The pandemic coronavirus disease (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus has spread globally impacting health and economy on an unprecedented scale. Hundreds of thousands of patients are dying worldwide. Many are adult men with three or more pre-existent comorbidities, especially metabolic syndrome (MS) and cardiovascular diseases (CVDs). Although COVID-19 is primarily a respiratory infection, patients with MS and CVDs experience disproportionately worse outcomes. Until an effective vaccine or a drug against SARS-CoV-2 become available, the only strategy appears to be a combination of social isolation, contact tracing and rapid diagnosis.1
In an attempt to hinder the spread of COVID-19, governments are taking measures that tighten the quarantine, requiring all citizens to stay home as much as possible. These measures have deleterious consequences on everyone’s life. Among others, there is also a serious concern related to the deleterious effects of physical inactivity. All sports events have been suspended or cancelled. As human droplets are the main vehicle of contagion, during physical activities, and especially in group activities, hyperventilation increases the risk of infection, despite maintaining the suggested social distance of 1.5 m. It has been reported that, under various combinations of environmental and patient conditions, droplets of all sizes can travel up to 7–8 m.2 However, to the best of our knowledge, there is no rigorous study investigating droplet spread during hard effort such as running or cycling. In addition, sports-related injury should be limited as hospitals are already engaged with the massive number of cases of COVID-19. Thus, on the one hand the limitation of physical activities serves to counteract the COVID-19 outbreak, on the other hand this certainly entails problems related to the abrupt interruption and/or severe limitation of physical activities.
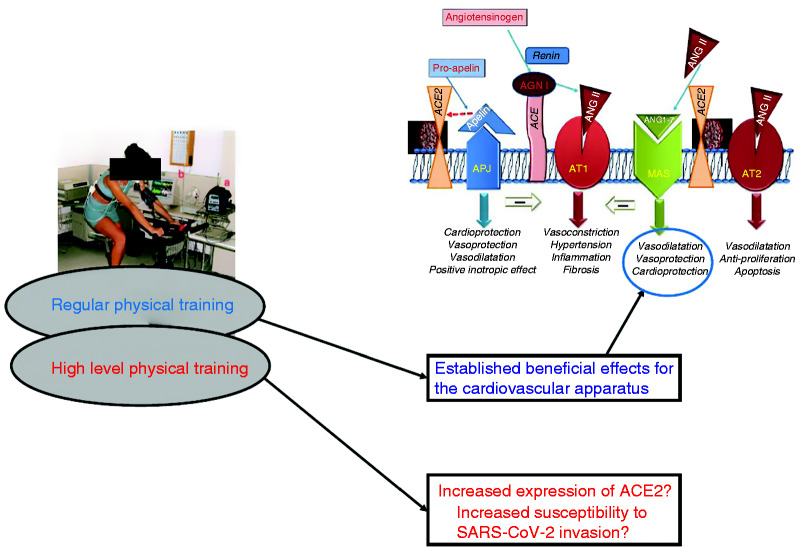
The SARS-CoV-2 virus is linked to the renin–angiotensin system (RAS), which plays a central role in blood pressure regulation and in the body’s response to exercise. However, regular physical activity affects RAS functioning.3 In this commentary, we highlight this RAS–COVID-19 relationship and analyse the possible consequences of a severe limitation of physical activity during this pandemic (see Figure 1).
Figure 1.
Simplified diagram showing the connection between physical training and the renin–angiotensin system. Top insert: schematic model of the angiotensin-converting enzyme (ACE) and ACE2 interactions at the cell membrane level. These two enzymes are aminopeptidases that remove amino acids from precursors to obtain ligands (i.e. angiotensin ANG II and ANG 1-7), which will bind to receptors (ANG II receptor (AT) ANG 1-7 receptor (MAS), respectively) obtaining specific effects on the cardiovascular system. Physical training can affect ACE2 expression, while coronavirus can interfere with ACE2 activity. Also apelin and its G-protein coupled receptor (APJ) are linked to ACE2 and apelin overexpression has been linked to physical training.
