | |
| Male | 639 (71.6) |
| Female | 253 (28.4) |
| Age (years) | |
| 18–24 | 38 (4.3) |
| 25–34 | 321 (35.9) |
| 35–44 | 492 (55.1) |
| 45–54 | 35 (3.9) |
| >54 | 6 (0.6) |
| Education | |
| Diploma | 56 (6.3) |
| Bachelor's degree | 422 (47.3) |
| Master's degree | 342 (38.3) |
| PhD | 58 (6.5) |
| Other | 14 (1.6) |
| Profession | |
| Consultant | 111 (12.4) |
| Physician | 234 (26.2) |
| Nurse | 351 (39.3) |
| Information professional | 13 (1.4) |
| Manager | 140 (15.7) |
| Other (MoH) | 28 (3.1) |
| Work experience (years) | |
| <2 | 86 (9.6) |
| 2–5 | 237 (26.5) |
| 5–10 | 414 (46.4) |
| >10 | 155 (17.4) |
Table 2 presents the responses of the participants towards various strategic factors influencing decision making on e-health. All the provided factors were identified to be important by the majority of the participants. Participants identified factors including focus on core function (strongly agree, 35.3%; agree, 40.9%), accelerating re-engineering benefits (strongly agree, 39.9%; agree, 39.6%) and regulations (strongly agree, 46.2%; agree, 30.7%) as highly important.
Table 2.
Frequency distribution of responses for strategic factors
| Items | Strongly agree, % | Agree, % | Neutral, % | Disagree, % | Strongly disagree, % |
|---|---|---|---|---|---|
| Focus on core function | 35.3 | 40.9 | 6.9 | 7.2 | 9.6 |
| Access to world class capabilities | 35.2 | 27.6 | 20.7 | 7.1 | 9.4 |
| Freeing resources for core activities | 32.0 | 16.9 | 28.7 | 8.4 | 14.0 |
| Accelerate reengineering benefits | 39.9 | 39.6 | 7.0 | 3.7 | 9.8 |
| Improve flexibility versus change | 29.0 | 32.2 | 11.3 | 18.4 | 9.1 |
| Risk sharing | 35.3 | 26.6 | 10.3 | 9.5 | 18.3 |
| Regulations governing | 46.2 | 30.7 | 3.0 | 14.5 | 5.6 |
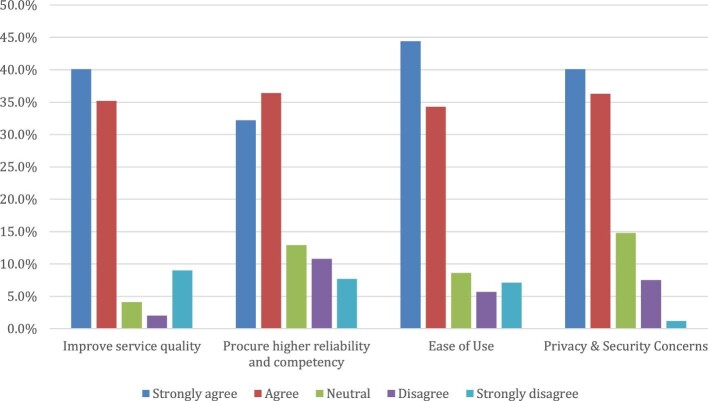
Figure 1 presents the responses of the participants towards various quality factors influencing decision making on e-health. All the provided factors were identified as important by the majority of the participants, including improving service quality (strongly agree, 40.1%; agree, 35.2%), ease of use (strongly agree, 44.4%; agree, 34.3%) and privacy and security concerns (strongly agree, 40.1%; agree, 36.3%) as highly important.
Figure 1.
