Graphical Abstract
This editorial refers to ‘All-cause mortality and location of death in patients with established cardiovascular disease before, during, and after the COVID-19 lockdown: a Danish nationwide cohort study’, by J. Butt et al., doi:10.1093/eurheartj/ehab028.
The coronavirus disease 2019 (COVID-19) pandemic is an unprecedented global public health emergency that has dramatically changed all aspects of our lives. To date, the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected almost 100 million people and directly caused >2 million deaths.1 To prevent the spread of the virus and relieve pressure on healthcare services, governments enforced lockdown measures. At the same time, healthcare systems rapidly repurposed by redeploying resources and staff to tackle this unique challenge. These strategies limited the impact of the first wave of COVID-19 but disrupted usual care pathways for non-COVID-19 conditions.
The prevalence of cardiovascular diseases has consistently increased over time as effective interventions have prolonged survival. Despite this, they are still the leading cause of morbidity and mortality worldwide, mandating ongoing efforts to provide prompt diagnosis, complex interventions, structured follow-up, and uninterrupted care.2 The advent of the COVID-19 pandemic has abruptly discontinued this continuum of care for all cardiovascular conditions, with potentially devastating consequences.
In this issue of the European Heart Journal, Butt et al. provide an interesting analysis of the impact of the COVID-19 pandemic on patients with cardiovascular disease in Denmark.3 Using the Danish nationwide registry, the authors did not find a difference in overall mortality for patients with established cardiovascular disease compared with the same period in 2019, despite lockdown measures and healthcare reconfiguration. They found lower in-hospital mortality that was, unfortunately, counter-balanced by higher out-of-hospital mortality. This important contribution adds to a growing literature on outcomes for patients admitted to hospital with cardiovascular disease during the COVID-19 pandemic. Furthermore, this report is one of the first to describe parallel changes in out-of-hospital mortality of patients with cardiovascular conditions and the temporal association with lockdown measures.
The COVID-19 pandemic has affected countries differently for several reasons, including the timing and extent of lockdown measures, which have ranged from almost none to severe draconian approaches. These measures were typically accompanied by public health messages urging the public to stay at home whenever possible. Most countries have struggled to manage the dramatic increase in demand for healthcare during the COVID-19 pandemic, and many systems have been stretched significantly, to the verge of collapse. The reconfiguration of both primary and secondary care has included the redeployment of medical staff, sudden cessation of routine face-to-face appointments, interruption of established care pathways, and reduced availability of medical facilities. Together with the public’s hesitancy to present to primary or secondary care, for new and established cardiovascular diseases, this has resulted in important changes in hospital admissions for cardiovascular conditions (Table 1).3–22 Most reports have consequently described a significant reduction in admission rates, including for acute coronary syndromes and acute heart failure.3,8,14,16,17,23 Patients often presented later, sicker, and with a higher prevalence of comorbidities.5,17,23 Moreover, in-hospital management changed: patients with cardiovascular conditions requiring admission were more frequently admitted to general medical wards, and had shorter lengths of stay and increased complication rates for invasive procedures.7,8,14,16,19 In this situation, despite lower absolute admission numbers, the resilience of healthcare systems to accommodate patients with more advanced disease was limited, ultimately leading to higher in-hospital mortality rates.5,7,13–15,19
Table 1.
