Abstract
Objective
We sought to support public health surveillance and response to coronavirus disease 2019 (COVID-19) through rapid development and implementation of novel visualization applications for data amalgamated across sectors.
Materials and Methods
We developed and implemented population-level dashboards that collate information on individuals tested for and infected with COVID-19, in partnership with state and local public health agencies as well as health systems. The dashboards are deployed on top of a statewide health information exchange. One dashboard enables authorized users working in public health agencies to surveil populations in detail, and a public version provides higher-level situational awareness to inform ongoing pandemic response efforts in communities.
Results
Both dashboards have proved useful informatics resources. For example, the private dashboard enabled detection of a local community outbreak associated with a meat packing plant. The public dashboard provides recent trend analysis to track disease spread and community-level hospitalizations. Combined, the tools were utilized 133 637 times by 74 317 distinct users between June 21 and August 22, 2020. The tools are frequently cited by journalists and featured on social media.
Discussion
Capitalizing on a statewide health information exchange, in partnership with health system and public health leaders, Regenstrief biomedical informatics experts rapidly developed and deployed informatics tools to support surveillance and response to COVID-19.
Conclusions
The application of public health informatics methods and tools in Indiana holds promise for other states and nations. Yet, development of infrastructure and partnerships will require effort and investment after the current pandemic in preparation for the next public health emergency.
Keywords: public health informatics, coronavirus, pandemics, health information interoperability, health information exchange
INTRODUCTION
BACKGROUND AND SIGNIFICANCE
Coronavirus disease 2019 (COVID-19), caused by the novel SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus, is a global pandemic that, as of November 12, 2020, had affected more than 52.6 million individuals and caused over 1.2 million deaths.1 In the United States, COVID-19 rapidly spread across large cities as well as across many rural areas. In Indiana, which ranks 17 among U.S. states by population with just under 6.7 million residents, COVID-19 challenged but did not overwhelm the health system. As of November 5, 2020, there were 196 176 confirmed cases with an estimated population-level prevalence between 3% and 15%.2,3
Public health (PH) agencies play a critical role in managing disease epidemics. In the United States, responsibility for health rests with each state’s governor, and therefore the state-level PH agency seeks to prevent disease, protect health, and promote well-being. Local and state-level PH agencies conduct disease surveillance, manage contact tracing, facilitate resource distribution including personal protective equipment (PPE), establish alternative care sites, coordinate investigation of long-term care facilities, and provide diagnostic support through laboratory testing. Federal PH agencies, such as the U.S. Centers for Disease Control and Prevention (CDC), support state-level efforts and coordinate response across states.4 During a pandemic, PH and healthcare systems work together to identify and manage disease cases while working to prevent disease spread.
To manage disease epidemics, PH agencies utilize a variety of information systems, such as laboratory information management systems and case management systems.5–7 Although existing information systems enable capture of data on laboratory-confirmed cases of COVID-19, the pandemic illuminated deficits in the U.S. information infrastructure.8,9 The holes in the “swiss cheese” of PH infrastructures are the topic of media articles10–13 because public demand for information quickly outstripped the capacity of most PH agencies to produce data on the emerging outbreak. For example, PH agencies do not typically receive information on hospitalizations until weeks postdischarge, when coding of the encounter has been finalized.14 That is insufficient for pandemics, during which PH agencies need real-time situational awareness of health threats.
OBJECTIVE
Leveraging data available through a statewide health information exchange (HIE), we sought to support PH surveillance and response to COVID-19 through the development and implementation of novel visualization applications. Whereas other applications either present data for a single healthcare facility15 or present aggregate counts of cases, our applications integrate clinical and PH data allowing for detailed examination of subpopulations. Our applications illustrate the role of informatics in PH, and their success is owed to (1) a robust health information infrastructure16; (2) strong collaboration across the health system, including PH organizations; and (3) expertise in biomedical informatics.
MATERIALS AND METHODS
The visualization applications were possible due to a robust informatics environment in Indiana. The state possesses a mature, statewide HIE and a leading biomedical informatics research organization. Both entities routinely engage the broader biomedical ecosystem in the state (eg, industry, government, academic) in collaborations to address clinical, PH, and research challenges. Before we describe the visualization applications, we discuss the unique strengths of Indiana that made the rapid development and implementation of the applications possible.
A statewide information infrastructure
The applications leverage the Indiana Network for Patient Care (INPC), one of the oldest and largest health information networks in the United States.17 The INPC is a repository of clinical and administrative health data collected from over 38 health systems representing 117 hospitals, 18 486 physician practices, commercial laboratories, and PH departments across the state. The INPC serves the clinical needs of providers, and it supports PH surveillance and research needs.18–20 Support for PH and research is unique among HIEs in the United States.21
Prior to the pandemic, the INPC possessed several hundred electronic feeds routinely capturing data from Indiana’s health system.22 Admission, discharge, and transfer (ADT) feeds provide real-time information on patients as they traverse the health system. Electronic laboratory report (ELR) messages are a required data feed for INPC members, allowing clinicians to access a patient’s recent lab values and PH agencies to receive notifiable disease alerts via the Notifiable Condition Detector.23,24 Encounter records are also provided by hospitals and clinics with diagnostic codes (eg, International Classification of Diseases–Tenth Revision–Clinical Modification) to enable review of problems and comorbidities. These data are exchanged predominantly using HL7 (Health Level 7) version 2.5.1 messages, although some source systems use alternative message formats including prior versions of HL7. The ADT and ELR messages further utilize LOINC as well as SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms), where available from the source.
In response to the pandemic, the Indiana HIE (IHIE) coordinated enhancements to the INPC with the Regenstrief Institute. Even before hospital and commercial laboratories began processing COVID-19 tests, the IHIE updated the Notifiable Condition Detector to recognize LOINC codes for COVID-19, leveraging the prereleased terms published on the LOINC website.25 This positioned the INPC to automatically identify COVID-19 test results and route them to PH authorities once hospital and commercial labs began performing approved tests. The IHIE further incorporated additional data from health systems and hospitals not part of the INPC. Data from these facilities are processed into the INPC using ADT and ELR feeds like other institutions, enabling their retrieval for pandemic purposes seamless in conjunction with the usual INPC data. Similarly, the Indiana State Department of Health and Family Social Services Administration provide daily feeds of laboratory test results from multiple statewide locations offering COVID-19 specific testing for symptomatic patients as well as healthcare workers and institutionalized patients (eg, prisoner, nursing homes). Death records from state vital records are captured by the IHIE through the Michiana Health Information Network, which recently merged with the IHIE.