Frequency distribution of responses for quality factors
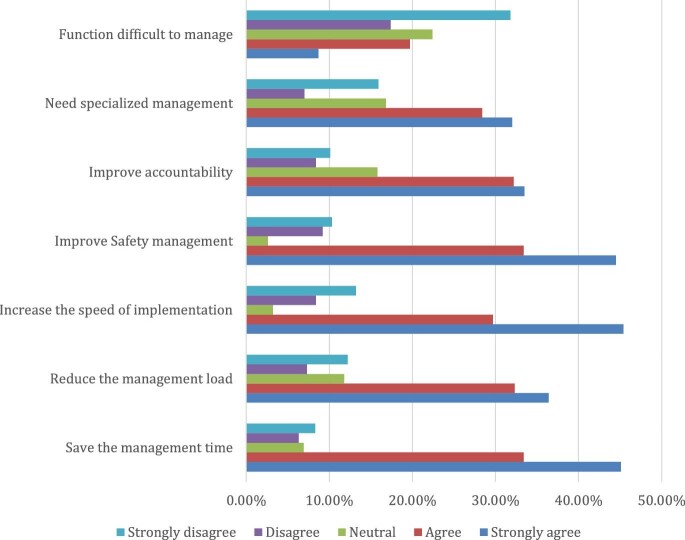
Figure 2 presents the responses of the participants towards various management factors influencing decision making on e-health. Most of the provided factors were identified as important by the majority of the participants, including saving management time (strongly agree, 45.1%; agree, 33.4%), increasing speed of implementation (strongly agree, 45.4%; agree, 29.7%) and improving safety management (strongly agree, 44.5%; agree, 33.4%). However, very few participants identified that the function (e-health) was difficult to manage (strongly agree, 8.7%; agree, 19.7%).
Figure 2.
Frequency distribution of responses for management factors
Table 3 presents the responses of the participants towards various technology factors influencing decision making on e-health. All the provided factors were identified as important by the majority of the participants, including achieving flexibility with changing technology (strongly agree, 36.4%; agree, 39.7%) and acquiring new skills and knowledge (strongly agree, 33%; agree, 42%).
Table 3.
Frequency distribution of responses for technology factors and function characteristics
| Items | Strongly agree, % | Agree, % | Neutral, % | Disagree, % | Strongly disagree, % | |
|---|---|---|---|---|---|---|
| Technology factors | Achieve flexibility with changing technology | 36.4 | 39.7 | 7.1 | 5.0 | 11.8 |
| Achieve innovative ideas | 34.2 | 27.5 | 14.0 | 11.0 | 13.3 | |
| Acquire new skills or technical knowledge | 33.0 | 42.0 | 11.1 | 5.0 | 8.9 | |
| Function characteristics | Complexity of function | 39.7 | 38.2 | 4.2 | 7.3 | 10.6 |
| Function integration and structure | 47.7 | 28.5 | 2.0 | 8.7 | 13.1 | |
| Function difficult to control | 16.4 | 13.8 | 18.5 | 31.0 | 20.3 |
Table 3 also presents the responses of the participants towards various function characteristics influencing decision making on e-health. Most of the provided factors were identified as important by the majority of the participants, including complexity of function (strongly agree, 39.7%; agree, 38.2%) and function integration and structure (strongly agree, 47.7%; agree, 28.5%). However, very few participants identified that function (e-health) was difficult to control (strongly agree, 16.4%; agree, 13.8%).
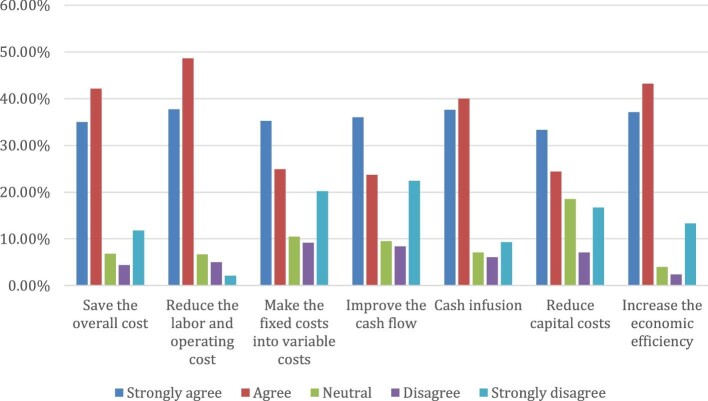
Figure 3 presents the responses of the participants towards various economic factors influencing decision making on e-health. All the provided factors were identified as important by the majority of the participants, including saving overall cost (strongly agree, 35%; agree, 42.1%), reducing labour and operational costs (strongly agree, 37.7%; agree, 48.6%), cash infusion (strongly agree, 37.6%; agree, 40%) and increasing economic efficiency (strongly agree, 37.1%; agree, 43.2%).
