Abstract
Aims
During the COVID-19 pandemic, concern regarding its effect on the management of non-communicable diseases has been raised. However, there are no data on the impact on cardiac implantable electronic devices (CIED) implantation rates. We aimed to determine the impact of SARS-CoV2 on the monthly incidence rates and type of pacemaker (PM) and implantable cardiac defibrillator (ICD) implantations in Catalonia before and after the declaration of the state of alarm in Spain on 14 March 2020.
Methods and results
Data on new CIED implantations for 2017–20 were prospectively collected by nine hospitals in Catalonia. A mixed model with random intercepts corrected for time was used to estimate the change in monthly CIED implantations. Compared to the pre-COVID-19 period, an absolute decrease of 56.5% was observed (54.7% in PM and 63.7% in ICD) in CIED implantation rates. Total CIED implantations for 2017–19 and January and February 2020 was 250/month (>195 PM and >55 ICD), decreasing to 207 (161 PM and 46 ICD) in March and 131 (108 PM and 23 ICD) in April 2020. In April 2020, there was a significant fall of 185.25 CIED implantations compared to 2018 [95% confidence interval (CI) 129.6–240.9; P < 0.001] and of 188 CIED compared to 2019 (95% CI 132.3–243.7; P < 0.001). No significant differences in the type of PM or ICD were observed, nor in the indication for primary or secondary prevention.
Conclusions
During the first wave of the COVID-19 pandemic, a substantial decrease in CIED implantations was observed in Catalonia. Our findings call for measures to avoid long-term social impact.
Keywords: Coronavirus, COVID-19, SARS-CoV2, Implantable cardiac defibrillator
What’s new?
Several publications have suggested a reduction of admissions for acute myocardial infarction and stroke during the COVID-19 pandemic. However, there is little evidence on its effect of the number of patients undergoing emergency and/or elective implantation of pacemakers (PMs) or cardioverter defibrillators.
This registry is the first to provide prospectively collected data on implantation rates of new cardiac implantable electronic devices (CIED) before and during the COVID-19 pandemic and highlights the dramatic impact of the COVID-19 pandemic.
A decline of >50% of CIED implantations [54.7% in pacemakers and 63.7% in implantable cardiac defibrillator (ICDs)], was observed, not only in elective interventions but also those that are normally urgent/emergency procedures (such as PM implantations and secondary prevention ICDs), suggesting a larger and multifactorial aetiology other than the mere reorganization of hospital resources to attend COVID-19 patients and suggesting the worrisome possibility of an increased out-of-hospital fatality due to these treatable conditions.
Introduction
With the spread of the coronavirus disease 2019 (COVID-19) worldwide, there is increasing concern about the potential effect the overwhelming burden that this disease puts on the health care system will have on the prevention and management of non-communicable diseases.
Since the beginning of the pandemic, major public health and cardiac organizations have issued guidance documents recommending deferral of all non-emergency procedures in order to manage the increasing need for hospital beds and human resources, including interventional procedures in chronic coronary syndromes and placement of cardiac implantable electronic devices (CIEDs).1–5 Furthermore, to reduce the spread of the virus, governments implemented several restrictive measures such as lockdowns and social distancing, and public health authorities in several countries warned the population against the use of emergency services for non-urgent conditions.
Several publications have suggested a decrease in the number of patients presenting to emergency departments with acute coronary syndromes.6–9 However, to date there are no data on the impact of the SARS-CoV2 pandemic on the rates of CIEDs implantation. Therefore, the aim of this study was to determine the impact of SARS-CoV2 on the monthly incidence rates and type of pacemaker (PM) and implantable cardiac defibrillator (ICD) implantations in Catalonia before and after the declaration of the state of alarm in Spain on 14 March 2020.
Methods
Study design and participating centres
This observational study included all CIED implantations in nine tertiary hospitals in Catalonia: six in Barcelona (Hospital Clínic de Barcelona, Hospital Vall d’Hebron, Hospital Sant Pau i Santa Creu, Hospital Bellvitge, Hospital del Mar and Hospital Germans Trias i Pujol), one in Girona (Hospital Dr Josep Trueta), one in Tarragona (Hospital Sant Joan de Deu), and one in Lleida (Hospital Arnau de Vilanova), accounting for 87% of all ICD implants in the region annually.10,11 The Ethical Committee of the coordinating centre (Hospital Clínic) was consulted waiving the need for approval given the nature of the data (aggregated).
Data collection
All of these centres prospectively collect data on PM and ICD implants for regional accounting as well as national registries of the Spanish Society of Cardiology.
For the purpose of this study, we collected data on new monthly CIED implantations for the years 2017 to September 2020 to account for temporal variations/trends. March 2020 was divided into the 1st and 2nd fortnights to quantify the number of CIED implantations during the COVID-19 period, which was considered between 15 March 2020 and 30 April 2020. A pre-COVID-19 period between 1 February 2020 and 14 March 2020 was used for comparisons.