Biomedical informatics expertise and health data partnerships
Multiple organizations collaborated to design and implement the novel visualization applications. The collaboration was led by the Regenstrief Institute, a support organization to the Indiana University (IU) School of Medicine, and an internationally recognized informatics and health services research organization that is home to the Clem McDonald Center for Biomedical Informatics. The Center is also home to a collaborative program in Public and Population Health Informatics between Regenstrief and the IU Fairbanks School of Public Health.26 The program team further partnered with the IHIE and state as well as county PH organizations to inform the design and use of the visualization applications, including Indiana State Department of Health, the Office of the Governor, Marion County Public Health Department, and Family Social Services Administration (which houses Indiana’s Medicaid program).
Prior to the pandemic, Regenstrief collaborated closely with many of the partners on a variety of healthcare initiatives. Regenstrief and the IHIE have the closest relationship, as the IHIE was created by Regenstrief in 2004 to allow the HIE to scale operations across Indiana. The INPC began as a biomedical informatics research project.27,28 Regenstrief now serves as the research and development partner to the IHIE, serving also as the honest data broker for the INPC. The PH informatics program at Regenstrief further meets regularly with PH agencies to discuss their informatics needs, and it routinely collaborates on CDC-funded projects to enhance the PH infrastructure in Indiana. Therefore, when the pandemic began, Regenstrief’s biomedical informatics experts were already in routine contact with PH leaders and aware of what the major PH challenges would be during the unfolding disease outbreak across the state.
The Regenstrief COVID-19 Dashboard
To support PH response, we developed the Regenstrief COVID-19 Dashboard, a Tableau-based visualization application that collates information on individuals tested for and infected with COVID-19 in parallel with data on individuals with COVID-like illnesses, including influenza and pneumonia. The dashboard harmonizes data captured from multiple sources to inform situational awareness with respect to COVID-related testing, cases, hospitalizations, emergency department visits, intensive care utilization, mortality, recovery, comorbidity, demographics, and geography.
The dashboard is designed to visualize data relevant to the 3 components of PH surveillance: person, place, and time.29 Persons are identified based on ELR message feeds and International Classification of Diseases–based diagnostic codes from emergency department and inpatient encounters. We employ probabilistic algorithms to uniquely identify each person across data sources to ensure accurate reporting of information because many persons receive multiple laboratory tests for COVID-19 due to (1) uncertainty in test results, (2) hospitals often test persons transferred from other hospitals and nursing homes, and (3) employers testing persons multiple times to determine eligibility to report for work. Place is based on the person’s home address. All addresses in the INPC are geocoded.30,31 Other data sources used by the dashboard report the person’s home zip code and county of residence. Multiple dates are used to examine time. Persons appear in the dashboard when they either (1) receive a laboratory test for COVID-19 or influenza typically using the collection date for the test specimen or (2) receive a clinical diagnosis of COVID-19 using the date of encounter.
The specific data elements and their corresponding PH surveillance dimension are summarized in Table 1. The table also includes the source of each data element.
Table 1.
Data elements and dimensions incorporated into the Regenstrief COVID-19 Dashboard to support population surveillance of COVID-19–like illnesses
| Person | Time | Source | |
|---|---|---|---|
| Laboratory testing (surveillance) | # persons tested | Date of specimen collection | ELR |
| # persons testing positive | Date of specimen collection | ELR | |
| % positivity (# positive / # tested) | Daily and 7-day moving average | Calculation | |
| Hospitalizations | # persons hospitalized up to 21 d before or after positive test | Date of admission | ADT |
| # persons discharged | Date of discharge | ADT | |
| # individuals admitted to intensive care during hospitalization | Date of transfer to intensive care | ADT | |
| Length of stay (in days) as population mean | Date of discharge minus date of admission, mean value | Calculation | |
| Emergency department visits | # persons seen at an emergency department up to 21 d before or after positive test | Date of emergency department visit | ADT |
| Reason for emergency department visit, either chief complaint or admission diagnosis | Date of emergency department visit | ADT | |
| Comorbidities | Diagnosis codes associated with hospitalizations, emergency, and outpatient visits up to 2 years before laboratory test | N/A | ICD-10 codes in ORU and ADT |
| Mortality | # individuals whose death is associated with COVID-19 | Date of death | Vital records provided by state health department |
| % individuals hospitalized who died while in the hospital | N/A | Calculation | |
| Recovery | # individuals who recovered from COVID-19, which are those who either never needed hospitalization or have been discharged; excludes individuals who died | At least 21 days since positive COVID-19 test without hospitalization OR discharged from hospital plus 7 days without readmission | ELR + ADT + vital records |
| Demographics | Age | At the time of COVID-19 testing or hospitalization | ADT or ELR |
| Sex | N/A | ADT or ELR | |
| Race | N/A | ADT or ELR | |
| County of residence | Last known address at the time of testing or hospitalization | ADT or ELR |
ADT: HL7 admission, discharge, transfer; COVID-19: coronavirus disease 2019; ELR: electronic laboratory reporting; ICD-10: International Classification of Diseases–Tenth Revision; N/A: not applicable; ORU: HL7 observation result unsolicited.
Analysts from Regenstrief’s Data Services team query data from the IHIE once per day and transform them into an analytical dataset for the dashboard. The daily process (24/7) of querying involves not only data extraction, linkage, and deduplication functionality, but also descriptive statistical calculations. The rate per 100 000 population is calculated by dividing the number of individuals meeting numerator criteria by the 2018 Census-based population of the geographic area selected by the user then multiplied by 100 000. Overall prevalence positivity is calculated by dividing the number of total unique individuals testing positive by the total number of unique individuals tested. Daily incidence positivity is calculated by dividing the number of total unique individuals testing positive per day by the total number of unique individuals tested per day. Both measures are important to PH stakeholders. Prevalence estimates the total disease burden on a population, whereas incidence measures the population of individuals newly infected. Incidence helps PH agencies identify current trends in disease spread.