Figure 3.
Frequency distribution of responses for economic factors
Table 4 presents the responses of the participants towards various sociocultural and demographic factors influencing decision making on e-health. All the provided factors were identified as important by the majority of the participants, including age (strongly agree, 45.4%; agree, 35%), prevalence of chronic diseases (strongly agree, 48.9%; agree, 36.8%), acceptance of technology (strongly agree, 37.6%; agree, 34.6%), awareness of e-health (strongly agree, 41.7%; agree, 45.3%) and religious and social norms (strongly agree, 45.6%; agree, 32.8%).
Table 4.
Frequency distribution of responses for sociocultural and demographic factors
| Items | Strongly agree, % | Agree, % | Neutral, % | Disagree, % | Strongly disagree, % |
|---|---|---|---|---|---|
| Age | 45.4 | 35.0 | 6.3 | 9.8 | 3.5 |
| Gender | 33.4 | 37.3 | 11.0 | 8.4 | 9.9 |
| Education | 31.1 | 40.9 | 9.8 | 11.0 | 7.3 |
| Income | 28.5 | 33.7 | 11.8 | 5.0 | 21.0 |
| MMR | 30.0 | 33.5 | 12.6 | 7.7 | 16.1 |
| Ethnicity | 31.3 | 32.4 | 13.8 | 4.8 | 17.7 |
| Place of residence (urban/rural) | 27.0 | 31.2 | 12.1 | 9.5 | 20.2 |
| Prevalence of chronic diseases | 48.9 | 36.8 | 2.4 | 7.4 | 14.5 |
| Disability indicators | 33.3 | 37.3 | 12.8 | 8.6 | 8.0 |
| Nutritional indicators | 34.9 | 35.4 | 13.9 | 11.0 | 4.8 |
| Acceptance of technology | 37.6 | 34.6 | 15.1 | 4.7 | 8.0 |
| Awareness of e-health | 41.7 | 45.3 | 5.5 | 6.4 | 11.0 |
| Religion and social norms | 45.6 | 32.8 | 6.5 | 10.8 | 4.3 |
The results were further analysed according to the preferences of different participants, as shown in Table 5. The percentage of participants by profession was identified by combining the scores for the options strongly agree and agree and the results are presented in Table 5.
Table 5.
Importance of influencing factors in decision making on e-health by participants
| Factors | Consultant, % | Physician, % | Nurse, % | Information professional, % | Manager, % | Other (MoH), % |
|---|---|---|---|---|---|---|
| Focus on core function | ≥75 | 60–74 | <60 | ≥75 | <60 | 60–74 |
| Access to world class capabilities | 60–74 | ≥75 | <60 | 60–74 | <60 | ≥75 |
| Freeing resources for core activities | ≥75 | <60 | <60 | 60–74 | 60–74 | ≥75 |
| Accelerate reengineering benefits | ≥75 | 60–74 | ≥75 | 60–74 | <60 | ≥75 |
| Improve flexibility versus change | ≥75 | 60–74 | 60–74 | <60 | ≥75 | ≥75 |
| Risk sharing | 60–74 | <60 | <60 | 60–74 | ≥75 | ≥75 |
| Regulations governing | ≥75 | ≥75 | ≥75 | 60–74 | ≥75 | 60–74 |
| Improve service quality | 60–74 | ≥75 | ≥75 | 60–74 | 60–74 | ≥75 |
| Procure higher reliability and competency | ≥75 | 60–74 | <60 | ≥75 | 60–74 | ≥75 |
| Ease of use | ≥75 | ≥75 | ≥75 | ≥75 | ≥75 | |
| Privacy and security concerns | ≥75 | 60–74 | <60 | ≥75 | ≥75 | |
| Save the management time | 60–74 | ≥75 | <60 | 60–74 | ≥75 | 60–74 |
| Reduce the management load | ≥75 | ≥75 | <60 | 60–74 | ≥75 | 60–74 |
| Increase the speed of implementation | ≥75 | 60–74 | ≥75 | 60–74 | ≥75 | ≥75 |
| Improve safety management | 60–74 | 60–74 | ≥75 | ≥75 | 60–74 | ≥75 |
| Improve accountability | ≥75 | 60–74 | <60 | ≥75 | ≥75 | ≥75 |
| Need specialized management | ≥75 | ≥75 | <60 | ≥75 | ≥75 | 60–74 |