Statistical analysis
Continuous variables are presented as counts or median [interquartile range (IQR)]. Categorical variables are presented as frequencies and percentages. The annual median number of implants per month was calculated using the total number of implantations between January and April. The median number of implantations per month in 2020 was also calculated separately for the pre-COVID-19 period using January and February. March 2020 was excluded to avoid over- or under-estimations. Standardized monthly implantation rates were calculated using the European Commission’s official dataset on number of monthly working days in Spain,12 and adjusted to the average number of working days per month in Spain (21 days).
Categorical variables were compared with the χ2 test. A mixed model with random intercepts corrected for a time as a categorical variable was used to estimate the change in monthly CIED implantations and to compare CIED implantations in the pre-COVID-19 and COVID-19 periods. To assess the difference in trajectories of total cumulative CIED implantations we used a time per period-interaction model.
For all tests, a two-sided P-value <0.05 was considered significant. Statistical analysis was performed using R software for Windows version 3.5.3 (R Foundation for Statistical Computing, Vienna, Austria, 2019). There were no missing data for the variables included.
Results
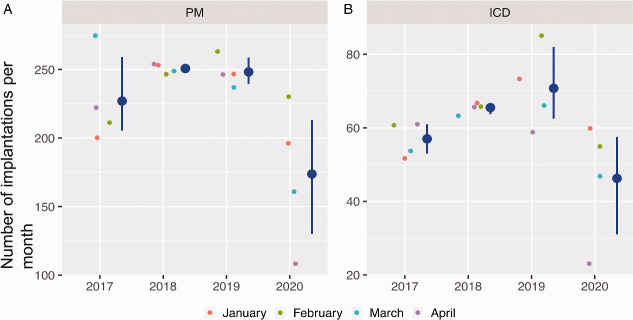
The total number of PM and ICD implantations for the 1st quarter and the adjusted rate per working dates gradually increased between 2017 and 2019 (Figure 1, Table 1). When compared to the pre-COVID-19 period (1 February to 14 March 2020), after mandatory lockdown, a significant decrease of 56.5% was observed in CIED implantation rates (Table 2).
Figure 1.
Total number of CIED implantations adjusted per working days for the 1st quarter of years 2017 to 2020. CIED, cardiac implantable electronic device; ICD, implantable cardiac defibrillator; PM, pacemaker.
Table 1.
Total number of implants by device type.
| A. Pacemaker implantations during the first quarter (2017–20) | ||||||
|---|---|---|---|---|---|---|
| 2017 | January | February | March | April | Total | |
| Single-chamber PM | 96 (97a) | 91 (96a) | 137 (126a) | 107 (127a) | 431 (446a) | |
| Dual-chamber PM | 93 (94a) | 108 (114a) | 127 (117a) | 109 (130a) | 437 (455a) | |
| CRT PM | 11 (11a) | 12 (13a) | 11 (10a) | 6 (7a) | 40 (41a) | |
| Total | 200 (202a) | 211 (223a) | 275 (253a) | 222 (264a) | 908 (942a) | |
| 2018 | January | February | March | April | Total | |
| Single-chamber PM | 107 (102a) | 108 (114a) | 110 (114a) | 115 (118a) | 440 (448a) | |
| Dual-chamber PM | 138 (132a) | 104 (110a) | 127 (132a) | 129 (133a) | 498 (507a) | |
| CRT PM | 8 (8a) | 12 (13a) | 12 (12a) | 10 (10a) | 42 (43a) | |
| Total | 253 (242a) | 224 (237a) | 249 (258a) | 254 (261a) | 980 (998a) | |
| 2019 | January | February | March | April | Total | |
| Single-chamber PM | 104 (104a) | 105 (111a) | 106 (107a) | 98 (109a) | 413 (425a) | |
| Dual-chamber PM | 130 (130a) | 140 (148a) | 117 (118a) | 138 (149a) | 525 (542a) | |
| CRT PM | 13 (13a) | 18 (19a) | 14 (14a) | 10 (20a) | 55 (57a) | |
| Total | 247 (247a) | 263 (278a) | 237 (238a) | 246 (278a) | 993 (1024 a) | |
| 2020 | January | February | 1st to 15th March | 16th to 31st March | April | Total |
| Single-chamber PM | 72 (72a) | 90 (95a) | 48 (46 a) | 29 (28a) | 41 (43a) | 277 (284a) |
