The COVID-19 pandemic is already responsible for >1 million deaths worldwide.1 Latin America is one of the most affected regions worldwide, with >300 000 deaths confirmed by September 2020.1 Latin America is also one of the most urbanized and unequal regions in the world, with wide inequities in longevity in its cities.2 Wide inequities in COVID-19 outcomes have been reported in other settings.3 However, policymakers in some Latin American countries have expressed scepticism about the existence of health inequities in COVID-19 mortality.4 We used mortality, population and census data to show a worsening of pre-existing inequities in mortality in the municipalities that make up the metropolitan region of Santiago (Chile) during the COVID-19 pandemic.
We obtained data for the 36 comunas (municipalities) that make up Greater Santiago, the metropolitan area of the capital of Chile, on: (i) mortality by age for the 2016–2020 period from the Department of Statistics and Health Information (DEIS); (ii) population projections by age for the 2016–2020 period from the National Institute of Statistics (INE); and (iii) average years of schooling among adults aged ≥25 years, and the proportion of households living in overcrowding (>2.5 people/bedroom) from the 2017 Chilean census. We selected these two indicators since they represent either good measures of area-level socio-economic status (SES) or are directly linked to COVID-19 transmission. We computed age-adjusted mortality rates, using the 2000 World Health Organization reference population, from January to August for the pre-pandemic (years 2016–2019) and pandemic (2020) periods. We estimated the association between log(mortality) and average years of schooling or proportion overcrowded households using a linear model for each period separately. Data and code for replication are available here: https://github.com/usamabilal/COVID_Chile_Inequities.
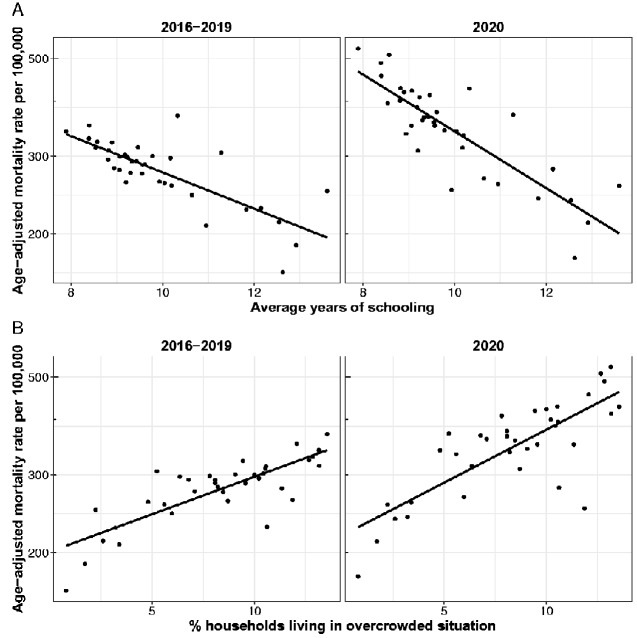
Figure 1 shows the main results. We found a strong association between SES and mortality in both periods, although this association was stronger in 2020. Specifically, we found a 9.0% lower mortality per 1-year increase in the average schooling years in the pre-pandemic period [relative risk (RR) = 0.91, 95% confidence interval (CI) 0.87 to 0.93] compared with a 13.8% lower mortality in the 2020 period (RR = 0.86, 95% CI 0.83 to 0.89). We also found that a 5% increase in the proportion of overcrowded households was associated with a 22% and 32% higher mortality in the pre-pandemic and pandemic periods, respectively (RR = 1.22, 95% CI 1.16 to 1.28; RR = 1.32, 95% CI 1.23 to 1.42).
Figure 1.
Area-level socio-economic status and age-adjusted mortality in 2016–2019 and 2020 in the municipalities of Santiago, Chile
(A) Average years of schooling for adults >25 years of age; (B) percentage of households living in overcrowded situations. The solid line represents a linear fit.