The initial version of the Regenstrief COVID-19 Dashboard was developed primarily to guide PH decisions in the early weeks of the pandemic. This “private” dashboard was accessible only to authenticated users in state and local health departments in order to enable data delivery at a level of granularity not appropriate for public consumption due to potential privacy concerns. After a few weeks, we developed a “public” version of the dashboard for broader use by health system leaders and other stakeholder groups. Given the rapidly developing nature of the pandemic, our dashboard team established a cadence of daily stand-up meetings to provide continuous dialogue and decision making in concert with our partners. Representatives from the IHIE and PH partners were on these calls. They informed which data would be harmonized and displayed and they provided input and feedback on designs conceived by the informatics team.
Both dashboards were developed using Tableau Desktop and are published each day using Tableau Server within the IU Information Technology Services environment. The project was approved by the institutional review board at Indiana University.
RESULTS
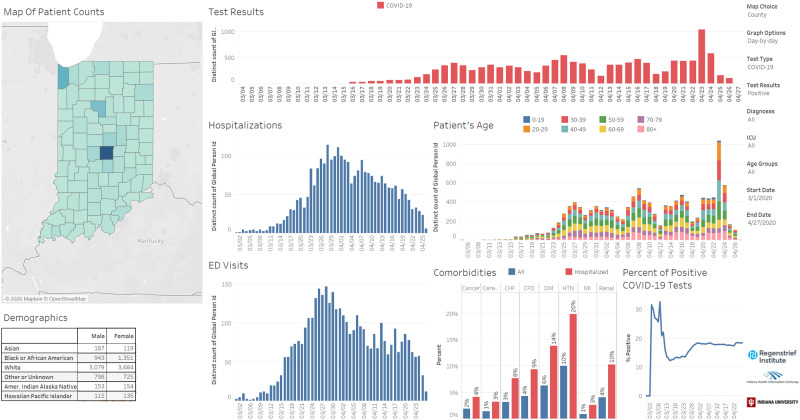
We launched the first version of the Regenstrief COVID-19 Dashboard on March 23, 2020. The dashboard debuted with a series of bar charts reporting individuals tested for COVID-19 or influenza as depicted in Figure 1. Demographics for each person were displayed using stacked bar charts, and line graphs depicted cumulative hospitalizations since the start of the outbreak. Users could filter results by selecting a geographic area of interest (eg, county, zip code) or use a radio button at the top to filter results to a specific diagnosis or laboratory test of interest. Users could also change the time period of interest, allowing examination of data before or after certain events, such as the governor’s stay-at-home order or the Fourth of July. These filters require recalculation of the descriptive statistics.
Figure 1.
Screenshot of the original Regenstrief COVID-19 Dashboard. This version debuted with simple bar charts to allow users to see daily counts of new COVID-19 cases and hospitalizations along with the demographics of infected individuals.
Enhancement of functionality and visualizations
Over the next 10 weeks, as cases and hospitalizations in Indiana continued to grow, we enhanced the functionality and information representations available in the dashboard. These enhancements were triggered by daily conversations with our PH partners as well as our internal experts, both groups desired new information or views of information to examine the unfolding outbreak. We further engaged business intelligence staff at the University Information Technology Services to support enhancement of the visualizations.
New functions and visualizations included:
Positivity: Early on PH partners suggested that, given delays between sample collection and test result availability, we should use COVID-19 test positivity in addition to the count of individuals reported as positive each day. Positivity normalizes reported infections as it divides the number of positive tests by the total number of tests performed. As testing capacity increases, positivity decreases when the same number of new cases are detected. PH officials desired to monitor testing capacity at state and county levels as well as in specific zip codes.
Estimated Recovery Metric: We also developed a metric to monitor the proportion of the population recovered from COVID-19. Our metric uses a 21-day window following a positive lab result. If an individual is not hospitalized, they likely have mild symptoms and is assumed to have recovered after 21 days. We also add to this population COVID-19–positive individuals who were hospitalized but have since been discharged for at least 1 week. We then subtract out from this metric the number of deaths among COVID-19 positive individuals.
Length of Stay: Using discharge dates as well as the difference in days between date of admission and today’s date (for patients still hospitalized), we calculate hospitalization length of stay. These metrics help PH officials and epidemiology modelers monitor and forecast impact of the disease on the health system given concerns about overcrowding.
Population Pyramids: Originally, the dashboard featured stacked bar charts to track the distribution of COVID-19 among various populations based on age, race, and gender. These visualizations were helpful, but they became difficult to interpret as time progressed (especially after 2 weeks elapsed since we displayed daily bar counts). We shifted these visualizations to population pyramid charts to better represent the proportions of tested and hospitalized individuals by sex and race.
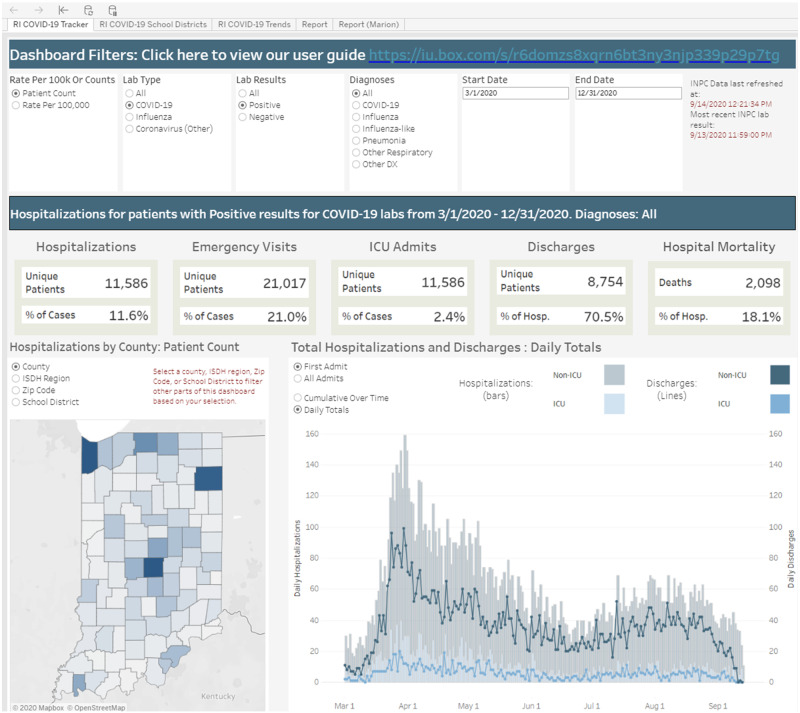
The evolving dashboard supported daily PH decision making, enabling measurement of key indicators like positivity and recovery. Enhanced information visualizations significantly changed the user experience, enabling novice users to more quickly interpret trends and proportions. An enhanced version of the private dashboard is depicted in Figure 2. Although not all of the enhancements are visible in the figure, the radio buttons that allow for filtering are depicted along with headline numbers that provide users with a snapshot of the cumulative impact of COVID-19 on the state population.