| Dual-chamber PM | 110 (110a) | 124 (131a) | 58 (55a) | 18 (17a) | 62 (66a) | 375 (379a) |
| CRT PM | 14 (14a) | 16 (17a) | 7 (7a) | 1 (1a) | 5 (5a) | 42 (44a) |
| TOTAL | 196 (196a) | 230 (243a) | 113 (108a) | 48 (46a) | 108 (115a) | 694 (708a) |
| B. Implantable cardiac defibrillators during the first quarter (2017–2020). | ||||||
|---|---|---|---|---|---|---|
| 2017 | January | February | March | April | Total | |
| Single-chamber ICD | 20 (20a) | 35 (37a) | 29 (27a) | 29 (34a) | 113 (118a) | |
| Dual-chamber ICD | 8 (8a) | 3 (3a) | 8 (7a) | 4 (5a) | 23 (23a) | |
| CRT ICD | 20 (20a) | 16 (17a) | 16 (15a) | 21 (25a) | 73 (77a) | |
| S-ICD | 4 (4a) | 7 (7a) | 1 (1a) | 7 (8a) | 19 (20a) | |
| Total | 52 (52a) | 61 (64a) | 54 (50a) | 61 (72a) | 228 (238a) | |
| 2018 | January | February | March | April | Total | |
| Single-chamber ICD | 36 (34a) | 37 (39a) | 34 (35a) | 41 (42a) | 148 (151a) | |
| Dual-chamber ICD | 4 (4a) | 4 (4a) | 5 (5a) | 3 (3a) | 16 (16a) | |
| CRT ICD | 21 (20a) | 20 (21a) | 19 (20a) | 20 (21a) | 80 (81a) | |
| S-ICD | 6 (6a) | 5 (5a) | 5 (5a) | 2 (2a) | 18 (18a) | |
| Total | 67 (64a) | 66 (69a) | 63 (65a) | 66 (68a) | 261 (266a) | |
| 2019 | January | February | March | April | Total | |
| Single-chamber ICD | 40 (40a) | 50 (53a) | 35 (35a) | 31 (33a) | 156 (161a) | |
| Dual-chamber ICD | 7 (7a) | 5 (5a) | 5 (5a) | 4 (4a) | 21 (21a) | |
| CRT ICD | 18 (18a) | 22 (23a) | 21 (21a) | 21 (22a) | 82 (84a) | |
| S-ICD | 8 (8a) | 8 (8a) | 5 (5a) | 3 (3a) | 24 (24a) | |
| Total | 73 (73a) | 85 (89a) | 66 (66a) | 59 (62a) | 283 (290) | |
| 2020 | January | February | 1st to 15th March | 16th to 31st March | April | Total |
| Single-chamber ICD | 31 (31a) | 32 (34a) | 20 (19a) | 5 (5a) | 9 (10a) | 97 (98a) |
| Dual-chamber ICD | 6 (6a) | 6 (6a) | 1 (1a) | 0 (0a) | 1 (1a) | 14 (14a) |
| CRT ICD | 18 (18a) | 15 (16a) | 11 (11a) | 4 (4a) | 13 (14 a) | 61 (62a) |
| S-ICD | 5 (5 a) | 2 (2a) | 4 (4a) | 1 (1a) | 0 (0a) | 12 (12a) |
| Total | 60 (60a) | 55 (58a) | 36 (35a) | 10 (10a) | 23 (25a) | 184 (186a) |
CRT, cardiac resynchronization therapy; ICD, implantable cardiac defibrillator; PM, pacemaker; S-ICD, subcutaneous implantable cardiac defibrillator.
Monthly rates adjusted per working days in Spain.12
Table 2.
Comparison of total number of implantations before and after mandatory lockdown in Spain
| Pre-COVID-19 period (1st February 2020 to 15th March 2020) | COVID-19 period (16th March 2020 to 30th April 2020) | Decrease % | ||
|---|---|---|---|---|
| PM total | 343 | 156 | ↓54.5% | <0.001 |
| PM single-chamber | 138 (40.2%) | 70 (44.9%) | ↓ 49.3% | |
| PM dual-chamber | 182 (53.1%) | 80 (51.3%) | ↓56.0% | |
| PM CRT | 23 (6.7%) | 6 (3.8%) | ↓73.9% | |
| ICD total | 91 | 33 | ↓63.7% | <0.001 |
| ICD single-chamber | 52 (57.1%) | 14 (42.4%) | ↓73.1% | |
| ICD dual-chamber | 7 (7.7%) | 1 (3.0%) | ↓85.7% | |
| ICD CRT | 26 (28.6%) | 17 (51.5%) | ↓34.6% | |
| ICD S-ICD | 6 (6.6%) | 1 (3.0%) | ↓83.3% | |
| Primary prevention | 48 (52.7%) | 16 (48.5%) | ↓66.7% | |
| ICD single-chamber | 25 | 4 | ||
| ICD dual-chamber | 3 | 0 | ||
| ICD CRT | 16 | 12 | ||
| S-ICD | 4 | 0 | ||
| Secondary prevention | 43 (47.3%) | 17 (51.5%) | ↓60.5% | |
| ICD single-chamber | 27 | 10 | ||
| ICD dual-chamber | 4 | 1 | ||
| ICD CRT | 10 | 5 | ||
| S-ICD | 2 | 1 | ||
| Overall | 434 | 189 | ↓56.5% | <0.001 |
CRT, cardiac resynchronization therapy; ICD, implantable cardiac defibrillator; S-ICD, subcutaneous implantable cardiac defibrillator; PM, pacemaker.