Effect of the COVID-19 pandemic on hospitalizations for cardiovascular conditions, mortality rates, and excess cardiovascular mortality worldwide, regardless of infection rates
| Study | COVID-19 impact | Country | Admission rate | In-hospital mortality | Out-of-hospital mortality | Overall CV mortality | Excess CV mortality |
|---|---|---|---|---|---|---|---|
| All CV conditions | |||||||
| Butt et al.3 | Low | Denmark | – | ↓ | ↑ | ↔ | 0% |
| Brant et al.4 | High | Brazil | – | – | – | ↑ | 4% |
| Konig et al.5 | Moderate | Germany | ↓ | ↑ | – | – | 1% |
| Del Pinto et al.6 | Lowa | Italy | ↓ | ↔ | – | – | –1% |
| Wu et al.7 | High | UK | – | ↔ | ↑ | ↑ | 8% |
| Bhatt et al.8 | High | USA | ↓ | ↔ | – | – | 2% |
| Acute coronary syndrome | |||||||
| Mesnier et al.9 | High | France | ↓ | ↔ | – | – | 2% |
| Popovic et al.10 | High | France | ↓ | ↑ | – | – | 22% |
| Nef et al.11 | Moderate | Germany | ↓ | – | – | ↑ | 12% |
| Primessnig et al.12 | Moderate | Germany | ↓ | ↑ | – | – | 13% |
| Tam et al.13 | High | Hong Kong | ↓ | ↑ | – | – | 7% |
| De Rosa et al.14 | High | Italy | ↓ | ↑ | – | – | 7% |
| Wilson et al.15 | High | UK | ↓ | ↔ | – | – | 3% |
| Gluckman et al.16 | High | USA | ↓ | ↔ | – | – | 0% |
| Heart failure | |||||||
| Andersson et al.17 | Low | Denmark | ↓ | ↔ | – | ↔ | 0% |
| Bollmann et al.18 | Moderate | Germany | ↓ | ↑ | – | – | 2% |
| Cannata et al.19 | High | UK | ↓ | ↑ | – | – | 3% |
| Doolub et al.20 | High | UK | ↓ | ↑ | – | – | 10% |
| Out-of-hospital cardiac arrest | |||||||
| Marijon et al.21 | High | France | ↑ | ↑ | ↑ | ↑ | 2% |
| Baldi et al.22 | High | Italy | ↑ | ↑ | ↑ | ↑ | 6% |
CV, cardiovascular.
Relatively low impact region for COVID cases at the time of the analysis.
Denmark promptly implemented local restrictions and experienced a relatively low burden of COVID-19 compared with some other countries.3 This might have resulted in the preservation of specialist hospital care that, despite the reconfiguration of medical services, contributed to avoid the excess in-hospital mortality compared with non-pandemic periods.3 Nonetheless, the implications for countries that have been more aggressively affected have been more unfavourable,5,7,13–15,17,19,23–25 and the findings of Butt et al.3 should be interpreted in the context of the wider sequelae of COVID-19.
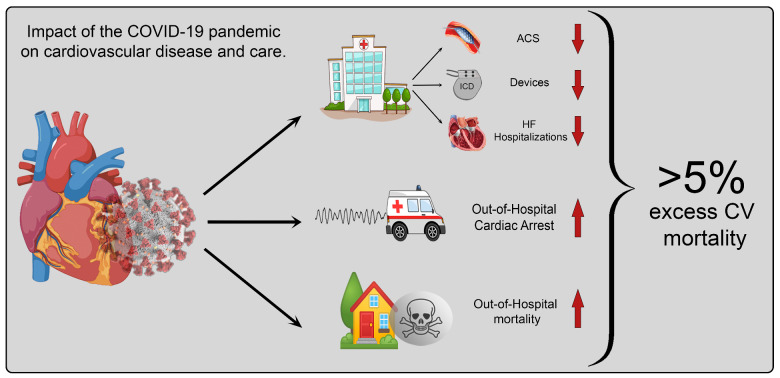
On the other hand, less is known about out-of-hospital mortality due to cardiovascular disease during the COVID-19 pandemic. To date, this is one of the few reports addressing this important topic. As reported by Butt et al., out-of-hospital mortality was significantly higher in Denmark during the lockdown, although it had a limited impact on overall mortality.3 The higher out-of-hospital mortality also reported in other countries has been attributed to lockdown restrictions and reluctance to seek medical care.3,7,24 Furthermore, delayed provision of medical help resulted in higher rates of out-of-hospital cardiac arrest during the COVID-19 pandemic, which was associated with increased response times and a significant reduction in advanced life support for these patients.25 Together with increased in-hospital mortality, these factors have combined to worsen overall outcomes and result in significant excess mortality for patients with cardiovascular diseases7,24 (Graphical abstract).
Graphical abstract.
Impact of the COVID-19 pandemic on patients with cardiovascular disease worldwide.
ACS, acute coronary syndrome; CV, cardiovascular; HF, heart failure; ICD, implantable cardioverter-defibrillator.