Figure 2.
Screenshot of the enhanced Regenstrief COVID-19 Dashboard. This version features enhanced functionality for users to filter the contents of the dashboard. It further debuted headline numbers that provide a snapshot of the cumulative impact of COVID-19 in the state as well as enhanced visualization of hospitalization data.
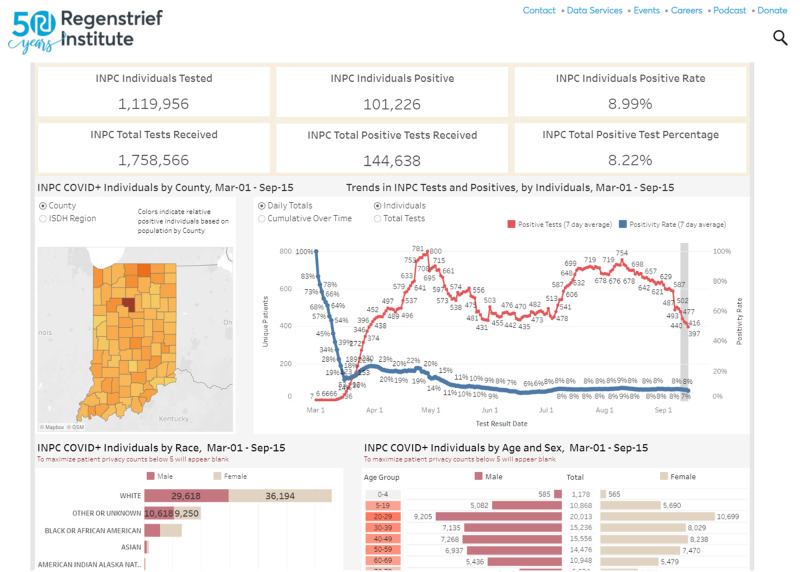
Making the dashboard publicly accessible
In addition to enhancing the dashboard’s functionality and visualizations, which are accessible behind the university’s firewall to authorized users, including Regenstrief personnel and faculty as well as state and county PH staff, we also created a public version depicted in Figure 3. In consultation with state PH officials, we identified information on the dashboard that would be useful to the public as well as health system leaders who could not access the private tool. Furthermore, the dashboard’s measurement of hospitalizations was selected as a key metric for the governor’s “Back on Track” plan32 for reopening the state following an executive stay-at-home order in March 23, 2020. Regenstrief’s public dashboard, therefore, would complement the state’s official website by augmenting available COVID-19 data with information on hospitalizations, comorbidities, and recovery.
Figure 3.
Screenshot of the public Regenstrief COVID-19 Dashboard. This public version illustrates enhanced visualizations added to the laboratory testing (surveillance) section of the tracker for demographics as well as calculation of test positivity.
To make the information public, we constrained the functionality to maintain confidentiality as follows. First, we implemented a rule to hide metrics when a cohort size was less than 5 people. While counts for lab tests and healthcare utilization as well as death can be reported when smaller than 5, information regarding demographics and medical history (eg, comorbidities) is censored. Second, we only include information publicly on individuals who test positive for COVID-19, as it is a reportable condition (eg, influenza in the tracker can only be viewed by PH business associates). Finally, we do not allow users of the public dashboard to filter the results using the radio buttons. While these measures limit functionality, they maximize privacy.
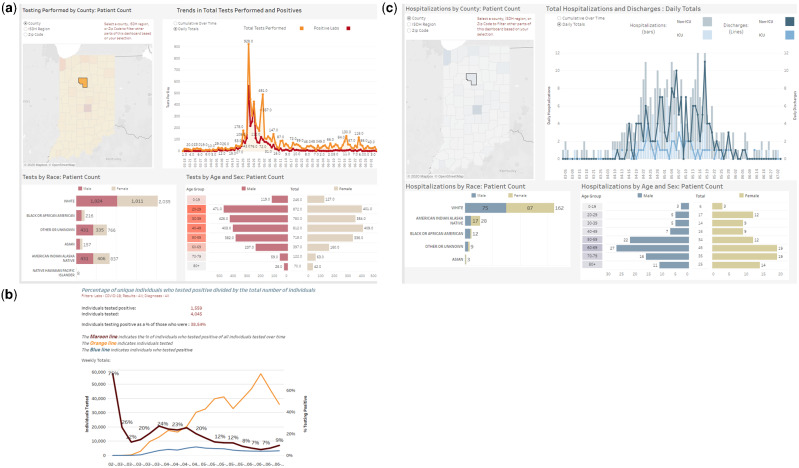
Using the dashboard to identify local COVID-19 outbreaks
The dashboard identified several local outbreaks, including the one in a meat packing plant located in Cass County (Figure 4). In early April 2020, individuals working at the Tyson Fresh Meats plant in Logansport, Indiana, began calling in sick.33 By mid-April, the number of people testing positive in the community around the plant rose dramatically (Figure 4A). The orange line represents daily COVID-19 tests performed, and the red line represents the number of daily positive cases. Positivity for COVID-19 tests rose in parallel (Figure 4B), indicating an outbreak. By April, around 1 in 4 tests came back positive for county residents, many of whom worked at the plant. The plant temporarily closed on April 20, 2020, for cleaning and sanitizing.34 Health officials also began testing all employees. On April 25, 2020, the plant closed for 2 full weeks due to growing numbers of employees testing positive.35 While the health department would not disclose the number of employees who tested positive, county-wide data from the dashboard reveals 1558 (38% of those tested) individuals were positive for COVID-19 between early April and mid-May (Figure 4B). This equates to a rate of 3998 per 100 000 population, which is 1.5 times the rate for New York City and 8 times the national rate per 100 000 for COVID-19 infections. Hospitalizations were not immediate, but the epidemiologic data in Figure 4C show a rise following the plant closure until end of May 2020. The hospitalized population (Figure 4D) skews older, whereas the infected population (Figure 4A) skews younger, illustrating community-level impact of COVID-19. A total of 248 (15.9%) individuals were hospitalized and 28 (1.8%) died.