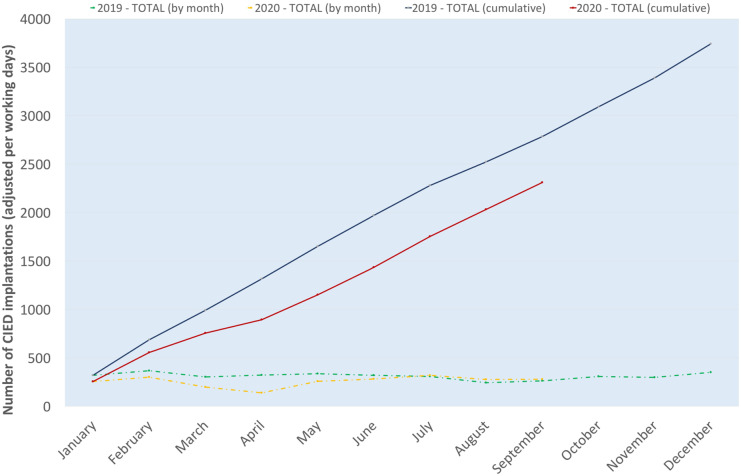
The total number of CIED implantations for years 2017–19 (January to April) and 2020 (January and February) was >250 per month. In contrast, the total number of CIED implantations decreased to 207 in March and 131 in April 2020. The median monthly CIED implantation rate reported by the 9 participating centres was 278 (IQR 27.5), 316 (IQR 7.25), and 312 (IQR 22.5) for the years 2017, 2018, and 2019. The median CIED implantation rate per month in 2020 was 232 (IQR 74.5): 270 (IQR 12.5) in the pre-COVID-19 period, decreasing to 131 implantations in April (Figure 2).
Figure 2.
Median CIED implantation rate per month for years 2017–20. (A) Pacemakers. (B) Implantable cardiac defibrillators. CIED, cardiac implantable electronic device; ICD, implantable cardiac defibrillator; PM, pacemaker.
The model estimated a significant fall of 153 CIED implantations between 2017 and April 2020 [95% confidence interval (CI) 97.3–208.7; P = 0.0037], 185.25 between 2018 and April 2020 (95% CI 129.6–240.9; P < 0.001) and a decrease of 188 CIED implantations between 2019 and April 2020 (95% CI 132.3–243.0.7; P < 0.001).
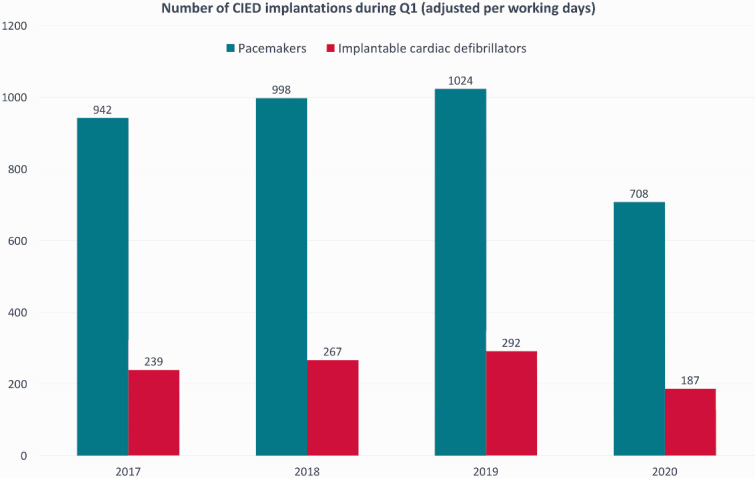
Following the peak of the pandemic (May to September 2020), the number of monthly implantations increased to levels comparable to 2019 (Figure 3); nonetheless, the cumulative number of CIEDs implanted during 2020 remains significantly lower than 2019 (P < 0.0001).
Figure 3.
Number of monthly and cumulative CIED implantations adjusted per working days for years 2019 and 2020. CIED, cardiac implantable electronic device.
Among the Barcelona area, the median monthly implantations during the 1st quarter of 2017 to 2019 was 212 (IQR 14), 232 (IQR 7.75), and 227 (IQR 10.5), respectively, decreasing to 166 (IQR 53.8) in the 1st quarter of 2020 (Supplementary material online, Table S1). The model estimated a significant fall of 126 CIED implantations between 2017 and April 2020 (95% CI 82.7–169.3; P < 0.0001), 139.8 between 2018 and April 2020 (95% CI 96.5–183.2; P < 0.0001) and a decrease of 136.3 CIED implantations between 2019 and April 2020 (95% CI 93.0–179.7; P < 0.0001). Among the hospitals outside the Barcelona area, the median monthly implantation rates were 66.5 (IQR 165), 84 (IQR 155), 90 (IQR 7.5), and 65 (19.2) for the 1st quarter of 2017 to 2020, respectively (Supplementary material online, Table S1). Despite the decrease in absolute numbers, the model did not estimate a significant fall between any of the comparisons: decrease of 83 CIED implantations between 2017 and April 2020 (95% CI 7.8–158.2; P = 0.3201), 98.3 CIED implantations between 2018 and April 2020 (95% CI 23.1–173.5; P = 0.1804) and a decrease of 109 CIED implantations between 2019 and April 2020 (95% CI 33.8–184.2; P = 0·1170).