| Function difficult to manage | <60 | 60–74 | ≥75 | <60 | ≥75 | 60–74 |
| Achieve flexibility with changing technology | 60–74 | ≥75 | ≥75 | <60 | ≥75 | 60–74 |
| Achieve innovative ideas | ≥75 | 60–74 | <60 | 60–74 | ≥75 | ≥75 |
| Acquire new skills or technical knowledge | ≥75 | ≥75 | ≥75 | 60–74 | ≥75 | ≥75 |
| Complexity of function | 60–74 | <60 | ≥75 | <60 | <60 | 60–74 |
| Function integration and structure | ≥75 | 60–74 | <60 | 60–74 | <60 | ≥75 |
| Function difficult to control | <60 | 60–74 | 60–74 | <60 | ≥75 | ≥75 |
| Save the overall cost | ≥75 | ≥75 | <60 | ≥75 | 60–74 | ≥75 |
| Reduce the labour and operating cost | ≥75 | <60 | ≥75 | ≥75 | 60–74 | ≥75 |
| Make the fixed costs into variable costs | 60–74 | 60–74 | ≥75 | ≥75 | <60 | <60 |
| Improve the cash flow | 60–74 | 60–74 | <60 | 60–74 | 60–74 | 60–74 |
| Cash infusion | ≥75 | 60–74 | <60 | 60–74 | 60–74 | ≥75 |
| Reduce capital costs | ≥75 | 60–74 | <60 | 60–74 | 60–74 | ≥75 |
| Increase the economic efficiency | ≥75 | <60 | <60 | 60–74 | ≥75 | ≥75 |
| Age | ≥75 | ≥75 | ≥75 | 60–74 | 60–74 | 60–74 |
| Gender | ≥75 | ≥75 | <60 | 60–74 | 60–74 | 60–74 |
| Education | ≥75 | <60 | ≥75 | 60–74 | 60–74 | 60–74 |
| Income | ≥75 | <60 | 60–74 | 60–74 | <60 | 60–74 |
| MMR | ≥75 | ≥75 | 60–74 | 60–74 | 60–74 | 60–74 |
| Ethnicity | <60 | ≥75 | 60–74 | 60–74 | ≥75 | <60 |
| Place of residence: urban/rural | ≥75 | 60–74 | <60 | 60–74 | <60 | 60–74 |
| Prevalence of chronic diseases | ≥75 | ≥75 | ≥75 | <60 | <60 | ≥75 |
| Disability indicators | 60–74 | <60 | <60 | <60 | ≥75 | ≥75 |
| Nutritional indicators | ≥75 | ≥75 | ≥75 | 60–74 | 60–74 | ≥75 |
| Acceptance of technology | ≥75 | 60–74 | ≥75 | <60 | 60–74 | ≥75 |
| Awareness of e-health | ≥75 | ≥75 | ≥75 | 60–74 | 60–74 | ≥75 |
| Religion and social norms | ≥75 | 60–74 | ≥75 | 60–74 | <60 | <60 |
It can be seen that strategic factors were considered to be of great importance by consultants and MoH employees compared with other participants such as physicians, nurses and informational professionals. As both consultants and MoH employees are involved in planning and policy making, it may be argued that strategic factors are considered to be of great importance to them. Quality factors were considered to be of great importance by almost all types of participants, especially MoH employees, who specifically focus on delivering high-quality services. Management factors were considered to be of great importance by consultants, physicians and managers. As managers, physicians and nurses are front-end implementers of healthcare services, they are often involved in various management decisions, such as allocation of ventilators to COVID-19 patients, implementation of COVID-19 safety treatment guidelines, treatment options etc., thus they might have considered management factors to be of great importance. Technology factors were considered to be of great importance by all the participants and function characteristics and economic (cost reduction) factors were considered to be of great importance mainly by consultants and MoH employees. Almost all items considered under sociocultural and demographic factors were identified to be significant by a majority of the participants, reflecting the importance of sociocultural and religious considerations in decision making.