To date, while we continue to experience further waves of the COVID-19 pandemic, exacerbated by the advent of new strains of the virus, we can only as yet hypothesize about a detailed and comprehensive evaluation of the global collateral damage. The potential global implications for patients with cardiac disease relate to missed or delayed diagnosis, reduced availability of routine testing, interrupted referral pathways, lack of proper and timely optimization of medical treatment, prevention of exacerbations, postponed or cancelled follow-ups, and reduced specialist care. Similarly, disruption in research, education, teaching, training, and personal growth for healthcare professionals will compound these insults. Furthermore, several hitherto uncharacterized features of the pandemic are likely to have affected cardiovascular health, including lifestyle changes, reduction in physical exercise, home working, disrupted education for pupils, reduced social interactions, more perilous mental health, and socioeconomic hardship. These may play a substantial role, in both the short and long term, in how history views the interplay between the COVID-19 pandemic and cardiovascular disease. These and other, as yet undetermined, social and medical factors will undeniably contribute to the longstanding impact of the COVID-19 pandemic. Therefore, the available reports of short-term out-of-hospital mortality are certain to be only the tip of the iceberg.
While it appears crucial to continue specialist and uninterrupted medical care for at-risk groups, including those with cardiovascular conditions, further research is needed to better understand the full scope of contributory factors to cardiovascular mortality during the COVID-19 pandemic, beyond infection rates. This information is essential to determine the best approaches to caring for patients, improving outcomes in extreme conditions, and minimizing collateral damage in future outbreaks. Novel analyses, like the elegant one published in this issue of the journal,3 are needed and welcome to address direct and indirect consequences of the pandemic. However, while comprehensive research will help us better understand the implications for patients with cardiovascular disease, for now, the full effect of the COVID-19 pandemic on cardiovascular disease cannot yet be seen. Only history will reveal the depth of the iceberg.
Acknowledgments
We are grateful to the staff of the King’s College Hospital who helped in the fight against COVID-19, and to all the people who supported research during these unprecedented times.
Conflicts of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. World Health Organization WHO. Coronavirus disease 2019 (COVID-19) Situation Report. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (28 January 2021).
- 2. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Butt J, Fosbøl E, Gerds T, Andersson C, Kragholm K, Biering-Sørensen T, Andersen J, Phelps M, Porsborg Andersen M, Gislason G, Torp-Pedersen C, Køber L, Schou M. All-cause mortality and location of death in patients with established cardiovascular disease before, during, and after the COVID-19 lockdown: a Danish nationwide cohort study. Eur Heart J 2021;doi:10.1093/eurheartj/ehab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brant LCC, Nascimento BR, Teixeira RA, Lopes MACQ, Malta DC, Oliveira GMM, Ribeiro ALP. Excess of cardiovascular deaths during the COVID-19 pandemic in Brazilian capital cities. Heart 2020;106:1898–1905. [DOI] [PubMed] [Google Scholar]
- 5. Konig S, Hohenstein S, Meier-Hellmann A, Kuhlen R, Hindricks G, Bollmann A; Helios Hospitals, Germany. In-hospital care in acute heart failure during the COVID-19 pandemic: insights from the German-wide Helios hospital network. Eur J Heart Fail 2020;22:2190–2201. [DOI] [PubMed] [Google Scholar]
- 6. Del Pinto R, Ferri C, Mammarella L, Abballe S, Dell’Anna S, Cicogna S, Grassi D, Sacco S, Desideri G. Increased cardiovascular death rates in a COVID-19 low prevalence area. J Clin Hypertens (Greenwich) 2020;22:1932–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wu J, Mamas MA, Mohamed MO, Kwok CS, Roebuck C, Humberstone B, Denwood T, Luescher T, de Belder MA, Deanfield JE, Gale CP. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart 2021;107:113–119. [DOI] [PubMed] [Google Scholar]