In-depth implantation counts by centre and device type, as well as additional summary figures and tables are provided in the Supplementary material online, Appendix
Pacemaker implantations
The absolute number of PM implantations after lockdown was declared on 14 March 2020 was 156, which represents a reduction of 54.7% compared to the pre-COVID-19 period.
The total number of PM implantations for 2017–19 (January to April) and 2020 (January and February) was >195 per month. In contrast, the total number of PM implantations decreased to 161 in March and 108 in April 2020. The median monthly PM implantation rate reported by the nine participating centres was 216.5 (IQR 27.0.0), 251 (IQR 4.75), and 246.5 (IQR 7.25) for the years 2017, 2018, and 2019. The median PM implantation rate per month in 2020 was 178 (IQR 57.5): 213 (IQR 17.0) in the pre-COVID-19 period, decreasing to 108 implantations in April (Figure 2).
The model showed a decrease of 119.0 PM implantations between 2017 and April 2020 (95% CI 67.3–170.7; P = 0.0119), 142.8 between 2018 and April 2020 (95% CI 91.06–194.5; P = 0.0035) and a decrease of 140.2 PM implantations between 2019 and April 2020 (95% CI 88.5–191.9; P = 0.004).
No significant differences in the type of PM implanted were observed when comparing the pre-COVID-19 to the COVID-19 period (P = 0.345).
Implantable cardiac defibrillator implantations
The absolute number of ICD implantations after lockdown was declared on 14th March 2020 was 33, representing a 63.0.7% decrease compared to the pre-COVID-19 period (66.7% in primary prevention and 60.5% in secondary prevention).
The total number of ICD implantations for 2017–19 (January to April) and 2020 (January and February) was >55 per month. In contrast, the total number of ICD implantations decreased to 46 in March and 23 in April 2020. The median monthly ICD implantation rate reported by the 9 participating centres was 57.5 (IQR 7.5), 66 (IQR 1.0) and 69.5 (IQR 11.75) for the years 2017, 2018, and 2019. The median CIED implantation rate per month in 2020 was 51.5 (IQR 16.0): 57.5 (IQR 2.5) in the pre-COVID-19 period, decreasing to 23 implantations in April (Figure 2).
The model showed a decrease of 34.0 ICD implantations between 2017 and April 2020 (95% CI 17.12–50.88; P = 0.0268), 42.5 between 2018 and April 2020 (95% CI 25.6–59.4; P = 0.0067) and a decrease of 47.75 ICD implantations between 2019 and April 2020 (95% CI 30.9–64.6; P = 0.0030).
When compared to the pre-COVID-19 period, there was no significant difference in the type of ICD implanted in the COVID-19 period (P = 0.0566), although no subcutaneous ICD (S-ICD) was placed following lockdown in any centre and there was a higher proportion of cardiac resynchronization therapy-ICD placement [28.6% (16/26 for primary prevention] in the pre-COVID-19 period vs. 51.55% 12/17 for primary prevention) in the COVID-19 period]. Furthermore, there were also no differences in the indication of ICD implantation: 48 out of 91 (52.7%) ICD implantations were primary prevention in the pre-COVID-19 period compared to 16 out 33 (48.5%) ICD implantations in the COVID-19 period (P = 0.829).
Discussion
Concern regarding the impact that COVID-19 is having on cardiovascular care has been raised. Although available data are mainly focused on the reduction of admissions for acute myocardial infarction (MI) and stroke in emergency departments,7–9,13–15 some reports also show a fall in urgent admissions for cardiac arrhythmias.15–17 Our analysis of CIED implantation activity in nine tertiary hospitals in Catalonia, Spain, which accounts for almost 90% of ICD implantations in the Catalonian region, showed a dramatic reduction (>50%) in CIED placements following the COVID-19 pandemic. Two recent small retrospective studies in Italy suggested a fall in PM placements.17,18 In Germany, a retrospective analysis of claims data showed a significant decrease in emergency hospitalizations for heart rhythm disorders (including bradycardia) and a reduction of cardiac rhythm management procedures (composite of PM and ICDs).16 To further support the prior findings, in our study, we provide prospectively collected data for the past 4 years to account for temporal variations/trends detailed analysis type of device.