The classic angiotensin-converting enzyme (ACE) and ACE2 are two important enzymes of RAS. These enzymes and their products act in balancing each other: while ACE converts angiotensin-I to angiotensin-II (Ang-II), a potent vasoconstrictor, ACE2 leads to the formation of angiotensin 1-7 (Ang-1-7), a potent vasodilator.4 Ang-II binding to type 1 receptors (AT1) also induces sympathetic activation, reactive oxygen species (ROS) generation and endothelial dysfunction, as well as the induction of inflammatory, thrombotic, proliferative and fibrotic processes. On the contrary, Ang-1-7 binding to the Mas receptor (MasR) mediates anti-inflammatory, anti-proliferative and anti-oxidative effects. These different effects explain their opposite role in hypertension, MS, diabetes and CVDs.4 Therefore, ACE, ACE2 and their products have multiple and opposite effects in the RAS and in exercise training (see Figure 1).3
In order to enter target cells, SARS-CoV-2 uses transmembrane protease serine 2 (TMPRSS2) to split the virus spike protein and uses ACE2 as a cellular receptor. The maximum expression of ACE2 is observed in the organs targeted by the virus, namely the lungs, kidneys, heart and their endothelium. Therefore, ACE2 could play a role in the mechanism of acute myocardial injury induced by COVID-19.1,5
The ACE2/Ang-1-7/MasR arm of the RAS exerts beneficial effects in skeletal muscle and is needed to develop muscle hypertrophy during exercise training. Actually, ACE2 knockout mice do not show muscle hypertrophy after exercise training. Moreover, Ang-1-7 has anti-atrophic effects and improves insulin sensitivity in skeletal muscles. However, Ang-1-7 acting on MasR stimulates the phosphorylation/activation of Akt, an enzyme involved in insulin signalling, and in cell survival and growth.6,7 Although in several CVDs there is an upregulation of the ACE/Ang-II/AT1 arm of the RAS, exercise training shifts the balance of the RAS towards the protective arm (ACE2/Ang1-7/MasR).3 ACE2 knockout mice spontaneously perform low exercise volumes and do not benefit in body composition.6 Studies suggest that a high exercise volume is necessary to shift the balance of RAS towards the ACE2/Ang-1-7/Mas receptor axis.3,6 Studies on the ACE genotype and RAS polymorphism demonstrated that RAS might also modulate the effect of exercise training in humans.8 COVID-19 infection, affecting lung and cardiovascular function, impairs exercise capacity. In addition, the inevitable quarantine and restrictions imposed by governments during the outbreak could exacerbate the negative consequences of the infection itself.
A sedentary lifestyle is the potential leading cause of CVDs, which are the major cause of death in the world. Due to mandatory homestay, the COVID-19 outbreak will probably worsen this situation because of the reduction in both habitual and recreational physical activities. The World Health Organization suggests that ‘Adults aged 18–64 should do at least 150 minutes of moderate-intensity aerobic physical activity or do at least 75 minutes of vigorous-intensity aerobic physical activity throughout the week or an equivalent combination of moderate and vigorous-intensity activity.’ (https://www.who.int/dietphysicalactivity/factsheet_adults/en/). Clearly it is very difficult to comply with these WHO recommendations for citizens in lockdown areas.
The notion that physical activity is cardioprotective and that being sedentary is a risk factor for MS and CVDs is supported by the great bulk of evidence. Regular physical activity has a significant impact in reducing the total and cardiac mortality rate. Moreover, exercise is a useful tool for cardiovascular rehabilitation. Conversely, inactive individuals have about a two-fold higher relative risk of coronary artery disease in comparison with physically active people. To support further the concept that regular physical activity is a good practice to stay healthy, there is evidence that physical capacity is a good predictor of the increased risk of death from any cause in healthy individuals as well as in patients with CVDs.
Regular physical activity reduces several risk factors related to CVDs. Besides the shift of the RAS balance towards the protective arm (ACE2/Ang1-7/MasR),3 improvement in insulin sensitivity, enhancement in endothelial functions, structural adaptations in the coronary tree and a reduction in autonomic activity and in vascular resistance and blood pressure have all been reported.9–11
Considering the positive effects of physical activity on the general and cardiovascular health state, it is advisable that the population keeps exercising at home. Good tools are treadmills, stationary bikes and rowing machines. The use of fitness balls, elastic bands and weights is advisable. Exercise driven by video and online-guided protocols may be very useful. Even going up and down the stairs can help. Local authorities should consider allowing, whenever possible, some outdoor activities with a sufficient interpersonal distance (more than 1.5 m). In this regard, a study investigating the distance reached by droplets during efforts is warranted.