Figure 4.
A series of 3 panels representing how the Regenstrief COVID-19 Dashboard was used to examine a localized coronavirus disease 2019 (COVID-19) outbreak in Cass County, Indiana. (A) The component of the dashboard that monitors COVID-19 laboratory tests and their results. (B) A rollover chart that displays weekly testing figures, including the number of individuals tested, the number of individuals testing positive, and the calculated test positivity. (C) The component of the dashboard that visualizes hospitalization data for individuals with COVID-19. Admissions and discharges are included in the graph as well as critical care utilization.
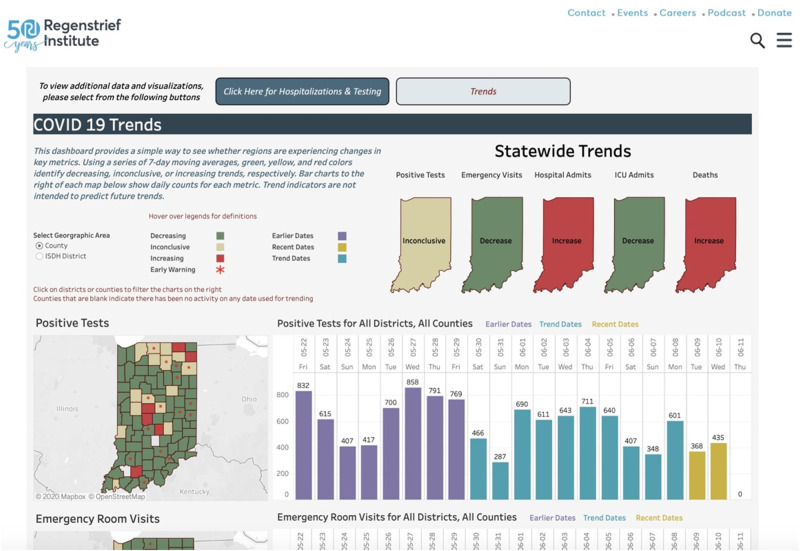
Monitoring localized COVID-19 trends
To support stakeholders (eg, health systems, community-based organizations) with identifying changing trends in their local area, we created a second page for the public dashboard to display recent patterns in COVID-19 metrics. This page identifies counties or demographic groups (eg, individuals 30-39 years of age) for which rates may be increasing or decreasing. This component of the dashboard, depicted in Figure 5 and released June 11, 2020, uses a stoplight color scheme to communicate the directionality of a given indicator. Red indicates an increasing trend in the most recent time period, and green indicates a decreasing trend during the most recent time period. Arrows are also used in the charts at the bottom of the page (not included in the figure) to help communicate direction, especially for those who may be colorblind.
Figure 5.
Trends section of the Regenstrief COVID-19 Dashboard. The figure depicts statewide trends in COVID-19 (coronavirus disease 2019) test results as well as geographical variation at the county level.
Trends are calculated using a 3-element vector composed of the differences (represented as increase, decrease, or no change) between 4 consecutive 7-day averages. The trends identify regions or groups that may be experiencing changes in key COVID-19 metrics. Bar charts to the right of each map below show daily counts for each metric. If a notable increase in daily counts is observed in the most recent 3 days, a red dot is displayed. A “notable increase” is defined as any individual count in the most recent 3 days that exceeds the average of the preceding 7 days.
Dashboard usage
To measure usage, we queried data from the IU Tableau Server for the 8-week period of June 21 to August 22, 2020. This period occurred several weeks after most major updates to the public dashboard were completed and during a time when the dashboards were regularly cited in broadcast media stories and social media posts. Combined there were 156 008 pageviews, of which 133 637 (74.2%) were unique. These pageviews occurred among 74 317 users, of which 67 821 (91.2%) were new users. Just over half (50.5%) of users accessed the public dashboard via a mobile device.
Although users came from 9 distinct countries, nearly all (96.6%) were from the United States. Of the 71 990 users located in the United States, most (70.8%) accessed the site from Indiana. Yet individuals in neighboring states of Illinois (7.9%), Kentucky (2.3%), Michigan (1.7%), and Ohio (1.4%) were also users. These users likely work in Indiana or live near the Indiana border.
DISCUSSION
The private and public versions of the Regenstrief COVID-19 Dashboard are applications of informatics methods designed to support PH surveillance and response to the COVID-19 pandemic. Visualization of data, a shared area of research in data science and informatics disciplines, has long been an important aspect of PH surveillance.36 Unlike past visualizations in the form of static reports published on a PH website, the dashboard represents a modern example of PH surveillance applications that offer interaction with dynamic visualized data, such as drilling down into county-level data or selecting a subpopulation. Interaction allows epidemiologists to explore trends and patterns of data more easily than traditional, more time-consuming approaches in which data are manipulated in spreadsheets. In a pandemic, this functionality enhances the ability to find patterns early, which can initiate PH investigation as well as response. Outbreaks of COVID-19 have not happened uniformly across the United States. Instead, outbreaks are highly localized events that require sophisticated applications for analysis of local data in near real time. The private dashboard helped PH officials identify trends and initiate response (eg, targeted testing in the community, shutting down impacted businesses) in Cass County, and it continues to help local and state health officers identify new clusters as well as shifting demographics among those impacted by COVID-19.