The description of the underlying causes leading to the marked decline in CIED implantation rates is beyond the scope of this study, but they are likely to be multifactorial. First, following the outbreak of the SARS-CoV2 infection, many governments took extraordinary measures including mandatory confinement and recommended avoidance of non-urgent hospital visits to preserve hospital beds and prepare for a possible shortage of human resources. These measures may have discouraged patients from consulting emergency departments or primary care practices. Second, with the purpose of protecting hospital resources, elective procedures and non-critical visits were postponed, leading to the cancellation of elective CIED implantations. This global trend was further enhanced by the recommendations of several cardiac societies to avoid non-urgent electrophysiological procedures including ICDs for primary prevention.1–5 Third, although speculative, it is possible that the fear of contagion also discouraged patients from accessing emergency medical services. The fact that the COVID-19 fatality rate is higher with advanced age has been widely reported in the media, and therefore, patient reluctance to present to the hospital would not be unexpected. Finally, it is possible that emergency departments were more focused on managing the pandemic, leading to reduced awareness of other clinical conditions or deferral of less urgent cases. This has been suggested as a possible cause for the significant decrease in non-ST-elevation myocardial infarction hospitalizations compared to ST-elevation events.6,9
These alarming data suggest the possibility of increased morbidity and mortality due to the unintended consequences of more than half of patients remaining in need of PM or ICD because of the implementation of public health policies during the current pandemic. Furthermore, data from the Spanish Society Cardiology of Cardiology have shown that, since 2005, there have been consistently lower ICD implantation rates per million population in Spain compared with the rest of Europe (overall implantation rate per million population was 152 in 2018 in Spain compared to 306 in Europe), with large geographical disparities and Catalonia always below the national average.10,11,19–31 Our data show the gradual increase in the number of CIED implantations between 2017 and 2019 in Catalonia, which has been suddenly stopped by COVID-19. The effect of the current pandemic may increase the existing inequalities if this reduction in ICD is experienced differently across regions.
The fact that the reduction in ICD implantation rates affected both primary and secondary prevention indications equally is particularly intriguing, considering that the recommendation of international societies of avoiding non-urgent/elective procedures only included ICD implantation for primary prevention.1–5 Several studies have suggested an increased incidence in out-of-hospital cardiac arrest fatality rates, which may underlie the marked reduction in ICD implantations for secondary prevention. Nonetheless, further studies are needed to evaluate this hypothesis.32,33
To reduce the risk of a major decline in new CIED implantations in the event of a resurgence of the pandemic, several health policy measures could be considered, including awareness campaigns for the general population (how to recognize cardiac symptoms and how to proceed), appropriate healthcare resource distribution (avoiding cancellation of all non-emergent procedures and ensuring adequate response of emergency medical systems), and dedicated COVID-19 and non-COVID-19 patient pathways (to reduce risk and the fear of contagion in the healthcare facility). Unfortunately, evidence-based evaluation of these policies in the current pandemic is lacking yet.
Limitations
This multicentre prospective study has several limitations. First, due to the limitation in human resources during the COVID-19 pandemic, we have not been able to collect extensive data on relevant variables such as patient sociodemographic data, indication for CIED implantation, and clinical presentation, among other data. For the same reason, we were only able to analyse CIED implantations by weeks from February to September 2020. Finally, and foremostly, the observational nature of the study did not allow any conclusion to be drawn in relation to the underlying causes for the significant decrease in CIED implantations during the COVID-19 pandemic. Over-treatment in the pre-COVID-19 period may be raised as a potential concern; however, the long life-expectancy in Spain,34,35 together with data from the Spanish and European Societies of Cardiology, suggest otherwise.10,11,19–31,36 Questions may be raised whether these patients were treated outside Catalonia; however, the lockdown measures during the alarm state, travel restrictions between communities thereafter, and, most importantly, the structured healthcare system provision in Spain (divided by regions), reduce the likelihood to a minimum.
Conclusion
In conclusion, during the COVID-19 pandemic, a worrying decrease in CIED implantations was observed in Catalonia. Further investigations should assess the possible underlying causes and the possible resulting adverse outcomes, such as an increase in morbidity and mortality.
Our findings call for measures to avoid long-term social impact.
Data availability
All data collected for the study will be made available as supplementary material to anyone who wishes access it for any purpose. Data will include detailed counts of cardiac implantable electronic device placement from 2017 to April 2020, by type and centre. The data will be accessible immediately following publication with no end date.
Conflict of interest: E.A., MD, PhD, MSc: Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; Lluis Mont, MD, PhD: Speaking and consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic; Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; J.M.T., MD, PhD: Consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic; Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; R.B., MSc: Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; N.R.-G., MD, PhD, MSc: Speaking honorarium from Abbott; J.F.-P., MD: Speaking honorarium from Abbott; Alba Santos-Ortega MD: Speaking honorarium from Abbott; J.M.G., MD, PhD: Speaking and consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic; E.R.-F., MD, PhD: Speaking and consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic. Other authors declare no conflict of interests.
Supplementary Material
References
- 1. The European Society for Cardiology. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance (21 April 2020, date last accessed).