Discussion
The consensus among the participants can be assessed based on their level of agreement and their opinions on the various factors. Agreement >75% was considered to be strong, 60–74% was considered to be moderate and <60% was considered to be weak.19 Thus, according to the criteria, it can be seen that consultants reflected strong consensus towards all the main factors, including strategic, quality, management, technology, economic, function characteristics and sociocultural and demographic factors. Physicians preferred quality, management and sociocultural and demographic factors, whereas nurse participants preferred quality, management, functional characteristics and sociocultural and demographic factors. Health information professionals preferred all the factors except strategic and economic factors, while managers preferred management, function characteristics, economic and sociocultural and demographic factors. Participants working under the MoH preferred all the factors. These findings were similar to the findings observed in McGinn et al.19 with respect to the experts, including physicians, healthcare professionals, information professionals and managers. However, it is essential to determine the main factors that are considered to be important in decision making on e-health. The most important criteria (based on a strong consensus among overall participants) is presented in the Table 6.
Table 6.
Prioritization of influencing factors (consensus ≥75%)
| Factor | Subfactor | Consensus |
|---|---|---|
| Strategic | Focus on core function | Strong |
| Accelerate reengineering benefits | Strong | |
| Regulations governing | Strong | |
| Quality | Improve service quality | Strong |
| Ease of use | Strong | |
| Privacy and security concerns | Strong | |
| Management | Save the management time | Strong |
| Increase the speed of implementation | Strong | |
| Improve safety management | Strong | |
| Technology | Achieve flexibility with changing technology | Strong |
| Acquire new skills or technical knowledge | Strong | |
| Function characteristics | Complexity of function | Strong |
| Function integration and structure | Strong | |
| Economic | Save the overall cost | Strong |
| Reduce the labour and operating cost | Strong | |
| Cash infusion | Strong | |
| Increase the economic efficiency | Strong | |
| Sociocultural and demographic | Age | Strong |
| Prevalence of chronic diseases | Strong | |
| Acceptance of technology | Strong | |
| Awareness of e-health | Strong | |
| Religion and social norms | Strong |
Prioritization of factors based on the results indicate that 22 subfactors were identified to be the most important criteria for decision making on e-health implementation in the GCC in light of the COVID-19 pandemic (Table 6). The findings are similar to those outlined in Kavozi et al.2 Technology-related issues such as privacy and security; users’ aspects such as ease of use and health and internet literacy; and strategic factors such as regulations and policies were identified as important challenges in e-health adoption in the GCC in previous studies.22–28 Most of the previous studies22–28 in the GCC were conducted before the COVID-19 pandemic, which may limit the identification of new challenges relevant to the pandemic. However, the addition of sociocultural and demographic factors to this study reflects the influence of the COVID-19 outbreak, as there is a strong emphasis on the prevalence of chronic diseases and awareness of e-health. The increased burden on healthcare resources due to the pandemic may affect the treatment and management of chronic diseases, as the majority of resources are being allocated to treating COVID patients. To address this issue, there is an increasing reliance on e-health technologies. However, it is very much essential to increase awareness about e-health and its benefits. This sudden change in access to healthcare services may have a major impact on patients’ attitudes, behaviour and adoption of these services. In addition, it can be observed that age and the prevalence of chronic disease are two important factors that need to be considered, as older people and people with chronic diseases are more affected by COVID-19.33
Considering the COVID-19 situation, it is evident that the pandemic has affected all sectors, including social, economic, environmental, political and cultural. In this context, the findings in this study have revealed various factors that influence the decision making process in implementing e-health applications. Given the importance and need for implementing e-health approaches on a larger scale to minimize the effects of COVID-19 on healthcare services delivery, the findings in this study can contribute to effective planning and decision making and also support future research related to the challenges of implementing e-health technologies in GCC member states.