- 8. Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, Januzzi JL, Butler J, Adler DS, Solomon SD, Vaduganathan M. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol 2020;76:280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, Thuaire C, Angoulvant D, Cayla G, Bouleti C, Gallet de Saint Aurin R, Goube P, Lhermusier T, Dillinger JG, Paganelli F, Saib A, Prunier F, Vanzetto G, Dubreuil O, Puymirat E, Boccara F, Eltchaninoff H, Cachanado M, Rousseau A, Drouet E, Steg PG, Simon T, Danchin N. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Public Health 2020;5:e536–e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Popovic B, Varlot J, Metzdorf PA, Jeulin H, Goehringer F, Camenzind E. Changes in characteristics and management among patients with ST-elevation myocardial infarction due to COVID-19 infection. Catheter Cardiovasc Interv 2020; doi: 10.1002/ccd.29114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nef HM, Elsässer A, Möllmann H, Abdel-Hadi M, Bauer T, Brück M, Eggebrecht H, Ehrlich JR, Ferrari MW, Fichtlscherer S, Hink U, Hölschermann H, Kacapor R, Koeth O, Korboukov S, Lamparter S, Laspoulas AJ, Lehmann R, Liebetrau C, Plücker T, Pons-Kühnemann J, Schächinger V, Schieffer B, Schott P, Schulze M, Teupe C, Vasa-Nicotera M, Weber M, Weinbrenner C, Werner G, Hamm CW, Dörr O; CoVCAD Study Group. Impact of the COVID-19 pandemic on cardiovascular mortality and catherization activity during the lockdown in central Germany: an observational study. Clin Res Cardiol 2021;110:292–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Primessnig U, Pieske BM, Sherif M. Increased mortality and worse cardiac outcome of acute myocardial infarction during the early COVID-19 pandemic. ESC Heart Fail 2020;8:333–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, Fang J, Tse HF, Siu CW. Impact of coronavirus disease 2019 (COVID-19) outbreak on outcome of myocardial infarction in Hong Kong, China. Catheter Cardiovasc Interv 2020;doi: 10.1002/ccd.28943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Perrone Filardi P, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C; Società Italiana di Cardiologia and the CCU Academy Investigators Group. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020;41:2083–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wilson SJ, Connolly MJ, Elghamry Z, Cosgrove C, Firoozi S, Lim P, Sharma R, Spratt JC. Effect of the COVID-19 pandemic on ST-segment-elevation myocardial infarction presentations and in-hospital outcomes. Circ Cardiovasc Interv 2020;13:e009438. [DOI] [PubMed] [Google Scholar]
- 16. Gluckman TJ, Wilson MA, Chiu ST, Penny BW, Chepuri VB, Waggoner JW, Spinelli KJ. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol 2020;5:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andersson C, Gerds T, Fosbol E, Phelps M, Andersen J, Lamberts M, Holt A, Butt JH, Madelaire C, Gislason G, Torp-Pedersen C, Kober L, Schou M. Incidence of new-onset and worsening heart failure before and after the COVID-19 epidemic lockdown in Denmark: a nationwide cohort study. Circ Heart Fail 2020;13:e007274. [DOI] [PubMed] [Google Scholar]
- 18. Bollmann A, Hohenstein S, König S, Meier-Hellmann A, Kuhlen R, Hindricks G. In-hospital mortality in heart failure in Germany during the Covid-19 pandemic. ESC Heart Fail 2020;7:4416–4419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cannatà A, Bromage DI, Rind IA, Gregorio C, Bannister C, Albarjas M, Piper S, Shah AM, McDonagh TA. Temporal trends in decompensated heart failure and outcomes during COVID-19: a multisite report from heart failure referral centres in London. Eur J Heart Fail 2020;22:2219–2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Doolub G, Wong C, Hewitson L, Todd F, Mohamed A, Gogola L, Skyrme-Jones A, Aziz S, Sammut E, Dastidar A. Impact of COVID-19 on inpatient referral of acute heart failure: a single-centre experience from the south-west of the UK. ESC Heart Fail 2021;doi: 10.1002/ehf2.13158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, Sharifzadehgan A, Waldmann V, Beganton F, Narayanan K, Lafont A, Bougouin W, Jouven X. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France : a population-based, observational study. Lancet Public Health 2020;5:e437–e443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S; Lombardia CARe Researchers. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J 2020;41:3045–3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bromage DI, Cannatà A, Rind IA, Gregorio C, Piper S, Shah AM, McDonagh TA. The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic. Eur J Heart Fail 2020;22:978–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kontis V, Bennett JE, Rashid T, Parks RM, Pearson-Stuttard J, Guillot M, Asaria P, Zhou B, Battaglini M, Corsetti G, McKee M, Di Cesare M, Mathers CD, Ezzati M. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat Med 2020;26:1919–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Bua D, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S; Lombardia CARe Researchers. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med 2020;383:496–498. [DOI] [PMC free article] [PubMed] [Google Scholar]