Neither dashboard would be possible without deep biomedical informatics expertise at Regenstrief, cross-sector partnerships, and the statewide HIE. The Faculty and Regenstrief Data Services team, already familiar with PH business processes, quickly pivoted their work to develop visualization applications to meet pandemic data needs. Together with PH leaders who regularly collaborate with Regenstrief faculty and staff, our response team defined then built the indicators necessary to track the spread of COVID-19. The operational HIE platforms in Indiana provided a solid foundation upon which the applications were quickly developed and deployed. Our close, unique relationship with the IHIE enabled Regenstrief to not only access the necessary data, but also expand available interfaces and connections to acquire new data streams. Staff at the IHIE further contributed ideas for analyzing and visualizing information, and they supported our efforts to secure, link, and present health information to PH authorities and the public. The role of our community-based HIE cannot be understated. Exchanges like the IHIE exist around the United States and globally, yet it is rare for HIE networks to support PH activities.21
Rapid harmonization of data was possible given the broad adoption of standards and support for interoperability available in Indiana. Regenstrief is the home of LOINC, and the IHIE works closely with its members to adopt and use data standards. Adoption of standards remains a challenge for many HIE networks, and it remains a work in progress for Indiana. Prior work documented limited adoption of data standards by Indiana health systems.37 Since then, the IHIE and Regenstrief worked to increase use of SNOMED CT and LOINC along with updated HL7 standards, including the C-CDA (Consolidated Clinical Document Architecture)38 and FHIR (Fast Health Interoperable Resources).39 When data are available in a clinical data network like INPC in a standardized format, retrieval becomes efficient and scalable. Efficiency is crucial during a pandemic when PH agencies desire rapid information exchange.
Where HIE infrastructures do not exist, states and nations should invest in HIE to support PH preparedness for pandemics while recognizing they further play a critical role in “peacetime” PH functions like chronic disease surveillance and immunization registries.40,41 Indiana took full advantage of prior funding opportunities from the federal government, including demonstration grants from the Agency for Healthcare Research and Quality and CDC as well as HITECH (Health Information Technology for Economic and Clinical Health Act) funding from the Office of the National Coordinator for Health Information Technology to develop its statewide infrastructure. The IHIE further created a business strategy (eg, sustainability model) to maintain and enhance the infrastructure over time through various HIE services. This includes a variety of HIE services that meet PH information needs, including notifiable disease reporting42 and syndromic surveillance.43 In Indiana, PH as well as research are primary functions of HIE, not simply “secondary uses” that risk being deprioritized when budgets need to be cut. Following the pandemic, the United States and other nations should invest in developing robust HIE infrastructures to support clinical, PH, and research capabilities to prepare for emerging infections disease outbreaks while addressing every day population health needs in their community. This sentiment is echoed in a recent manuscript written by authors from 15 academic medical centers, including ours,21 and it is embedded in the Public Health 3.0 framework described by DeSalvo et al.44
Beyond increased investment in HIE infrastructure focused on PH, states need to work with regional HIE networks to ensure they are sustainable and create value for providers, patients, and communities. As national and state-level architectures are developed, HIE networks need to play key roles in population health activities. For example, Medicaid programs desire to address social determinants and upstream issues which require connecting social service agencies with clinical providers. HIE networks can and should offer services that create value for Medicaid programs and populations, including better care coordination following discharge45 and improved access to wraparound services.46 Over time, the IHIE developed new services on top of its robust infrastructure that create value for state agencies, providers, and patients, which sustains the core infrastructure while expanding to meet evolving community needs. Enabling this was a governance structure that includes representation (eg, on the IHIE Board of Directors) by PH and research leaders, alongside representative leaders from regional healthcare systems. As the Indiana experience also demonstrates, regional public and population health needs are unlikely to be fully addressed by EHR-based HIE services (eg, Commonwell, Carequality), which focus on retrieval of information for a single patient. By developing services that are multipurpose and responsive to local and state PH needs, regional HIE networks can add value to population health initiatives that meaningfully transform care delivery and outcomes.
An important limitation of any informatics application is the underlying data. Data quality challenges are widespread, and our efforts are no exception. In particular, we note that the full power of these tools cannot be realized given limited data on race and ethnicity. A sizable proportion of individuals tested for COVID-19 are missing race and ethnicity data, and EHR data were not available to backfill missing data in ELR messages. As noted in prior work,47,48 health systems should improve their capture of race and ethnicity information. Improvements could include asking patients to self-report race and ethnicity directly into EHR or HIE systems using patient-facing tools.
CONCLUSION
Rapid development and deployment of PH informatics applications such as analytical dashboards during a pandemic requires a robust, interoperable health information infrastructure as well as strong cross-sector partnerships. Also critical is the ability to quickly engineer complex operational and infrastructural data processes to support mission critical PH data operations. These elements existed in Indiana, allowing the Regenstrief Institute, Indiana HIE, and PH agencies to quickly implement advanced visualization applications to monitor the spread and impact of COVID-19. Investment in infrastructure as well as rethinking the primary uses of HIE will be required to replicate Indiana’s response for the next pandemic in other states and nations.
FUNDING
This work was supported by a grant from the Indiana State Department of Health to the Regenstrief Institute to support COVID-19 pandemic response. BED is further supported by grant number R21HS025502 from the U.S. Agency for Healthcare Research and Quality. The funders did not have a role in the writing or editing of this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
AUTHOR CONTRIBUTIONS
The visualization applications were conceived and led by BED, PJE, and SJG. CM and AAB supported the data management needed to amalgamate the data, and CM developed the dashboards. UT facilitated the backend data services that support all aspects of the dashboards. AW, WM-C, and JLW coordinated the development and implementation of the dashboards along with the backend services necessary to operationalize them. BED drafted the manuscript. All authors contributed to revisions and approved the final version. All authors assume public responsibility for the accuracy and integrity of the work.
DATA AVAILABILITY STATEMENT
The data underlying the dashboards described in this paper originate from multiple sources, each of which has its own set of governance permitting access to third-parties. Publicly available datasets on COVID-19 indicators in Indiana represented on the dashboards can be downloaded from the Regenstrief Institute. Parties interested in these datasets should visit https://www.regenstrief.org/data-downloads/ to complete a request form and agree to the terms and conditions. They will then be permitted to download up-to-date data.