Implications
Various implications can be drawn from the findings of this study. First, this study contributes to the e-health literature in the areas of challenges associated with e-health adoption in light of the COVID-19 pandemic, where new factors (sociocultural, demographic and economic [financing]) emerged as strongly influencing e-health adoption in the GCC. These factors were not identified to be strongly influencing e-health adoption before the pandemic. Second, this study has practical implications, as the findings can be used by decision makers and healthcare practitioners in implementing e-health approaches for improving healthcare services in GCC states.
Limitations and future research
There are a few limitations to this study from a methodological perspective. Adopting mixed methods such as both qualitative (e.g. interviews) and quantitative (surveys) can enhance the quality of findings. Qualitative methods can be used for in-depth analysis of the challenges associated with e-health by collecting data from various perspectives that can then be compared and analysed with qualitative findings. However, due to the ongoing pandemic, personal interviews were not conducted due to preventive procedures such as social distancing. In addition, due to the increased stress and workload of healthcare practitioners, appointments for telephone or online interviews were impractical. As a result, an online questionnaire-based survey was used, which can be answered by participants at their convenience. Another major limitation was that this study did not consider the service receivers or users’ (patients’) perspectives, which may require additional data collection instruments involving factors that are different from policy- and decision-makers’ perspectives. Moreover, the users’ perspectives of e-health technologies may include a wide range of factors that will increase the complexity of data collection and analysis. Therefore, future work should include separate research focusing exclusively on users’ perspectives. Accordingly, future research should focus on using multiple methods in the identification of various influencing factors and extend the research in other regions.
Conclusions
This study has provided effective criteria to support decision making on e-health implementation during the COVID-19 pandemic in GCC member states, most of which are in the process of digitizing their healthcare infrastructure. The study reflected that decision making in relation to e-health is a complex process that requires consideration of various factors. It also identified that attention should be paid to sociocultural and demographic factors that need to be considered in increasing healthcare access during the COVID-19 pandemic. Moreover, the findings of this study can help in making the right decisions for developing and implementing e-health strategies in GCC member states.
Acknowledgements
We would like to thank Dr Saif, Dr Saad, Dr Tahnoun and Dr Zayed for providing links to the communities of healthcare practitioners in the UAE, Bahrain, Oman and Qatar for conducting the survey.
Appendix A: Survey questionnaire
Survey on factors influencing decision making on e-health adoption during the COVID-19 pandemic in the GCC.
This survey is aimed at investigating the most important criteria affecting the decision making on implementing e-health strategies in GCC member states. The survey is divided into two sections. The first section is aimed at collecting the participants information. The second section focuses on the various factors affecting decision making on e-health strategies, which includes multiple choice questions to which the participants need to select the relevant options they feel are true to their knowledge.