- 2. Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M et al. Guidance for cardiac electrophysiology during the coronavirus (COVID-19) pandemic from the Heart Rhythm Society COVID-19 task force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Circulation 2020;17:e233–e241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hassan A, Arora RC, Adams C, Bouchard D, Cook R, Gunning D et al. Cardiac surgery in Canada during the COVID-19 pandemic: a guidance statement from the Canadian Society of Cardiac Surgeons. Can J Cardiol 2020;36:952–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wood DA, Sathananthan J, Gin K, Mansour S, Ly HQ, Quraishi A-U-R et al. Precautions and procedures for coronary and structural cardiac interventions during the COVID-19 pandemic: guidance from Canadian Association of Interventional Cardiology. Can J Cardiol 2020;36:780–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Haft JW, Atluri P, Ailawadi G, Engelman DT, Grant MC, Hassan A et al. Adult cardiac surgery during the COVID-19 pandemic: a tiered patient triage guidance statement. Ann Thorac Surg 2020;110: 697– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung S-H et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020;383:691–3. [DOI] [PubMed] [Google Scholar]
- 8. Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic. A survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes 2020;6:210–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fernández Lozano I, Osca Asensi J, Alzueta Rodríguez J . Spanish Implantable Cardioverter-defibrillator Registry. 14th Official Report of the Spanish Society of Cardiology Electrophysiology and Arrhythmias Section (2017). Rev Esp Cardiol (Engl Ed) 2018;71:1047–58. [DOI] [PubMed] [Google Scholar]
- 11. Fernández Lozano I, Osca Asensi J, Alzueta Rodríguez J . Spanish Implantable Cardioverter-defibrillator Registry. 15th Official Report of the Spanish Society of Cardiology Electrophysiology and Arrhythmias Section (2018). Rev Esp Cardiol (Engl Ed) 2019;72:1054–64. [DOI] [PubMed] [Google Scholar]
- 12. European Comission. Euro area and EU working days to build Calendar Adjustment Regressor. https://ec.europa.eu/eurostat/cros/content/euro-area-and-eu-working-days-build-calendar-adjustment-regressor_en [https://ec.europa.eu/eurostat/cros/content/euro-area-and-eu-working-days-build-calendar-adjustment-regressor_en].
- 13. Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol 2020;83:213–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R . Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke 2020;51:1996–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Toniolo M, Negri F, Antonutti M, Masè M, Facchin D . Unpredictable fall of severe emergent cardiovascular diseases hospital admissions during the COVID-19 pandemic: experience of a Single Large Center in Northern Italy. J Am Heart Assoc 2020;9:e017122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bollmann A, Hohenstein S, Meier-Hellmann A, Kuhlen R, Hindricks G .on behalf of Helios hospitals Group. Emergency hospital admissions and interventional treatments for heart failure and cardiac arrhythmias in Germany during the Covid-19 outbreak: insights from the German-wide Helios hospital network. Eur Heart J Qual Care Clin Outcomes 2020;6:221–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Compagnucci P, Volpato G, Pascucci R, Falanga U, Misiani A, Molini S et al. Impact of the COVID-19 pandemic on a tertiary-level electrophysiology laboratory in Italy. Circ: Arrhythmia Electrophysiol 2020;13:e008774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Migliore F, Zorzi A, Gregori D, Monte AD, Falzone PV, Verlato R, et al. on behalf of The Padua School of Cardiology Network. Urgent pacemaker implantation rates in the Veneto Region of Italy after the COVID-19 outbreak. Circ: Arrhythmia Electrophysiol 2020;13:e008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peinado R, Arenal A, Arribas F, Torrecilla E, Alvarez M, Ormaetxe JM et al. Spanish implantable cardioverter-defibrillator registry. First official report of the spanish society of cardiology working group on implantable cardioverter-defibrillators (2002-2004). Rev Esp Cardiol 2005;58:1435–49. [PubMed] [Google Scholar]
- 20. Peinado R, Torrecilla EG, Ormaetxe J, Alvarez M . Spanish on Registry Implantable Cardioverter Defibrillator Second Official Report of the Spanish Society of Cardiology Working Group on Implantable Cardioverter Defibrillators (2005). Rev Esp Cardiol 2006;59:1292–302. [DOI] [PubMed] [Google Scholar]
- 21. Peinado R, Torrecilla EG, Ormaetxe J, Alvarez M . [Spanish Implantable Cardioverter-Defibrillator Registry. Third Official Report of the Spanish Society of Cardiology Working Group on Implantable Cardioverter-Defibrillators (2006)]. Rev Esp Cardiol 2007;60:1290–301. [DOI] [PubMed] [Google Scholar]