ACKNOWLEDGMENTS
We thank the Indiana University Decision Support Initiative, especially Mr Richard Shepherd, for their management of the Tableau infrastructure, troubleshooting technical challenges, and input on the visualizations. We further acknowledge the amazing support from the larger Regenstrief Data Services team whose many hours of extra effort are appreciated by the authors as well as the public health agencies in Indiana. Linking and receiving data from the state health agency was supported by the Management Performance Hub (https://www.in.gov/mph/). Finally, we thank our public health agency partners for their rapid input on the applications and their many hours on the front lines in response to COVID-19.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
References
- 1. World Health Organization. Coronavirus disease (COVID-19) pandemic. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Accessed September 15, 2020.
- 2. Menachemi N, Yiannoutsos CT, Dixon BE, et al. Population point prevalence of SARS-CoV-2 infection based on a statewide random sample - Indiana, April 25-29, 2020. MMWR Morb Mortal Wkly Rep 2020; 69 (29): 960–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rudavsky S. Indiana has passed 100,000 cases of the coronavirus. Here's what that means. Indianapolis Star. September 7, 2020. https://www.indystar.com/story/news/health/2020/09/07/indiana-coronavirus-why-surpassing-100-000-cases-matters/5721646002/ Accessed September 15, 2020. [Google Scholar]
- 4. Yoon P, Pollock D, Foldy S. National public health informatics, United States. In: Magnuson JA, Dixon BE, eds. Public Health Informatics and Information Systems. Cham, Switzerland: Springer International; 2020: 439–58. [Google Scholar]
- 5. Meigs M, Merrick R, Hinrichs S. Public health laboratories. In: Magnuson JA, Dixon BE, eds. Public Health Informatics and Information Systems. 3rd ed. Cham, Switzerland: Springer Nature; 2020: 259–68. [Google Scholar]
- 6. Dixon BE Rahurkar S. Public health informatics. In: Hoyt RE, Hersh WR, eds. Health Informatics: Practical Guide. 7th ed. Bethesda, MD: American Medical Informatics Association; 2018: 373–95. [Google Scholar]
- 7. Magnuson JA, Hopkins R, McFarlane TD. Informatics in disease prevention and epidemiology. In: Magnuson JA, Dixon BE, eds. Public Health Informatics and Information Systems. 3rd ed. Cham, Switzerland: Springer Nature; 2020: 239–58. [Google Scholar]
- 8. Sittig DF, Singh H. COVID-19 and the need for a national health information technology infrastructure. JAMA 2020; 323 (23): 2373–4. [DOI] [PubMed] [Google Scholar]
- 9. Dixon BE, Caine VA, Halverson PK. Deficient response to COVID-19 makes the case for evolving the public health system. Am J Prev Med 2020; 59 (6): 887–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cortez M, Tozzi J. Bloomberg What happened to the CDC? The storied disease agency is taking a back seat in the U.S. response to the coronavirus. Fortune. https://fortune.com/2020/04/12/cdc-coronavirus-testing-us-covid-19-response-trump-american-government/ Accessed June 10, 2020.
- 11. Stein M. The Federal Response to Covid-19 We Should Have Expected. https://www.publichealthpost.org/viewpoints/the-federal-response-to-covid-19-we-should-have-expected/ Accessed June 10, 2020.
- 12. Tahir D. Coronavirus adds new stress to antiquated health record-keeping. https://www.politico.com/news/2020/03/11/coronavirus-health-record-keeping-125841 Accessed September 15, 2020.
- 13. Meyer H. COVID data failures create pressure for public health system overhaul. https://www.modernhealthcare.com/information-systems/covid-data-failures-create-pressure-public-health-system-overhaul Accessed September 15, 2020.
- 14. Andrews RM. Statewide hospital discharge data: collection, use, limitations, and improvements. Health Serv Res 2015; 50 (Suppl 1): 1273–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc 2020; 27 (6): 853–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dixon BE, Grannis SJ. Information infrastructure to support public health. In: Magnuson JA, Dixon BE, eds. Public Health Informatics and Information Systems. 3rd ed. Cham, Switzerland: Springer Nature; 2020: 85–104. [Google Scholar]
- 17. Overhage JM. The Indiana Health Information Exchange. In: Dixon BE, ed. Health Information Exchange: Navigating and Managing a Network of Health Information Systems. 1st ed. Waltham, MA: Academic Press, 2016: 267–79. [Google Scholar]
- 18. Dixon BE, Tao G, Wang J, et al. An integrated surveillance system to examine testing, services, and outcomes for sexually transmitted diseases. Stud Health Technol Inform 2017; 245: 361–5. [PubMed] [Google Scholar]
- 19. Rahurkar S, McFarlane TD, Wang J, et al. Leveraging health information exchange to construct a registry for traumatic brain injury, spinal cord injury and stroke in Indiana. AMIA Annu Symp Proc 2017; 2017: 1440–9. [PMC free article] [PubMed] [Google Scholar]
- 20. Whipple EC, Dixon BE, McGowan JJ. Linking health information technology to patient safety and quality outcomes: a bibliometric analysis and review. Inform Health Soc Care 2013; 38 (1): 1–14. doi: 10.3109/17538157.2012.678451[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 21. Madhavan S, Bastarache L, Brown JS, et al. Use of electronic health records to support a public health response to the COVID-19 pandemic in the United States: a perspective from 15 academic medical centers. J Am Med Inform Assoc 2020. Nov 3 [E-pub ahead of print]; doi: 10.1093/jamia/ocaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zafar A, Dixon BE. Pulling back the covers: technical lessons of a real-world health information exchange. Stud Health Technol Inform 2007; 129 (Pt 1): 488–92. [PubMed] [Google Scholar]
- 23. Dixon BE, Zhang Z, Arno JN, Revere D, Joseph Gibson P, Grannis SJ. Improving notifiable disease case reporting through electronic information exchange-facilitated decision support: a controlled before-and-after trial. Public Health Rep 2020; 135 (3): 401–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fidahussein M, Friedlin J, Grannis S. Practical challenges in the secondary use of real-world data: the notifiable condition detector. AMIA Annu Symp Proc 2011; 2011: 402–8. [PMC free article] [PubMed] [Google Scholar]
- 25. LOINC Team. SARS-CoV-2 and COVID-19 related LOINC terms. 2020. https://loinc.org/sars-cov-2-and-covid-19/ Accessed July 4, 2020.