PART A: PARTICIPANTS DETAILS
1. NAME
2. AGE: <15 years; 15–24 years; 25–34 years; 35–44 years; 45–54 years; >54 years
3. GENDER: M/F
4. EDUCATION: School/Bachelor Degree/Master's/PhD/Other
5. Profession:
6. Work Experience: <2 years; 2–5 years; 5–10 years; >10 years
PART B: INFLUENCING FACTORS
7. Please rate the importance of following strategic factors influencing decision making for e-health strategies on a scale of (1: strongly disagree; 2: disagree; 3: neutral; 4: agree; 5: strongly agree)
Focus on core function
Access to world class capabilities
Freeing resources for core activities
Accelerate reengineering benefits
Improve flexibility versus change
Risk sharing
Regulations governing
8. Please rate the importance of following quality factors influencing decision making for e-health strategies on a scale of (1: strongly disagree; 2: disagree; 3: neutral; 4: agree; 5: strongly agree)
Improve service quality
Procure higher reliability and competency
Ease of use
Privacy and security concerns
9. Please rate the importance of following management factors influencing decision making for e-health strategies on a scale of (1: strongly disagree; 2: disagree; 3: neutral; 4: agree; 5: strongly agree)
Save the management time
Reduce the management load
Increase the speed of implementation
Improve safety management
Improve accountability
Need specialized management
Function difficult to manage
10. Please rate the importance of following technological factors influencing decision making for e-health strategies on a scale of (1: strongly disagree; 2: disagree; 3: neutral; 4: agree; 5: strongly agree)
Achieve flexibility with changing technology
Achieve innovative ideas
Acquire new skills or technical knowledge
11. Please rate the importance of the following functions (characteristics) influencing decision making for e-health strategies on a scale of (1: strongly disagree; 2: disagree; 3: neutral; 4: agree; 5: strongly agree)
Complexity of function
Function integration and structure
Function difficult to control
12. Please rate the importance of the following economic factors influencing decision making for e-health strategies on a scale of (1: strongly disagree; 2: disagree; 3: neutral; 4: agree; 5: strongly agree)
Save the overall cost
Reduce the labour and operating cost
Make the fixed costs into variable costs
Improve the cash flow
Cash infusion
Reduce capital costs
Increase the economic efficiency
13. Please rate the importance of the following sociocultural and demographic factors influencing decision making for e-health strategies on a scale of (1: strongly disagree; 2: disagree; 3: neutral; 4: agree; 5: strongly agree)
Age
Gender
Education
Income
MMR
Ethnicity
Place of residence: urban/rural
Prevalence of chronic diseases
Disability indicators
Nutritional indicators
Acceptance of technology
Awareness of e-health
Religion and social norms
Authors’ contributions
Funding
None.
Competing interests
None declared.
Ethical approval
Ethical approval was obtained from the institutional review board of Imam Abdulrahman Bin Faisal University.
Data availability
Data available on request from the authors.
References
- 1. Masoumpour SM, Rahimi SH, Kharazmi E et al. Assessing waiting time in emergency department of Shahid Faghihi hospital, Shiraz and presenting appropriate strategies using quality function deployment (QFD) method, 2011–2012. Hakim Res J. 2013;16(2):159–68. [Google Scholar]
- 2. Kavosi Z, Rahimi H, Khanian S et al. Factors influencing decision making for healthcare services outsourcing: a review and Delphi study. Med J Islam Repub Iran. 2018;32:327–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tan B, Chew N, Lee G et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Soreide K, Hallet J, Matthews J et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020;107(10):1250–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nicola M, Alsafi Z, Sohrabi C et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization . WHO coronavirus disease (COVID-19) dashboard. Available from: https://covid19.who.int/?gclid=EAIaIQobChMI8dbP5JeB7AIV-yCtBh3j2wNREAAYASAAEgK5w_D_BwE [accessed 24 September 2020]. [Google Scholar]
- 7. Alandijany T, Faizo A, Azhar E. Coronavirus disease of 2019 (COVID-19) in the Gulf Cooperation Council (GCC) countries: current status and management practices. J Infect Public Health. 2020;13(6):839–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. El-Saharty S, Kheyfets I, Herbst C et al. The GCC countries’ responses to COVID-19. In: Fostering Human Capital in the Gulf Cooperation Council Countries. Washington, DC: World Bank; 2020:39–57. [Google Scholar]