- 22. Peinado R, Torrecilla EG, Ormaetxe J, Alvarez M . [Spanish Implantable Cardioverter-Defibrillator Registry. Fourth Official Report of the Spanish Society of Cardiology Working Group on Implantable Cardioverter-Defibrillators (2007)]. Rev Esp Cardiol 2008;61:1191–203. [PubMed] [Google Scholar]
- 23. Peinado R, Torrecilla EG, Ormaetxe J, Álvarez M, Cózar R, Alzueta J . Implantable Cardioverter-Defibrillator Registry. 5th Official Report of the Spanish Society of Cardiology Working Group on Implantable Cardioverter-Defibrillators (2008). Rev Esp Cardiol 2009;62:1435–49. [PubMed] [Google Scholar]
- 24. Alzueta J, Linde A, Barrera A, Peña J, Peinado R . Implantable Cardioverter-Defibrillator Registry. Sixth Official Report of the Spanish Society Of Cardiology Working Group on Implantable Cardioverter-defibrillators (2009). Rev Esp Cardiol 2010;63:1468–81. [PubMed] [Google Scholar]
- 25. Alzueta J, Fernández JM . [Spanish Implantable Cardioverter-Defibrillator Registry. Seventh Official Report of the Spanish Society of Cardiology Working Group on Implantable Cardioverter-Defibrillators (2010)]. Rev Esp Cardiol 2011;64:1023–34. [DOI] [PubMed] [Google Scholar]
- 26. Alzueta J, Fernández JM . Spanish Implantable Cardioverter-Defibrillator Registry. Eighth Official Report of the Spanish Society of Cardiology Working Group on Implantable Cardioverter-Defibrillators (2011). Rev Esp Cardiol (Engl Ed) 2012;65:1019–29. [DOI] [PubMed] [Google Scholar]
- 27. Alzueta J, Fernández JM . Spanish Implantable Cardioverter-Defibrillator Registry. Ninth Official Report of the Spanish Society of Cardiology Electrophysiology and Arrhythmias Section (2012). Rev Esp Cardiol (Engl Ed) 2013;66:881–93. [DOI] [PubMed] [Google Scholar]
- 28. Alzueta J, Pedrote A, Fernández Lozano I . Spanish Implantable Cardioverter-defibrillator Registry. Tenth Official Report of the Spanish Society of Cardiology Electrophysiology and Arrhythmias Section (2013). Rev Esp Cardiol (Engl Ed) 2014;67:936–47. [DOI] [PubMed] [Google Scholar]
- 29. Alzueta J, Asso A, Quesada A . Spanish Implantable Cardioverter-defibrillator Registry. Eleventh Official Report of the Spanish Society of Cardiology Electrophysiology and Arrhythmias Section (2014). Rev Esp Cardiol (Engl Ed) 2015;68:996–1007. [DOI] [PubMed] [Google Scholar]
- 30. Alzueta J, Fernández-Lozano I, Barrera A . Spanish Implantable Cardioverter-Defibrillator Registry. Twelfth Official Report of the Spanish Society of Cardiology Electrophysiology and Arrhythmias Section (2015). Rev Esp Cardiol (Engl Ed) 2016;69:1168–79. [DOI] [PubMed] [Google Scholar]
- 31. Alzueta J, Fernández-Lozano I . Spanish Implantable Cardioverter-Defibrillator Registry. 13th Official Report of the Spanish Society of Cardiology Electrophysiology and Arrhythmias Section (2016). Rev Esp Cardiol (Engl Ed) 2017;70:960–70. [DOI] [PubMed] [Google Scholar]
- 32. Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C . Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health 2020;S2468-667:30117–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med 2020;383:496–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. OECD. Health at a Glance 2019. OECD Indicators. Paris (France): OECD Publishing; 2019. [Google Scholar]
- 35. OECD. OECD data: life expectancy at birth. https://data.oecd.org/healthstat/life-expectancy-at-birth.htm. OECD Publishing; 2020.
- 36. Raatikainen MJP, Arnar DO, Merkely B, Nielsen JC, Hindricks G, Heidbuchel H et al. A decade of information on the use of cardiac implantable electronic devices and interventional electrophysiological procedures in the European Society of Cardiology Countries: 2017 Report from the European Heart Rhythm Association. Europace 2017;19:ii1–ii90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data collected for the study will be made available as supplementary material to anyone who wishes access it for any purpose. Data will include detailed counts of cardiac implantable electronic device placement from 2017 to April 2020, by type and centre. The data will be accessible immediately following publication with no end date.
Conflict of interest: E.A., MD, PhD, MSc: Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; Lluis Mont, MD, PhD: Speaking and consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic; Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; J.M.T., MD, PhD: Consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic; Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; R.B., MSc: Institutional support for fellowship programs from Abbott, Biotronik, Boston Scientific and Medtronic; N.R.-G., MD, PhD, MSc: Speaking honorarium from Abbott; J.F.-P., MD: Speaking honorarium from Abbott; Alba Santos-Ortega MD: Speaking honorarium from Abbott; J.M.G., MD, PhD: Speaking and consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic; E.R.-F., MD, PhD: Speaking and consulting honorarium from Abbott, Biotronik, Boston Scientific and Medtronic. Other authors declare no conflict of interests.