- 26. Regenstrief Institute. Public & Population Health Informatics. 2020. https://www.regenstrief.org/areas-of-focus/public-population-health-informatics/ Accessed July 4, 2020.
- 27. Overhage JM, Dexter PR, Perkins SM, et al. A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med 2002; 39 (1): 14–23. [DOI] [PubMed] [Google Scholar]
- 28. McDonald CJ, Overhage JM, Barnes M, et al. ; the INPC Management Committee. The Indiana network for patient care: a working local health information infrastructure. An example of a working infrastructure collaboration that links data from five health systems and hundreds of millions of entries. Health Affairs (Millwood) 2005; 24 (5): 1214–20. [DOI] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention. Principles of Epidemiology in Public Health Practice: An Introduction to Applied Epidemiology and Biostatistics. 3rd ed. Atlanta, GA: U.S. Department of Health and Human Services; 2012.
- 30. Dixon BE, Zou J, Comer KF, Rosenman M, Craig JL, Gibson PJ. Using electronic health record data to improve community health assessment. Front Public Health Serv Sys Res 2016; 5 (5): 50–6. [Google Scholar]
- 31. Comer KF, Grannis S, Dixon BE, Bodenhamer DJ, Wiehe SE. Incorporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Rep 2011; 126 (Suppl 3): 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Holcomb E. Back on Track Indiana: Governor Holcomb's Roadmap to Safely Reopen Indiana. 2020. https://backontrack.in.gov/ Accessed July 4, 2020.
- 33. Mills W. Logansport Pork Plant Deals with COVID-19 Cases. 2020. https://www.insideindianabusiness.com/story/42033453/cass-county-logansport-pork-plant-deals-with-covid19-cases Accessed July 5, 2020.
- 34. DePompei E, Bowman S. Meat plant in Logansport to close after 146 employees test positive for coronavirus. Indianapolis Star April 22, 2020. https://www.indystar.com/story/news/health/2020/04/22/tyson-logansport-closes-meat-plant-shuts-down-due-coronavirus/3006225001 Accessed July 5, 2020.
- 35. DePompei E. Tyson meat plant in Logansport to resume limited production after coronavirus outbreak. Indianapolis Star May 1, 2020. https://www.indystar.com/story/news/health/2020/05/01/tyson-meat-plant-logansport-reopen-after-coronavirus-outbreak/3063902001/ Accessed July 5, 2020.
- 36. Chiolero A, Buckeridge D. Glossary for public health surveillance in the age of data science. J Epidemiol Commun Health 2020; jech-2018-211654. doi: 10.1136/jech-2018-211654[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dixon BE, Vreeman DJ, Grannis SJ. The long road to semantic interoperability in support of public health: experiences from two states. J Biomed Inform 2014; 49: 3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hosseini M, Meade J, Schnitzius J, Dixon BE. Consolidating CCDs from multiple data sources: a modular approach. J Am Med Inform Assoc 2016; 23 (2): 317–23. [DOI] [PubMed] [Google Scholar]
- 39. Dixon BE, Taylor DE, Choi M, Riley M, Schneider T, Duke J. Integration of FHIR to facilitate electronic case reporting: results from a pilot study. Stud Health Technol Inform 2019; 264: 940–4. [DOI] [PubMed] [Google Scholar]
- 40. Hosseini M, Ahmadi M, Dixon BE. A service oriented architecture approach to achieve interoperability between immunization information systems in Iran. AMIA Annu Symp Proc 2014; 2014: 1797–805. [PMC free article] [PubMed] [Google Scholar]
- 41. Grannis S, Dixon BE, Brand B. Leveraging Immunization Data in the E-Health Era: Exploring the Value, Tradeoffs, and Future Directions of Immunization Data Exchange. Atlanta, GA: Public Health Informatics Institute; 2010.
- 42. Dixon BE, Zhang Z, Lai PTS, et al. Completeness and timeliness of notifiable disease reporting: a comparison of laboratory and provider reports submitted to a large county health department. BMC Med Inform Decis Mak 2017; 17 (1): 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Grannis SJ, Stevens KC, Merriwether R. Leveraging health information exchange to support public health situational awareness: the Indiana experience. Online J Public Health Inform 2010; 2 (2): ojphi.v2i2.3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. DeSalvo KB, O’Carroll PW, Koo D, Auerbach JM, Monroe JA. Public health 3.0: time for an upgrade. Am J Public Health 2016; 106 (4): 621–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Unruh MA, Jung HY, Kaushal R, Vest JR. Hospitalization event notifications and reductions in readmissions of Medicare fee-for-service beneficiaries in the Bronx, New York. J Am Med Inform Assoc 2017; 24 (e1): e150–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Vest JR, Menachemi N, Grannis SJ, et al. Impact of risk stratification on referrals and uptake of wraparound services that address social determinants: a stepped wedged trial. Am J Prev Med 2019; 56 (4): e125–33. [DOI] [PubMed] [Google Scholar]
- 47. Polubriaginof FCG, Ryan P, Salmasian H, et al. Challenges with quality of race and ethnicity data in observational databases. J Am Med Inform Assoc 2019; 26 (8–9): 730–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lee SJ, Grobe JE, Tiro JA. Assessing race and ethnicity data quality across cancer registries and EMRs in two hospitals. J Am Med Inform Assoc 2016; 23 (3): 627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying the dashboards described in this paper originate from multiple sources, each of which has its own set of governance permitting access to third-parties. Publicly available datasets on COVID-19 indicators in Indiana represented on the dashboards can be downloaded from the Regenstrief Institute. Parties interested in these datasets should visit https://www.regenstrief.org/data-downloads/ to complete a request form and agree to the terms and conditions. They will then be permitted to download up-to-date data.