While there is no doubt that an active lifestyle confers protection against CVDs, some potential controversy regarding ACE2 expression deserves much attention, especially considering that it is necessary for the beneficial effects of exercise, but it provides the pathway for the SARS-CoV-2 virus to enter the body. Although never proved in humans, an overexpression of ACE2 has been demonstrated in animal models of high volume exercise training. Moreover, once the body is infected, the SARS-CoV-2 virus has the capacity to deplete ACE2.3,6
The potential overexpression of ACE2 in highly trained athletes may lead us to hypothesise that, despite their good health, they are more sensitive to SARS-CoV-2 invasion and COVID-19 consequences. Thus, it can be speculated that they may be more sensitive to RAS homeostasis perturbation by COVID-19. This is somehow similar to the hypothesised deleterious effects of ACE inhibitors and AT1 blockers. These hypotheses/speculations deserve attention and require appropriate investigations, but there is no evidence to recommend stopping exercise or stopping ACE inhibitors.12 Whereas there are no data on the potential risks related to COVID-19 in people with high-level training, there is evidence that MS worsens COVID-19, while exercise is beneficial in the general population. Thus, exercise benefits may outweigh the hypothesised risks.
One challenging point is how to distance people during exercise. There is an urgent need for rigorous investigations on droplet spread during hard efforts. In the meantime, as droplets can probably travel for several metres during hyperventilation, the use of masks during exercise appears to be mandatory.
It is clearly a challenge for governments to decide when the benefits of a reduction of cardiovascular risks with exercise surpass the need for strict measures for containment of the epidemic. In our opinion people should, in any case, keep exercising at home whenever possible. Jogging alone and wearing a mask could be a step forward when epidemic conditions improve (i.e. the prevalence and increase in new cases are appreciably reduced). We are only at the beginning of the battle against this terrible pandemic, so let’s run!
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Liu PP, Blet A, Smyth D, et al. The science underlying COVID-19: implications for the cardiovascular system. Circulation 2020; in press. [DOI] [PubMed] [Google Scholar]
- 2. Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19. JAMA 2020; in press. [DOI] [PubMed] [Google Scholar]
- 3. Frantz EDC, Prodel E, Braz ID, et al. Modulation of the renin–angiotensin system in white adipose tissue and skeletal muscle: focus on exercise training. Clin Sci (Lond) 2018; 132: 1487–1507. doi: 10.1042/CS20180276. [DOI] [PubMed] [Google Scholar]
- 4. Pagliaro P, Penna C.. Rethinking the renin–angiotensin system and its role in cardiovascular regulation. Cardiovasc Drugs Ther 2005; 19: 77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020; 181: 271–280.e8. doi:10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Motta-Santos D, Dos Santos RA, Oliveira M, et al. Effects of ACE2 deficiency on physical performance and physiological adaptations of cardiac and skeletal muscle to exercise. Hypertens Res 2016; 39: 506–512. [DOI] [PubMed] [Google Scholar]
- 7. Muñoz MC, Giani JF, Dominici FP.. Angiotensin-(1-7) stimulates the phosphorylation of Akt in rat extracardiac tissues in vivo via receptor Mas. Regul Pept 2010; 161: 1–7. doi: 10.1016/j.regpep.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 8. Hamada T, Kotani K, Nagai N, et al. Genetic polymorphisms of the renin-angiotensin system and obesity-related metabolic changes in response to low-energy diets in obese women. Nutrition 2011; 27: 34–39. 10.1016/j.nut.2009.10.012 [DOI] [PubMed] [Google Scholar]
- 9. Crisafulli A, Pagliaro P, Roberto S, et al. Diabetic cardiomyopathy and ischemic heart disease: prevention and therapy by exercise and conditioning. Int J Mol Sci 2020; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kemps H, Kränkel N, Dörr M, et al. Exercise training for patients with type 2 diabetes and cardiovascular disease: what to pursue and how to do it. A Position Paper of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol 2019; 26: 709–727. [DOI] [PubMed] [Google Scholar]
- 11. Kränkel N, Bahls M, Van Craenenbroeck EM, et al. Exercise training to reduce cardiovascular risk in patients with metabolic syndrome and type 2 diabetes mellitus: how does it work? Eur J Prev Cardiol 2019; 26: 701–708. [DOI] [PubMed] [Google Scholar]
- 12. Rossi GP, Sanga V, Barton M.. Potential harmful effects of discontinuing ACE-inhibitors and ARBs in COVID-19 patients. Elife 2020; 9: pii: e57278. doi: 10.7554/eLife.57278. [DOI] [PMC free article] [PubMed] [Google Scholar]