- 9. Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir J Med Sci. 2020; doi: 10.1007/s11845-020-02299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bokolo AJ. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Altios . Understanding the impact of COVID-19 in the UAE and GCC region. Available from: https://altios.com/wp-content/uploads/2020/06/COVID-19-IMPACT-IN-THE-UAE-AND-GCC-REGION.pdf [accessed 24 September 2020]. [Google Scholar]
- 12. AbuKhousa E, Mohamed N, Al-Jaroodi J. e-health cloud: opportunities and challenges. Future Internet. 2012;4(3):621–45. [Google Scholar]
- 13. Chenthara S, Ahmed K, Wang H et al. Security and privacy-preserving challenges of e-health solutions in cloud computing. IEEE Access. 2019;7:74361–82. [Google Scholar]
- 14. Abrams E, Shaker M, Oppenheimer J et al. The challenges and opportunities for shared decision making highlighted by COVID-19. J Allergy Clin Immunol Pract. 2020;8(8):2474–80.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bashshur R, Doarn C, Frenk J et al. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 2020;26(5):571–3. [DOI] [PubMed] [Google Scholar]
- 16. Low C, Hsueh Chen Y. Criteria for the evaluation of a cloud-based hospital information system outsourcing provider. J Med Syst. 2012;36(6):3543–53. [DOI] [PubMed] [Google Scholar]
- 17. Tajdini S, Nazari M. Is outsourcing decision: a quantitative approach. Int J Business Manag. 2012;7(2):113–29. [Google Scholar]
- 18. Al-Nehmi AA. Decision Factors for Outsourcing the Maintenance Services of Saudi Universities. Master's thesis, King Fahd University of Petroleum and Minerals. Available from: https://eprints.kfupm.edu.sa/id/eprint/136091/ [accessed 25 September 2020]. [Google Scholar]
- 19. McGinn C, Gagnon M, Shaw N et al. Users’ perspectives of key factors to implementing electronic health records in Canada: a Delphi study. BMC Med Inform Decis Mak. 2012;12:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoque M, Bao Y. Cultural influence on adoption and use of e-health: evidence in Bangladesh. Telemed J E Health. 2015;21(10):845–51. [DOI] [PubMed] [Google Scholar]
- 21. Mieczkowska S, Hinton M, Barnes D. Barriers to e-health business processes. Int J Electron Healthc. 2004;1(1):47–59. [DOI] [PubMed] [Google Scholar]
- 22. Jiménez-Rodríguez D, Santillán García A, Montoro Robles J et al. Increase in video consultations during the COVID-19 pandemic: healthcare professionals’ perceptions about their implementation and adequate management. Int J Environ Res Public Health. 2020;17(14):5112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Alsulame K, Khalifa M, Househ M. E-health status in Saudi Arabia: a review of current literature. Health Pol Technol. 2016;5(2):204–10. [Google Scholar]
- 24. Uluc C, Ferman M. A comparative analysis of user insights for e-health development challenges in Turkey, Kingdom of Saudi Arabia, Egypt and United Arab Emirates. J Manag Market Logist. 2016;3(2):176–89. [Google Scholar]
- 25. AlBar A, Hoque M. Patient acceptance of e-health services in Saudi Arabia: an integrative perspective. Telemed J E Health. 2019;25(9):847–52. [DOI] [PubMed] [Google Scholar]
- 26. Weber A, Turjoman R, Shaheen Y et al. Systematic thematic review of e-health research in the Gulf Cooperation Council (Arabian Gulf): Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and United Arab Emirates. J Telemed Telecare. 2016;23(4):452–9. [DOI] [PubMed] [Google Scholar]
- 27. Zolait A, Radhi N, Alhowaishi M et al. Can Bahraini patients accept e-health systems? Int J Health Care Qual Assur. 2019;32(4):720–30. [DOI] [PubMed] [Google Scholar]
- 28. Al-Khatlan H, Alazmi S, Almutairi B. Knowledge, attitude and practice of e-health among health care providers in Kuwait. Green J Med Sci. 2017;7(5):42–51. [Google Scholar]
- 29. Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;140:1–55. [Google Scholar]
- 30. Etikan I. Comparison of convenience sampling and purposive sampling. Am J Theoret Appl Stat. 2016;5(1):1–4. [Google Scholar]
- 31. Alanezi F, Aljahdali A, Alyousef S et al. Implications of public understanding of COVID-19 in Saudi Arabia for fostering effective communication through awareness framework. Front Public Health. 2020;8:494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. QuestionPro . Home page. Available from: https://www.questionpro.com/ [accessed 25 September 2020]. [Google Scholar]
- 33. Brooke J, Jackson D. Older people and COVID-19: isolation, risk and ageism. J Clin Nurs. 2020;29(13–14):2044–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.