In summary, we found a worsening of pre-existing inequities in mortality in the metropolitan area of Santiago de Chile during the COVID-19 pandemic. The association of years of schooling and overcrowding with mortality in the pre-pandemic period (2016–2019) is consistent with previous research in Santiago, showing wide gaps in life expectancy2 and infant mortality.5 Our finding that mortality inequities in 2020 were greater than in previous periods contradicts statements made in September 2020 by the Minister of Health of Chile, which indicated that there is no relationship between mortality due to COVID-19 and poverty, as this would imply discriminatory healthcare due to the place of origin of the patients.4 This assertion ignores existing structural inequalities in Chile, including inequities in healthcare access and utilization by type of insurance both before6 and during the pandemic,7 along with social determinants of health beyond the health system. These include factors driving not only incidence and increased exposure to the virus,3 such as more precarious employment conditions, loss of income and the need to work outside the home, but also an increased prevalence of conditions that aggravate the consequences of the disease, which show a strong social patterning in Chile.8 Mitigating health inequities was an explicit objective of the Chilean National Health Strategy9 and the aggravation of these inequities amidst the COVID-19 pandemic represents a step in the wrong direction. Our analysis is limited by the lack of individual-level mortality data and a validated SES index. However, we are using whole-population vital-registration data in a country with a good vital-registration system,10 which lends strength to our findings.
Interventions to reduce these inequities are greatly needed to avoid the continued widening of these gaps, including but not exclusively focused on healthcare, in addition to addressing the other health and economic consequences of the pandemic, which will likely also affect these vulnerable groups more frequently, intensely and for more prolonged periods of time.
Funding
U.B. was supported by the Office of the Director of the National Institutes of Health under award number DP5OD26429. U.B., T.A. and A.V. were also supported by the Salud Urbana en América Latina (SALURBAL)/Urban Health in Latin America project, funded by the Wellcome Trust (205177/Z/16/Z). The funding sources had no role in the analysis, writing or decision to submit the manuscript.
Acknowledgements
The data underlying this article are available at https://github.com/usamabilal/COVID_Chile_Inequities/. All analyses were conducted with publicly available de-identified surveillance data.
Conflict of interest
None declared.
References
- 1. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bilal U, Alazraqui M, Caiaffa WT et al. Inequalities in life expectancy in six large Latin American cities from the SALURBAL study: an ecological analysis. Lancet Planet Health 2019;3:e503–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berkowitz RL, Gao X, Michaels EK, Mujahid MS. Structurally vulnerable neighbourhood environments and racial/ethnic COVID-19 inequities. Cities & Health 2020;1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Basoalto H, Silva D. Ministro Paris por fallecidos por Covid: ‘No hay una relación entre letalidad y pobreza, eso significaría que los pacientes son atendidos en forma discriminada’. La Tercera 2020. https://www.latercera.com/nacional/noticia/ministro-paris-por-fallecidos-por-covid-no-hay-una-relacion-entre-letalidad-y-pobreza-eso-significaria-que-los-pacientes-son-atendidos-en-forma-discriminada/S5LPFNI4VRDZ7EP7FHJEVJNJ2A/ [Google Scholar]
- 5. Gonzalez F, Alfaro T, Horna-Campos O. Mortalidad Infantil en las comunas de la Región Metropolitana, periodo 2005-2014. Rev Chil Pediatr 2020;91:34–45. [DOI] [PubMed] [Google Scholar]
- 6. Castillo-Laborde C, Aguilera-Sanhueza X, Hirmas-Adauy M et al. Health insurance scheme performance and effects on health and health inequalities in Chile. MEDICC Review 2017;19:57–64. [DOI] [PubMed] [Google Scholar]
- 7. Escuela de Salud Pública de la Universidad de Chile, Colegio Médico de Chile. Monitoreo Nacional de Síntomas y Prácticas COVID-19 en Chile (MOVID-19): ¿Cuál ha sido el impacto de la pandemia en el acceso a atenciones de salud?Un análisis para la adaptación de nuestro sistema de salud. 2020. https://www.movid19.cl/publicaciones/decimo-informe/
- 8. Ortiz MS, Cabieses B, Oyarte M, Repetto P. Disentangling socioeconomic inequalities of type 2 diabetes mellitus in Chile: a population-based analysis. PloS One 2020;15:e0238534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministerio de Salud (Chile). Estrategia Nacional de Salud. Gobierno de Chile Town: Santiago de Chile. 2011.
- 10. Bilal U, Hessel P, Perez-Ferrer C et al. Life expectancy and mortality in 363 cities of Latin America. Nature Medicine 2021. 10.1038/s41591-020-01214-4 [DOI] [PMC free article] [PubMed] [Google Scholar]