This editorial refers to ‘Cardiac arrest in COVID-19: characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation’, by P. Sultanian et al., doi:10.1093/eurheartj/ehaa1067.
Since its first diagnosis in December 2019, countries across the world have faced one or several waves of coronavirus disease 2019 (COVID-19), the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Individual countries have adopted varying strategies for disease prevention and management, based on their medical resources and public health policies. Sweden has tried a unique strategy, avoiding lockdown, which should be taken into account in the interpretation of the results provided by Sultanian et al. in the present issue of the European Heart Journal.1 The impact of COVID-19 on out-of-hospital cardiac arrest (OHCA) has previously been observed and reported in several regions. The Lombardy region, Paris, and New York City have all reported increases in the number of OHCAs during the acute phase of the initial wave in March–May.2–4 However, the question remains regarding the respective roles of direct and indirect effects of COVID-19 in the increase of OHCA. The current study by Sultanian et al. sheds some light on this issue. Among 1946 cases of OHCA and 1080 cases of in-hospital cardiac arrest (IHCA) from the Swedish Registry for Cardiopulmonary Resuscitation during the first COVID-19 wave, COVID-19 infection was diagnosed in 10% and 16%, respectively. The 30-day mortality was increased by two- to three-fold in COVID-19-related cardiac arrest compared with non-COVID-19-related cardiac arrest.
Different mechanisms have been described to explain the deleterious association between COVID-19 and the occurrence of OHCA.2 Cardiac involvement leads to worse outcomes in infected subjects, with cardiovascular comorbidity.5 COVID-19 can directly cause OHCA through acute respiratory distress syndrome as well as an exaggerated immune response with cytokine storm, cardiovascular injury, and myocarditis.6 Some drug treatments, such as hydroxychloroquine or azithromycin, might also increase OHCA risk, especially in subjects with pre-existing cardiac disease.7 Acute cardiac events including heart failure and arrhythmias have been observed in the course of COVID-19, therefore making OHCA a possible presentation. Finally, a major prothrombotic state has been reported during COVID-19 infections,8 with a consequent increase in thrombo-embolic events including pulmonary embolism and acute coronary syndrome.9
However, although these aforementioned pathophysiological explanations are all plausible, the study of Sultanian et al. highlights that the proportion of actual COVID-19-positive patients among the OHCAs that occurred during the pandemic surge is relatively low. This finding is in line with the observations in Paris, where confirmed and suspected COVID-19 infections altogether accounted for only a third of the increase in OHCA incidence,2 arguing against an important direct role for COVID-19 and suggesting that the association between OHCA and the COVID-19 period could in part be driven by indirect effects. What are these likely indirect effects?
The COVID-19 pandemic had adverse consequences on routine healthcare and health systems.10 Lockdown and movement restrictions imposed in several countries, as well as the fear of acquiring infection in hospital, made patients reluctant to call the emergency medical services or present to emergency rooms, resulting in inappropriate delays and suboptimal care for urgent/emergent symptoms. In addition, the entire healthcare systems had to be reorganized in order to cope with the unprecedented surge of patients with a novel, highly contagious disease. Elective medical activity, including scheduled hospitalizations and consultations, had to be cancelled, with re-allocation of resources to meet the COVID-19 demand, as well as to avoid unnecessary exposure of stable patients to the risk of infection in hospital. In several regions, guidance to only seek care for severe symptoms was issued to avoid further overwhelming of the healthcare system. As patients could not reach their doctors, the decision on what constituted a severe symptom was left to the patient. Additionally, early cardiac signs including exertional angina or dyspnoea were not so noticeable to the patient due to the limited physical activity taking place during lockdown.
As regards overt acute cardiovascular events, their management was also jeopardized by the pandemic. The overwhelmed healthcare capacities had difficulties in handling further demands, given the pressure at the pre-hospital level, especially emergency medical services, and the in-hospital level, with shortages in critical care resources, including medical/paramedical teams, equipment, and intensive care beds. The subsequent delays in patient handling and treatment initiation resulted in more severe presentations.
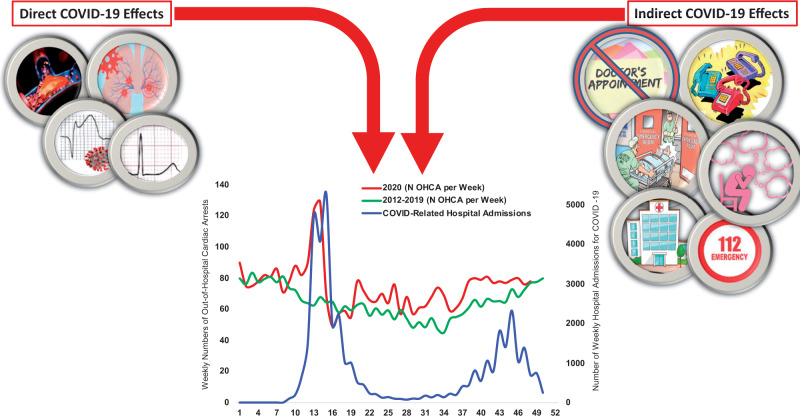
The evolution of the incidence of OHCAs during the second wave of the COVID-19 pandemic might provide more insights to further understanding the respective roles of direct and indirect effects of COVID-19 on OHCA. A doubling of the incidence of OHCA was reported in Paris during the first pandemic wave, with a concomitant reduction in OHCA survival. The updated data for the second wave of the pandemic presented in Graphical abstract show a lesser magnitude of increase in OHCA, despite a significant surge in COVID-19 infections. This suggests that the experience gained during the first pandemic has led to a better management of the second wave, thereby lessening the adverse impact of COVID-19 on routine healthcare. Indeed, the scientific and medical community has become more aware of the negative impact of the pandemic on non-COVID-19 diseases and of the risk of neglecting non-COVID-19 diseases. After an initial phase of the pandemic during which robust data were often difficult to obtain and publications were focused mainly on COVID-19 infection and treatment, more recent studies have looked at the negative impact of the pandemic on other diseases. Massive public campaigns have encouraged patients to pursue medical care despite the pandemic. On the clinical side, access to care was preserved, with general practitioners, cardiologists, and cardiac surgeons maintaining scheduled hospitalizations, interventions, and consultations, without systematically re-allocating resources for COVID-19, sometimes against strong administrative pressures.
Graphical abstract.
Greater Paris area: weekly numbers of out-of-hospital cardiac arrest in 2020, compared with previous years (2012–2019), as well as the number of hospital admissions for COVID-19.
The positive results of these measures on the incidence of OHCA, in contrast to the OHCA surge observed during the first wave, highlight the importance of anticipation and planning in the management of healthcare crises. However, unexpected disease outbreaks or excessive demands on the healthcare system are poorly accounted for in planning strategies. The observations with respect to the COVID-19 pandemic and OHCA should serve as an important wake-up call for healthcare systems worldwide to develop blueprints and contingency plans for preparedness in the case of such eventualities.
Conflict of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. Sultanian P, Lundgren P, Strömsöe A, Aune S, Bergström G, Hagberg E, Hollenberg J, Lindqvist J, Djärv T, Castelheim A, Thorén A, Hessulf F, Claesson A, Friber H, Nordberg P, Omerovic E, Rosengren A, Herlitz J, Rawshani A. Cardiac arrest in COVID-19: characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur Heart J 2021;42:doi:10.1093/eurheartj/ehaa1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, Sharifzadehgan A, Waldmann V, Beganton F, Narayanan K, Lafont A, Bougouin W, Jouven X. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health 2020;5:e437–e443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Bua D, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S CARe Lombardia Researchers. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med 2020;383:496–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lai PH, Lancet EA, Weiden MD, Webber MP, Zeig-Owens R, Hall CB, Prezant DJ. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol 2020;5:1154–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Libby P, Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J 2020;41:3038–3044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fried JA, Ramasubbu K, Bhatt R, Topkara VK, Clerkin KJ, Horn E, Rabbani L, Brodie D, Jain SS, Kirtane AJ, Masoumi A, Takeda K, Kumaraiah D, Burkhoff D, Leon M, Schwartz A, Uriel N, Sayer G. The variety of cardiovascular presentations of COVID-19. Circulation 2020;141:1930–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mercuro NJ, Yen CF, Shim DJ, Maher TR, McCoy CM, Zimetbaum PJ, Gold HS. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:1036–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;191:145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fauvel C, Weizman O, Trimaille A, Mika D, Pommier T, Pace N, Douair A, Barbin E, Fraix A, Bouchot O, Benmansour O, Godeau G, Mecheri Y, Lebourdon R, Yvorel C, Massin M, Leblon T, Chabbi C, Cugney E, Benabou L, Aubry M, Chan C, Boufoula I, Barnaud C, Bothorel L, Duceau B, Sutter W, Waldmann V, Bonnet G, Cohen A, Pezel T; Critical Covid-19 France Investigators. Pulmonary embolism in COVID-19 patients: a French multicentre cohort study. Eur Heart J 2020;41:3058–3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med 2020;382:2368–2371. [DOI] [PubMed] [Google Scholar]